Abstract
Advances in our understanding of the pathology, radiology and clinical behaviour of peripheral lung adenocarcinomas facilitated a more robust terminology and classification of these lesions. The International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) classification introduced new terminology to better reflect this heterogeneous group of adenocarcinomas formerly known as bronchoalveolar cell carcinoma (BAC). There is now a clear distinction between pre-invasive, minimally invasive and frankly invasive lesions. The radiographic appearance of these ranges from pure ground glass nodules to solid mass lesions. Radiologists must be aware of the new classification in order to work alongside multidisciplinary colleagues to allow accurate staging and treatment. This article reviews the new classification of lung adenocarcinomas. Management options of these lesions with particular focus on radiological implications of the new classification will be reviewed.
Keywords: Adenocarcinoma, bronchiolo-alveolar, non-small cell lung cancer, computed tomography (CT), multiple pulmonary nodules, solitary pulmonary nodules
Lung cancer is the second most common cancer and accounts for 14% of new cancers (1). It is the leading cause of cancer deaths in the United Kingdom, the most frequent cause of major cancer incidence and mortality in men, and the second most common cause of cancer mortality in women (2,3). In 2010, over 42,000 people were diagnosed with lung cancer and there were nearly 35,000 deaths (4). Non-small cell lung cancers account for around 85% of cases (1) and of these adenocarcinomas are most common (5,6). The prevalence of adenocarcinoma is increasing (7) and it presents frequently in asymptomatic females, especially those from East Asia, and often in non-smokers.
The radiological appearance of peripheral lung adenocarcinomas encompasses a spectrum from ground glass nodules (GGNs) to solid mass lesions on computed tomography (CT), reflecting their heterogeneous histological subtypes. This spectrum was previously referred to using the single term bronchoalveolar cell carcinoma (BAC) which frequently caused confusion (8). It became clear that a more robust classification was required and with advances in understanding of the oncology, molecular biology, pathology, radiology and surgery of lung adenocarcinoma this became possible.
The International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) international multidisciplinary classification of lung adenocarcinoma (6) introduces new terminology and diagnostic criteria. Multidisciplinary management pathways have been improved to reflect our increased understanding of this disease (6,9) and subsequently guidelines for the radiological management of subsolid nodules have been introduced (10). The new classification also highlights the importance of consistency of scanning and sampling techniques.
Radiologists must be aware of the new classification and guidelines for the management of GGNs as they will play an important role in differentiating invasive from pre-invasive lesions. These lesions are likely to be picked up with increasing frequency in lung cancer screening studies. This article describes the terminology used in the new classification and discusses associated prognostic implications. Radiographic appearances of the lung adenocarcinoma spectrum will be reviewed with pathologic correlation, and management options discussed.
The revised lung adenocarcinoma (IASLC/ATS/ERS) classification
One of the strongest recommendations of the new classification is to discontinue use of the term BAC. Previously this term was applied to tumours with a pure bronchioloalveolar growth pattern characterised by lepidic growth—growth of neoplastic cells along pre-existing structures and alveolar septa without invasion of the stoma, pleura or vessels (11). Lepidic growth manifests radiologically as ground glass opacification (6) hence the importance of the GGN.
Work by Noguchi et al. in the 1990s demonstrated that patients with GGNs had a better prognosis than those with solid nodules (12). This was reflected in the 1999 (13) and 2004 (14) WHO classifications of lung cancer. The evolution of GGNs (typically lepidic growth) to more solid (and so more likely invasive) nodules was well documented prior to the revised classification (15). Data from lung cancer screening literature shows a higher rate of malignancy in incidental part-solid nodules compared to incidental solid nodules (16) and the majority of persistent GGNs represent adenocarcinoma spectrum lesions (17,18).
The previous classification of BAC included a heterogenous spectrum of subtypes including mucinous, non-mucinous and mixed. This frequently caused confusion due to their varied radiological appearance (19). The term was applied to invasive and non-invasive adenocarcinomas with varying prognoses ranging from 100% 5 years survival following resection of non-invasive lesions (20) to less than 10% 3 years survival for some invasive adenocarcinomas (21).
The revised classification better reflects the pathologic, radiologic and clinical correlation of lung adenocarcinoma. What was previously classified as BAC is now categorized into the following terms—adenocarcinoma in situ (AIS), minimally invasive adenocarcinoma (MIA), lepidic predominant adenocarcinoma (LPA), predominantly invasive adenocarcinoma with some nonmucinous lepidic component and invasive mucinous adenocarcinoma. Table 1 demonstrates the revised classification, which more clearly follows the multistep progression that many lung adenocarcinoma spectrum lesions are thought to take (22). This allows better differentiation between pre-invasive, minimally invasive and frankly invasive lesions. Figure 1 demonstrates the definitions of nodules as used in the new classification.
Table 1. The revised classification of lung adenocarcinoma (6).
| (I) Preinvasive lesions |
| (i) Adenocarcinoma in situ (AIS) —mucinous, nonmucinous, or mixed |
| (ii) Atypical adenomatous hyperplasia (AAH) |
| (II) Minimally invasive lesions |
| (i) Minimally invasive adenocarcinomas (MIA) —mucinous, nonmucinous, or mixed |
| (III) Invasive adenocarcinoma |
| (i) Acinar predominant |
| (ii) Papillary predominant |
| (iii) Micropapillary predominant |
| (iv) Solid predominant with mucin production |
| (v) Lepidic predominant adenocarcinoma (LPA) |
| (IV) Variants of invasive adenocarcinoma |
| (i) Invasive mucinous adenocarcinoma |
| (ii) Colloid, fetal, and enteric |
IASLC/ATS/ERS classification of lung adenocarcinoma in resection specimens; IASLC/ATS/ERS, the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society.
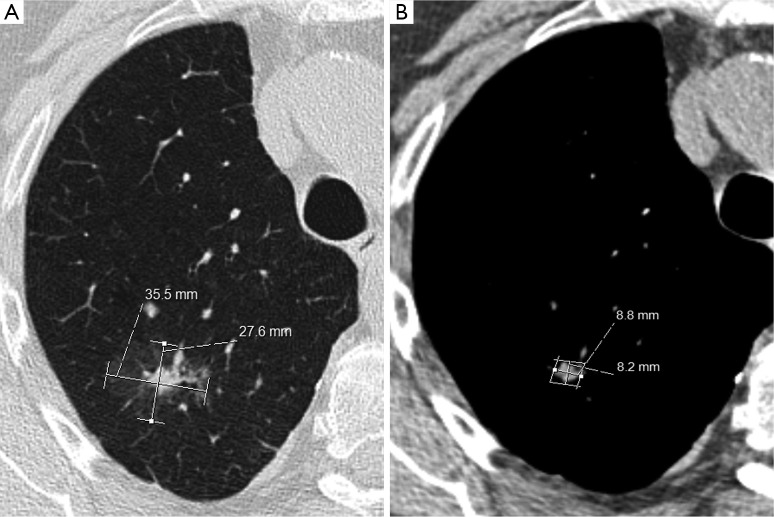
Figure 1.
Definition of nodules used in the classification of lung adenocarcinoma—based on the Fleishner Society glossary of terms (10).
There is good inter-observer agreement between pathologists using the new classification (23) though few studies have investigated agreement between radiologists. The new classification better reflects the varying prognoses associated with these lesions. Radiologists must be able to distinguish invasive mucinous adenocarcinoma from non-mucinous predominant pre-invasive adenocarcinoma spectrum lesions as this impacts on treatment algorithms including surgical intervention, follow up planning and prognosis prediction (24).
Radiographic appearances of the new classification
Pre-invasive lesions
Atypical adenomatous hyperplasia (AAH)
AAH is the earliest detectable pre-invasive lesion and is equivalent to the term squamous dysplasia. Its histologic and radiologic features predate the new classification and so are well validated. AAH manifests as a small GGN typically less than 5 mm in size with no solid or part-solid component (19). Bronchial and vascular margins are preserved and AAH is less opaque than AIS. Histologically there is proliferation of mild to moderately atypical cuboidal to columnar epithelial cells along alveoli and respiratory bronchioles, with no invasion. Adenocarcinoma spectrum lesions are often multifocal and AAH is often found adjacent to resected invasive adenocarcinomas. Figure 2 demonstrates one such case of pure ground glass nodules typical of AAH. There is a continuum of morphologic changes between AAH and AIS and histopathologists are adjusting to the new classification and its application (23,25).
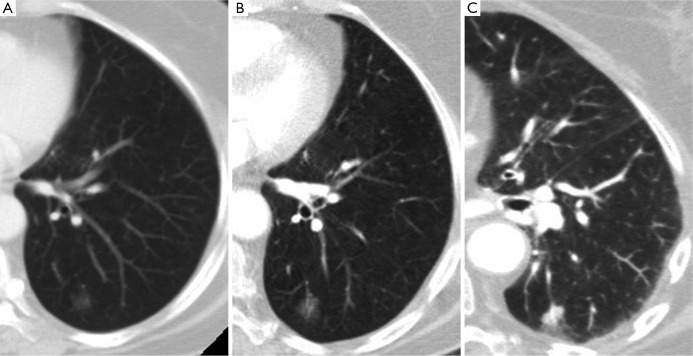
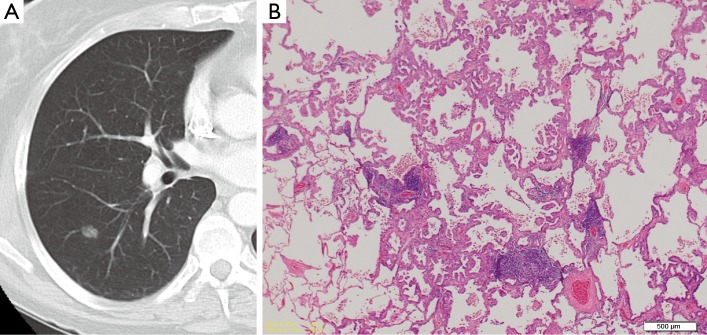
Figure 2.
(A) A persistent pure ground glass nodule (GGN) characteristic of atypical adenomatous hyperplasia (AAH); (B) a GGN which was superior to an invasive adenocarcinoma; (C) histologic specimen, hematoxylin and eosin (H and E) stain of the GGN demonstrating a 0.6 mm focus of atypical cuboidal to columnar epithelial cells along alveolar spaces.
Adenocarcinoma in situ (AIS)
AIS refers to purely lepidic growth without stromal, vascular or pleural invasion. It is equivalent to carcinoma in situ. Like AAH it is a pre-invasive tumour but is typically larger. Most measure between 5 and 20 mm but AIS can be as large as 3 cm. Although still a GGN, AIS is typically of greater attenuation than AAH. Figure 3 demonstrates a GGN of higher attenuation than that characteristic of AAH and its pathologic correlate.
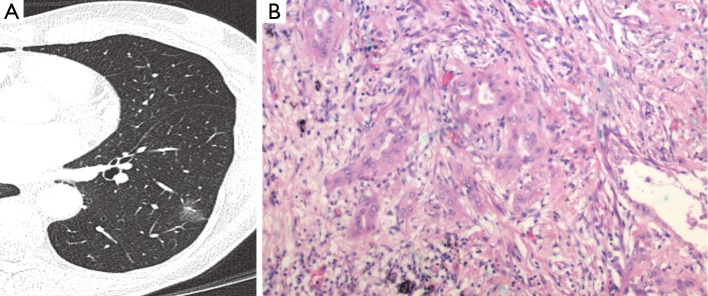
Figure 3.
(A) A persistent pure ground glass nodule (GGN) characteristic of adenocarcinoma in situ (AIS); (B) histologic specimen, H&E stain demonstrating lepidic growth pattern of atypical columnar cells with lack of invasion.
Invasive lesions
Minimally invasive adenocarcinoma (MIA)
MIA describes a solitary adenocarcinoma 3 cm or less in size. Again this is a LPA but unlike the pre-invasive lesions is characterized by a small invasive component of tumour cells infiltrating myofibroblastic stroma. Most MIA are non-mucinous. The actual size of the invasive component at histology is likely to measure no greater than 5 mm (26). This requires validation on CT as a variety of other associated components of small adenocarcinomas including collapse, fibrosis and mucous can also cause a solid appearance. Thus on CT the solid component may be larger (27). MIA is excluded if there is any invasion to lymphatics, pleura, blood vessels or tumour necrosis. Radiologically MIA manifests as a part-solid nodule in contrast to the GGNs of pre-invasive adenocarcinomas, the solid component representing the focus of invasion. Figure 4 demonstrates a part-solid nodule which proved to be MIA. Mucinous and non-mucinous MIA can present and solid and part-solid nodules.
Figure 4.
(A) A part-solid nodule with a small central component measuring less than 5 mm characteristic of minimally invasive adenocarcinoma (MIA); (B) histologic specimen, H&E stain of MIA demonstrating desmoplastic stroma around invasive mucinous acini.
Importantly MIA, as well as AIS, can be considered for sublobar resection (28). Differences between MIA and mucinous AIS are a greater size, an extent of invasion of greater than 5 mm, multiple nodules, and the spread of the nodule into adjacent lung parenchyma with an indistinct border (29).
Invasive adenocarcinoma
Invasive adenocarcinoma is present when there is at least one invasive tumour focus measuring more than 5 mm in its greatest dimension (6). They represent over 70% of resected adenocarcinomas and consist of a heterogenous and complex mixture of histologic subtypes. Although previously referred to as adenocarcinoma of mixed subtype they are now classified according to their predominant histologic component principally acinar, papillary, micropapillary, solid and lepidic. Invasive adenocarcinomas are predominantly mucinous compared to the predominant non-mucinous pre-invasive lesions. Mucinous BAC has been reclassified as an invasive mucinous adenocarcinoma an example of which is shown in Figure 5. These are differentiated from non-mucinous tumours by the mucinous cells, which consist of columnar cells, abundant apical mucin and small basally orientated nuclei.
Figure 5.
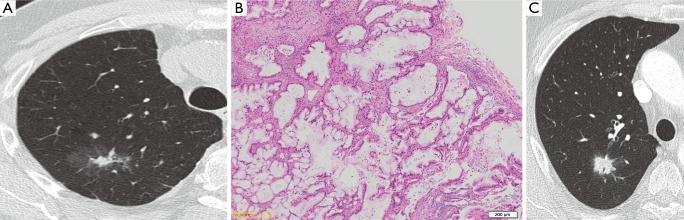
(A) A part-solid nodule with a spiculate central solid component measuring over 1 cm consistent with invasive adenocarcinoma; (B) histologic specimen following resection, H&E stain, demonstrating an invasive mucinous adenocarcinoma; (C) a further example of an invasive adenocarcinoma which in this case was a more solid spiculate nodule with internal air bronchograms.
Invasive adenocarcinomas are typically solid or mostly solid on CT, frequently display air bronchograms, have a lobar or multilobar distribution and most often consist of nodular or consolidative opacities (30,31). When multifocal these were previously called multicentric BAC, a term now discontinued.
Lepidic predominant adenocarcinoma (LPA) describes an invasive adenocarcinoma with predominant lepidic growth pattern. Unlike MIA it consists of at least one focus of invasion into vessels, pleura or lymphatics, or is necrotic. LPA is applied to purely non-mucinous adenocarcinomas; any mucinous component would make it an invasive adenocarcinoma.
CT evaluation and measurement of part-solid nodules
Accurate assessment of part-solid nodules requires thin slice CT using slice thickness of less than 3 mm and ideally 1-1.5 mm (32,33). This allows accurate detection of subtle changes in ground glass attenuation and differentiation between ground glass and solid components as well as subtle changes in the size and solid component of the nodule (34).
The size of the invasive component, corresponding to the solid component of a nodule versus the ground glass lepidic component, correlates with prognosis. The radiologist should document the total size of any subsolid nodule as well as the size of any solid component due to the implications upon prognosis and treatment options of the solid component. The solid component should be measured on mediastinal windows to aid consistency (35) as demonstrated in Figure 6. With further validation studies it is likely that the T staging in future TNM classifications will relate not to the total size of a subsolid nodule but to the size of the solid component due to prognostic implications of an invasive component.
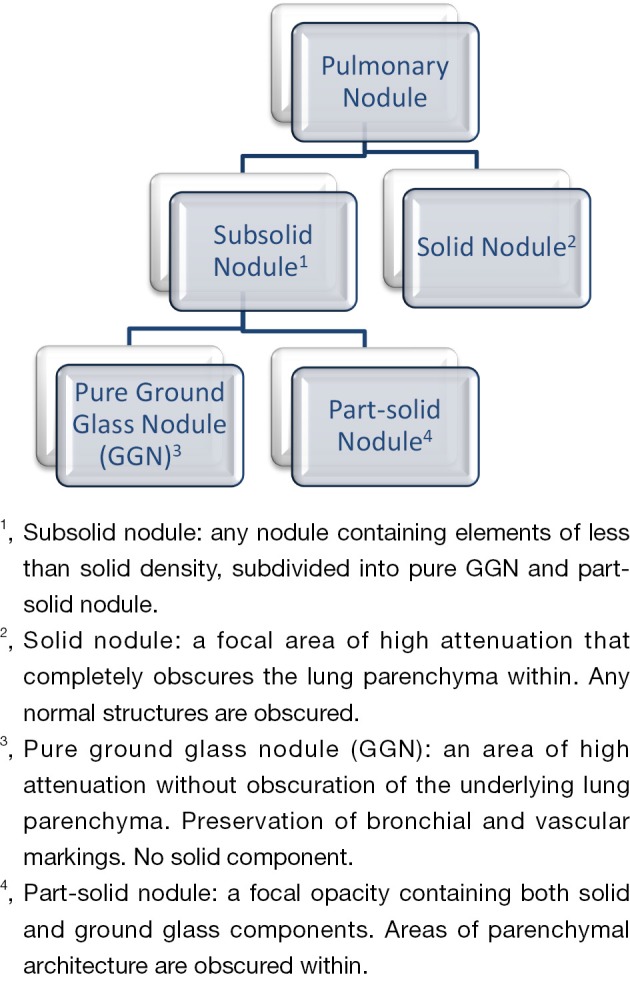
Figure 6.
Measurement of a part-solid nodule using mediastinal windows to measure the size of the solid component.
The margin of GGNs is less distinct than that of solid lesions, which can impede accurate and consistent measurement. Using commercial software can reduce variations in the volume and attenuation measurements (36) but currently there is no consensus on the optimum evaluation of subsolid nodules. Techniques such as histogram evaluation of attenuation (37) require validation. Current best practice is to use thin-slice CT, measure the solid component on mediastinal windows and also give the total size of the nodule including the ground glass component.
Radiological management of adenocarcinoma spectrum lesions
The differential diagnosis of subsolid nodules ranges from infection and focal interstitial fibrosis to malignant lung adenocarcinoma (38). Because the majority of GGNs will resolve the initial management of any GGN or subsolid nodule is a repeat scan. A persistent GGN is of greater malignant potential than an equivalent persistent solid nodule (17,18) and the differential diagnosis of a persistent GGN includes AAH, adenocarcinoma spectrum, lymphoproliferative disorder and also organizing pneumonia/fibrosis (36).
Certain characteristics of a subsolid nodule can help determine the likelihood of invasion (29) and the radiologist should be alert to the implications of these findings. The presence of air bronchograms, spiculate margins or pleural retraction suggest increased likelihood of invasion (39) as does a concave notch in the solid component or lobular border (40,41). In contrast, spherical pure GGNS are more likely to be preinvasive.
The size of a GGN correlates with invasive potential. A size of less than 10 mm is a highly specific discriminator of a preinvasive lesion over an invasive adenocarcinoma (41). A separate study identified that a size of greater than 8 mm is an independent predictor of malignancy (26). Any increase in the attenuation of a nodule on follow up should also be considered significant, even if the size has remained stable (42). As size or attenuation increase so too does the risk of malignancy (16).
The Fleischner Society has introduced recommendations for the management of subsolid pulmonary nodules detected at CT (35). Despite a lack of strong evidence the guidelines are based on expert consensus and extensive literature searching and are the current gold-standard in the management of subsolid nodules. The guidance is essential reading for any radiologist involved in the follow up of these nodules and are summarized below and in Table 2.
Table 2. Summary of the Fleischner Society guidelines for the management of subsolid pulmonary nodules (10).
| Nodule type | Recommendation |
|---|---|
| Solitary pure GGN <5 mm (assessed with contiguous CT sections of <1 mm) | |
| ≤5 mm | No follow up |
| >5 mm | Follow up with CT at 3 months, and then yearly monitoring for a minimum of 3 years if persistant and unchanged. (FDG-PET is of limited value and therefore not recommended) |
| Subsolid GGNs | Follow up with CT at 3 months to confirm persistence |
| <5 mm | If persistent and solid measuring <5 mm, then yearly CT monitoring for a minimum of 3 years |
| ≥5 mm | If persistent and solid measuring ≥5 mm, then biopsy or surgical resection should be considered. If subsolid nodules measure >10 mm FDG PET should be considered for further evaluation |
| Multiple subsolid nodules | Follow up with CT at 3 months to confirm persistence |
| Pure GGNs ≤5 mm | Follow up CT at 2 and 4 years to monitor. If persistent and solid measuring <5 mm, then yearly CT monitoring for a minimum of 3 years |
| Pure GGNs >5 mm with no dominant lesion | If persistent biopsy or surgical resection should be considered, especially if lesion has a >5 mm solid component |
| Dominant nodule with subsolid or solid component |
GGN, ground glass nodule; CT, computed tomography.
Solitary GGNs that measure less than 5 mm do not require any further follow-up. It is unknown exactly how frequently these would progress to invasive adenocarcinomas, their small size precludes any meaningful interval assessment given a doubling time likely to be many years, and such follow up would have financial implications and expose patients to increased radiation.
Pure GGNs greater than 5 mm require an interval scan to determine persistence and subsequently annual surveillance for at least 3 years with contiguous thin slice CT if they remain unchanged. Figure 7 demonstrates a GGN that increased in size and attenuation over a period of 7 years. Although these lesions can be benign in up to 20% (43), without a truly accurate method to assess malignant potential other than surgical resection and because of the greater likelihood of these representing AAH/AIS/MIA they require surveillance to detect signs of evolving malignancy as described including increased size, attenuation or solid component.
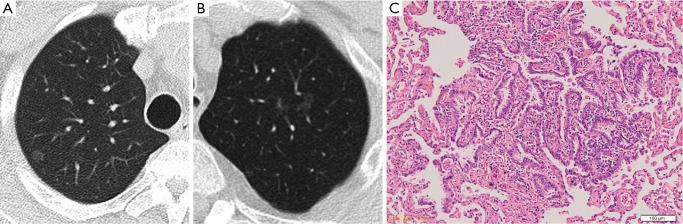
Figure 7.
(A) A pure GGN in a patient with previously resected invasive adenocarcinoma; (B) the patient was lost to follow up and presented 5 years later at which point the nodule was of slightly higher attenuation; (C) 1 year later there is a clear solid component highly suggestive of progression to invasive adenocarcinoma. GGN, ground glass nodule.
In contrast to pure GGNs, subsolid nodules, particularly those with a solid component greater than 5 mm are considered malignant until lack of growth is demonstrated at interval CT in 3 months. The greater the size of the solid component the more likely it is amenable to accurate CT biopsy and assessment with PET particularly once measuring 8-10 mm. CT guided biopsy of GGNs using co-axial biopsy technique, has been shown to have a diagnostic accuracy of 93% (17).
Multifocal persistent ground glass nodules often represent either primary lung cancers or lung metastases. AAH and pre-invasive adenocarcinomas are more frequently seen in multiple ground glass nodules (44). The Fleischner Society also gives recommendations for the management of multiple GGNs and subsolid nodules. For multiple GGNs of less than 5 mm a conservative approach with surveillance CT at 2 and 4 years is advocated. For multiple nodules greater than 5 mm without a dominant nodule initial CT at 3 months followed by annual CT is advocated. The guidelines introduce the concept of a dominant nodule which if present mandates a more aggressive approach particularly in the presence of a solid component >5 mm.
Summary
The revised classification of lung adenocarcinoma has introduced new terminology to better reflect the multistep progression of lung adenocarcinoma. There is now differentiation between pre-invasive and invasive lesions. This more robust classification replaces the term BAC more accurately reflecting the correlation between radiology, pathology and prognosis. Radiologists play an important role in distinguishing pre-invasive from invasive lesions and must be familiar with the new Fleischner Society recommendations regarding the management of subsolid pulmonary nodules. The classification heralds an exciting era in lung adenocarcinoma. It is likely that suggested changes for nodule measurement and determination of T stage will be reflected in future TNM and WHO classifications.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.American cancer society. Cancer facts and figures July 2013. Available online: http://www.cancer.org/cancer/lungcancer-non-smallcell/detailedguide/non-small-cell-lung-cancer-key-statistics
- 2.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300. [DOI] [PubMed] [Google Scholar]
- 4.Cancer research society. Available online: http://www.cancerresearchuk.org
- 5.Garfield DH, Cadranel JL, Wislez M, et al. The bronchioloalveolar carcinoma and peripheral adenocarcinoma spectrum of diseases. J Thorac Oncol 2006;1:344-59. [PubMed] [Google Scholar]
- 6.Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers--a different disease. Nat Rev Cancer 2007;7:778-90. [DOI] [PubMed] [Google Scholar]
- 8.Garfield DH, Cadranel J, West HL. Bronchioloalveolar carcinoma: the case for two diseases. Clin Lung Cancer 2008;9:24-9. [DOI] [PubMed] [Google Scholar]
- 9.Lee SM, Goo JM, Park CM, et al. A new classification of adenocarcinoma: what the radiologists need to know. Diagn Interv Radiol 2012;18:519-26. [DOI] [PubMed] [Google Scholar]
- 10.Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013;266:304-17. [DOI] [PubMed] [Google Scholar]
- 11.Christiani DC, Pao W, DeMartini JC, et al. BAC consensus conference, November 4-6, 2004: epidemiology, pathogenesis, and preclinical models. J Thorac Oncol 2006;1:S2-7. [PubMed] [Google Scholar]
- 12.Noguchi M, Morikawa A, Kawasaki M, et al. Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer 1995. Jun;75:2844-52. [DOI] [PubMed] [Google Scholar]
- 13.Travis WD, Colby TV, Corrin B, et al. World Heatlh Organisation International Histological Classification of Tumours. Histological Typing of Lung and Pleural Tumours. 3rd edition. Berlin, Germany: Springer-Verlag, 1999. [Google Scholar]
- 14.Travis W, Brambilla E, Muller-Hermelink HK, et al. eds. Pathology and Genetics. Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC press, 2004. [Google Scholar]
- 15.Lee HY, Lee KS, Han J, et al. Mucinous versus nonmucinous solitary pulmonary nodular bronchioloalveolar carcinoma: CT and FDG PET findings and pathologic comparisons. Lung Cancer 2009;65:170-5. [DOI] [PubMed] [Google Scholar]
- 16.Henschke CI, Yankelevitz DF, Mirtcheva R, et al. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 2002;178:1053-7. [DOI] [PubMed] [Google Scholar]
- 17.Lu CH, Hsiao CH, Chang YC, et al. Percutaneous computed tomography-guided coaxial core biopsy for small pulmonary lesions with ground-glass attenuation. J Thorac Oncol 2012;7:143-50. [DOI] [PubMed] [Google Scholar]
- 18.Kim HY, Shim YM, Lee KS, et al. Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 2007;245:267-75. [DOI] [PubMed] [Google Scholar]
- 19.Trigaux JP, Gevenois PA, Goncette L, et al. Bronchioloalveolar carcinoma: computed tomography findings. Eur Respir J 1996;9:11-6. [DOI] [PubMed] [Google Scholar]
- 20.Maeshima AM, Tochigi N, Yoshida A, et al. Histological scoring for small lung adenocarcinomas 2 cm or less in diameter: a reliable prognostic indicator. J Thorac Oncol 2010;5:333-9. [DOI] [PubMed] [Google Scholar]
- 21.Travis WD, Garg K, Franklin WA, et al. Evolving concepts in the pathology and computed tomography imaging of lung adenocarcinoma and bronchioloalveolar carcinoma. J Clin Oncol 2005;23:3279-87. [DOI] [PubMed] [Google Scholar]
- 22.Yatabe Y, Borczuk AC, Powell CA. Do all lung adenocarcinomas follow a stepwise progression? Lung Cancer 2011;74:7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thunnissen E, Beasley MB, Borczuk AC, et al. Reproducibility of histopathological subtypes and invasion in pulmonary adenocarcinoma. An international interobserver study. Mod Pathol 2012;25:1574-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol 2005;40:90-7. [DOI] [PubMed] [Google Scholar]
- 25.Warth A, Stenzinger A, von Brünneck AC, et al. Interobserver variability in the application of the novel IASLC/ATS/ERS classification for pulmonary adenocarcinomas. Eur Respir J 2012;40:1221-7. [DOI] [PubMed] [Google Scholar]
- 26.Borczuk AC, Qian F, Kazeros A, et al. Invasive size is an independent predictor of survival in pulmonary adenocarcinoma. Am J Surg Pathol 2009;33:462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saito H, Kameda Y, Masui K, et al. Correlations between thin-section CT findings, histopathological and clinical findings of small pulmonary adenocarcinomas. Lung Cancer 2011;71:137-43. [DOI] [PubMed] [Google Scholar]
- 28.El-Sherif A, Gooding WE, Santos R, et al. Outcomes of sublobar resection versus lobectomy for stage I non-small cell lung cancer: a 13-year analysis. Ann Thorac Surg 2006;82:408-15; discussion 415-6. [DOI] [PubMed] [Google Scholar]
- 29.Kim HY, Shim YM, Lee KS, et al. Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 2007;245:267-75. [DOI] [PubMed] [Google Scholar]
- 30.Lee HY, Lee KS, Han J, et al. Mucinous versus nonmucinous solitary pulmonary nodular bronchioloalveolar carcinoma: CT and FDG PET findings and pathologic comparisons. Lung Cancer 2009;65:170-5. [DOI] [PubMed] [Google Scholar]
- 31.Gaeta M, Vinci S, Minutoli F, et al. CT and MRI findings of mucin-containing tumors and pseudotumors of the thorax: pictorial review. Eur Radiol 2002;12:181-9. [DOI] [PubMed] [Google Scholar]
- 32.Lee HY, Goo JM, Lee HJ, et al. Usefulness of concurrent reading using thin-section and thick-section CT images in subcentimetre solitary pulmonary nodules. Clin Radiol 2009;64:127-32. [DOI] [PubMed] [Google Scholar]
- 33.Aoki T, Hanamiya M, Uramoto H, et al. Adenocarcinomas with predominant ground-glass opacity: correlation of morphology and molecular biomarkers. Radiology 2012;264:590-6. [DOI] [PubMed] [Google Scholar]
- 34.Hansell DM, Bankier AA, MacMahon H, et al. Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008;246:697-722. [DOI] [PubMed] [Google Scholar]
- 35.Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013;266:304-17. [DOI] [PubMed] [Google Scholar]
- 36.Park CM, Goo JM, Lee HJ, et al. Persistent pure ground-glass nodules in the lung: interscan variability of semiautomated volume and attenuation measurements. AJR Am J Roentgenol 2010;195:W408-14. [DOI] [PubMed] [Google Scholar]
- 37.Ikeda K, Awai K, Mori T, et al. Differential diagnosis of ground-glass opacity nodules: CT number analysis by three-dimensional computerized quantification. Chest 2007;132:984-90. [DOI] [PubMed] [Google Scholar]
- 38.Park CM, Goo JM, Lee HJ, et al. Focal interstitial fibrosis manifesting as nodular ground-glass opacity: thin-section CT findings. Eur Radiol 2007;17:2325-31. [DOI] [PubMed] [Google Scholar]
- 39.Lee SM, Park CM, Goo JM, et al. Transient part-solid nodules detected at screening thin-section CT for lung cancer: comparison with persistent part-solid nodules. Radiology 2010;255:242-51. [DOI] [PubMed] [Google Scholar]
- 40.Lim HJ, Ahn S, Lee KS, et al. Persistent pure ground-glass opacity lung nodules ≥10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 2013;144:1291-9. [DOI] [PubMed] [Google Scholar]
- 41.Lee SM, Park CM, Goo JM, et al. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology 2013;268:265-73. [DOI] [PubMed] [Google Scholar]
- 42.Lee HJ, Goo JM, Lee CH, et al. Predictive CT findings of malignancy in ground-glass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol 2009;19:552-60. [DOI] [PubMed] [Google Scholar]
- 43.Oda S, Awai K, Murao K, et al. Computer-aided volumetry of pulmonary nodules exhibiting ground-glass opacity at MDCT. AJR Am J Roentgenol 2010;194:398-406. [DOI] [PubMed] [Google Scholar]
- 44.Kim TJ, Goo JM, Lee KW, et al. Clinical, pathological and thin-section CT features of persistent multiple ground-glass opacity nodules: comparison with solitary ground-glass opacity nodule. Lung Cancer 2009;64:171-8. [DOI] [PubMed] [Google Scholar]