Abstract
Diabetic cardiomyopathy (DCM), as one of the major cardiac complications in diabetic patients, is known to related with oxidative stress that is due to a severe imbalance between reactive oxygen species (ROS) and/or reactive nitrogen species (RNS) generation and their clearance by antioxidant defense systems. Transcription factor nuclear factor NF-E2-related factor 2 (Nrf2) plays an important role in maintaining the oxidative homeostasis by regulating multiple downstream antioxidants. Diabetes may up-regulate several antioxidants in the heart as a compensative mechanism at early stage, but at late stage, diabetes not only generates extra ROS and/or RNS but also impairs antioxidant capacity in the heart, including Nrf2. In an early study, we have established that Nrf2 protect the cardiac cells and heart from high level of glucose in vitro and hyperglycemia in vivo, and in the following study demonstrated the significant down-regulation of cardiac Nrf2 expression in diabetic animals and patients. Using Nrf2-KO mice or Nrf2 inducers, blooming evidence has indicated the important protection by Nrf2 from cardiac pathogenesis in the diabetes. Therefore, this brief review summarizes the status of studies on Nrf2's role in preventing DCM and even other complications, the need for new and safe Nrf2 inducer screening and the precaution for the undesirable side of Nrf2 under certain conditions.
Keywords: Antioxidant therapy, Diabetic cardiomyopathies, Nrf2, Oxidative stress
INTRODUCTION
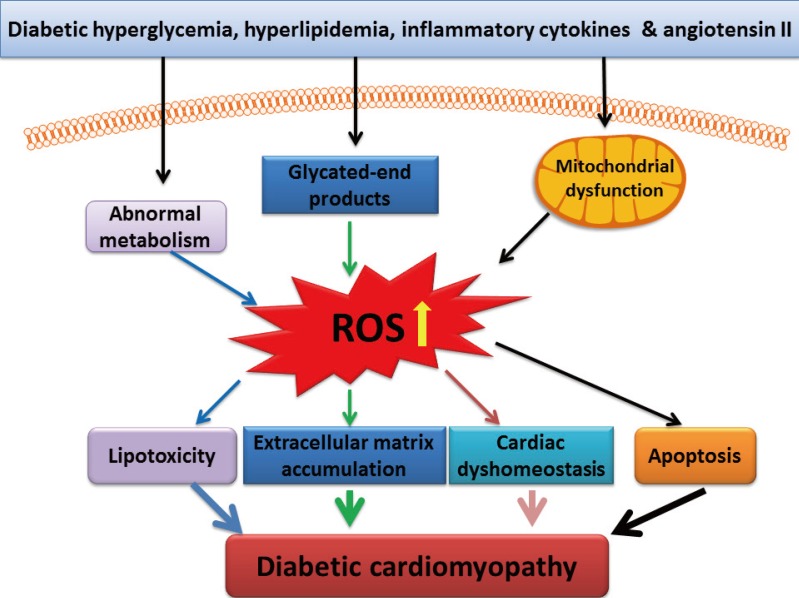
Diabetic cardiomyopathy (DCM) is one of the major cardiac complications in diabetic patients. Several mechanisms responsible for DCM have been proposed [1,2,3]: (1) impaired regulation of intracellular calcium, leading to impaired cardiac contractility; (2) mitochondrial dysfunction, leading to over-production of reactive oxygen species (ROS), reactive nitrogen species (RNS), and eventually cardiac cell death; (3) accumulation of advanced glycated end-products in the heart, leading to extracellular matrix accumulation that in turn results in cardiac diastolic dysfunction and eventually functional failure; (4) abnormal cellular metabolism, leading to accumulation of toxic lipids in the heart; and (5) essential trace metal dyshomeostasis such as zinc and copper. Although these pathogeneses may be primarily caused by hyperglycemia, other pathogenic factors including hyperlipidemia, inflammatory cytokines, and angiotensin system such as angiotensin II also play important roles in the initiation or progression of DCM. These pathogenic factors cause the pathogenesis of DCM probably via different mechanisms, but all these effects are thought related to oxidative stress [1,3,4,5,6], as illustrated in Fig. 1.
Fig. 1.
Pathological responses mediated by reactive oxygen species (ROS) in the diabetic cardiomyopathy. ROS are involved in lipotoxicity, extracellular matrix accumulation, calcium dyshomeostasis, and apoptosis.
ANTIOXIDANT THERAPY AND METALLOTHIONEIN
Oxidati vestress indicates a severe imbalance between ROS and/or RNS generation and their clearance by antioxidant defense systems [3]. Due to low contents of antioxidants in the normal heart compared to other organs, the heart is a highly susceptible organ to oxidative stress and damage [7,8]. Diabetes may up-regulate several antioxidants in the heart as a compensative mechanism at early stage, but at late stage, diabetes not only generates extra ROS and/or RNS but also impairs antioxidant capacity in the heart [4,9]. Decreased expression of heat shock protein 60 and heme oxygenase-1 in the diabetic heart made the heart high susceptible to oxidative damage [9,10,11]. Therefore, antioxidant therapy for DCM has been attractive, but its outcomes to prevent cardiac complications in diabetic patients by dietary supplementation of antioxidants are controversial [12,13,14]. Several reasons including the difficulty in maintaining a consistent circulating antioxidant levels for supplied exogenous antioxidants, inadequate tissue distribution, and lack of suitable exogenous antioxidants have been discussed [3,14,15]. This might be one of the reasons that single or a few of antioxidants together would remove limited kinds of free radicals while diabetes can induce multiple kinds of free radicals.
This concept may be implicated by the action of metallothionein (MT). MT is a cysteine-rich (1/3 of 61 amino acids) and binds zinc under physiological condition [16,17,18]. As a nonspecific antioxidant, MT is able to quench a wide of free radicals, including superoxide, hydrogen peroxide, hydroxyl radical, and peroxynitrite [16,17,18]. We have shown that MT as a potent, nonspecific antioxidant significantly prevented various diabetic complications in animal models and human, suggesting its great potential for clinical application to prevent DCM [5,15,19,20,21,22,23,24]. However, MT remains a single antioxidant, which promotes us to further look for an approach to up-regulating multiple antioxidants, including MT, for efficiently preventing diabetic complications.
THE TRANSCRIPTION FACTOR NUCLEAR Nrf2
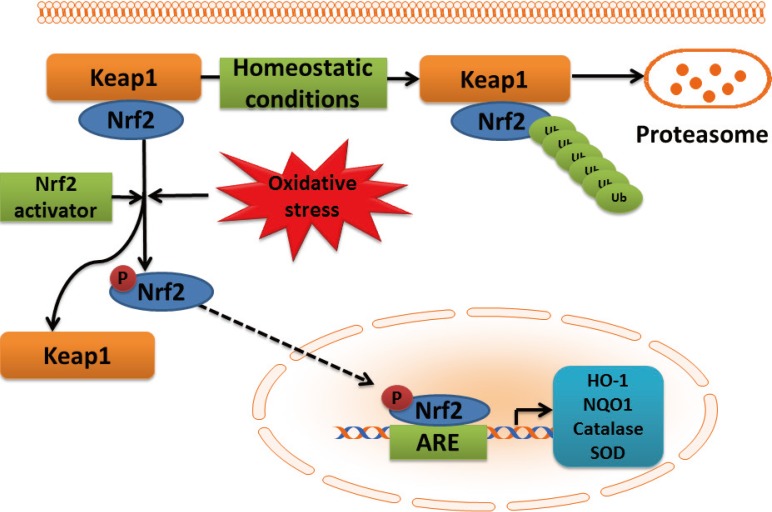
Cells contain a number of genes coding many proteins to counteract ROS-, RNS-, or electrophile-mediated injury. Transcriptional regulation of these protective genes is controlled in part through antioxidant response elements (AREs) [25,26]. The transcription factor nuclear factor NF-E2-related factor 2 (Nrf2) plays an important role in ARE-mediated basal and inducible expression of more than 200 genes that can be grouped into several categories including antioxidant genes and phase II detoxifying enzymes [25,26], as outlined in Fig. 2. These antioxidant components include heme oxygenase-1, thioredoxin reductase, glutathione-S-transferase, and NAD(P)H:quinone oxidoreductase (NQO)-1, antioxidant enzymes such as superoxide dismutase and catalase, and nonenzymatic scavengers such as glutathione. The protein stability and transcriptional activity of Nrf2 is principally regulated by a BTB-Kelch protein, Keap1 that functions as a substrate adaptor for a cullin (Cul)3-dependent E3 ubiquitin ligase complex. Keap1 targets Nrf2 for ubiquitination and subsequent degradation by the 26S proteasome [25,26].
Fig. 2.
Schematic presentation of NF-E2-related factor 2 (Nrf2)-antioxidant response element (ARE) pathway activation by reactive oxygen species (ROS). In the cytoplasm, under normal conditions, Nrf2 is constitutively bound to Keap1 protein. Keap1 inhibits Nrf2 signaling pathway by promoting Nrf2 ubiquitination and subsequent degradation through proteasomal pathway. Mild oxidative stress and Nrf2 activators cause dissociation of Nrf2-Keap1 complex, phosphorylation of Nrf2, and the nuclear translocation. In the nucleus, Nrf2 promotes transcriptional activation of antioxidants (heme oxygenase-1 [HO-1], NAD(P)H:quinone oxidoreductase 1 [NQO1], catalase, and superoxide dismutase [SOD]) and detoxifying enzymes by binding to the ARE in the promoter regions of the target genes.
In an early study, we have indicated the important role of Nrf2 in preventing high glucose-induced production of ROS and apoptotic cell death in both primary neonatal and adult cardiomyocytes from the mice with deletion of the Nrf2 gene (Nrf2-KO) than those from the Nrf2 wild-type mice [27]. Primary adult cardiomyocytes from Nrf2-KO diabetic mice showed a loss of isoproterenol-stimulated contraction compared to those from Nrf2 wild-type diabetic mice. Our finding was the first one to establish Nrf2 as a critical regulator of defense against ROS in normal and diabetic hearts [27]. We further showed the significant down-regulation of cardiac Nrf2 expression in diabetic animals and patients [28]. Now it is clear that down-regulation of Nrf2 is a significant reason for the initiation of various diabetic complications [29,30]. Using Nrf2-KO mice or Nrf2 inducers blooming evidence has indicated the protection by Nrf2 from diabetes [31,32] and from various diabetic complications [33,34,35,36,37]. We have worked on the prevention of DCM and other diabetic complications with several Nrf2 inducers [33,35,38,39,40,41,42], as summarized in Table 1 [32,35,36,37,39,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60].
Table 1.
The effect of Nrf2 activators on diabetes and diabetic complications
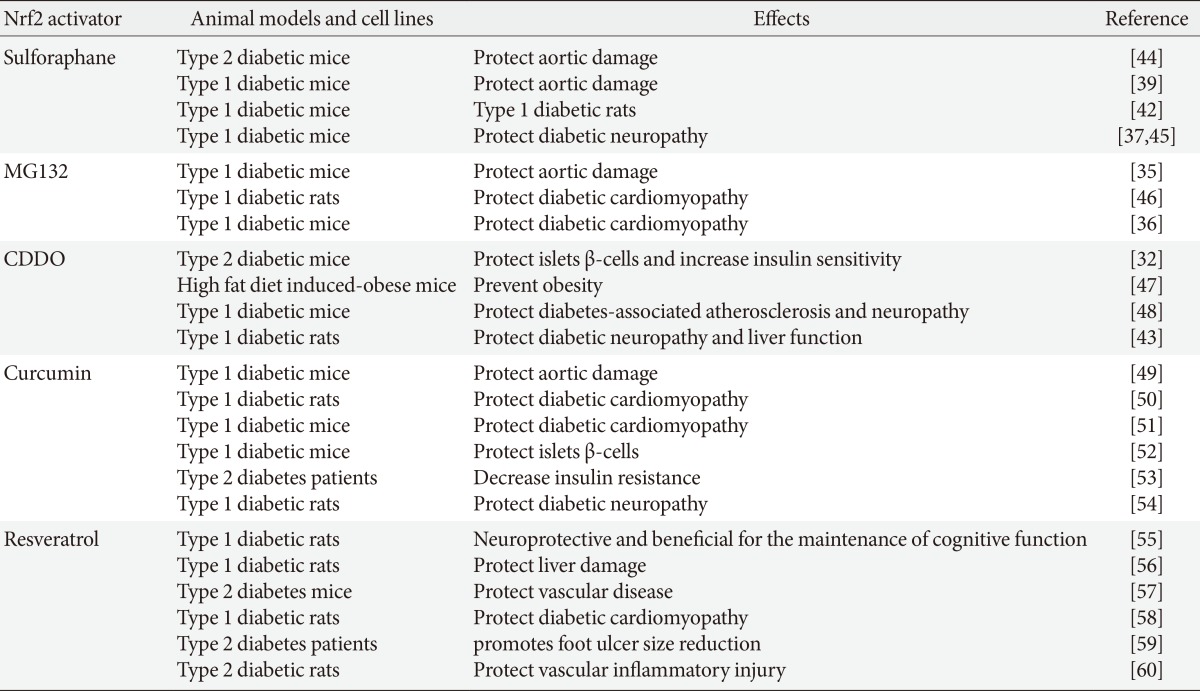
Nrf2, NF-E2-related factor 2; CDDO, 1-[2-cyano-3,12-dioxooleana-1,9(11)-dien-28-oyl].
The effective protection from diabetic complications by up-regulating Nrf2 function in animal models promoted clinical trials with Nrf2 inducer to prevent diabetic nephropathy. In 2011, the phase II clinical trial by following-up 52 weeks for the treatment of participants with moderate-to-severe diabetic kidney disease with bardoxolone methyl (BM) [61] reported the improvement of renal function compared to non-BM-treated diabetic patients. But the phase 3 clinical trial for the patients with advanced diabetic kidney disease [62] was prematurely terminated due to the strong adverse effects associated with BM treatment, including increased rates of heart failure and cardiovascular events. The failure of BM clinical trial suggests that more detail study in preclinical animal models is urgently needed before new clinical trials. Given the efficient prevention of diabetic complications with Nrf2 inducers in various animal models and the escalating human and societal costs of diabetic complications, efforts to find new safe and effective drugs via up-regulating Nrf2 remain vital [63,64,65,66].
Monascus-fermented metabolite monascin acts as a novel natural peroxisome proliferator-activated receptor-γ (PPARγ) agonist that improves insulin sensitivity, but dislike rosiglitazone, monascin was also able to activate Nrf2 to further elevate glyoxalase-1 expression. Monascin may be a novel natural Nrf2 activator with PPARγ-agonist activity. Therefore, monascin acts as an antidiabetic and antioxidative stress agent to a greater degree than rosiglitazone and thus may have therapeutic potential for the prevention of diabetes [67].
UNDESIRABLE SIDE OF Nrf2
It should be mentioned that everything has both sides; Nrf2 also has its undesirable side. It is well-known that ROS derived from multiple sources plays a causal role in multiple types of insulin resistance and contributes to β-cell dysfunction, leading to enhance the development and progression of type 2 diabetes, in another word: the detrimental ROS also plays a substantial role in the normal insulin signal transduction and glucose-stimulated insulin secretion in β-cell. Therefore persistent activation of Nrf2 gene may cause over-reduction of these required ROS signaling in the body. Consequently the detrimental effects of Nrf2 due to its aberrant activation have also been highlighted in recent years. A few of such examples include: (1) constitutive Nrf2 activation worsens insulin resistance, impairs lipid accumulation in adipose tissue, and increases hepatic steatosis in leptin-deficient mice [68]; (2) Nrf2 deficiency improves glucose tolerance in mice fed a high-fat diet [69]; and (3) Nrf2 deficiency prevents reductive stress-induced hypertrophic cardiomyopathy [70,71]. For instance, the latter cases highlighted that certain amount intracellular oxidative modification of proteins is a key event required for proper ubiquitination and protein degradation [72]. If substantial activation of Nrf2 may cause a significant decrease of protein oxidation in association with the induction of chronic reducing stress, which in turn causes deubiquitination and downstream protein degradation pathways, resulting in the development of cardiac hypertrophy and remodeling [70,71].
In addition, although the undesirable side of Nrf2 has been extensively mentioned in the cancer research field, Nrf2 has been shown to protect normal cells from tumor formation by decreasing the oxidative stress and preventing the DNA damage in cells. However, recently the cancer-promoting role of Nrf2 has been revealed. Nrf2 was found to be constitutively up-regulated in several types of human cancer tissues and cancer cell lines, and to protect tumors and cell lines from chemotherapeutic drugs [73,74].
CONCLUSIONS
In summary, the development and progression of DCM, one of the major cardiac complications in diabetic patients, is predominantly related to oxidative stress that is due to a severe imbalance between ROS and/or RNS generation and their clearance by antioxidant defense systems. In our body, cells have a well-established defense system against oxidative stress, such as Nrf2 that plays an important role in maintaining the oxidative homeostasis by regulating multiple downstream antioxidants. Diabetes, at late stage, not only generates extra ROS and/or RNS but also impairs antioxidant capacity in the heart, including Nrf2. We have demonstrated that Nrf2 protects the cardiac cells and heart from high level of glucose in vitro and hyperglycemia in vivo, respectively. We also found that diabetes significantly down-regulated cardiac Nrf2 expression in diabetic animals and patients, which might explain the development and progression of DCM. By using Nrf2-KO mouse model, the important role of Nrf2 in protecting various organs including the heart from diabetes has been extensively approved. Therefore various Nrf2 inducers have been explored with the objective of developing an applicable approach to pharmacologically up-regulate our systemic levels of Nrf2 in diabetic individuals for a prevention of their complications. Although the first candidate, bardoxolone methyl, has been failed in the phase II clinical trial that showed the potent cardiac toxicity when bardoxolone methyl was applied to diabetic patients with renal dysfunction, this could not stop searching for an efficient and safe new Nrf2 inducer. In addition, it also gradually is realized that anything can not be too much even though it is beneficial to us at most time. Similarly Nrf2 was found to also have its undesirable side when it is substantially and overexpressed. Therefore, when we continually explore for the approach to enhancing organ's Nrf2 expression with the purpose of prevention of cardiovascular complications, we also should keep in mind of its undesirable side under certain conditions.
ACKNOWLEDGEMENTS
The cited studies from the author's laboratory were supported in part by American Diabetes Association with the Basic Science Award (1-11-BS-17).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115:3213–3223. doi: 10.1161/CIRCULATIONAHA.106.679597. [DOI] [PubMed] [Google Scholar]
- 2.Monkemann H, De Vriese AS, Blom HJ, Kluijtmans LA, Heil SG, Schild HH, Golubnitschaja O. Early molecular events in the development of the diabetic cardiomyopathy. Amino Acids. 2002;23:331–336. doi: 10.1007/s00726-001-0146-y. [DOI] [PubMed] [Google Scholar]
- 3.Cai L, Kang YJ. Oxidative stress and diabetic cardiomyopathy: a brief review. Cardiovasc Toxicol. 2001;1:181–193. doi: 10.1385/ct:1:3:181. [DOI] [PubMed] [Google Scholar]
- 4.Hamblin M, Friedman DB, Hill S, Caprioli RM, Smith HM, Hill MF. Alterations in the diabetic myocardial proteome coupled with increased myocardial oxidative stress underlies diabetic cardiomyopathy. J Mol Cell Cardiol. 2007;42:884–895. doi: 10.1016/j.yjmcc.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cai L, Wang Y, Zhou G, Chen T, Song Y, Li X, Kang YJ. Attenuation by metallothionein of early cardiac cell death via suppression of mitochondrial oxidative stress results in a prevention of diabetic cardiomyopathy. J Am Coll Cardiol. 2006;48:1688–1697. doi: 10.1016/j.jacc.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Adeghate E. Molecular and cellular basis of the aetiology and management of diabetic cardiomyopathy: a short review. Mol Cell Biochem. 2004;261:187–191. doi: 10.1023/b:mcbi.0000028755.86521.11. [DOI] [PubMed] [Google Scholar]
- 7.Doroshow JH, Locker GY, Myers CE. Enzymatic defenses of the mouse heart against reactive oxygen metabolites: alterations produced by doxorubicin. J Clin Invest. 1980;65:128–135. doi: 10.1172/JCI109642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Saari JT, Kang YJ. Weak antioxidant defenses make the heart a target for damage in copper-deficient rats. Free Radic Biol Med. 1994;17:529–536. doi: 10.1016/0891-5849(94)90092-2. [DOI] [PubMed] [Google Scholar]
- 9.Di Filippo C, Marfella R, Cuzzocrea S, Piegari E, Petronella P, Giugliano D, Rossi F, D'Amico M. Hyperglycemia in streptozotocin-induced diabetic rat increases infarct size associated with low levels of myocardial HO-1 during ischemia/reperfusion. Diabetes. 2005;54:803–810. doi: 10.2337/diabetes.54.3.803. [DOI] [PubMed] [Google Scholar]
- 10.Bruce CR, Carey AL, Hawley JA, Febbraio MA. Intramuscular heat shock protein 72 and heme oxygenase-1 mRNA are reduced in patients with type 2 diabetes: evidence that insulin resistance is associated with a disturbed antioxidant defense mechanism. Diabetes. 2003;52:2338–2345. doi: 10.2337/diabetes.52.9.2338. [DOI] [PubMed] [Google Scholar]
- 11.Liu X, Wei J, Peng DH, Layne MD, Yet SF. Absence of heme oxygenase-1 exacerbates myocardial ischemia/reperfusion injury in diabetic mice. Diabetes. 2005;54:778–784. doi: 10.2337/diabetes.54.3.778. [DOI] [PubMed] [Google Scholar]
- 12.Koh KK, Oh PC, Quon MJ. Does reversal of oxidative stress and inflammation provide vascular protection? Cardiovasc Res. 2009;81:649–659. doi: 10.1093/cvr/cvn354. [DOI] [PubMed] [Google Scholar]
- 13.Giannini C, Lombardo F, Curro F, Pomilio M, Bucciarelli T, Chiarelli F, Mohn A. Effects of high-dose vitamin E supplementation on oxidative stress and microalbuminuria in young adult patients with childhood onset type 1 diabetes mellitus. Diabetes Metab Res Rev. 2007;23:539–546. doi: 10.1002/dmrr.717. [DOI] [PubMed] [Google Scholar]
- 14.Ceriello A. New insights on oxidative stress and diabetic complications may lead to a "causal" antioxidant therapy. Diabetes Care. 2003;26:1589–1596. doi: 10.2337/diacare.26.5.1589. [DOI] [PubMed] [Google Scholar]
- 15.Cai L. Diabetic cardiomyopathy and its prevention by metallothionein: experimental evidence, possible mechanisms and clinical implications. Curr Med Chem. 2007;14:2193–2203. doi: 10.2174/092986707781389646. [DOI] [PubMed] [Google Scholar]
- 16.Cai L, Klein JB, Kang YJ. Metallothionein inhibits peroxynitrite-induced DNA and lipoprotein damage. J Biol Chem. 2000;275:38957–38960. doi: 10.1074/jbc.C000593200. [DOI] [PubMed] [Google Scholar]
- 17.Quesada AR, Byrnes RW, Krezoski SO, Petering DH. Direct reaction of H2O2 with sulfhydryl groups in HL-60 cells: zinc-metallothionein and other sites. Arch Biochem Biophys. 1996;334:241–250. doi: 10.1006/abbi.1996.0452. [DOI] [PubMed] [Google Scholar]
- 18.Thornalley PJ, Vasak M. Possible role for metallothionein in protection against radiation-induced oxidative stress. Kinetics and mechanism of its reaction with superoxide and hydroxyl radicals. Biochim Biophys Acta. 1985;827:36–44. doi: 10.1016/0167-4838(85)90098-6. [DOI] [PubMed] [Google Scholar]
- 19.Cai L, Wang J, Li Y, Sun X, Wang L, Zhou Z, Kang YJ. Inhibition of superoxide generation and associated nitrosative damage is involved in metallothionein prevention of diabetic cardiomyopathy. Diabetes. 2005;54:1829–1837. doi: 10.2337/diabetes.54.6.1829. [DOI] [PubMed] [Google Scholar]
- 20.Zhou G, Li X, Hein DW, Xiang X, Marshall JP, Prabhu SD, Cai L. Metallothionein suppresses angiotensin II-induced nicotinamide adenine dinucleotide phosphate oxidase activation, nitrosative stress, apoptosis, and pathological remodeling in the diabetic heart. J Am Coll Cardiol. 2008;52:655–666. doi: 10.1016/j.jacc.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Xu J, Wang G, Wang Y, Liu Q, Xu W, Tan Y, Cai L. Diabetes- and angiotensin II-induced cardiac endoplasmic reticulum stress and cell death: metallothionein protection. J Cell Mol Med. 2009;13(8A):1499–1512. doi: 10.1111/j.1582-4934.2009.00833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y, Feng W, Xue W, Tan Y, Hein DW, Li XK, Cai L. Inactivation of GSK-3beta by metallothionein prevents diabetes-related changes in cardiac energy metabolism, inflammation, nitrosative damage, and remodeling. Diabetes. 2009;58:1391–1402. doi: 10.2337/db08-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cai L. Suppression of nitrative damage by metallothionein in diabetic heart contributes to the prevention of cardiomyopathy. Free Radic Biol Med. 2006;41:851–861. doi: 10.1016/j.freeradbiomed.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Yang L, Li H, Yu T, Zhao H, Cherian MG, Cai L, Liu Y. Polymorphisms in metallothionein-1 and -2 genes associated with the risk of type 2 diabetes mellitus and its complications. Am J Physiol Endocrinol Metab. 2008;294:E987–E992. doi: 10.1152/ajpendo.90234.2008. [DOI] [PubMed] [Google Scholar]
- 25.Li J, Ichikawa T, Janicki JS, Cui T. Targeting the Nrf2 pathway against cardiovascular disease. Expert Opin Ther Targets. 2009;13:785–794. doi: 10.1517/14728220903025762. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen T, Nioi P, Pickett CB. The Nrf2-antioxidant response element signaling pathway and its activation by oxidative stress. J Biol Chem. 2009;284:13291–13295. doi: 10.1074/jbc.R900010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He X, Kan H, Cai L, Ma Q. Nrf2 is critical in defense against high glucose-induced oxidative damage in cardiomyocytes. J Mol Cell Cardiol. 2009;46:47–58. doi: 10.1016/j.yjmcc.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Tan Y, Ichikawa T, Li J, Si Q, Yang H, Chen X, Goldblatt CS, Meyer CJ, Li X, Cai L, Cui T. Diabetic downregulation of Nrf2 activity via ERK contributes to oxidative stress-induced insulin resistance in cardiac cells in vitro and in vivo. Diabetes. 2011;60:625–633. doi: 10.2337/db10-1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheng X, Chapple SJ, Patel B, Puszyk W, Sugden D, Yin X, Mayr M, Siow RC, Mann GE. Gestational diabetes mellitus impairs Nrf2-mediated adaptive antioxidant defenses and redox signaling in fetal endothelial cells in utero. Diabetes. 2013;62:4088–4097. doi: 10.2337/db13-0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Velmurugan GV, Sundaresan NR, Gupta MP, White C. Defective Nrf2-dependent redox signalling contributes to microvascular dysfunction in type 2 diabetes. Cardiovasc Res. 2013;100:143–150. doi: 10.1093/cvr/cvt125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yagishita Y, Fukutomi T, Sugawara A, Kawamura H, Takahashi T, Pi J, Uruno A, Yamamoto M. Nrf2 protects pancreatic β-cells from oxidative and nitrosative stress in diabetic model mice. Diabetes. 2014;63:605–618. doi: 10.2337/db13-0909. [DOI] [PubMed] [Google Scholar]
- 32.Uruno A, Furusawa Y, Yagishita Y, Fukutomi T, Muramatsu H, Negishi T, Sugawara A, Kensler TW, Yamamoto M. The Keap1-Nrf2 system prevents onset of diabetes mellitus. Mol Cell Biol. 2013;33:2996–3010. doi: 10.1128/MCB.00225-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu Z, Wei Y, Gong J, Cho H, Park JK, Sung ER, Huang H, Wu L, Eberhart C, Handa JT, Du Y, Kern TS, Thimmulappa R, Barber AJ, Biswal S, Duh EJ. NRF2 plays a protective role in diabetic retinopathy in mice. Diabetologia. 2014;57:204–213. doi: 10.1007/s00125-013-3093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhong Q, Mishra M, Kowluru RA. Transcription factor Nrf2-mediated antioxidant defense system in the development of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2013;54:3941–3948. doi: 10.1167/iovs.13-11598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miao X, Cui W, Sun W, Xin Y, Wang B, Tan Y, Cai L, Miao L, Fu Y, Su G, Wang Y. Therapeutic effect of MG132 on the aortic oxidative damage and inflammatory response in OVE26 type 1 diabetic mice. Oxid Med Cell Longev. 2013;2013:879516. doi: 10.1155/2013/879516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y, Sun W, Du B, Miao X, Bai Y, Xin Y, Tan Y, Cui W, Liu B, Cui T, Epstein PN, Fu Y, Cai L. Therapeutic effect of MG-132 on diabetic cardiomyopathy is associated with its suppression of proteasomal activities: roles of Nrf2 and NF-kappaB. Am J Physiol Heart Circ Physiol. 2013;304:H567–H578. doi: 10.1152/ajpheart.00650.2012. [DOI] [PubMed] [Google Scholar]
- 37.Zheng H, Whitman SA, Wu W, Wondrak GT, Wong PK, Fang D, Zhang DD. Therapeutic potential of Nrf2 activators in streptozotocin-induced diabetic nephropathy. Diabetes. 2011;60:3055–3066. doi: 10.2337/db11-0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cui W, Bai Y, Miao X, Luo P, Chen Q, Tan Y, Rane MJ, Miao L, Cai L. Prevention of diabetic nephropathy by sulforaphane: possible role of nrf2 upregulation and activation. Oxid Med Cell Longev. 2012;2012:821936. doi: 10.1155/2012/821936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miao X, Bai Y, Sun W, Cui W, Xin Y, Wang Y, Tan Y, Miao L, Fu Y, Su G, Cai L. Sulforaphane prevention of diabetes-induced aortic damage was associated with the up-regulation of Nrf2 and its downstream antioxidants. Nutr Metab (Lond) 2012;9:84. doi: 10.1186/1743-7075-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cui W, Li B, Bai Y, Miao X, Chen Q, Sun W, Tan Y, Luo P, Zhang C, Zheng S, Epstein PN, Miao L, Cai L. Potential role for Nrf2 activation in the therapeutic effect of MG132 on diabetic nephropathy in OVE26 diabetic mice. Am J Physiol Endocrinol Metab. 2013;304:E87–E99. doi: 10.1152/ajpendo.00430.2012. [DOI] [PubMed] [Google Scholar]
- 41.Miao X, Wang Y, Sun J, Sun W, Tan Y, Cai L, Zheng Y, Su G, Liu Q, Wang Y. Zinc protects against diabetes-induced pathogenic changes in the aorta: roles of metallothionein and nuclear factor (erythroid-derived 2)-like 2. Cardiovasc Diabetol. 2013;12:54. doi: 10.1186/1475-2840-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bai Y, Cui W, Xin Y, Miao X, Barati MT, Zhang C, Chen Q, Tan Y, Cui T, Zheng Y, Cai L. Prevention by sulforaphane of diabetic cardiomyopathy is associated with up-regulation of Nrf2 expression and transcription activation. J Mol Cell Cardiol. 2013;57:82–95. doi: 10.1016/j.yjmcc.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 43.Chin M, Lee CY, Chuang JC, Bumeister R, Wigley WC, Sonis ST, Ward KW, Meyer C. Bardoxolone methyl analogs RTA 405 and dh404 are well tolerated and exhibit efficacy in rodent models of type 2 diabetes and obesity. Am J Physiol Renal Physiol. 2013;304:F1438–F1446. doi: 10.1152/ajprenal.00387.2012. [DOI] [PubMed] [Google Scholar]
- 44.Wang Y, Zhang Z, Sun W, Tan Y, Liu Y, Zheng Y, Liu Q, Cai L, Sun J. Sulforaphane attenuation of type 2 diabetes-induced aortic damage was associated with the upregulation of Nrf2 expression and function. Oxid Med Cell Longev. 2014;2014:123963. doi: 10.1155/2014/123963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Negi G, Kumar A, Sharma SS. Nrf2 and NF-kappaB modulation by sulforaphane counteracts multiple manifestations of diabetic neuropathy in rats and high glucose-induced changes. Curr Neurovasc Res. 2011;8:294–304. doi: 10.2174/156720211798120972. [DOI] [PubMed] [Google Scholar]
- 46.Luo ZF, Qi W, Feng B, Mu J, Zeng W, Guo YH, Pang Q, Ye ZL, Liu L, Yuan FH. Prevention of diabetic nephropathy in rats through enhanced renal antioxidative capacity by inhibition of the proteasome. Life Sci. 2011;88:512–520. doi: 10.1016/j.lfs.2010.12.023. [DOI] [PubMed] [Google Scholar]
- 47.Shin S, Wakabayashi J, Yates MS, Wakabayashi N, Dolan PM, Aja S, Liby KT, Sporn MB, Yamamoto M, Kensler TW. Role of Nrf2 in prevention of high-fat diet-induced obesity by synthetic triterpenoid CDDO-imidazolide. Eur J Pharmacol. 2009;620:138–144. doi: 10.1016/j.ejphar.2009.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tan SM, Sharma A, Stefanovic N, Yuen DY, Karagiannis TC, Meyer C, Ward KW, Cooper ME, de Haan JB. A derivative of Bardoxolone methyl, dh404, in an inverse dose-dependent manner, lessens diabetes-associated atherosclerosis and improves diabetic kidney disease. Diabetes. 2014;63:3091–3103. doi: 10.2337/db13-1743. [DOI] [PubMed] [Google Scholar]
- 49.Liu Y, Wang Y, Miao X, Zhou S, Tan Y, Liang G, Zheng Y, Liu Q, Sun J, Cai L. Inhibition of JNK by compound C66 prevents pathological changes of the aorta in STZ-induced diabetes. J Cell Mol Med. 2014;18:1203–1212. doi: 10.1111/jcmm.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abo-Salem OM, Harisa GI, Ali TM, El-Sayed ES, Abou-Elnour FM. Curcumin ameliorates streptozotocin-induced heart injury in rats. J Biochem Mol Toxicol. 2014;28:263–270. doi: 10.1002/jbt.21562. [DOI] [PubMed] [Google Scholar]
- 51.Wang Y, Zhou S, Sun W, McClung K, Pan Y, Liang Q, Tan Y, Zhao Y, Liu Q, Sun J, Cai L. Inhibition of JNK by novel curcumin analog C66 prevents diabetic cardiomyopathy with a preservation of cardiac metallothionein expression. Am J Physiol Endocrinol Metab. 2014;306:E1239–E1247. doi: 10.1152/ajpendo.00629.2013. [DOI] [PubMed] [Google Scholar]
- 52.Castro CN, Barcala Tabarrozzi AE, Winnewisser J, Gimeno ML, Antunica Noguerol M, Liberman AC, Paz DA, Dewey RA, Perone MJ. Curcumin ameliorates autoimmune diabetes. Evidences in accelerated murine models of type 1 diabetes. Clin Exp Immunol. 2014;177:149–160. doi: 10.1111/cei.12322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chuengsamarn S, Rattanamongkolgul S, Phonrat B, Tungtrongchitr R, Jirawatnotai S. Reduction of atherogenic risk in patients with type 2 diabetes by curcuminoid extract: a randomized controlled trial. J Nutr Biochem. 2014;25:144–150. doi: 10.1016/j.jnutbio.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 54.Zhao WC, Zhang B, Liao MJ, Zhang WX, He WY, Wang HB, Yang CX. Curcumin ameliorated diabetic neuropathy partially by inhibition of NADPH oxidase mediating oxidative stress in the spinal cord. Neurosci Lett. 2014;560:81–85. doi: 10.1016/j.neulet.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 55.Thomas J, Garg ML, Smith DW. Dietary resveratrol supplementation normalizes gene expression in the hippocampus of streptozotocin-induced diabetic C57Bl/6 mice. J Nutr Biochem. 2014;25:313–318. doi: 10.1016/j.jnutbio.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 56.Sadi G, Bozan D, Yildiz HB. Redox regulation of antioxidant enzymes: post-translational modulation of catalase and glutathione peroxidase activity by resveratrol in diabetic rat liver. Mol Cell Biochem. 2014;393:111–122. doi: 10.1007/s11010-014-2051-1. [DOI] [PubMed] [Google Scholar]
- 57.Guo R, Liu B, Wang K, Zhou S, Li W, Xu Y. Resveratrol ameliorates diabetic vascular inflammation and macrophage infiltration in db/db mice by inhibiting the NF-kappaB pathway. Diab Vasc Dis Res. 2014;11:92–102. doi: 10.1177/1479164113520332. [DOI] [PubMed] [Google Scholar]
- 58.Bresciani L, Calani L, Bocchi L, Delucchi F, Savi M, Ray S, Brighenti F, Stilli D, Del Rio D. Bioaccumulation of resveratrol metabolites in myocardial tissue is dose-time dependent and related to cardiac hemodynamics in diabetic rats. Nutr Metab Cardiovasc Dis. 2014;24:408–415. doi: 10.1016/j.numecd.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 59.Bashmakov YK, Assaad-Khalil SH, Abou Seif M, Udumyan R, Megallaa M, Rohoma KH, Zeitoun M, Petyaev IM. Resveratrol promotes foot ulcer size reduction in type 2 diabetes patients. ISRN Endocrinol. 2014;2014:816307. doi: 10.1155/2014/816307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zheng X, Zhu S, Chang S, Cao Y, Dong J, Li J, Long R, Zhou Y. Protective effects of chronic resveratrol treatment on vascular inflammatory injury in steptozotocin-induced type 2 diabetic rats: role of NF-kappa B signaling. Eur J Pharmacol. 2013;720:147–157. [PubMed] [Google Scholar]
- 61.Pergola PE, Raskin P, Toto RD, Meyer CJ, Huff JW, Grossman EB, Krauth M, Ruiz S, Audhya P, Christ-Schmidt H, Wittes J, Warnock DG BEAM Study Investigators. Bardoxolone methyl and kidney function in CKD with type 2 diabetes. N Engl J Med. 2011;365:327–336. doi: 10.1056/NEJMoa1105351. [DOI] [PubMed] [Google Scholar]
- 62.de Zeeuw D, Akizawa T, Audhya P, Bakris GL, Chin M, Christ-Schmidt H, Goldsberry A, Houser M, Krauth M, Lambers Heerspink HJ, McMurray JJ, Meyer CJ, Parving HH, Remuzzi G, Toto RD, Vaziri ND, Wanner C, Wittes J, Wrolstad D, Chertow GM BEACON Trial Investigators. Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med. 2013;369:2492–2503. doi: 10.1056/NEJMoa1306033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang DD. Bardoxolone brings Nrf2-based therapies to light. Antioxid Redox Signal. 2013;19:517–518. doi: 10.1089/ars.2012.5118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Himmelfarb J, Tuttle KR. New therapies for diabetic kidney disease. N Engl J Med. 2013;369:2549–2550. doi: 10.1056/NEJMe1313104. [DOI] [PubMed] [Google Scholar]
- 65.Li B, Liu S, Miao L, Cai L. Prevention of diabetic complications by activation of Nrf2: diabetic cardiomyopathy and nephropathy. Exp Diabetes Res. 2012;2012:216512. doi: 10.1155/2012/216512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ding Y, Stidham RD, Bumeister R, Trevino I, Winters A, Sprouse M, Ding M, Ferguson DA, Meyer CJ, Wigley WC, Ma R. The synthetic triterpenoid, RTA 405, increases the glomerular filtration rate and reduces angiotensin II-induced contraction of glomerular mesangial cells. Kidney Int. 2013;83:845–854. doi: 10.1038/ki.2012.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hsu WH, Lee BH, Chang YY, Hsu YW, Pan TM. A novel natural Nrf2 activator with PPARgamma-agonist (monascin) attenuates the toxicity of methylglyoxal and hyperglycemia. Toxicol Appl Pharmacol. 2013;272:842–851. doi: 10.1016/j.taap.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 68.Xu J, Kulkarni SR, Donepudi AC, More VR, Slitt AL. Enhanced Nrf2 activity worsens insulin resistance, impairs lipid accumulation in adipose tissue, and increases hepatic steatosis in leptin-deficient mice. Diabetes. 2012;61:3208–3218. doi: 10.2337/db11-1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang YK, Wu KC, Liu J, Klaassen CD. Nrf2 deficiency improves glucose tolerance in mice fed a high-fat diet. Toxicol Appl Pharmacol. 2012;264:305–314. doi: 10.1016/j.taap.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rajasekaran NS, Varadharaj S, Khanderao GD, Davidson CJ, Kannan S, Firpo MA, Zweier JL, Benjamin IJ. Sustained activation of nuclear erythroid 2-related factor 2/antioxidant response element signaling promotes reductive stress in the human mutant protein aggregation cardiomyopathy in mice. Antioxid Redox Signal. 2011;14:957–971. doi: 10.1089/ars.2010.3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kannan S, Muthusamy VR, Whitehead KJ, Wang L, Gomes AV, Litwin SE, Kensler TW, Abel ED, Hoidal JR, Rajasekaran NS. Nrf2 deficiency prevents reductive stress-induced hypertrophic cardiomyopathy. Cardiovasc Res. 2013;100:63–73. doi: 10.1093/cvr/cvt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Willis MS, Townley-Tilson WH, Kang EY, Homeister JW, Patterson C. Sent to destroy: the ubiquitin proteasome system regulates cell signaling and protein quality control in cardiovascular development and disease. Circ Res. 2010;106:463–478. doi: 10.1161/CIRCRESAHA.109.208801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marchan R, Bolt HM. The cytoprotective and the dark side of Nrf2. Arch Toxicol. 2013;87:2047–2050. doi: 10.1007/s00204-013-1165-7. [DOI] [PubMed] [Google Scholar]
- 74.Grossman R, Ram Z. The dark side of Nrf2. World Neurosurg. 2013;80:284–286. doi: 10.1016/j.wneu.2011.09.055. [DOI] [PubMed] [Google Scholar]