Abstract
Cardiovascular magnetic resonance (CMR) allows the nonradiating assessment of coronary arteries; to achieve better image quality cardiorespiratory artefacts should be corrected. Coronary MRA (CMRA) at the moment is indicated only for the detection of abnormal coronary origin, coronary artery ectasia and/or aneurysms (class I indication) and coronary bypass grafts (class II indication). CMRA utilisation for coronary artery disease is not yet part of clinical routine. However, the lack of radiation is of special value for the coronary artery evaluation in children and women. CMRA can assess the proximal part of coronary arteries in almost all cases. The best results have been observed in the evaluation of the left anterior descending and the right coronary artery, while the left circumflex, which is located far away from the coil elements, is frequently imaged with reduced quality, compared to the other two. Different studies detected an increase in wall thickness of the coronaries in patients with type I diabetes and abnormal renal function. Additionally, the non-contrast enhanced T1-weighed images detected the presence of thrombus in acute myocardial infarction. New techniques using delayed gadolinium enhanced imaging promise the direct visualization of inflamed plaques in the coronary arteries. The major advantage of CMR is the potential of an integrated protocol offering assessment of coronary artery anatomy, cardiac function, inflammation and stress perfusion-fibrosis in the same study, providing an individualized clinical profile of patients with heart disease.
Keywords: Coronary angiography, Coronary venous system, Gadolinium, Magnetic resonance imaging
Core tip: Cardiovascular magnetic resonance (CMR) allows the non-radiating assessment of coronary arteries. At the moment it is indicated only to detection of abnormal coronary artery origin, ectasia and/or aneurysms (class I indication) and coronary artery bypass grafts (class II indication). The utilisation of coronary MRA (CMRA) for coronary artery disease diagnosis is not at the moment part of clinical routine. However, due to lack of radiation is particularly useful for children and women. A combined CMR protocol, including CMRA and stress perfusion-fibrosis evaluation may offer a non-invasive assessment of cardiovascular profile in high risk patients.
INTRODUCTION
Coronary artery disease (CAD) with its sequelae including myocardial infarction and heart failure, is the main cause of increased mortality in our days[1,2]. The usual way for CAD assessment is the use of invasive coronary angiography; however, the high incidence of CAD and the queries of invasive assessment necessitate the use of a noninvasive evaluation of coronaries[3,4].
Cardiovascular magnetic resonance (CMR) can provide a combined approach including coronary arteries, cardiac function and stress myocardial perfusion-fibrosis evaluation. Coronary magnetic resonance angiography (CMRA) has been already used for assessment of coronary anatomy and vessels’ wall, providing useful information in CAD[5-7].
In this review we provide an update of clinical applications of CMRA, discussing the current limitations and the challenges for future applications.
INDICATIONS FOR CMRA
The clinical indications of CMRA are at the moment limited only to the detection of abnormal origin of coronary arteries, coronary ectasia and/or aneurysms (class I indication) and coronary bypass grafts (CABG) evaluation (class II indication). The routine application of CMRA for diagnosis of CAD is not at the moment part of clinical practice[8,9].
CORONARY VESSELS ABNORMALITIES AND ANEURYSMS (CLASS I INDICATION)
CMRA assesses precisely the abnormal coronary arteries and the location and dimensions of coronary aneurysms. The larger caliber and the proximal location of the coronary artery aneurysms (CAA) facilitate their imaging. The most important benefit of CMRA is the absence of ionizing radiation, which is of special clinical value for children and women[8,10]. Clinical entities, characterized by ectatic or aneurysmatic coronaries, include Kawasaki disease, autoimmune vasculitis and coronary artery ectasia[11,12].
KAWASAKI DISEASE AND OTHER AUTOIMMUNE VASCULITIS
In Kawasaki disease, CMR can diagnose lesions both in acute and chronic phase. During the acute phase, a complete evaluation of the coronary anatomy, left and right ventricular function, myocardial inflammation and myocardial fibrosis either due to inflammatory process or due to myocardial infarction is essential.
The presence of CAA needs serial evaluation for patients’ risk stratification. Although transthoracic echocardiography is usually sufficient in young children, the visualization of the coronary arteries becomes progressively more difficult as children grow up. According to previous publications, coronary magnetic resonance, using navigator techniques, has an excellent correlation with X-ray coronary angiography using both Pearson coefficient and Bland-Altman analysis and can be used as a reliable alternative for KD patients[13,14]. Recently, the application of free-breathing techniques in children with KD using the whole-heart approach detected successfully not only the abnormalities of coronary lumen, but also the abnormally thickened vessel wall and improved risk stratification and monitoring of therapy[15]. In parallel with coronary assessment, during the same examination, an evaluation of function and wall motion of both ventricles can be also performed using the standard SSFP sequence[16]. However, only anatomic evaluation is not sufficient to successfully risk stratify KD patients. Previous studies in patients with atherosclerotic coronary artery disease proved that maybe a severe anatomic lesion could not provoke severe myocardial ischemia and in contrary, a marginal coronary lesion can induce significant myocardial ischemia[17]. Magnetic resonance (MR) first-pass myocardial perfusion imaging during hyperaemia, due to the vasodilating agent adenosine, demonstrates a high diagnostic performance of MR perfusion imaging for the detection of anatomically defined coronary artery stenoses[18].
Other autoimmune vasculitis that can potentially develop coronary aneurysms include polyarteritis nodosa, microscopic polyangiitis and Wegener granulomatosis[19]. In these diseases the application of coronary MRA with simultaneous assessment of myocardial oedema-fibrosis may reveal disease activity and pathophysiology of heart lesion noninvasively and without radiation[20].
CORONARY ARTERY ECTASIA
Coronary artery ectasia (CAE) represents a form of atherosclerosis, detected in 3%-8% of subjects during X-ray coronary angiography. Sluggish blood flow is produced within the ectatic segments, leading to chest pain in effort and myocardial infarction, independently of the significance of coexisting stenosis. CAE is the dilatation of an artery 1.5 times greater than the normal coronary artery and is assessed in 5% of angiographic and in 0.22%-1.4% of autopsy cases[21-24]. It may involve the entire vessel or be localized in a specific part of the vessel. If it involves the entire vessel, it is called “ectasia”. It is due to atherosclerosis in > 50% of cases. Ectasia coexists with coronary artery disease in the majority of patients. Only 10%-20% of CAE coexist with systemic diseases[25,26], such as scleroderma[27,28], Ehlers-Danlos syndrome[29], different types of antineutrophil cytoplasmic antibody (ANCA)-related vasculitis[19] (Figure 1A), syphilitic aortitis[30] and Kawasaki disease[14] (Figure 1B). In some patients, CAE has a congenital origin[31]. The differentiation between congenital and acquired coronary aneurysms is rather difficult. Acquired CAE should also be differentiated from aneurysms due to different coronary procedures.
Figure 1.
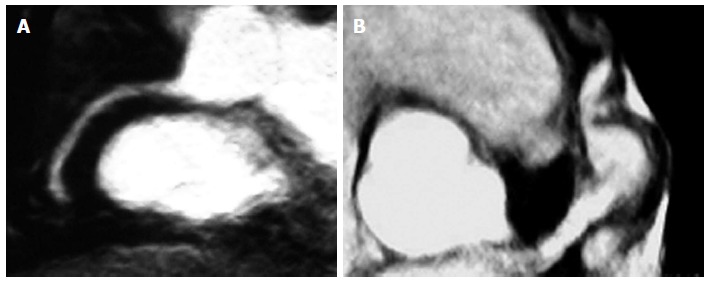
Magnetic resonance angiography. A: Ectatic coronaries in a patient with polyarteritis nodosa, assessed by MRA; B: Aneurysmatic coronaries in a patient with Kawasaki disease, assessed by MRA. MRA: Magnetic resonance angiography.
The correct follow up of ectatic vessels demands repeated angiograms and CMRA offers an excellent alternative for the evaluation of the initial part of left main, left anterior descending and right coronary arteries[32]. CMRA has been already proved a valuable clinical tool for diagnosis of abnormal coronary origin, and is in some cases superior to X-ray coronary angiography; however, it is still under investigation for the assessment of the CAD[32]. Our group proved that CMRA is equal to quantitative coronary angiography for evaluation of ecstatic/aneurysmatic disease. Furthermore, it is a non-invasive, nonradiating technique[4]. Compared with CT, CMRA does not need use of a contrast agent. CMRA can also give additional data about, vessels’ blood flow and stress perfusion-fibrosis pattern[33].
CORONARY BYPASS-GRAFTS (CLASS II INDICATION)
Bypass grafts can be assessed very well by coronary MRA, because they are relatively immobile and have larger diameter compared to coronary arteries. Different imaging ways have been already used, including spin echo[34-37] and gradient echo techniques. The application of contrast agents for better imaging of the blood signal[38,39]. increased the sensitivity to 95%.
However, metallic clips in grafts constitute the commonest limitation of coronary bypass MRA. Coronary MRA can be used at some special centers to detect lesions in bypass grafts[8].
CORONARY MAGNETIC RESONANCE ANGIOGRAPHY FOR ASSESSMENT OF CAD
Coronary MRA assesses the initial part of the coronary arteries in almost 100% of patients, with excellent results acquired for the left anterior descending (LAD) and the right coronary artery (RCA); the left circumflex (LCX), due to its peculiar way, is at a increased distance from the cardiac coil, and therefore its visualization is of inferior quality. According top revious studies, the imaged length for LAD is 50 mm, for RCA is 80 mm and for LCX is 40 mm[40-47]. An excellent agreement between the proximal parts of coronary arteries measured by MRA and by invasive angiography was assessed by previous studies[48].
Unfortunately, the resolution of CMRA remains lower compared with invasive coronary angiography and does not allow the evaluation of stenosis in small coronary arteries. This is the reason of the low specificity documented in a recent international multicenter study[4]; however, CMRA was shown to have a high sensitivity (92%) for the detection of CAD and its diagnostic performance was ameliorated. In a subanalysis of left main or three vessel disease, a sensitivity of 100% and a negative predictive value of 100% was documented. These findings were also supported by smaller single-center studies[40,49-57].
Recently, a meta-analysis compared coronary MRA and multi-slice computed tomography (CT) for assessment of significant CAD[34]. CT was more accurate than MRA and therefore CT was suggested as the preferred non-invasive alternative to X-ray coronary angiography. However, the superiority of CMRA is that it can offer more data about the patient, including cardiac anatomy, function, inflammation, stress perfusion and fibrosis evaluation.
Recently, a multicenter study showed that whole-heart CMRA at 1.5 T can detect significant CAD with high sensitivity (88%) and moderate specificity (72%). Additionally, a negative predictive value (NPV) of 88% indicates that this technique can effectively be used to exclude the presence of significant CAD[58]. We should mention that this NPV reported by this trial is identical to the NPV of the CORE-64 CTA multicenter study[59]. Proving the value of CMRA to rule out CAD in patients with low pre-test probability (< 20%)[60].
Finally, in a direct comparison between CMRA and CTA no significant difference was proved for the detection of CAD between 3 T MR and 64-slice CTA[61]. A comparison between coronary MRA, CTA and invasive coronary angiography (CA) is shown in Table 1.
Table 1.
Comparison between invasive coronary coronary angiography, CTA and magnetic resonance angiography
| CA | CTA | MRA | |
| Noninvasive | No | Yes | Yes |
| Radiation | Yes | Yes | No |
| Nephrotoxicity | Yes | Yes | No |
| Accuracy | +++ | ++ | + |
| Negative predictive value | +++ | +++ | ++ |
| Cost | High | High | High |
| Calcium detection | ± | + | - |
| Anomalous coronaries | +++ | +++ | +++ |
| Ectasia/aneurysm | +++ | +++ | +++ |
| Graft assessment | +++ | +++ | +++ |
| CAD evaluation | +++ | ++ | + |
| Plaque evaluation | +++ | ± | ± |
CA: Coronary angiography; MRA: Magnetic resonance angiography; CAD: Coronary artery disease; CTA: Computed tomography coronary angiography.
CORONARY VESSEL WALL ASSESSMENT
The initial CMR images of the coronary vessel wall were taken using fast spin echo techniques[62,63]. A double inversion recovery preparation was used to take black-blood images improving the contrast between blood and vessel wall[64]. Recently, the double inversion recovery prepulse has been combined with fast gradient echo[65], spiral[66] and radial acquisitions[67].
Various studies documented the capability of vessel wall imaging to detect remodeling of coronary arteries in CAD and increased vessel wall thickness in type I diabetes with abnormal renal function[68,69]. It was also documented by Jansen et al[70] that non-contrast enhanced T1-weighed MR visualized thrombus in acute myocardial infarction.
Recently, new techniques using delayed gadolinium enhancement facilitated the direct assessment of inflamed plaques in the coronary arteries. Clinically used contrast agents showed non-specific uptake in plaques of patients with chronic angina[71]. Acute coronary syndromes[72] and systemic lupus erythematosus[73]. The contrast enhancement by CMR, assessed in patients with stable angina, was associated with calcified or mixed plaques on MSCT, while in ACS it was transient, probably due to inflammatory process.
New contrast agents have been already used in animals and their accumulation in blood was associated with increased endothelial permeability and/or increased neo-vascularization[74]. Additionally, increased accumulation of iron-oxide particles (USPIO) was indicative of increased endothelial permeability and vessel wall inflammation, due to intraplaque macrophages[75,76].
Such molecules have been used as targets for new molecular contrast agents that allowed the assessment of inflammatory indexes, such as intercellular adhesion molecule-1 (ICAM-1), vascular adhesion molecule-1 (VCAM-1) or matrix metalloproteinase (MMP)[77,78]. Furthrmore, thrombi labeling using a fibrin-specific contrast agent[79,80] and evaluation of extracellular matrix remodelling, using targeting elastin is a new promising molecular imaging technique[81,82] for early detection of plaque vulnerability[83].
CONCLUSION
CMR is a non-invasive, non-radiating technique for evaluation of coronary arteries and coronary wall. Its major advantage is the potential of a combined protocol, including coronary arteries, cardiac anatomy, function, inflammation and stress perfusion-fibrosis in the same study in CAD and/or heart failure.
CMRA current indications include: (1) assessment of abnormal coronary arteries, coronary ectasia and/or aneurysm (class I indication); and (2) coronary bypass grafts (class II indication). In the future, it may be used to exclude CAD in selected patients. However, further improvements are needed to support its use for routine assessment of high risk populations.
Footnotes
P- Reviewer: Ueda H S- Editor: Song XX L- Editor: A E- Editor: Wu HL
References
- 1.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, Brindis RG, Douglas PS. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886–895. doi: 10.1056/NEJMoa0907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim WY, Danias PG, Stuber M, Flamm SD, Plein S, Nagel E, Langerak SE, Weber OM, Pedersen EM, Schmidt M, et al. Coronary magnetic resonance angiography for the detection of coronary stenoses. N Engl J Med. 2001;345:1863–1869. doi: 10.1056/NEJMoa010866. [DOI] [PubMed] [Google Scholar]
- 5.Spuentrup E, Botnar RM. Coronary magnetic resonance imaging: visualization of the vessel lumen and the vessel wall and molecular imaging of arteriothrombosis. Eur Radiol. 2006;16:1–14. doi: 10.1007/s00330-005-2886-7. [DOI] [PubMed] [Google Scholar]
- 6.Chiribiri A, Kelle S, Götze S, Kriatselis C, Thouet T, Tangcharoen T, Paetsch I, Schnackenburg B, Fleck E, Nagel E. Visualization of the cardiac venous system using cardiac magnetic resonance. Am J Cardiol. 2008;101:407–412. doi: 10.1016/j.amjcard.2007.08.049. [DOI] [PubMed] [Google Scholar]
- 7.Chiribiri A, Kelle S, Köhler U, Tops LF, Schnackenburg B, Bonamini R, Bax JJ, Fleck E, Nagel E. Magnetic resonance cardiac vein imaging: relation to mitral valve annulus and left circumflex coronary artery. JACC Cardiovasc Imaging. 2008;1:729–738. doi: 10.1016/j.jcmg.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA, Friedrich MG, Ho VB, Jerosch-Herold M, Kramer CM, Manning WJ, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol. 2010;55:2614–2662. doi: 10.1016/j.jacc.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiribiri A, Ishida M, Nagel E, Botnar RM. Coronary imaging with cardiovascular magnetic resonance: Current state of the art. Prog Cardiovasc Dis. 2011;54:240–252. doi: 10.1016/j.pcad.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Chiribiri A, Ishida M, Nagel E, Botnar RM. Coronary imaging with cardiovascular magnetic resonance: current state of the art. Prog Cardiovasc Dis. 2011;54:240–252. doi: 10.1016/j.pcad.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Mavrogeni S, Papadopoulos G, Hussain T, Chiribiri A, Botnar R, Greil GF. The emerging role of cardiovascular magnetic resonance in the evaluation of Kawasaki disease. Int J Cardiovasc Imaging. 2013;29:1787–1798. doi: 10.1007/s10554-013-0276-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mavrogeni S. Coronary artery ectasia: from diagnosis to treatment. Hellenic J Cardiol. 2010;51:158–163. [PubMed] [Google Scholar]
- 13.Mavrogeni S, Papadopoulos G, Douskou M, Kaklis S, Seimenis I, Baras P, Nikolaidou P, Bakoula C, Karanasios E, Manginas A, et al. Magnetic resonance angiography is equivalent to X-ray coronary angiography for the evaluation of coronary arteries in Kawasaki disease. J Am Coll Cardiol. 2004;43:649–652. doi: 10.1016/j.jacc.2003.08.052. [DOI] [PubMed] [Google Scholar]
- 14.Greil GF, Stuber M, Botnar RM, Kissinger KV, Geva T, Newburger JW, Manning WJ, Powell AJ. Coronary magnetic resonance angiography in adolescents and young adults with kawasaki disease. Circulation. 2002;105:908–911. doi: 10.1161/hc0802.105563. [DOI] [PubMed] [Google Scholar]
- 15.Greil GF, Seeger A, Miller S, Claussen CD, Hofbeck M, Botnar RM, Sieverding L. Coronary magnetic resonance angiography and vessel wall imaging in children with Kawasaki disease. Pediatr Radiol. 2007;37:666–673. doi: 10.1007/s00247-007-0498-x. [DOI] [PubMed] [Google Scholar]
- 16.Mavrogeni S, Papadopoulos G, Douskou M, Kaklis S, Seimenis I, Varlamis G, Karanasios E, Krikos X, Giannoulia A, Cokkinos DV. Magnetic resonance angiography, function and viability evaluation in patients with Kawasaki disease. J Cardiovasc Magn Reson. 2006;8:493–498. doi: 10.1080/10976640600604773. [DOI] [PubMed] [Google Scholar]
- 17.Doesch C, Seeger A, Doering J, Herdeg C, Burgstahler C, Claussen CD, Gawaz M, Miller S, May AE. Risk stratification by adenosine stress cardiac magnetic resonance in patients with coronary artery stenoses of intermediate angiographic severity. JACC Cardiovasc Imaging. 2009;2:424–433. doi: 10.1016/j.jcmg.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 18.Giang TH, Nanz D, Coulden R, Friedrich M, Graves M, Al-Saadi N, Lüscher TF, von Schulthess GK, Schwitter J. Detection of coronary artery disease by magnetic resonance myocardial perfusion imaging with various contrast medium doses: first European multi-centre experience. Eur Heart J. 2004;25:1657–1665. doi: 10.1016/j.ehj.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 19.Mavrogeni S, Manoussakis MN, Karagiorga TC, Douskou M, Panagiotakos D, Bournia V, Cokkinos DV, Moutsopoulos HM. Detection of coronary artery lesions and myocardial necrosis by magnetic resonance in systemic necrotizing vasculitides. Arthritis Rheum. 2009;61:1121–1129. doi: 10.1002/art.24695. [DOI] [PubMed] [Google Scholar]
- 20.Mavrogeni S, Sfikakis PP, Gialafos E, Bratis K, Karabela G, Stavropoulos E, Spiliotis G, Sfendouraki E, Panopoulos S, Bournia V, et al. Cardiac tissue characterization and the diagnostic value of cardiovascular magnetic resonance in systemic connective tissue diseases. Arthritis Care Res (Hoboken) 2014;66:104–112. doi: 10.1002/acr.22181. [DOI] [PubMed] [Google Scholar]
- 21.Hartnell GG, Parnell BM, Pridie RB. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J. 1985;54:392–395. doi: 10.1136/hrt.54.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Markis JE, Joffe CD, Cohn PF, Feen DJ, Herman MV, Gorlin R. Clinical significance of coronary arterial ectasia. Am J Cardiol. 1976;37:217–222. doi: 10.1016/0002-9149(76)90315-5. [DOI] [PubMed] [Google Scholar]
- 23.Oliveros RA, Falsetti HL, Carroll RJ, Heinle RA, Ryan GF. Atherosclerotic coronary artery aneurysm. Report of five cases and review of literature. Arch Intern Med. 1974;134:1072–1076. doi: 10.1001/archinte.134.6.1072. [DOI] [PubMed] [Google Scholar]
- 24.Swaye PS, Fisher LD, Litwin P, Vignola PA, Judkins MP, Kemp HG, Mudd JG, Gosselin AJ. Aneurysmal coronary artery disease. Circulation. 1983;67:134–138. doi: 10.1161/01.cir.67.1.134. [DOI] [PubMed] [Google Scholar]
- 25.Falsetti HL, Carrol RJ. Coronary artery aneurysm. A review of the literature with a report of 11 new cases. Chest. 1976;69:630–636. doi: 10.1378/chest.69.5.630. [DOI] [PubMed] [Google Scholar]
- 26.Befeler B, Aranda MJ, Embi A, Mullin FL, El-Sherif N, Lazzara R. Coronary artery aneurysms: study of the etiology, clinical course and effect on left ventricular function and prognosis. Am J Med. 1977;62:597–607. doi: 10.1016/0002-9343(77)90423-5. [DOI] [PubMed] [Google Scholar]
- 27.Chaithiraphan S, Goldberg E, O’Reilly M, Jootar P. Multiple aneurysms of coronary artery in sclerodermal heart disease. Angiology. 1973;24:86–93. doi: 10.1177/000331977302400204. [DOI] [PubMed] [Google Scholar]
- 28.Tarek el-G, Yasser AE, Gheita T. Coronary angiographic findings in asymptomatic systemic sclerosis. Clin Rheumatol. 2006;25:487–490. doi: 10.1007/s10067-005-0073-5. [DOI] [PubMed] [Google Scholar]
- 29.Imahori S, Bannerman RM, Graf CJ, Brennan JC. Ehlers-Danlos syndrome with multiple arterial lesions. Am J Med. 1969;47:967–977. doi: 10.1016/0002-9343(69)90210-1. [DOI] [PubMed] [Google Scholar]
- 30.Davidson A, Eshaghpour E, Young N, Mintz GS. Late thrombosis of a coronary artery mycotic aneurysm. Am Heart J. 1991;121:1549–1550. doi: 10.1016/0002-8703(91)90168-h. [DOI] [PubMed] [Google Scholar]
- 31.Cohen P, O’Gara PT. Coronary artery aneurysms: a review of the natural history, pathophysiology, and management. Cardiol Rev. 2008;16:301–304. doi: 10.1097/CRD.0b013e3181852659. [DOI] [PubMed] [Google Scholar]
- 32.Bluemke DA, Achenbach S, Budoff M, Gerber TC, Gersh B, Hillis LD, Hundley WG, Manning WJ, Printz BF, Stuber M, et al. Noninvasive coronary artery imaging: magnetic resonance angiography and multidetector computed tomography angiography: a scientific statement from the american heart association committee on cardiovascular imaging and intervention of the council on cardiovascular radiology and intervention, and the councils on clinical cardiology and cardiovascular disease in the young. Circulation. 2008;118:586–606. doi: 10.1161/CIRCULATIONAHA.108.189695. [DOI] [PubMed] [Google Scholar]
- 33.Mavrogeni SI, Manginas A, Papadakis E, Foussas S, Douskou M, Baras P, Seimenis I, Cokkinos DV. Correlation between magnetic resonance angiography (MRA) and quantitative coronary angiography (QCA) in ectatic coronary vessels. J Cardiovasc Magn Reson. 2004;6:17–23. doi: 10.1081/jcmr-120027801. [DOI] [PubMed] [Google Scholar]
- 34.Galjee MA, van Rossum AC, Doesburg T, van Eenige MJ, Visser CA. Value of magnetic resonance imaging in assessing patency and function of coronary artery bypass grafts. An angiographically controlled study. Circulation. 1996;93:660–666. doi: 10.1161/01.cir.93.4.660. [DOI] [PubMed] [Google Scholar]
- 35.Jenkins JP, Love HG, Foster CJ, Isherwood I, Rowlands DJ. Detection of coronary artery bypass graft patency as assessed by magnetic resonance imaging. Br J Radiol. 1988;61:2–4. doi: 10.1259/0007-1285-61-721-2. [DOI] [PubMed] [Google Scholar]
- 36.Rubinstein RI, Askenase AD, Thickman D, Feldman MS, Agarwal JB, Helfant RH. Magnetic resonance imaging to evaluate patency of aortocoronary bypass grafts. Circulation. 1987;76:786–791. doi: 10.1161/01.cir.76.4.786. [DOI] [PubMed] [Google Scholar]
- 37.White RD, Caputo GR, Mark AS, Modin GW, Higgins CB. Coronary artery bypass graft patency: noninvasive evaluation with MR imaging. Radiology. 1987;164:681–686. doi: 10.1148/radiology.164.3.3497409. [DOI] [PubMed] [Google Scholar]
- 38.Vrachliotis TG, Bis KG, Aliabadi D, Shetty AN, Safian R, Simonetti O. Contrast-enhanced breath-hold MR angiography for evaluating patency of coronary artery bypass grafts. AJR Am J Roentgenol. 1997;168:1073–1080. doi: 10.2214/ajr.168.4.9124118. [DOI] [PubMed] [Google Scholar]
- 39.Wintersperger BJ, von Smekal A, Engelmann MG, Knez A, Penzkofer HV, Laub G, Reiser M. [Contrast media enhanced magnetic resonance angiography for determining patency of a coronary bypass. A comparison with coronary angiography] Rofo. 1997;167:572–578. doi: 10.1055/s-2007-1015585. [DOI] [PubMed] [Google Scholar]
- 40.Botnar RM, Stuber M, Danias PG, Kissinger KV, Manning WJ. Improved coronary artery definition with T2-weighted, free-breathing, three-dimensional coronary MRA. Circulation. 1999;99:3139–3148. doi: 10.1161/01.cir.99.24.3139. [DOI] [PubMed] [Google Scholar]
- 41.Hofman MB, Paschal CB, Li D, Haacke EM, van Rossum AC, Sprenger M. MRI of coronary arteries: 2D breath-hold vs 3D respiratory-gated acquisition. J Comput Assist Tomogr. 1995;19:56–62. [PubMed] [Google Scholar]
- 42.Lobbes MB, Miserus RJ, Heeneman S, Passos VL, Mutsaers PH, Debernardi N, Misselwitz B, Post M, Daemen MJ, van Engelshoven JM, et al. Atherosclerosis: contrast-enhanced MR imaging of vessel wall in rabbit model--comparison of gadofosveset and gadopentetate dimeglumine. Radiology. 2009;250:682–691. doi: 10.1148/radiol.2503080875. [DOI] [PubMed] [Google Scholar]
- 43.Manning WJ, Li W, Boyle NG, Edelman RR. Fat-suppressed breath-hold magnetic resonance coronary angiography. Circulation. 1993;87:94–104. doi: 10.1161/01.cir.87.1.94. [DOI] [PubMed] [Google Scholar]
- 44.Paschal CB, Haacke EM, Adler LP. Three-dimensional MR imaging of the coronary arteries: preliminary clinical experience. J Magn Reson Imaging. 1993;3:491–500. doi: 10.1002/jmri.1880030311. [DOI] [PubMed] [Google Scholar]
- 45.Post JC, van Rossum AC, Hofman MB, Valk J, Visser CA. Three-dimensional respiratory-gated MR angiography of coronary arteries: comparison with conventional coronary angiography. AJR Am J Roentgenol. 1996;166:1399–1404. doi: 10.2214/ajr.166.6.8633453. [DOI] [PubMed] [Google Scholar]
- 46.Stuber M, Botnar RM, Danias PG, Sodickson DK, Kissinger KV, Van Cauteren M, De Becker J, Manning WJ. Double-oblique free-breathing high resolution three-dimensional coronary magnetic resonance angiography. J Am Coll Cardiol. 1999;34:524–531. doi: 10.1016/s0735-1097(99)00223-5. [DOI] [PubMed] [Google Scholar]
- 47.Scheidegger MB, Müller R, Boesiger P. Magnetic resonance angiography: methods and its applications to the coronary arteries. Technol Health Care. 1994;2:255–265. [PubMed] [Google Scholar]
- 48.Bogaert J, Kuzo R, Dymarkowski S, Beckers R, Piessens J, Rademakers FE. Coronary artery imaging with real-time navigator three-dimensional turbo-field-echo MR coronary angiography: initial experience. Radiology. 2003;226:707–716. doi: 10.1148/radiol.2263011750. [DOI] [PubMed] [Google Scholar]
- 49.Dewey M, Teige F, Schnapauff D, Laule M, Borges AC, Rutsch W, Hamm B, Taupitz M. Combination of free-breathing and breathhold steady-state free precession magnetic resonance angiography for detection of coronary artery stenoses. J Magn Reson Imaging. 2006;23:674–681. doi: 10.1002/jmri.20568. [DOI] [PubMed] [Google Scholar]
- 50.Jahnke C, Paetsch I, Nehrke K, Schnackenburg B, Gebker R, Fleck E, Nagel E. Rapid and complete coronary arterial tree visualization with magnetic resonance imaging: feasibility and diagnostic performance. Eur Heart J. 2005;26:2313–2319. doi: 10.1093/eurheartj/ehi391. [DOI] [PubMed] [Google Scholar]
- 51.Jahnke C, Paetsch I, Schnackenburg B, Bornstedt A, Gebker R, Fleck E, Nagel E. Coronary MR angiography with steady-state free precession: individually adapted breath-hold technique versus free-breathing technique. Radiology. 2004;232:669–676. doi: 10.1148/radiol.2323031225. [DOI] [PubMed] [Google Scholar]
- 52.Maintz D, Aepfelbacher FC, Kissinger KV, Botnar RM, Danias PG, Heindel W, Manning WJ, Stuber M. Coronary MR angiography: comparison of quantitative and qualitative data from four techniques. AJR Am J Roentgenol. 2004;182:515–521. doi: 10.2214/ajr.182.2.1820515. [DOI] [PubMed] [Google Scholar]
- 53.Manning WJ, Li W, Edelman RR. A preliminary report comparing magnetic resonance coronary angiography with conventional angiography. N Engl J Med. 1993;328:828–832. doi: 10.1056/NEJM199303253281202. [DOI] [PubMed] [Google Scholar]
- 54.Ozgun M, Hoffmeier A, Kouwenhoven M, Botnar RM, Stuber M, Scheld HH, Manning WJ, Heindel W, Maintz D. Comparison of 3D segmented gradient-echo and steady-state free precession coronary MRI sequences in patients with coronary artery disease. AJR Am J Roentgenol. 2005;185:103–109. doi: 10.2214/ajr.185.1.01850103. [DOI] [PubMed] [Google Scholar]
- 55.Sakuma H, Ichikawa Y, Chino S, Hirano T, Makino K, Takeda K. Detection of coronary artery stenosis with whole-heart coronary magnetic resonance angiography. J Am Coll Cardiol. 2006;48:1946–1950. doi: 10.1016/j.jacc.2006.07.055. [DOI] [PubMed] [Google Scholar]
- 56.Sakuma H, Ichikawa Y, Suzawa N, Hirano T, Makino K, Koyama N, Van Cauteren M, Takeda K. Assessment of coronary arteries with total study time of less than 30 minutes by using whole-heart coronary MR angiography. Radiology. 2005;237:316–321. doi: 10.1148/radiol.2371040830. [DOI] [PubMed] [Google Scholar]
- 57.Schuetz GM, Zacharopoulou NM, Schlattmann P, Dewey M. Meta-analysis: noninvasive coronary angiography using computed tomography versus magnetic resonance imaging. Ann Intern Med. 2010;152:167–177. doi: 10.7326/0003-4819-152-3-201002020-00008. [DOI] [PubMed] [Google Scholar]
- 58.Kato S, Kitagawa K, Ishida N, Ishida M, Nagata M, Ichikawa Y, Katahira K, Matsumoto Y, Seo K, Ochiai R, et al. Assessment of coronary artery disease using magnetic resonance coronary angiography: a national multicenter trial. J Am Coll Cardiol. 2010;56:983–991. doi: 10.1016/j.jacc.2010.01.071. [DOI] [PubMed] [Google Scholar]
- 59.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, Paul N, Clouse ME, Shapiro EP, Hoe J, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–2336. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 60.Nagel E. Magnetic resonance coronary angiography: the condemned live longer. J Am Coll Cardiol. 2010;56:992–994. doi: 10.1016/j.jacc.2010.02.069. [DOI] [PubMed] [Google Scholar]
- 61.Hamdan A, Asbach P, Wellnhofer E, Klein C, Gebker R, Kelle S, Kilian H, Huppertz A, Fleck E. A prospective study for comparison of MR and CT imaging for detection of coronary artery stenosis. JACC Cardiovasc Imaging. 2011;4:50–61. doi: 10.1016/j.jcmg.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 62.Botnar RM, Stuber M, Kissinger KV, Kim WY, Spuentrup E, Manning WJ. Noninvasive coronary vessel wall and plaque imaging with magnetic resonance imaging. Circulation. 2000;102:2582–2587. doi: 10.1161/01.cir.102.21.2582. [DOI] [PubMed] [Google Scholar]
- 63.Fayad ZA, Fuster V, Fallon JT, Jayasundera T, Worthley SG, Helft G, Aguinaldo JG, Badimon JJ, Sharma SK. Noninvasive in vivo human coronary artery lumen and wall imaging using black-blood magnetic resonance imaging. Circulation. 2000;102:506–510. doi: 10.1161/01.cir.102.5.506. [DOI] [PubMed] [Google Scholar]
- 64.Edelman RR, Chien D, Kim D. Fast selective black blood MR imaging. Radiology. 1991;181:655–660. doi: 10.1148/radiology.181.3.1947077. [DOI] [PubMed] [Google Scholar]
- 65.Botnar RM, Stuber M, Lamerichs R, Smink J, Fischer SE, Harvey P, Manning WJ. Initial experiences with in vivo right coronary artery human MR vessel wall imaging at 3 tesla. J Cardiovasc Magn Reson. 2003;5:589–594. doi: 10.1081/jcmr-120025232. [DOI] [PubMed] [Google Scholar]
- 66.Botnar RM, Kim WY, Börnert P, Stuber M, Spuentrup E, Manning WJ. 3D coronary vessel wall imaging utilizing a local inversion technique with spiral image acquisition. Magn Reson Med. 2001;46:848–854. doi: 10.1002/mrm.1268. [DOI] [PubMed] [Google Scholar]
- 67.Katoh M, Spuentrup E, Buecker A, Schaeffter T, Stuber M, Günther RW, Botnar RM. MRI of coronary vessel walls using radial k-space sampling and steady-state free precession imaging. AJR Am J Roentgenol. 2006;186:S401–S406. doi: 10.2214/AJR.04.1864. [DOI] [PubMed] [Google Scholar]
- 68.Kim WY, Stuber M, Börnert P, Kissinger KV, Manning WJ, Botnar RM. Three-dimensional black-blood cardiac magnetic resonance coronary vessel wall imaging detects positive arterial remodeling in patients with nonsignificant coronary artery disease. Circulation. 2002;106:296–299. doi: 10.1161/01.cir.0000025629.85631.1e. [DOI] [PubMed] [Google Scholar]
- 69.Kim WY, Astrup AS, Stuber M, Tarnow L, Falk E, Botnar RM, Simonsen C, Pietraszek L, Hansen PR, Manning WJ, et al. Subclinical coronary and aortic atherosclerosis detected by magnetic resonance imaging in type 1 diabetes with and without diabetic nephropathy. Circulation. 2007;115:228–235. doi: 10.1161/CIRCULATIONAHA.106.633339. [DOI] [PubMed] [Google Scholar]
- 70.Jansen CH, Perera D, Makowski MR, Wiethoff AJ, Phinikaridou A, Razavi RM, Marber MS, Greil GF, Nagel E, Maintz D, et al. Detection of intracoronary thrombus by magnetic resonance imaging in patients with acute myocardial infarction. Circulation. 2011;124:416–424. doi: 10.1161/CIRCULATIONAHA.110.965442. [DOI] [PubMed] [Google Scholar]
- 71.Yeon SB, Sabir A, Clouse M, Martinezclark PO, Peters DC, Hauser TH, Gibson CM, Nezafat R, Maintz D, Manning WJ, et al. Delayed-enhancement cardiovascular magnetic resonance coronary artery wall imaging: comparison with multislice computed tomography and quantitative coronary angiography. J Am Coll Cardiol. 2007;50:441–447. doi: 10.1016/j.jacc.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 72.Ibrahim T, Makowski MR, Jankauskas A, Maintz D, Karch M, Schachoff S, Manning WJ, Schömig A, Schwaiger M, Botnar RM. Serial contrast-enhanced cardiac magnetic resonance imaging demonstrates regression of hyperenhancement within the coronary artery wall in patients after acute myocardial infarction. JACC Cardiovasc Imaging. 2009;2:580–588. doi: 10.1016/j.jcmg.2008.12.029. [DOI] [PubMed] [Google Scholar]
- 73.Puntmann VO, D’Cruz D, Taylor PC, Hussain T, Indermuhle A, Butzbach B, Botnar R, Nagel E. Contrast enhancement imaging in coronary arteries in SLE. JACC Cardiovasc Imaging. 2012;5:962–964. doi: 10.1016/j.jcmg.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 74.Phinikaridou A, Andia ME, Protti A, Indermuehle A, Shah A, Smith A, Warley A, Botnar RM. Noninvasive magnetic resonance imaging evaluation of endothelial permeability in murine atherosclerosis using an albumin-binding contrast agent. Circulation. 2012;126:707–719. doi: 10.1161/CIRCULATIONAHA.112.092098. [DOI] [PubMed] [Google Scholar]
- 75.Kooi ME, Cappendijk VC, Cleutjens KB, Kessels AG, Kitslaar PJ, Borgers M, Frederik PM, Daemen MJ, van Engelshoven JM. Accumulation of ultrasmall superparamagnetic particles of iron oxide in human atherosclerotic plaques can be detected by in vivo magnetic resonance imaging. Circulation. 2003;107:2453–2458. doi: 10.1161/01.CIR.0000068315.98705.CC. [DOI] [PubMed] [Google Scholar]
- 76.Tang TY, Howarth SP, Miller SR, Graves MJ, Patterson AJ, U-King-Im JM, Li ZY, Walsh SR, Brown AP, Kirkpatrick PJ, et al. The ATHEROMA (Atorvastatin Therapy: Effects on Reduction of Macrophage Activity) Study. Evaluation using ultrasmall superparamagnetic iron oxide-enhanced magnetic resonance imaging in carotid disease. J Am Coll Cardiol. 2009;53:2039–2050. doi: 10.1016/j.jacc.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 77.Nahrendorf M, Jaffer FA, Kelly KA, Sosnovik DE, Aikawa E, Libby P, Weissleder R. Noninvasive vascular cell adhesion molecule-1 imaging identifies inflammatory activation of cells in atherosclerosis. Circulation. 2006;114:1504–1511. doi: 10.1161/CIRCULATIONAHA.106.646380. [DOI] [PubMed] [Google Scholar]
- 78.Nahrendorf M, Keliher E, Panizzi P, Zhang H, Hembrador S, Figueiredo JL, Aikawa E, Kelly K, Libby P, Weissleder R. 18F-4V for PET-CT imaging of VCAM-1 expression in atherosclerosis. JACC Cardiovasc Imaging. 2009;2:1213–1222. doi: 10.1016/j.jcmg.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Botnar RM, Buecker A, Wiethoff AJ, Parsons EC, Katoh M, Katsimaglis G, Weisskoff RM, Lauffer RB, Graham PB, Gunther RW, et al. In vivo magnetic resonance imaging of coronary thrombosis using a fibrin-binding molecular magnetic resonance contrast agent. Circulation. 2004;110:1463–1466. doi: 10.1161/01.CIR.0000134960.31304.87. [DOI] [PubMed] [Google Scholar]
- 80.Botnar RM, Perez AS, Witte S, Wiethoff AJ, Laredo J, Hamilton J, Quist W, Parsons EC, Vaidya A, Kolodziej A, et al. In vivo molecular imaging of acute and subacute thrombosis using a fibrin-binding magnetic resonance imaging contrast agent. Circulation. 2004;109:2023–2029. doi: 10.1161/01.CIR.0000127034.50006.C0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Makowski MR, Wiethoff AJ, Blume U, Cuello F, Warley A, Jansen CH, Nagel E, Razavi R, Onthank DC, Cesati RR, et al. Assessment of atherosclerotic plaque burden with an elastin-specific magnetic resonance contrast agent. Nat Med. 2011;17:383–388. doi: 10.1038/nm.2310. [DOI] [PubMed] [Google Scholar]
- 82.von Bary C, Makowski M, Preissel A, Keithahn A, Warley A, Spuentrup E, Buecker A, Lazewatsky J, Cesati R, Onthank D, et al. MRI of coronary wall remodeling in a swine model of coronary injury using an elastin-binding contrast agent. Circ Cardiovasc Imaging. 2011;4:147–155. doi: 10.1161/CIRCIMAGING.109.895607. [DOI] [PubMed] [Google Scholar]
- 83.Chiribiri A, Botnar RM, Nagel E. Magnetic resonance coronary angiography: where are we today? Curr Cardiol Rep. 2013;15:328. doi: 10.1007/s11886-012-0328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


