Abstract
Mental disorders traditionally have been viewed as distinct, episodic, and categorical conditions. This view has been challenged by evidence that many disorders are sequentially comorbid, recurrent/chronic, and exist on a continuum. Using the Dunedin Multidisciplinary Health and Development Study, we examined the structure of psychopathology, taking into account dimensionality, persistence, co-occurrence, and sequential comorbidity of mental disorders across 20 years, from adolescence to midlife. Psychiatric disorders were initially explained by three higher-order factors (Internalizing, Externalizing, and Thought Disorder) but explained even better with one General Psychopathology dimension. We have called this dimension the p factor because it conceptually parallels a familiar dimension in psychological science: the g factor of general intelligence. Higher p scores are associated with more life impairment, greater familiality, worse developmental histories, and more compromised early-life brain function. The p factor explains why it is challenging to find causes, consequences, biomarkers, and treatments with specificity to individual mental disorders. Transdiagnostic approaches may improve research.
Keywords: psychiatric epidemiology, developmental psychopathology, DSM
A psychiatric nosology—the classification of mental disorders—is a practical tool. A nosology is useful for research because it is used to integrate and guide empirical studies. A nosology is useful for health-care delivery because it is used to make prognoses and to decide on treatment need and choice of treatment. The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) is the current ascendant nosology in clinical psychology and psychiatry. It may not be perfect (Sanislow et al., 2010), but it is what many of us work with in both research and clinical practice (Kupfer, Kuhl, & Regier, 2013).
A persistent challenge to the DSM and related nosologies is comorbidity, the coexistence of two or more conditions or disorders (Hasin & Kilcoyne, 2012; Kessler, Chiu, Demler, Merikangas, & Walters, 2005) Comorbidity rates are very high in psychiatry and conform roughly to the rule of 50%: Half of individuals who meet diagnostic criteria for one disorder meet diagnostic criteria for a second disorder at the same time, half of individuals with two disorders meet criteria for a third disorder, and so forth (Newman, Moffitt, Caspi, & Silva, 1998). The high rates of comorbidity observed among mental disorders suggest that there may be a more parsimonious structure to psychopathology than implied by current nosologies that identify many separate and distinct disorders. This article begins by providing a brief historical review of empirical research on the structure of psychiatric disorders. It then offers an empirical update, suggesting that most common psychiatric disorders are unified by a single psychopathology dimension representing lesser-to-greater severity of psychopathology that is associated with compromised brain integrity.
Soon after the publication of the DSM-IV (American Psychiatric Association, 1994), psychological scientists noted the need for research that would examine patterns of comorbidity to “elucidate the broad, higher-order structure of phenotypic psychopathology” (Clark, Watson. & Reynolds, 1995, p. 131) We responded to this call by using confirmatory factor analysis (CFA) to evaluate alternative hypotheses about the latent structure underlying 10 common mental disorders among young adults, ages 18 to 21 years (Krueger, Caspi, Moffitt, & Silva, 1998). In contrast to the prominence of categorical models in the classification of adult psychopathologies, dimensional models had long enjoyed success in research on the classification of childhood psychopathologies, and empirical studies had converged on two primary dimensions as a way to characterize childhood disorders: Internalizing (including anxious and depression symptoms) and Externalizing (including aggressive, delinquent, and hyperactive-impulsive symptoms; Achenbach & Edelbrock, 1981). We could see no reason why this highly replicable two-dimensional structure of psychopathologies should suddenly vanish when research participants and patients suddenly turned age 18 years. Our data confirmed that a two-factor model accounted for the comorbidity of different young-adult disorders, and it bore a striking similarity to the model of childhood psychopathologies.
On the basis of this initial finding, we put forth the hypothesis that common DSM psychiatric disorders in adulthood may be characterized by two underlying core psychopathological processes: an Internalizing dimension indicating liability to experience mood and anxiety disorders, such as major depression (MDE), generalized anxiety disorder (GAD), panic disorder, and social phobia; and an Externalizing dimension indicating liability to experience substance disorders and antisocial disorders. During the past 15 years, multiple studies in different parts of the world, in different age-groups, in general community samples, and in clinical populations (e.g., Forbush & Watson, 2013; Kendler, Prescott, Myers, & Neale, 2003; Krueger, 1999; Slade & Watson, 2006; Vollebergh et al., 2001) have replicated this basic finding (Krueger & Markon, 2006, 2011).
With the publication of the DSM-5 and debate fomenting over the need for a dimensional nosology (Insel, 2013), now is a good time to take stock of what is known about the structure of psychopathology. We have drawn on insights stemming from six recent findings about the epidemiology of mental disorders.
First, life-course epidemiology points to the need for longitudinal research designs to study the course of psychopathology. Previous research on the structure of psychopathology has been carried out using cross-sectional designs, focusing on individuals who report symptoms within a specified period (most often using the past 12 months as the reporting period). However, research has shown that cross-sectional snapshots mix single-episode, one-off cases with recurrent and chronic cases, which are known to differ in the extent of their comorbid conditions, the severity of their conditions, and possibly the etiology of their conditions. This is true for a variety of common disorders, including, for example, depression and alcohol-use disorders (Jackson & Sartor, in press; Monroe & Harkness, 2011), but also for psychotic experiences (van Os, Linscott, Myin-Germeys, Delespaul, & Krabbendam, 2009). That is, whether manifested as recurrence or chronicity, some people are more prone than others to have persistent (as well as comorbid and severe) psychopathology, These results underscore the need to take the longitudinal course of mental disorders into account when modeling the higher-order structure of psychopathology.
Second, sequential comorbidity points to the need to model multiple disorders over time. Previous research has focused on comorbidity as defined by the co-occurrence of two or more disorders at the same time, but both retrospective (Kessler et al., 2011) and prospective-longitudinal (Copeland, Shanahan, Costello, & Angold, 2011) research has shown that comorbidity is also sequential. For example, longitudinal research has shown that GAD and MDE are linked to each other sequentially such that each disorder increases the likelihood of developing the other disorder in the future among individuals who presented with only one condition at one point in time (Moffitt et al., 2007). These results underscore the need to take into account both concurrent and sequential comorbidity when evaluating the structure of psychopathology.
Third, psychotic disorders can be included in models of the structure of psychopathology. In most previous studies, researchers have omitted psychotic disorders from their evaluation of the structure of psychopathology. There are practical explanations for this omission (e.g., most surveys of psychiatric disorders do not assess psychotic symptoms), but their absence from studies of the structure of psychopathology is conspicuous for three reasons: (a) New research on the dimensional model of psychosis has directed attention to the fact that psychotic symptoms are more commonly experienced in the general population than previously assumed, (b) psychotic disorders are striking in their especially high rates of comorbidity, and (c) psychotic disorders have extraordinary high economic burden, as expressed in the number of years lost due to ill health, disability, or early death (Murray et al., 2012; van Os et al., 2009). A few researchers recently have incorporated psychotic symptoms and symptoms of schizotypal personality disorders into their assessment of the structure of psychopathology, pointing to the existence of a third, distinct Thought Disorder spectrum (Kotov, Chang, et al., 2011; Kotov, Ruggero, et al., 2011). These results underscore the concern that efforts to model the structure of psychopathology without consideration of psychotic symptoms may not capture the true structure in the population.
Fourth, twin studies and risk-factor studies have suggested not only that there are substantial phenotypic correlations among pairs of psychiatric disorders but also that the liability to many disorder pairs (e.g., schizophrenia and bipolar disorder; MDE and GAD; and alcohol and cannabis dependence) is influenced by the same genetic factors (Kendler, 1996; Lichtenstein et al., 2009; Sartor et al., 2010) and that many disorder pairs are characterized by shared intermediate phenotypes (Nolen-Hoeksema & Watkins, 2011). These findings imply that the causes of different disorders may be similar, highlighting the potential value of a transdiagnostic approach to psychiatric disorders. The value of a transdiagnostic approach has been further underscored by evidence that different disorders often respond to the same treatments (Barlow et al., 2011).
Fifth, symptom variation above and below diagnostic cut points implies modeling disorder data at the level of symptom scales. Researchers in most previous studies of the structure of psychopathology have modeled DSM disorders as dichotomous variables, although the few that have used symptom scales have generated comparable results (e.g., Markon, 2010). Diagnostic thresholds increasingly have been acknowledged to be somewhat arbitrary, and it has been recognized that there is meaningful and useful clinical information both above and below diagnostic thresholds (Kessler et al., 2003; Lewinsohn, Shankman, Gau, & Klein, 2004). The DSM-5 also opted to emphasize dimensional conceptualizations of psychiatric disorders.
Sixth, the possibility of one General Psychopathology factor should be tested. This issue has arisen from the observation that disorders are positively correlated not just at the disorder level but substantially so at the spectrum level as well; for example, the correlation between the Externalizing and Internalizing spectra is ~.5. and the correlation between the Internalizing and Thought Disorder spectra has been estimated at ~.6 (Wright et al., 2013). Given high correlations at the spectrum level, Lahey et al. (2012) suggested the intriguing possibility that in addition to propensities to specific forms of psychopathology (e.g., Internalizing vs. Externalizing), there may be one underlying factor that summarizes individuals’ propensity to develop any and all forms of common psychopathologies. They used confirmatory factor models to test a hierarchical bifactor model that derives a general factor from the correlation matrix between different mental disorders and found that depression, anxiety, substance use, and conduct/antisocial disorders all loaded strongly on a single factor, in addition to specific Internalizing and Externalizing spectra (Lahey et al. did not include symptoms of psychosis in their work).
A useful way to think about the meaning of such a general factor in psychopathology is by analogy in relation to cognitive abilities. These abilities are dissociable into separate abilities, such as verbal skills, visuospatial skills, working memory, or processing speed. Nonetheless, the general factor in intelligence (called the g factor) summarizes the observation that individuals who do well on one type of cognitive test tend to do well on all other types of cognitive tests (Deary, 2001; Jensen, 1998; Spearman, 1904). Although specific factors account for variation in each test, the g factor accounts for the positive correlation among all test scores, suggesting that all cognitive functions, to some extent, are influenced by common etiology. Just as there is a general factor of cognitive ability, it is possible that there also is a general factor of psychopathology.
Given the aforementioned new findings and insights, we used data from a comprehensive prospective-longitudinal study of mental disorders; during the past 20 years, we repeatedly assessed symptoms of 11 kinds of common adult mental disorders in a representative birth cohort, from ages 18 to 38 years. The research reported here had four aims. First, we tested alternative models of the structure of psychopathology using data that take into account information about the dimensionality, persistence, co-occurrence, and sequential comorbidity of mental disorders, including psychosis. Second, we evaluated the validity of the structure of psychopathology by testing associations between the factors obtained and independent information about the study members’ personality functioning and life impairment. Third, we tested the family histories and developmental histories associated with each of the factors representing the structure of psychopathology. Fourth, we tested the hypothesis that individual differences in severe and impairing psychopathology are associated with compromised brain integrity from early life.
Method
Dunedin Study
Participants are members of the Dunedin Muitidisciplinary Health and Development Study, a longitudinal investigation of health and behavior in a complete birth cohort. Study members (N = 1,037; 91% of eligible births; 52% male, 48% female) were all individuals born between April 1972 and March 1973 in Dunedin, New Zealand, who were eligible for the longitudinal study based on residence in the province at age 3 and who participated in the first follow-up assessment at age 3. The cohort represents the full range of socioeconomic status in the general population of New Zealand’s South Island and is primarily White. Assessments were carried out at ages 3, 5, 7, 9, 11, 13, 15, 18, 21, 26, 32, and most recently, 38 years, when we assessed 95% of the 1,007 study members still alive. At each assessment wave, study members (including emigrants and prisoners) are brought to the Dunedin Muitidisciplinary Health and Development Research Unit for a full day of interviews and examinations. These data are supplemented by searches of official records and by questionnaires that are mailed, as developmentally appropriate, to parents, teachers, and informants nominated by the study members themselves. The University of Otago Ethics Committee approved each phase of the study.
Assessment of symptoms of mental disorders
The Dunedin Study longitudinally ascertains mental disorders using a strategy akin to experience sampling: Every 2 to 6 years, we interview participants about past-year symptoms. Past-year reports maximize reliability and validity because recall of symptoms over longer periods has been shown to be inaccurate. It is possible that past-year reports separated by 1 to 5 years miss episodes of mental disorder occurring only in gaps between assessments. We tested for this possibility by using life-history calendar interviews to ascertain indicators of mental disorder occurring in the gaps between assessments, including inpatient treatment, outpatient treatment, or spells taking prescribed psychiatric medication (indicators that are salient and recalled more reliably than individual symptoms). Life-history calendar data indicated that virtually all participants having a disorder consequential enough to be associated with treatment have been detected in our net of past-year diagnoses made at ages 18, 21, 26, 32, and 38. Specifically, we identified only 11 people who reported treatment but had not been captured in our net of diagnoses from ages 18 to 38 (many of whom had a brief postnatal depression).
Symptom counts for the examined disorders were assessed via private structured interviews using the Diagnostic Interview Schedule (Robins, Cottler, Bucholz, & Compton, 1995) at ages 18, 21, 26, 32, and 38. Interviewers are health professionals, not lay interviewers. We studied DSM-defined symptoms of the following disorders that were repeatedly assessed in our longitudinal study (see Table S1 in the Supplemental Material available online): alcohol dependence, cannabis dependence, dependence on hard drugs, tobacco dependence (assessed with the Fagerström Test for Nicotine Dependence; Heatherton, Kozlowski, Frecker, & Fagerström, 1991), conduct disorder, MDE, GAD, fears/phobias, obsessive-compulsive disorder (OCD), mania, and positive and negative schizophrenia symptoms. Ordinal measures represented the number of the 7 (e.g., mania and GAD) to 10 (e.g., alcohol dependence and cannabis dependence) observed DSM-defined symptoms associated with each disorder (see Table S1 in the Supplemental Material). Fears/phobias were assessed as the count of diagnoses for simple phobia, social phobia, agoraphobia, and panic disorder that a study member reported at each assessment. Symptoms were assessed without regard for hierarchical exclusionary rules to facilitate the examination of comorbidity. Of the 11 disorders, 4 were not assessed at every occasion, but each disorder was measured at least three times (see Fig. 1 for the structure of psychopathology models and see Table S1 in the Supplemental Material).
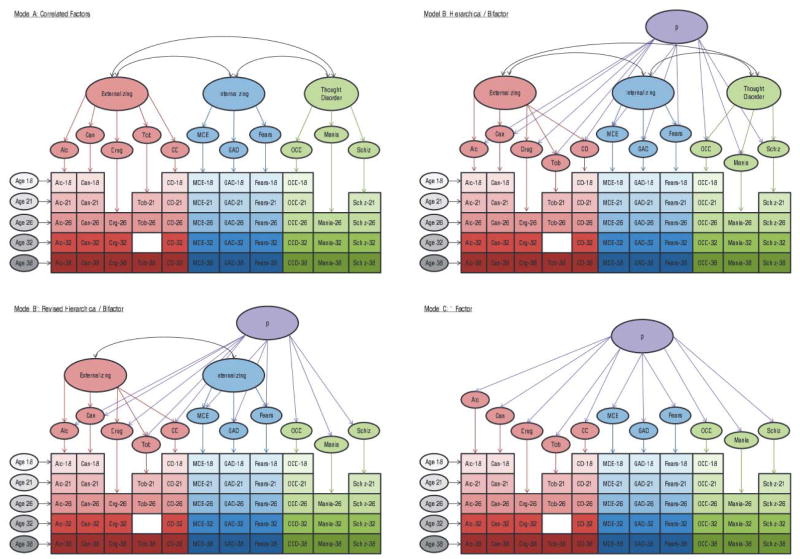
Fig. 1.
The structure of psychopathology Three models were tested using confirmatory factor analysis: a correlated-factors model (Model A), a hierarchical or bifactor model (Model B), and a 1-factor model (Model C) Model B′ shows the final revised hierarchical model Colored ovals represent latent (unobserved) continuous symptom trait factors colored boxes represent observed symptom counts for each disorder at each assessment age The following 11 disorder/symptoms were assessed alcohol dependence, cannabis dependence, dependence on hard drugs, tobacco dependence, conduct disorder, major depression, generalized anxiety disorder, fears/phobias, obsessive-compulsive disorder, mania and positive and negative schizophrenia symptoms. Disorder/symptoms were assessed at ages 18, 21, 26, 32, and 38 years (not all disorders were assessed at every age, but each disorder was measured at least three times; missing assessments are depicted by white space) Gray ovals represent method/state factors designed to pull out age- and assessment-related variance (e.g., interviewer effects, mood effects, and age-specific vulnerabilities) that was uncorrected with trait propensity toward psychopathology. Note Alc = alcohol; Can = cannabis; Drg = hard drugs Tob = tobacco; CD = conduct disorder; MDE = major depression; GAD = generalized anxiety disorder; Fears = fears/phobias; OCD = obsessive-compulsive disorder; Schiz = schizophrenia
Elsewhere we have shown that the past-year prevalence rates of psychiatric disorders in the Dunedin cohort are similar to prevalence rates in nationwide surveys of the United States and New Zealand (Moffitt et al., 2010). Of the original 1,037 study members, we included 1.000 study members who had symptom count assessments for at least one age (871 study members had present symptom counts for all five assessment ages, 955 for four, 974 for three, and 989 for two). The 37 excluded study members comprised those who died or left the study before age 18 or who had such severe developmental disabilities that they could not be interviewed with the Diagnostic Interview Schedule.
Correlates of disorder liability
Table S2 in the Supplemental Material provides measurement details about the correlates of psychopathology reported here, including personality functioning, life impairment, family histories and developmental histories of psychiatric disorders, and measures of brain integrity.
Results
The structure of psychopathology
Using CFA, we tested three standard models (Brunner, Nagy, Wilhelm, 2012; Rindskopf & Rose, 1988) that are frequently used to examine hierarchically structured constructs: (a) a correlated-factors model, (b) a hierarchical or bifactor model, and (c) a 1-factor model (see Fig. 1, Models A, B, and C, respectively). In CFA, latent continuous factors are hypothesized to account for the pattern of covariance among observed variables. As shown in Figure 1, our CFAs were run as multitrait-multimethod models. In these models, observed variables represented each of the 11 disorders with a symptom scale at each assessment age (see Table S1 in the Supplemental Material; e.g., alcohol dependence was measured with a symptom scale at ages 18, 21, 26, 32, and 38). Each model also included method/state factors designed to pull out age- and assessment-related variance (e.g., interviewer effects, mood effects, and age-specific vulnerabilities) that was uncorrected with trait propensity toward psychopathology.
Because symptom-level data are ordinal and have highly skewed distributions, we used polychoric correlations when testing our models. Polychoric correlations provide estimates of the Pearson correlation by mapping thresholds to underlying normally distributed continuous latent variables that are assumed to give rise to the observed ordinal variables. Correlations between disorder/symptom scales ranged from −.05 to .68. In total, 99.0% of the 1,128 correlations were positive. Substantial correlations were observed both within and across disorders (see Table S3 in the Supplemental Material).
All CFA analyses were performed in MPlus version 7.1 (Muthén & Muthén, 1998–2013) using the weighted least squares means and variance adjusted (WLSMV) algorithm. The WLSMV estimator is appropriate for categorical and nonmultivariate normal data and provides consistent estimates when data are missing at random with respect to covariates (Asparouhov & Muthén, 2010).
We assessed how well each model in Figure 1 fit the data using the chi-square value, the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root-mean-square error of approximation (RMSEA). Nonsignificant chi-square tests indicate good model fit; nonetheless, this test is generally overpowered in large sample sizes such as ours. CFI values greater than .95 and TLI values greater than 0.95 indicate good fit; RMSEA scores less than .05 are considered good (Bollen & Curran, 2006).
Do mental disorders form three dimensions? The correlated-factors model
Our first model, a correlated-factors model (see Fig. 1, Model A), has been consistently used in prior research about the structure of psychopathology. Using this model, we tested the hypothesis that there are latent trait factors, each of which influences a subset of the diagnostic symptoms. In our case, we tested three factors representing Externalizing (with loadings from alcohol, cannabis, drugs, smoking, and conduct disorder), Internalizing (with loadings from MDE, GAD, and fears/phobias), and Thought Disorder (with loadings from OCD, mania, and schizophrenia). The model assumes that the Externalizing, Internalizing, and Thought Disorder factors may be correlated. The Externalizing and Internalizing factors have been well documented. Less is known about the usefulness of the Thought Disorder factor in modeling comorbidity. Mania and schizophrenia-spectrum disorders have been suggested as components of this factor, given shared psychotic features and possibly shared genetic etiology between bipolar disorder and schizophrenia (Lichtenstein et al., 2009). OCD has not been consistently included in studies of the structure of psychopathology. However, we included OCD on the Thought Disorder factor because there is increasing recognition that unusual beliefs are the fundamental features of the disorder, at least as much as anxiety (Stein et al., 2010). (Of note, models in which we moved OCD to the Internalizing factor produced comparable results)
Table 1 shows this model with standardized factor loadings and the correlations between the three specific factors (see also Tables S4–S6 in the Supplemental Material). The model fit the data well: χ2(1018, N = 1,000) = 1,737.159, CFI = .962, TLI = 0.958, RMSEA =.027, 90% confidence interval (CI) = [.024, .029]. Loadings on the three specific factors were all positive, generally high (all ps < .001), and averaged 0.834—Externalizing: average loading = 0.807; Internalizing: average loading = 0.870; Thought Disorder: average loading = 0.845. Correlations between the three factors were all positive and ranged from .328 between Internalizing and Externalizing to .849 between Internalizing and Thought Disorder. Thus, this model confirmed that three correlated factors (i.e., Internalizing, Externalizing, and Thought Disorder) explain well the structure of the 11 disorder symptoms examined across 20 years of adulthood.
Table 1.
The Structure of Psychopathology; Model Fit Statistics, Standardized Factor Loadings, and Factor Correlations From Three Different Models
| Statistics, loadings, and correlations | Correlated factors (Model A)
|
Hierarchical/Bifactor (Model B′)
|
1-Factor (Model C)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model fit | Externalizing | Internalizing | Thought disorder | Model fit | P | Externalizing | Internalizing | Model fit | P | |
| Statistic | ||||||||||
| Chi-square (WLSMV) | 1.737.159 | 1,652.586 | 3.404,568 | |||||||
| Degrees of freedom | 1018 | 1012 | 1021 | |||||||
| Comparative Fit Index | 962 | .966 | 875 | |||||||
| Tucker-Lewis Index | 0.958 | 0.963 | 0.862 | |||||||
| RMSEA [90% CI] | .027 [.024, .029] | .025 [.023, .0271 | .048 [.047, .050] | |||||||
| Standardized factor loading | ||||||||||
| Alcohol | 0.733 | 0.397 | 0.626 | 0.698 | ||||||
| Cannabis | 0.885 | 0.455 | 0.811 | 0.825 | ||||||
| Hard drugs | 0.839 | 0.452 | 0.709 | 0.812 | ||||||
| Tobacco | 0.668 | 0.504 | 0.420 | 0.658 | ||||||
| Conduct disorder | 0.909 | 0.557 | 0.691 | 0.865 | ||||||
| Major depression | 0.972 | 0.835 | 0.340 | 0.643 | ||||||
| Generalized anxiety | 0.934 | 0.812 | 0.497 | 0.600 | ||||||
| Fears/phobias | 0.704 | 0.623 | 0.441 | 0.420 | ||||||
| Obsessive-compulsive disorder | 0.726 | 0.725 | 0.578 | |||||||
| Mania | 0.982 | 0.973 | 0.817 | |||||||
| Schizophrenia | 0.826 | 0.819 | 0.685 | |||||||
| Factor correlation | ||||||||||
| Externalizing | .328 | .577 | −.471 | |||||||
| Internalizing | .849 | |||||||||
Note: WLSMV = weighted least squares means and variance adjusted; RMSEA = root-mean-square error of approximation; CI = confidence interval
Is there one General Psychopathology factor? The hierarchical (bifactor) model
Our second model, the hierarchical or bifactor model (see Fig. 1, Model B), has recently been used to demonstrate the existence of a single General Psychopathology factor in adulthood (Lahey et al., 2012). Using this model, we tested the hypothesis that the ordinal symptom measures reflect both General Psychopathology and three narrower styles of psychopathology. General Psychopathology (labeled p in Fig. 1, Model B) is represented by a factor that directly influences all of the diagnostic symptom factors. In addition, styles of psychopathology are represented by three factors, each of which influences a smaller subset of the symptom items. For example, alcohol symptoms load jointly on the General Psychopathology factor and on the Externalizing style factor. The specific factors represent the constructs of Externalizing, Internalizing, and Thought Disorder over and above General Psychopathology. Although the classic hierarchical or bifactor model generally assumes that the specific factors also are uncorrected (Yung, Thissen, & McLeod, 1999), this is not a fundamental requirement of the model (see Park, Sher, Todorov, & Heath, 2011; Rindskopf & Rose, 1988). We allowed the three specific factors to correlate with each other.
Model B had a Heywood case, an estimated variance that was negative for one of the lower-order disorder/symptom factors (specifically, OCD), suggesting this was not a valid model. Inspection of the results revealed the source of the convergence problem. Specifically, the Thought Disorder factor was subsumed in p; that is, in the hierarchical model, symptoms of OCD, mania, and schizophrenia loaded very highly on p, but unlike symptoms of Externalizing and Internalizing, they could not form a separate Thought Disorder factor independently of p.
We respecified the model accordingly, and the results are shown in Table 1 (see also Tables S4–S6 in the Supplemental Material) and depicted in Model B′ of Figure 1. This model fit the data well: χ2(1012, N = 1,000) = 1,652.586, CFT = .966, TLI = 0.963, RMSEA = .025, 90% CT [.023, .027]. Loadings on the General factor (p) were all positive, generally high (all ps < .001), and averaged 0.650; the highest standardized loadings were for mania (0.973), MDE (0.835), schizophrenia (0.819), and GAD (0.812). Similarly, the loadings for the two specific factors were all positive and averaged 0.651 for Externalizing and 0.426 for Internalizing. Because Models A and B′ are not nested, we could not directly compare them. Moreover, the WLSMV estimator does not produce comparative model fit indices such as Akaike information criterion or Bayesian information criterion. We can conclude that Models A and B′ fit our data similarly well, with Model B′ offering a slightly more parsimonious solution. The findings suggest that Model B′, with General Psychopathology, must be considered a serious contender accounting for individual differences in the liability to psychiatric disorders in the population.
What happens to Internalizing and Externalizing after p is extracted?
Comparing the factor loadings in the correlated-factors model versus the hierarchical model (see Fig. 1, Models A and B′, respectively) provides useful information about the relative importance of the general versus specific factors in explaining manifest psychopathology (see Table 1). If the loadings of the manifest variables on the specific factors are substantially reduced from Model A to Model B′, we can conclude that a particular manifestation of psychopathology (e.g., conduct disorder or MDE) is relatively more indicative of General Psychopathology (p). For example, the standardized loading for conduct disorder symptoms in the correlated-factors model was 0.909, but in the hierarchical model, the standardized loading of conduct disorder symptoms on Externalizing was reduced to 0.691. This result indicates that much of the propensity to persistent conduct disorder symptoms from adolescence to midlife is indicative of General Psychopathology rather than specific to an Externalizing style. In contrast, the standardized loading for cannabis dependence on Externalizing remained similar from Model A to Model B′, suggesting that the propensity to cannabis dependence is a combination of an Externalizing style along with a general tendency to psychopathology.
Comparing the factor correlations in the correlated-factors model (Model A) versus the hierarchical model (Model B′) revealed a significant positive correlation (r = .328) between Externalizing and Internalizing in the correlated-factors model but a negative correlation (r = −.471) between Externalizing and Internalizing in the hierarchical model. This result suggests that Externalizing and Internalizing are positively correlated in the population because they share a common liability to General Psychopathology, but after controlling for General Psychopathology, individuals who are prone to substance use and antisocial behavior are less prone to depression and anxiety, and vice versa.
Will a simple 1-factor model suffice?
Given that the model with p fit well, the question arises: Are the specific factors needed? Therefore, we tested a simple structural model that assigned each diagnostic symptom factor only to the General Psychopathology factor (see Fig. 1, Model C). Loadings onto the general factor were all positive, generally high (all ps < .001), and averaged 0.691 (see Table 1). However, this model did not fit the data well: χ2(1021, N = 1,000) = 3,404.568, CFI = .875, TLI = 0.862, RMSEA = .048, 90% CI [.047, .050] We concluded that p alone is insufficient to describe our data: Internalizing and Externalizing dimensions add information beyond p.
How are disorder-liability factor scores correlated across different models?
We output factor scores from the correlated-factors model (A) and the hierarchical model (B′), saved them, and calculated their correlations with each other (see Table S7 in the Supplemental Material). These correlations make three points. First, all three factors from the correlated-factors model were highly correlated with General Psychopathology (rs ranged from .639 for Externalizing to .997 for Thought Disorder), suggesting that to some extent, all three factors in the correlated-factors model reflect General Psychopathology. Second, the extremely high correlation between Thought Disorder and General Psychopathology (r = .997) suggests that the Thought Disorder factor from the correlated-factors model reflects General Psychopathology to the greatest extent. Third, the Externalizing factor from the correlated-factors model is less indicative of General Psychopathology than the Internalizing factor. This is suggested by the finding that Externalizing correlated less strongly than Internalizing with General Psychopathology (rs = .639 vs. .917) and that the Externalizing factor showed more consistency than the Internalizing factor from the correlated-factors model to the hierarchical model (rs = .844 vs. .461).
Sex differences in disorder liabilities
In the correlated-factors model (A), males were more likely to exhibit Externalizing and females were more likely to exhibit Internalizing, with no sex differences in Thought Disorder (see Table 2). Moving to the hierarchical model (B′), there were no sex differences in the tendency toward General Psychopathology. It is interesting that sex differences in Externalizing and Internalizing became more pronounced once General Psychopathology was taken into account; the absolute magnitude of the correlation between sex and Externalizing increased from .277 to .386 and that between sex and Internalizing increased from −.197 to −.431, suggesting that independently of a liability to General Psychopathology, Externalizing and Internalizing are highly gendered styles. In all further analyses, we controlled for sex.
Table 2.
Correlations Between Disorder-Liability Factor Scores and Gender, Adult Personality Trait Scores, Life Impairment, Developmental History, and Brain Integrity
| Measure | Correlated factors (Model A)
|
Hierarchical/Bifactor (Model B′)
|
||||
|---|---|---|---|---|---|---|
| Externalizing | Internalizing | Thought Disorder | Externalizing | Internalizing | p | |
| Gender | .277 | −.197 | −.025 | .386 | −.431 | −.042 |
| 5-factor model of personality | ||||||
| Extraversion | .086 | −.051 | −.009 | .128 | −.134 | −.018 |
| Agreeableness | −.319 | −.222 | −.300 | −.184 | .129 | −.308 |
| Conscientiousness | −.330 | −.252 | −.316 | −.209 | .106 | −.313 |
| Neuroticism | .226 | .418 | .413 | −.024 | .148 | .423 |
| Openness to Experience | .031 | .049 | .034 | .031 | .014 | .024 |
| Life impairment | ||||||
| Suicide attempt | .370 | .377 | .421 | .179 | −.028 | .426 |
| Psychiatric hospitalization | .241 | .258 | .291 | .106 | −.040 | .293 |
| Duration of social-welfare benefit use | .388 | .326 | .403 | .210 | −.104 | .415 |
| Violence conviction | .426 | .190 | .305 | .334 | −.227 | .311 |
| Developmental history | ||||||
| Social class | −.129 | −.095 | −.137 | −.062 | .067 | −.143 |
| Family history of psychiatric disorder | ||||||
| Major depression | .155 | .238 | .225 | .044 | .068 | .224 |
| Anxiety | .161 | .218 | .219 | .045 | .053 | .224 |
| Psychosis | .094 | .114 | .132 | .031 | −.016 | .132 |
| Conduct disorder or antisocial personality | .265 | .224 | .263 | .145 | −.042 | .272 |
| Substance dependence | .325 | .240 | .281 | .221 | −.062 | .288 |
| Childhood history of psychiatric disorder | ||||||
| Externalizing | .361 | .219 | .301 | .253 | −.149 | .308 |
| Internalizing | .085 | .294 | .256 | −.080 | .189 | .261 |
| Childhood maltreatment | .193 | .183 | .203 | .098 | −.023 | .210 |
| Brain integrity | ||||||
| Adulthood | ||||||
| WAIS-IV Full Scale IQ | −.164 | −.118 | −.174 | −.072 | .070 | −.189 |
| Verbal Comprehension | −.139 | −.049 | −.115 | −.084 | .112 | −.129 |
| Perceptual Reasoning | −.116 | −.077 | −.116 | −.054 | .062 | −.129 |
| Working Memory | −.126 | −.154 | −.171 | −.028 | −.027 | −.183 |
| Processing Speed | −.126 | −.134 | −.166 | −.035 | .019 | −.176 |
| Executive function | ||||||
| Trail Making Test B | .077 | .150 | .162 | −.025 | .037 | .169 |
| WMS-III Mental Control | −.212 | −.158 | −.198 | −.130 | .047 | −.204 |
| CANTAB Rapid Visual Information Processing: A-Prime | −.119 | −.142 | −.168 | −.031 | .001 | −.172 |
| Memory test | ||||||
| Rey Auditory Verbal Learning: Total Recall | −.124 | −.110 | −.147 | −.052 | .037 | −.155 |
| Rey Auditory Verbal Learning Delayed Recall | −.120 | −.082 | −.121 | −.065 | .061 | −.128 |
| CANTAB Visual Paired Associates Learning: Total Errors | .127 | .118 | .137 | .065 | −.023 | .138 |
| Motor test | ||||||
| Grooved Pegboard | .063 | .132 | .154 | −.038 | .003 | .161 |
| One-Legged Balance | −.076 | −.111 | −.111 | −.012 | −.035 | −.120 |
| CANTAB Reaction Time: 5-Choice Reaction Time | −.022 | .062 | .055 | −.071 | .042 | .055 |
| Everyday cognitive impairment | .302 | .272 | .329 | .157 | −.052 | .331 |
| Retinal microvasculature | ||||||
| Arteriolar caliber | .025 | −.006 | .013 | .017 | −.023 | .014 |
| Venular caliber | .098 | .123 | .122 | .045 | .006 | .126 |
| Preschool (age 3) | ||||||
| Preschool brain integrity factor | −.053 | −.146 | −.155 | .049 | −.024 | −.162 |
| Pea body Picture Vocabulary | −.050 | −.083 | −.095 | .009 | .008 | −.103 |
| Bayley Motor Skills | .018 | −.085 | −.073 | .071 | −.048 | −.071 |
| Reynell Verbal Comprehension Scale | −.051 | −.140 | −.147 | .046 | −.027 | −.153 |
| Neurologic abnormalities | .056 | .115 | .127 | −.023 | .018 | .130 |
| Examiner-rated lack of control | .046 | .096 | .110 | −.023 | −.005 | .116 |
| Childhood | ||||||
| Stanford-Binet IQ (age 5) | −.092 | −.133 | −.164 | .011 | .015 | −.173 |
| WISC-R IQ (ages 7–11) | −.057 | −.119 | −.138 | .045 | −.017 | −.151 |
| Low self-control factor | .192 | .211 | .248 | .058 | −.013 | .257 |
Note: All analyses controlled for sex Arteriolar and venular caliber were each adjusted for the effect of the other vessel as recommended, to isolate the unique effects for each vessel (see Shalev et al, 2013) All correlations greater than 10 (p ~ < 01) are displayed in bold font WAIS-IV = Wechsler Adult Intelligence Scale–IV; WMS-III = Wechsler Memory Scale–III; WISC-R = Wechsler Intelligence Scale for Children–Revised
Interpreting the disorder-liability dimensions by describing their correlates
Personality functioning and disorder liabilities
Each of the three factors from the correlated-factors model (A) was significantly associated with low trait Agreeableness, low Conscientiousness, and high Neuroticism (see Table 2). According to the hierarchical model (B′), this is because the disorder-liability factors each tap General Psychopathology, Table 2 shows that General Psychopathology is distinctly characterized by high Neuroticism and low Agreeableness and Conscientiousness. The hierarchical model also revealed some prominent differences between the personality styles associated with Externalizing and Internalizing syndromes net of General Psychopathology. Individuals who score high on a liability to Externalizing disorders, net of a tendency toward General Psychopathology, have poorer impulse control (low Conscientiousness); can be aggressive, rude, and manipulative (low Agreeableness); but also evoke and enjoy social attention and appear to be sensitive to potential rewards (high Extraversion). In contrast, individuals who score high on a liability to Internalizing style disorders, net of General Psychopathology, are more easily distressed (high Neuroticism) and tend to refrain from actively approaching, engaging, or exploring their environment (low Extraversion), although they tend to be agreeable.
Life impairment and disorder liabilities
Each of the three factors from the correlated-factors model (A) was significantly and positively associated with life impairment (see Table 2). The hierarchical model (B′) revealed that part of the reason each of the liability factors is related to suicide attempts, psychiatric hospitalization, greater reliance on social-welfare benefits throughout adulthood, and violence convictions is that each factor taps General Psychopathology, Table 2 shows that General Psychopathology was more strongly correlated with these indicators of life impairment than were the specific factor scores. An interesting exception was the Externalizing spectrum, which also was associated with impairment (e.g., suicide attempts, reliance on government benefits, and violence convictions) independently of General Psychopathology, suggesting that individuals with a liability to antisocial and substance-use disorders disproportionately tax a nation’s health, welfare, and justice systems. However, in general, people with higher levels of p had the greatest life impairment.
Developmental histories of disorder liabilities
It is well known that social class is related to most types of mental disorders (see Table 2). The hierarchical model (B′) revealed that part of the reason for these ubiquitous associations is that more deprived childhoods are associated with increased risk of General Psychopathology.
Table 2 shows that family psychiatric history was linked to each of the three factors from the correlated-factors model (A). However, there was little specificity in these associations. The hierarchical model (B′) revealed that part of the reason family histories of specific disorders were related to all disorder liabilities is that disorder liability taps General Psychopathology. Table 2 shows that General Psychopathology was more strongly correlated with the family history of each disorder than were the specific factor scores. An interesting caveat is again apparent in relation to the Externalizing factor from the hierarchical model, which was associated with family history of antisocial and substance-use disorders, suggesting that the liability to Externalizing disorders also transmits within families independently of General Psychopathology.
Adults who scored high on each of the three disorder-liability factors were significantly more likely to have met diagnostic criteria for a psychiatric disorder before age 15 years (see Table 2). The hierarchical model showed that this too is due in part to the fact that early onset of psychiatric disorder was especially likely to be linked to a liability to General Psychopathology in adulthood.
Finally, adults who scored high on each of the disorder-liability factors also were significantly more likely to have been maltreated in childhood. Nonetheless, the hierarchical model suggests that maltreatment is associated with greater General Psychopathology but not with any specific manifestation type (see Table 2).
Brain integrity and disorder liabilities across the life course
Multiple measurement tools revealed compromised brain function among adults who scored high on each of the disorder-liability factors. The hierarchical model (B′) showed that this result mostly is due to compromised mental functions associated with high levels of p. Table 2 shows that adults with higher levels of p scored lower on an IQ test than their age peers with lower levels of p. A closer look at separate scores representing the major components of intelligence, as well as additional tests of executive function, memory, and motor functioning, shows that adults with higher levels of p fared less well on tests requiring attention, concentration, mental control, visual-perceptual speed, and visual-motor coordination. Attesting to the ecological validity of these deficits, people who knew them well said that individuals with high levels of p experienced cognitive problems in their everyday lives.
A further window onto the health of the brain is provided by retinal imaging. Retinal and cerebral small vessels share similar embryological origin, structural, and physiological features (Patton et al., 2005). Thus, assessing retinal vasculature provides a noninvasive method to visualize the health of the vascular network of the brain (Shalev et al., 2013). Of particular interest is the caliber of the retinal arterioles and venules because they are the most commonly studied retinal parameters in relation to cerebrovascular disease (Ikram, Ong, Cheung, & Wong, 2013). Vessel caliber may relate to mental disorders as cause, consequence, or both. As Table 2 shows, p was associated, in particular, with wider venules, which are thought to reflect, in part, damage to microvasculature associated with problems of oxygen supply to the brain (de jong et al., 2008).
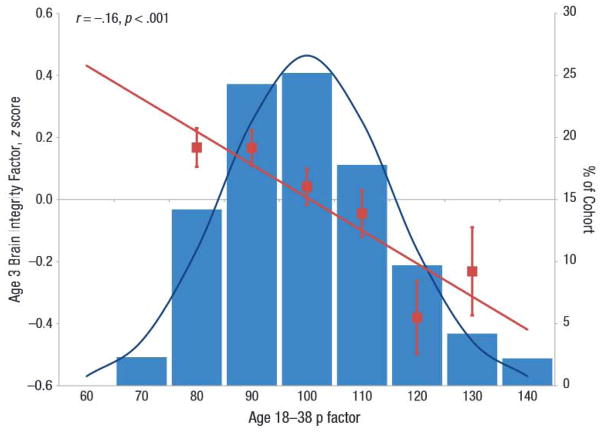
Table 2 shows that compromised brain functions were already apparent in the first decade of life and reach back to age 3 years. Early variation in brain integrity is likely to have genetic as well as environmental origins. Children who grew up to score high on the p factor displayed less brain integrity (e.g., they presented with neurologic soft signs, impairments in receptive language development, and deficits on standard IQ tests). Figure 2 shows the distribution of the p factor in the population and the association between the p factor and brain integrity. Moreover, poor childhood self-control, reflecting executive deficits and emotional dysregulation, cut across all disorder liabilities and was a salient early developmental feature of the p factor (see Table 2).
Fig. 2.
Association between p factor scores and age-3 brain Integrity. The p factor is standardized to a mean of 100 (SD = 15), and higher p scores Indicate more Generalized Psychopathology. The bars of the histograms graph the percentages of the sample at different levels of the p factor. The squares and standard error bars show the scores of individuals on the age-3 brain integrity factor as a function of p scores less than 85, 85 to 95, 95 to 105, 105 to 115, 115 to 125, and greater than 125. The regression line shows the correlation between the p factor and childhood brain integrity.
Discussion
We examined the structure of psychopathology taking into account dimensionality, persistence, co-occurrence, and sequential comorbidity of mental disorders across 20 years, from adolescence to midlife. The structure of mental disorders could be summarized by three core psychopathological dimensions: An Internalizing liability to depression and anxiety; an Externalizing liability to antisocial and substance-use disorders; and a Thought Disorder liability to symptoms of psychosis. In addition, we found evidence pointing to one general underlying dimension that summarized individuals’ propensity to develop any and all forms of common psychopaihologies. Higher scores on this dimension were associated with more life impairment, greater familiality, worse developmental histories, and more compromised early-life brain function.
These findings about the structure of psychopathology align with several studies in suggesting that in addition to the well-established dimensions of Internalizing and Externalizing liabilities, there is a third, distinct dimension, characterized by disordered thoughts (Kotov, Ruggero, el al., 2011; Markon, 2010). There are some minor differences between the nature of the Thought Disorder factor that has been uncovered across these recent studies; for example, in some studies, it includes schizophrenia and schizotypical personality disorder, whereas in others it also includes avoidant personality trails. Here we included OCD (but the factor was robust with or without OCD). These differences are most likely due to the different content sampled in different studies (e.g., a mixture of Axis I and Axis II disorders vs. Axis I disorders alone), but the unmistakable conclusion is that the structure of common psychiatric disorders in the population is insufficiently described without including disordered thought.
Although the existence of a Thought Disorder dimension may not surprise, the possibility of a General Psychopathology dimension may (Lahey et al., 2012). Al the level of the population, this General Psychopathology factor reflects the epidemiological reality that psychiatric disturbance tends to unfold across years of development as persistent and comorbid. At the level of the individual, this factor reflects meaningful differences between persons on a single dimension that represents the tendency to experience psychiatric problems as persistent and comorbid. Personality information we obtained from independent sources (informants) showed that individuals who score high on this General Psychopathology factor are characterized by three traits that compromise processes by which people maintain stability—low Agreeableness, low Conscientiousness, and high Neuroticism (DeYoung, Peterson, & Higgins, 2002); that is, high- p individuals experience difficulties in regulation/control when dealing with others, the environment, and the self.
Here we have coined the term p factor to represent this dimension of General Psychopathology, in recognition that it conceptually parallels a dimension already familiar in behavioral science: the g factor, or general intelligence. General intelligence is known to influence correct/incorrect performance on hundreds of cognitive test items, which aggregate into a dozen or more distinct mental abilities, which further aggregate into two overarching verbal versus visuospatial domains, which finally aggregate into one normally distributed dimension of mental ability from low to high: g, usually measured by the IQ. Almost all of the variation in the lower-order abilities is accounted for by g. We propose that p influences present/absent performance on hundreds of psychiatric symptoms, which are typically aggregated into dozens of distinct diagnoses, which further aggregate into two overarching Externalizing versus Internalizing domains, which finally aggregate into one normally distributed dimension of psychopathology from low to high: p. Almost all of the variation in the lower-order abilities is accounted for by p. As the g dimension reflects low-to-high mental ability, the p dimension may represent low-to-high psychopathology severity. The higher a person scores on p, the worse that person fares on indicators tapping severity, duration of disorder, extent of sequential comorbidity, adult life impairment, childhood developmental history, family history of liability to psychiatric illness, and brain function from early life to midlife.
This collection of observations implies that p is a dimension that unites all disorders and has neurological roots. It is important to acknowledge that the uniformly positive correlations we observed within and across disorders—and the resulting factor solutions—do not prove the existence of a unitary g-like causal factor. As has been pointed out in relation to intelligence (van der Maas et al., 2006), such positive intercorrelations also could result from dynamic processes during development, rather than from a single unitary cause (e.g., having one disorder could raise the risk of developing most other disorders). The findings presented in this article suggest that there may be a factor that accounts for meaningful variance across major forms of psychopathology, and etiological and nosological research could benefit from probing its origins.
Our initial look at the correlates of psychopathology in longitudinal data generated the expected associations with the Internalizing and Externalizing factors. Yet after p was isolated as a higher-order factor, these correlations decreased considerably in size and in many cases dropped to insignificant (see Table 2). After extracting variance from Externalizing that belonged to p, associations between Externalizing and life-impairment indicators more than halved (excepting with violence). Post-p, Externalizing reduced its correlations with etiological factors, including family psychiatric history, child maltreatment, and indicators of brain integrity. Post-p, Externalizing was associated with a personality style of Extraversion, low Agreeableness, and low Conscientiousness, and it is interesting that its association with male sex grew stronger. Likewise, after extracting variance from Internalizing that belonged to p, Internalizing was uncorrelated with life-impairment indicators (excepting a negative association with violence). Post-p, Internalizing lost its correlations with etiological factors, including family psychiatric history, child maltreatment, and indicators of brain integrity. Post-p, Internalizing was associated with a personality style of Introversion and Neuroticism, and it is interesting that its association with female sex grew notably stronger. These post-p reductions imply that the Externalizing and Internalizing components of the structure of psychopathology primarily represent gendered personality styles. Net of p, there remain individual differences in symptom picture, but they do not necessarily involve harmful dysfunction (i.e., not psychopathology; wakefield, 2007).
Research is needed to uncover how these Externalizing versus Internalizing styles shape a patient’s particular symptom picture. A comparison to g is illustrative. Even within the top .5% of intellectually gifted junior high school students characterized by extreme high g, followed up in midlife, gifted persons with relatively greater talent for verbal versus visuospatial problem solving had veered toward career paths in the humanities and law, whereas gifted persons with relatively greater visuospatial than verbal talent had ended up in science, technology, engineering, and mathematics fields (Kell, Lubinski, & Benbow, 2013). It is possible that the Externalizing and Internalizing factors represent gender-linked behavioral styles and preferences that steer how an individual’s tendency toward General Psychopathology will be expressed as particular diagnosed disorders (Martel, in press).
A methodological advantage of the current study is that it draws on what may be the most comprehensive longitudinal-epidemiological study of psychiatric disorders. Even so, our analysis is not without limitations. First, we studied only Axis I disorders and did not assess all such disorders, especially very low base-rate disorders. Researchers with more complete psychiatric data must test whether the observed structure of psychopathology will be robust to the addition of new disorders. Second, our data are right censored at age 38 years, and we have yet to assess aging-related disorders. Researchers with older cohorts must test whether the observed structure of psychopathology will prove age invariant. Third, we used an experience-sampling approach, ascertaining disorder/symptoms in five 1-year windows spaced across 20 years. Contiguous annual assessments would be better, but neither funders nor research participants favor this approach. Fourth, we were not able to test sex differences in the structure of psychopathology because we calculated that our sample size is underpowered for conducting such tests in the estimated models. Larger samples might test sex differences. Fifth, our findings are limited to a cohort born in the early 1970s in one city in New Zealand. Other samples must test whether Thought Disorder and General Psychopathology generalize across time, place, and culture. We have been encouraged by similar structural models reported recently from American and Australian samples (Kotov, Ruggero, et al., 2011; Lahey et al., 2012; Wright et al., 2013). Against this background, we hope that the present study, like our initial study (Krueger et al., 1998), generates further tests, extensions, and discussions about the structure of common mental disorders. In the following section, we offer hypotheses.
Research on the structure of psychopathology was initially motivated by the notion that comorbidity could be exploited to inform, rather than confuse, understanding of the structure of mental disorders (Caron & Rutter, 1991; Wittchen. 1996). Specifically, it was hoped that grouping disorders into clusters would facilitate research and treatment. But despite enthusiasm for grouping schemes such as Internalizing and Externalizing, the bulk of mental-health research is still conducted on single disorders one by one, and hope springs eternal for biomarkers that will cleanly make differential diagnoses between disorders, even within a cluster (Kapur, Phillips, & Insel, 2012). Now, the possibility that there may be a single General Psychopathology factor that summarizes individuals’ propensity to develop all forms of common psychopathologies complicates the theory picture. Is p merely a statistical reductio ad absurdum or is it real and meaningful? We do not know yet, but below we speculate about what p could mean by pointing to testable hypotheses.
A structural hypothesis is that as a dimension of severity, p has Thought Disorder symptoms at its pinnacle. Any individual who carries a strong General Psychopathology liability might, if their disorder grows severe enough, experience psychotic thought processes, whatever the presenting diagnosis; that is, unwanted irrational thoughts are not just for the formal psychoses. Cognitive behavioral therapies aimed at correcting patients’ inaccurate thoughts are among the most effective treatments for a wide variety of disorders. The clinical literature is replete with discussion of disordered thought processes in the context of affective disorders, anxiety disorders, eating disorders, autism, posttraumatic stress disorder, somatoform disorders, dissociative disorders, identity disorders, personality disorders, and substance disorders. Most chapters of the DSM mention thought symptoms. Indeed, in general, the only disorders lacking prominent focus on disordered thought in their symptom criteria are disorders of childhood.
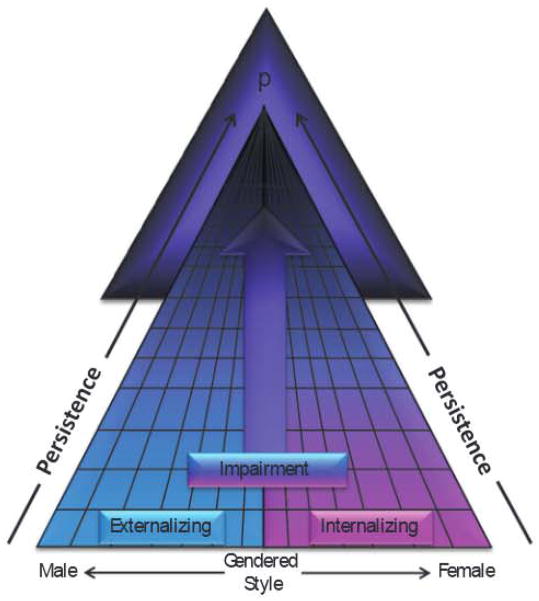
A developmental extension of this dimensional severity hypothesis is that there could be a developmental progression of severity. In such a developmental progression, many individuals manifest a brief episode of an individual disorder, a smaller subset of individuals progress to develop a persistent Internalizing or persistent Externalizing syndrome, whereas only a very few individuals progress to the extreme elevation of p, ultimately emerging with a psychotic condition most likely during late adolescence or adulthood (see Fig. 3 for a graphic representation of the p factor). Such a developmental progression would require in the first instance that brief episodes of single disorders are widespread in the population, which is supported by the high lifetime prevalence rates of individuals with disorder accumulated during years of follow-up in longitudinal studies (Copeland et al., 2011; Moffitt et al., 2010). A developmental progression also would require that individuals who manifest psychosis have an extensive prior history of many other disorders, which has been reported (Gyllenberg et al., 2010; Kim-Cohen et al., 2003; Sourander et al., 2005). In addition, a developmental progression would anticipate that when individuals are followed long enough, those with the most severe liability to psychopathology will tend to move in and out of diagnostic categories. Today’s patient with schizophrenia was yesterday’s boy with conduct disorder or girl with social phobia (and tomorrow’s older adult with dementia and severe depression). This developmental progression hypothesis is consistent with evidence that sequential comorbidity is the rule rather than the exception (Cerda, Sagdeo, & Galea, 2008) and that individuals experiencing sequentially comorbid disorders also exhibit more severe psychopathology (e.g., Moffitt et al., 2007).
Fig. 3.
The p factor. Many individuals manifest a brief episode of a gendered individual disorder, a smaller subset of individuals progress to develop persistent and increasingly impairing externalizing and internalizing disorders, whereas only a few individuals progress to extreme elevation of p, ultimately emerging with disordered thought processes.
It is noteworthy that we can recover the p factor at each of the separate assessment ages (18–38 years) in our longitudinal study. This result is important because it suggests (a) the presence of p at different ages and (b) that other researchers who have cross-sectional data—rather than a long-term longitudinal study—may be able to replicate this structure. That said, longitudinal data allowed us to capture recurrence and sequential comorbidity, providing a better handle on severity and impairment. For example, the longitudinal p factor correlated .426 with suicide attempt and .293 with psychiatric hospitalization, whereas the cross-sectional p factors, on average, correlated .345 and .239 with these indicators of life impairment. Likewise, childhood brain integrity correlated −.162 with the longitudinal p factor but, on average, correlated −.132 with the cross-sectional p factors.
An etiological hypothesis is that the origins of p begin with genetic liability, with the genes involved operating in pleiotropic fashion to enhance risk for any and all disorders rather than breeding true to any single disorder. This is implied by our finding that p was equally well predicted by family histories of depression, anxiety, psychosis, antisocial disorders, and substance disorders. A recent genome-wide association study that indicated that genetic variants are linked to multiple diagnoses is consistent with this hypothesis (Smoller et al., 2013). This liability might be initially manifested as (or exacerbated by) neurological deficits in the earliest years of life, as suggested by our data here. The implications of p for etiological research are not inconsistent with those espoused in the Research Domain Criteria project: that research should not be constrained by current DSM categories, that mental disorders are brain disorders, and that psychopathology is dimensional (Insel, 2013; Sanislow et al., 2010). Uncovering the etiology of p will require measurements across genetic, neural, cognitive, and environmental domains.
Our final speculative hypothesis is that p might have implications for the scientific concept of specificity (sometimes also referred to as differential validity; Garber & Hollon, 1991). For example, the existence of p may explain why it has been so difficult to identify etiological factors that confer differential risk to one specific psychiatric disorder but not another. Indeed, virtually all of the risk factors and correlates that we tested were associated with liabilities to develop Internalizing, Externalizing, and Thought Disorder, and this nonspecificity was empirically due to the fact that all of the risk factors were primarily associated with p. Consider childhood maltreatment. Childhood maltreatment appears to be a risk factor in the history of patients having many different psychiatric outcomes, including mood disorders, anxiety disorders, behavior disorders, and substance-use disorders (Green et al., 2010; Scott, Smith, & Ellis, 2010), as well as schizophrenia, psychosis, and psychotic-like experiences and symptoms (Varese et al., 2012). Indeed, it is more difficult to identify a disorder to which childhood maltreatment is not linked than to identify a disorder to which it is linked with specificity. In addition, childhood maltreatment predicts disorder that is severe: recurrent, persistent, and treatment resistant (Nanni, Uher, & Danese, 2012). An intriguing possibility, suggested by our results, is that childhood maltreatment raises risk for a particular psychiatric disorder because maltreatment exacerbates the liability to experience any disorder at all (Keyes et al., 2012; Lahey et al., 2012).
This question raised by p about the dubious specificity of etiological variables extends to other variables studied in psychological science, suggesting that researchers should not expect to routinely find single-disorder loyalty in biomarkers (e.g., neuroimaging findings, cognitive task performance, and hypothalamic-pituitary-adrenal axis hormones), consequences (e.g., suicide attempts and impaired relationships), treatments (e.g., psychotherapy and pharmacotherapy), or causes (e.g., maltreatment and genes).
We do not argue that disorder-specific correlates can never be found. Just as the existence of g does not preclude a specific cause (e.g., stroke, tumor, or head injury) disrupting one isolated mental function, the existence of p would not preclude a specific cause generating an isolated syndrome. Instead, we suggest that they will be challenging to find because if a disorder’s connections to biomarkers/causes/consequences/treatments covary in a dose-response fashion with the disorder’s severity, then the same biomarkers/causes/consequences/treatments must tend to characterize other disorders too. This promiscuity of correlates is an inevitable consequence of the fact that severe disorders tend to be comorbid, concurrently and sequentially.
Again, the parallel between p and g is informative. In neuropsychological research, before claiming a specific association between any lower-order Cognitive Ability X and Correlate Y, researchers usually ask whether the association survives statistical control for the contribution of g (IQ). If our hypothesis about p is correct, then to document a specific association between any particular Psychiatric Disorder X and Correlate Y, the contribution of p to their association should be considered first. Doing so requires reliable and valid measures of p for research use, which need to be developed. Translational studies seeking biomarkers for one disorder certainly should include not only healthy control participants but also psychiatric control participants who have other disorders (Kapur et al., 2012; Schwartz & Susser, 2011). At a minimum, researchers should no longer assume a specific relation between the disorder they study and a biomarker/cause/consequence/treatment without empirical verification. Rather, our finding suggests the default assumption must be that biomarkers/causes/consequences/treatments relate first to p.
Supplementary Material
Acknowledgments
The authors thank the Dunedin Study members, their families, Dunedin Multidisciplinary Health and Development Research Unit research staff, and study founder Phil Silva.
Funding
This research received support from the National Institute on Aging (NIA; Grant G032282) and the Medical Research Council (Grant MRK00381X). Additional support was provided by the National Institute of Child Health and Human Development (NICHD; Grant HD061298) and the Jacobs Foundation. D. W. Belsky was supported by a postdoctoral fellowship from the NIA (T32 AG000029). S. J. Goldman-Mellor was supported by a postdoctoral fellowship from the NICHD (T32 HD07376). S. Israel was supported by a Rothschild Fellowship from the Yad Hanadiv Rothschild Foundation. M. H. Meier was supported by a postdoctoral fellowship from the National institute on Drug Abuse (P30 DA023026). The Dunedin Multidisciplinary Health and Development Research Unit is supported by the NewZealand Health Research Council.
Footnotes
Reprints and permission: sagepub.com/journalsPermissions.nav
Declaration of Conflicting Interests
The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
Author Contributions
A. Caspi, R. M. Houts, and T. E. Moffitt created the study concept and design and drafted the manuscript. A. Caspi, S. Ramrakha, R. Poulton, and T. E. Moffitt acquired the data. A. Caspi, R. M. Houts, D. W. Belsky, S. J. Goldman-Mellor, H. Harrington, S. Israel, M. H. Meier, I. Shalev, R. Poulton, and T. E. Moffitt analyzed and interpreted the data. D. W. Belsky, S. J. Goldman-Mellor, H. Harrington, S. Israel, M. H. Meier, I. Shalev, and R. Poulton critically revised the manuscript for important intellectual content. R. M. Houts and H. Harrington provided statistical analysis. A. Caspi, R. Poulton, and T. E. Moffitt obtained funding. H. Harrington and S. Ramrakha provided administrative, technical, and material support. A. Caspi and T. E. Moffitt supervised the study.
Additional supporting information may be found at http://cpx.sagepub.com/content/by/supplemental-data
References
- Achenbach TM, Edelbrock C. Behavioral problems and competencies reported by parents of normal and disturbed children aged 4 through 16. Monographs of the Society for Research in Child Development. 1981;46(188) [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Asparouhov T, Muthen B. Weighted least squares estimation with missing data. 2010 Retrieved from http://www.statmodel.com/download/GstrucMissingRevision.pdf.
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J. The unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York, NY: Oxford University Press; 2011. [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation approach. New York, NY: Wiley; 2006. [Google Scholar]
- Brunner M, Nagy G, Wilhelm O. A tutorial on hierarchically structured constructs. Journal of Personality. 2012;80:796–846. doi: 10.1111/j.1467-6494.2011.00749.x. [DOI] [PubMed] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Cerda M, Sagdeo A, Galea S. Comorbid forms of psychopathology: Key patterns and future research directions. Epidemiologic Reviews. 2008;30:155–177. doi: 10.1093/epirev/mxn003. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: Challenges to the current system and future directions. Annual Review of Psychology. 1995;46:121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: A prospective cohort analysis from the Great Smoky Mountains Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deary IJ. Intelligence, a very short introduction. Oxford, England: Oxford University Press; 2001. [Google Scholar]
- de Jong FJ, Vernooij MW, Ikram MK, Ikram MA, Hofman A, Krestin GP, Breteler MM. Arteriolar oxygen saturation, cerebral blood flow, and retinal vessel diameters: The Rotterdam Study. Ophthalmology. 2008;115:887–892. doi: 10.1016/j.ophtha.2007.06.036. [DOI] [PubMed] [Google Scholar]
- DeYoung CG, Peterson JB, Higgins DM. Higher-order factors of the Big Five predict conformity: Are there neuroses of health? Personality and Individual Differences. 2002;33:533–552. [Google Scholar]
- Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychological Medicine. 2013;43:97–108. doi: 10.1017/s0033291712001092. [DOI] [PubMed] [Google Scholar]
- Garber J, Hollon SD. What can specificity designs say about causality in psychopathology research? Psychological Bulletin. 1991;110:129–136. doi: 10.1037/0033-2909.110.1.129. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyllenberg D, Sourander A, Niemela S, Helenius H, Sillanmaki L, Piha J, Almqvist F. Childhood predictors of later psychiatric hospital treatment: Findings from the Finnish 1981 birth cohort study. European Child & Adolescent Psychiatry. 2010;19:823–833. doi: 10.1007/s00787-010-0129-1. [DOI] [PubMed] [Google Scholar]
- Hasin D, Kilcoyne B. Comorbidity of psychiatric and substance use disorders in the United States: Current issues and findings from the NESARC. Current Opinion in Psychiatry. 2012;25:165–171. doi: 10.1097/YCO.0b013e3283523dcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Ikram MK, Ong YT, Cheung CY, Wong TY. Retinal vascular caliber measurements: Clinical significance, current knowledge and future perspectives. Ophthalmologica. 2013;229:125–136. doi: 10.1159/000342158. [DOI] [PubMed] [Google Scholar]
- Insel T. Transforming diagnosis [Web log post] 2013 Apr 29; Retrieved from http://www.nimh.nih.gov/about/director/2013/transforming-diagnosis.shtml.
- Jackson KM, Sartor CE. The natural course of substance use and dependence. In: Sher KJ, editor. Oxford handbook of substance use disorders. New York, NY: Oxford University Press; in press. [Google Scholar]
- Jensen AR. The g factor. New York, NY: Praeger; 1998. [Google Scholar]
- Kapur S, Phillips AG, Insel TR. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Molecular Psychiatry. 2012;17:1174–1179. doi: 10.1038/mp.2012.105. [DOI] [PubMed] [Google Scholar]
- Kell HJ, Lubinski D, Benbow CP. Who rises to the top? Early indicators. Psychological Science. 2013;24:648–659. doi: 10.1177/0956797612457784. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Major depression and generalised anxiety disorder same genes, (partly) different environments— Revisited. British Journal of Psychiatry. 1996;168(Suppl 30):68–75. [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR, Berglund P, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-V. Archives of General Psychiatry. 2003;60:1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Uestuen TB. Development of lifetime comorbidity in the World Health Organization World Mental Health Surveys. Archives of General Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, Hasin DS. Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry. 2012;200:107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kotov R, Chang SW, Fochtmann LJ, Mojtabai R, Carlson GA, Sedler MJ, Bromet EJ. Schizophrenia in the internalizing-externalizing framework: A third dimension? Schizophrenia Bulletin. 2011;37:1168–1178. doi: 10.1093/schbul/sbq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. A dimensional-spectrum model of psychopathology: Progress and opportunities. Archives of General Psychiatry. 2011;68:10–11. doi: 10.1001/archgenpsychiatry.2010.188. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Kuhl EA, Regier DA. DSM-5— The future arrived. JAMA. 2013;309:1691–1692. doi: 10.1001/jama.2013.2298. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121:971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Shankman SA, Gau JM, Klein DN. The prevalence and co-morbidity of subthreshold psychiatric conditions. Psychological Medicine. 2004;34:613–622. doi: 10.1017/s0033291703001466. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P, Yip BH, Bjork C, Pawitan Y, Cannon TD, Sullivan PF, Hultman CM. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: A population-based study. Lancet. 2009;373:234–239. doi: 10.1016/s0140-6736(09)60072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;40:273–288. doi: 10.1017/s0033291709990183. [DOI] [PubMed] [Google Scholar]
- Martel MM. Sexual selection and sex differences in the prevalence of childhood externalizing and adolescent internalizing disorders. Psychological Bulletin. doi: 10.1037/a0032247. in press. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40:899–909. doi: 10.1017/s0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Harrington HL, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalised anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Recurrence in major depression: A conceptual analysis. Psychological Review. 2011;118:655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Lopez AD. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. MPlus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2013. [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry. 2012;169:141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Silva PA. Comorbid mental disorders: Implications for treatment and sample selection. Journal of Abnormal Psychology. 1998;107:305–311. doi: 10.1037//0021-843x.107.2.305. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science. 2011;6:589–609. doi: 10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- Park A, Sher KJ, Todorov AA, Heath AC. Interaction between the DRD4 VNTR polymorphism and proximal and distal environments in alcohol dependence during emerging and young adulthood. Journal of Abnormal Psychology. 2011;120:585–595. doi: 10.1037/a0022648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton N, Aslam T, Macgillivray T, Pattie A, Deary IJ, Dhillon B. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: A rationale based on homology between cerebral and retinal microvasculatures. Journal of Anatomy. 2005;206:319–348. doi: 10.1111/j.1469-7580.2005.00395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rindskopf D, Rose T. Some theory and applications of confimatory 2nd-order factor-analysis. Multivariate Behavioral Research. 1988;23:51–67. doi: 10.1207/s15327906mbr2301_3. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler L, Bucholz KK, Compton W. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University School of Medicine; 1995. [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Cuthbert BN. Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Sartor CE, Grant JD, Bucholz KK, Madden PA, Heath AC, Agrawal A, Lynskey MT. Common genetic contributions to alcohol and cannabis use and dependence symptomatology. Alcoholism: Clinical and Experimental Research. 2010;34:545–554. doi: 10.1111/j.1530-0277.2009.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S, Susser E. The use of well controls: An unhealthy practice in psychiatric research. Psychological Medicine. 2011;41:1127–1131. doi: 10.1017/s0033291710001595. [DOI] [PubMed] [Google Scholar]
- Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Archives of General Psychiatry. 2010;67:712–719. doi: 10.1001/archgenpsychiatry.2010.71. [DOI] [PubMed] [Google Scholar]
- Shalev I, Moffitt TE, Wong TY, Meier MH, Ding J, Cheung CY, Poulton R. Retinal vessel caliber and lifelong neuropsychological functioning: Retinal imaging as an investigative tool for cognitive epidemiology. Psychological Science. 2013;24:1198–1207. doi: 10.1177/0956797612470959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/s0033291706008452. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Craddock N, Kendler K, Lee PH, Neale BM, Numberger JI, Sullivan PF. Identification of risk loci with shared effects on five major psychiatric disorders: A genome-wide analysis. Lancet. 2013;381:1371–1379. doi: 10.1016/s0140-6736(12)62129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sourander A, Multimaki P, Nikolakaros G, Haavisto A, Ristkari T, Helenius H, Almqvist F. Childhood predictors of psychiatric disorders among boys: A prospective community-based follow-up study from age 8 years to early adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:756–767. doi: 10.1097/01.chi.0000164878.79986.2f. [DOI] [PubMed] [Google Scholar]
- Spearman C. “General intelligence,” objectively determined and measured. American Journal of Psychology. 1904;15:201–292. doi: 10.2307/1412107. [DOI] [Google Scholar]
- Stein DF, Fineberg NA, Beinvenu OJ, Denys D, Lochner C, Nestadt G, Phillips KA. Should OCD be classified as an anxiety disorder in DSM-V? Depression and Anxiety. 2010;27:495–506. doi: 10.1002/da.20699. [DOI] [PubMed] [Google Scholar]
- van der Maas HL, Dolan CV, Grasman R, Wicherts JM, Huizenga HM, Raijmakers ME. A dynamical model of general intelligence: The positive manifold of intelligence by mutualism. Psychological Review. 2006;113:842–861. doi: 10.1037/0033-295X.113.4.842. [DOI] [PubMed] [Google Scholar]
- van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: Evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychological Medicine. 2009;39:179–195. doi: 10.1017/s0033291708003814. [DOI] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Bentall RP. Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollebergh WA, ledema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: The NEMESIS study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Wakefield JC. The concept of mental disorder: Diagnostic implications of the harmful dysfunction analysis. World Psychiatry. 2007;6:149–156. [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU. Critical issues in the evaluation of comorbidity of psychiatric disorders. British Journal of Psychiatry. 1996;168:9–16. [PubMed] [Google Scholar]
- Wright AG, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, Slade T. The structure of psychopathology: Toward an expanded quantitative empirical model. Journal of Abnormal Psychology. 2013;122:281–294. doi: 10.1037/a0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung YF, Thissen D, Mcleod LD. On the relationship between the higher-order factor model and the hierarchical factor model. Psychometrika. 1999;64:113–128. doi: 10.1007/bf02294531. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.