Abstract
Allergy to laboratory animals is a well known occupational hazard and remains a health concern for individuals in contact with lab animals. This study evaluates the prevalence of allergy symptoms among medical researchers exposed to laboratory animals. We analyzed data from a cross-sectional survey, involving subjects (n=169, 21–59 yr), working in Kochi Medical School, Japan. They were asked to fill out a questionnaire to evaluate symptoms related to contact with laboratory animals. The overall response rate was 86.2%. The prevalence of laboratory animal allergy was 17.6%. The symptoms most reported were allergic rhino-conjunctivitis and asthma. A small number of the subjects received education on the allergy issue and 62.5% of subjects with an allergy to laboratory animals claimed to have atopy. Protection from animal allergens should be a high priority for institutions using lab animals; providing continuous education to animal handlers would be meaningful to reduce and control exposure.
Keywords: Allergy, Laboratory animals, Laboratory animal allergy, Medical researchers, Occupational allergy
Introduction
Laboratory animal allergy (LAA) is a type of occupational allergic disease common among people engaged in the care or use of lab animals1,2,3). Its prevalence is high, between 11% and 44%, and symptoms may adversely affect the life and careers up to one third of animal experimenters4). Symptoms include rhino-conjunctivitis, skin rashes and asthma-related symptoms of which the latter constitute the most severe possible consequences5).
Reports on the prevalence of LAA vary considerably since both reported symptoms and in vivo evidence of immunoglobulin E are independently used for the diagnosis. Because of inconsistencies in the methods of diagnosis, a comparison of findings from different studies is not easy6).
Rats, mice, rabbits, dogs, guinea pigs, hamsters, cats, and monkeys are the most common animal species handled in Japanese research facilities. In 1992, the prevalence of LAA was 23.1% in Japan7). Based on the prevention approach, exposure to animal allergens is the most well-known risk factor that predisposes subjects to the development of LAA4); other risk factors for animal allergen sensitization include atopic status, tobacco smoking and pre-existing allergies to pets5, 8, 9). The most reported routes of exposure are inhalation, followed by skin contact and eye exposure10).
Much has been done in regard to the risk assessment and management of LAA, however, new cases continue to appear; from the standpoint of medical cost, absenteeism, and loss of efficiency among laboratory animal handlers, LAA is still a serious health concern11). To the best of our knowledge, there is no recent available data about LAA in our research facility. In these conditions, we felt that assessment of the situation in our institution in order to prevent LAA would be a worthwhile public-health goal.
This study was designed to evaluate the prevalence of LAA among medical researchers and to assess factors predisposing them to sensitization and therefore, contribute to prevent disabling diseases.
Materials and Methods
Setting and survey data collection
It was a cross-sectional study where factors related to LAA were investigated among medical researchers (research scientists, physicians and teachers) between November 2008 and December 2008 in Kochi Medical School, Japan.
There were 369 subjects conducting medical research in Kochi Medical School, they were all invited to participate in this study. We did not use any predefined sampling method that would give an epidemiologically valid representation of the study sample, and being a medical researcher in Kochi Medical School was the inclusion criteria.
A total of 196 subjects agreed to fill out a self-administered questionnaire, however, 27 of them (13.8%) did not return the completed questionnaire.
The questionnaire assessed LAA related symptoms, other allergic diseases, past history and family history of allergic diseases, job description, experience of working with lab animals, time spent with lab animals or their waste, use of personal protective equipment and its effects, and demographic characteristics-including age, sex, education and smoking- and other work-related aspects. They were also asked to report information about domestic pet proprietorship.
We defined LAA subjects as subjects who had subjective symptoms related to contact with laboratory animals, such as allergic rhinitis, bronchial asthma, contact dermatitis and allergic conjunctivitis12). These symptoms were classified as eye symptoms (eyes itching, lacrimation), nose symptoms (sneezing, rhinorrhea, nasal congestion), skin symptoms (itching, urticaria) and asthma symptoms (coughing, wheezing, dyspnea and expectoration). Animal handlers were defined as the researchers who were in contact with laboratory animals or their waste.
Ethical approval for this study was obtained from the Research Ethics Committee of Kochi Medical School and the study was carried out in accordance with the Helsinki Declaration.
Statistical Analysis
The data were analyzed using Statistical Package for the Social Sciences (SPSS) version 16.0 for Windows program; and a significance criterion of probability value of p<0.05 was used. The χ2 test and Student’s t-test were performed respectively to evaluate differences in categorical variables and continuous variables. Odds ratios and 95% confidence intervals were calculated in order to determine the relationship between the presence of LAA and risk factors. Multiple logistic regression analysis was carried out to determine the relationship between the presence of LAA and studied parameters.
Results
Out of the 196 subjects sampled, 169 returned the filled questionnaire (Response rate 86.2%). The sample was skewed towards animal handlers, a total of 136 (80.5%), of which 24 (17.6%) reported at least one or more LAA-related symptoms. General characterstics of the subjects are displayed in Table 1. The study included more males (68.6%) than females (31.4%) and the mean age was 36.4 ± 9.7 yr old (range 21−59 yr), with non-animal handlers being younger than subjects handling animals (37.4 ± 10.0 vs. 32.4 ± 7.3 yr; p=0.004). Both subjects with LAA and those without LAA were close in age. A small number of subjects were smokers and the smoking behaviors were the same in both symptomatic and asymptomatic researchers (Table 1).
Table 1. Characteristics of the subjects (n=169).
| Variable | Subjects with LAA | Subjects without LAA | Non animal handlers | p value | ||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | * | # | † | |
| Total | 24 (14.2) | 112 (66.3) | 33 (19.5) | |||
| Age in year, mean (range) | 37.1 ± 9.7 (23–56) | 37.4 ± 10.2 (21–59) | 32.4 ± 7.3 (21–46) | 0.4477 | 0.0207 | 0.004 |
| Gender | ||||||
| Male | 17 (10.0) | 79 (46.7) | 20 (12.0) | 0.977 | 0.424 | 0.281 |
| Female | 7 (4.1) | 33 (19.5) | 13 (7.7) | |||
| Smoking habit | ||||||
| Current smoker | 4 (2.4) | 15 (9.0) | 5 (3.0) | 0.675 | 0.877 | 0.797 |
| Non-smoker | 20 (11.8) | 97 (57.4) | 28 (16.6) | |||
| Education on allergenic material | 4 (2.4) | 29 (17.2) | _ | 0.644 | _ | _ |
| History of allergy | ||||||
| Personal history of allergy | 15 (9.0) | 29 (17.2) | 10 (6.0) | 0.001 | 0.016 | 0.555 |
| No personal history of allergy | 8 (4.7) | 79 (46.7) | 21 (12.4) | |||
| Family history of allergy | 16 (9.5) | 42 (25.0) | 9 (5.3) | 0.006 | 0.003 | 0.332 |
| No family history of allergy | 7 (4.1) | 67 (39.7) | 22 (13.0) | |||
| Exposure hour/week, median (range) | 6 (1–45) | 5 (1–35) | _ | 0.023 | _ | _ |
| Working experience with lab animals | ||||||
| 0–5 | 13 (7.7) | 65 (38.4) | _ | 0.623 | _ | _ |
| >5 | 11 (6.5) | 44 (26.0) | _ | |||
| Latency period (yr) | ||||||
| 0–3 | 12 (7.1) | _ | _ | _ | _ | _ |
| 4–8 | 6 (3.6) | _ | _ | _ | _ | _ |
| 9–14 | 3 (1.8) | _ | _ | _ | _ | _ |
| LAA related symptoms | ||||||
| Nose/eye symptoms | 19 (11.2) | _ | _ | _ | _ | _ |
| Skin symptoms | 11 (6.5) | _ | _ | _ | _ | _ |
| Asthma symptoms | 5 (3.0) | _ | _ | _ | ||
| Use of personal protective equipments | ||||||
| Mask | 21 (12.4) | 92 (54.4) | _ | 0.525 | _ | _ |
| Gloves | 21 (12.4) | 110 (65) | _ | 0.011 | _ | _ |
| Clothing | 15 (9.0) | 50 | _ | 0.112 | _ | _ |
| Head covering | 2 (1.2) | 4 (2.4) | _ | 0.303 | _ | _ |
| Eye protectors | 1 (0.6) | 2 (1.2) | _ | 0.471 | _ | _ |
* Subjects with LAA vs. without LAA. # Subjects with LAA vs. Non animal handlers. † Subjects without LAA vs. Non animal handlers. There are missing data, so some total may not add up. LAA: Laboratory animal allergy.
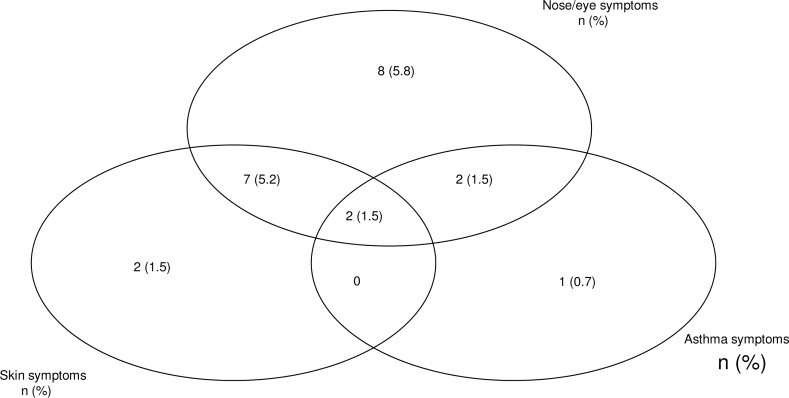
The average weekly time of work with animals was 6 h (range, 1–45 h) for LAA subjects, and 5 h for non LAA subjects (range, 1–35). In this survey, we found a positive correlation between the development of LAA and the length of handling animals per day (OR=0.4; 95% CI= 0.2–0.5; p=0.035). Subjects with LAA who had long hours of exposure per week (83.3%) were likely to report symptoms more frequently than those who were less exposed per week (p=0.04). Ninety-one subjects (53.9%) used animals in their routine experiments, and 45 (26.6%) had done so in the past. In the LAA group, nasal and eye symptoms were the most reported symptoms (14.0%) followed by skin symptoms (8.2%) and asthmatic symptoms (3.7%) (Fig. 1).
Fig. 1.
Prevalence of reported LAA symptoms among 136 medical researchers working with laboratory animals. n= number of subject with laboratory animal allergy.
In most of the cases nose and eye symptoms were associated. Among the five subjects with asthmatic symptoms four subjects had rhino-conjuntivitis.
Our survey showed that affected subjects handling mice and rats had the highest prevalence of LAA (19.3%), followed by rabbits (16.3%) guinea pigs (9.7%), and dogs (3.2%). Mice and rats were the animals most used, as shown in Table 2.
Table 2. Prevalence of LAA symptoms by animal species handled (n=136).
| Species | Number of handlers, n (%) | Prevalence of LAA (%) |
|---|---|---|
| Mouse | 119 (87.5) | 19.3 |
| Rat | 88 (64.7) | 19.3 |
| Rabbit | 69 (36.0) | 16.3 |
| Guinea pig | 22 (16.2) | 9.7 |
| Dog | 12 (8.8) | 3.2 |
| Others | 4 (2.9) | 2.5 |
LAA: Laboratory animal allergy
A positive correlation was found between personal history of allergy and the occurrence of LAA (OR=0.1; 95% CI=0.05–0.43; p<0.001). This correlation remained significant even after adjusting for potential confounders such as smoking habits, education on allergenic material, and family history of allergy (Table 3). The results were similar regarding family history of allergy and the occurrence of LAA using simple logistic regression analysis (OR=0.2; 95% CI=0.10–0.72; p=0.009). However, the correlation between family history of allergy and the occurrence of LAA was no longer significant in the multiple logistic regression analysis (Table 3).
Table 3. Multiple logistic regression analysis for the occurrence of LAA and studied parameters.
| Predictor | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Personal history of allergy (yes or no) | 0.1 | 0.04–0.46 | 0.001 |
| Family history of allergy (yes or no) | 0.5 | 0.16–1.38 | 0.175 |
| Smoking (yes or no) | 0.6 | 0.25–1.15 | 0.113 |
| Age | 0.9 | 0.94–1.05 | 0.956 |
| Sex | 1.1 | 0.33–3.47 | 0.902 |
| Education on allergenic material (yes or no) | 1.5 | 0.45–5.06 | 0.496 |
LAA: Laboratory animal allergy
Among the 24 subjects with LAA, 14 (58.3%) reported that a medical doctor confirmed the diagnosis of LAA, 21 (87.5%) were able to report the latency of LAA, and more than half of them (57.2%) developed LAA symptoms within their first three years of exposure (Table 1). The majority of LAA subjects (79.1%) who were allergic to domestic pets were more likely to report LAA symptoms then others. Regarding subjects who have been into contact with at least two animal species, the proportion of those from the LAA group was relatively higher than those from the non-LAA group (70.8% vs. 29.2%, p=0.07).
Concerning the use of personal protective equipment and its effects, 83.0% of exposed subjects used to wear gloves but rarely wore goggles or caps, and none used respirators.
Discussion
LAA represents an important health concern for subjects in contact with experimental animals and may lead to asthma13, 14). Extensive efforts have been made in the risk assessment and management of LAA, but new cases continue to appear6) with both social and medical consequences. Thus, LAA remains a common threat for those working with lab animals11). The overall prevalence of LAA found in this survey (17.6%) falls within the general reported range of 11% to 44%4). It was mainly due to exposure to mice (39.6%) and rats (29.2%), probably as these animals are the ones most frequently used in research facilities14). A similar prevalence of LAA has been reported in Japan (23.1%)7), and in the United States of America (15%)15); but the study by Bryant et al.16), that used the skin reactivity test reported a higher (56%) prevalence than ours. The inconsistency in study design in these studies may explain this fact. We did not perform face-to-face interviews, and no objective tests were done to confirm allergy; the prevalence of LAA was solely estimated on the reported symptoms, although 58.3% of allergic patients reported that a medical doctor confirmed their diagnosis clinically.
There is a laboratory-regulation insisting that everyone who works in lab animal facilities must use personal protective equipment and be well educated about laboratory hazards. This study revealed that among 136 subjects who performed animal experiments, only 33 (24.2%) subjects received education on allergenic material. This shows that the majority of the subjects was not aware of the allergic issues, and could have used more education to acquire knowledge about work-related allergic disease and techniques to reduce and control exposure. Some researchers were inexperienced animal handlers and may have been highly exposed to allergens, suggesting that more personal initiative is needed in controlling exposure to allergens.
In our study, most of the subjects (57.2%) developed LAA within a few months in the first three years of animal contact, which is in good agreement with other studies7, 15). However, the latency period was 14 yr for one participant, meaning that the threat of developing LAA remains even years later.
Among the 196 subjects, we were able to get feedback from 169 (86.2%) subjects. Those who did not complete the questionnaire were likely not to be interested in this study; another reason for non-reply could be hesitation to disclose their medical conditions to others17).
Allergic rhinitis is considered as an important health condition that affects patient’s quality of life in terms of sleep pattern18,19,20). Its prevalence among animal handlers is estimated at between 10% to 33%21). In the current study, allergic rhinitis was the most frequently reported symptom and was found in 14.0% of subjects, although there was no way to differentiate true work-related rhinitis from that caused by non-occupational allergens. Only one subject with respiratory symptoms did not report rhinitis, supporting the fact that animal allergens strongly sensitize the respiratory tract22).
Concerning asthma due to LAA, five subjects (3.7%) were affected by work-related asthma symptoms. Although the results for lung function tests were not available and we could not assess asthma severity, all participants with asthma asserted that a physician carried out a clinical diagnosis.
Atopic subjects tend to develop LAA at low levels of exposure to animal allergens23). Out of the 24 symptomatic subjects, 15 (62.5%) reported a personal history of allergy to environmental factors other than laboratory animals, denoting that pre-existing atopy had contributed to the development of LAA. In our study, however, this is only a hypothesis because it is a cross-sectional study where the cause-effect relationship cannot be established. On the other hand, respiratory symptoms due to LAA are believed to be more common among smokers24). Nevertheless, reports are conflicting, and our survey failed to show the contributing effect of cigarette smoking on LAA development, probably because of the cross sectional design of our study and the small number of smokers found in this study.
In this survey, we found a positive correlation between the development of LAA and the length of handling animals per day and per week. These findings support the dose-response relationships described by Elliott25). Our study had some limitations: all subjects were aware of our objectives, and this constituted a potential information bias that may have affected the magnitude of prevalence in terms of overestimation.
These findings provide further support for the fact that LAA obviously remains a serious health concern despite modern techniques used in animal facilities, although our prevalence of LAA was within the general range reported in the literature. Therefore, we suggest that people in close contact with lab animals or their waste should take the lead in protecting themselves from allergens exposure, and further support the need for institutions to establish more effective programs using their current knowledge.
The authors thank the medical researchers who kindly completed the survey questionnaire. They are also grateful to Mr. Daniel Ribble, Dr Narongpon Dumavibhat, Mugo Andrew, and Mrs Mansongi Biyela Carine for their enthusiastic participation. There are no potential conflicts of interest regarding the content of this article.
References
- 1.Bush RK. (2001) Assessment and treatment of laboratory animal allergy. ILAR J 42, 55–64. [DOI] [PubMed] [Google Scholar]
- 2.Bush RK. (2001) Mechanism and epidemiology of laboratory animal allergy. ILAR J 42, 4–11. [DOI] [PubMed] [Google Scholar]
- 3.Larese Filon F, Siracusa A, Rui F, Matteucci G, Pace ML, Fiorito A, Morucci P, Marabbini A. (2002) [Prevalence of occupational allergy to laboratory animals in two towns of northern and central Italy]. Med Lav 93, 87–94. [PubMed] [Google Scholar]
- 4.Bush RK, Stave GM. (2003) Laboratory animal allergy: an update. ILAR J 44, 28–51. [DOI] [PubMed] [Google Scholar]
- 5.Kruize H, Post W, Heederik D, Martens B, Hollander A, van der Beek E. (1997) Respiratory allergy in laboratory animal workers: a retrospective cohort study using pre-employment screening data. Occup Environ Med 54, 830–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruoppi P, Koistinen T, Susitaival P, Honkanen J, Soininen H. (2004) Frequency of allergic rhinitis to laboratory animals in university employees as confirmed by chamber challenges. Allergy 59, 295–301. [DOI] [PubMed] [Google Scholar]
- 7.Aoyama K, Ueda A, Manda F, Matsushita T, Ueda T, Yamauchi C. (1992) Allergy to laboratory animals: an epidemiological study. Br J Ind Med 49, 41–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cullinan P, Cook A, Gordon S, Nieuwenhuijsen MJ, Tee RD, Venables KM, McDonald JC, Taylor AJ. (1999) Allergen exposure, atopy and smoking as determinants of allergy to rats in a cohort of laboratory employees. Eur Respir J 13, 1139–43. [DOI] [PubMed] [Google Scholar]
- 9.Krakowiak A, Szulc B, Górski P. (1997) Occupational respiratory diseases in laboratory animal workers: initial results. Int J Occup Med Environ Health 10, 31–6. [PubMed] [Google Scholar]
- 10.Acton D, McCauley L. (2007) Laboratory animal allergy: an occupational hazard. AAOHN J 55, 241–4. [DOI] [PubMed] [Google Scholar]
- 11.Pacheco KA. (2007) New insights into laboratory animal exposures and allergic responses. Curr Opin Allergy Clin Immunol 7, 156–61. [DOI] [PubMed] [Google Scholar]
- 12.Renström A, Malmberg P, Larsson K, Larsson PH, Sundblad BM. (1995) Allergic sensitization is associated with increased bronchial responsiveness: a prospective study of allergy to laboratory animals. Eur Respir J 8, 1514–9. [PubMed] [Google Scholar]
- 13.Elliott L, Heederik D, Marshall S, Peden D, Loomis D. (2005) Progression of self-reported symptoms in laboratory animal allergy. J Allergy Clin Immunol 116, 127–32. [DOI] [PubMed] [Google Scholar]
- 14.Hollander A, Doekes G, Heederik D. (1996) Cat and dog allergy and total IgE as risk factors of laboratory animal allergy. J Allergy Clin Immunol 98, 545–54. [DOI] [PubMed] [Google Scholar]
- 15.Gross NJ. (1980) Allergy to laboratory animals: epidemiologic, clinical, and physiologic aspects, and a trial of cromolyn in its management. J Allergy Clin Immunol 66, 158–65. [DOI] [PubMed] [Google Scholar]
- 16.Bryant DH, Boscato LM, Mboloi PN, Stuart MC. (1995) Allergy to laboratory animals among animal handlers. Med J Aust 163, 415–8. [DOI] [PubMed] [Google Scholar]
- 17.Asai A, Ohnishi M, Nishigaki E, Sekimoto M, Fukuhara S, Fukui T. (2002) Attitudes of the Japanese public and doctors towards use of archived information and samples without informed consent: preliminary findings based on focus group interviews. BMC Med Ethics 3, E1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.del Cuvillo A, Montoro J, Bartra J, Valero A, Ferrer M, Jauregui I, Dávila I, Sastre J, Mullol J. (2010) Validation of ARIA duration and severity classifications in Spanish allergic rhinitis patients—The ADRIAL cohort study. Rhinology 48, 201–5. [DOI] [PubMed] [Google Scholar]
- 19.Storms W. (2008) Allergic rhinitis-induced nasal congestion: its impact on sleep quality. Prim Care Respir J 17, 7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blaiss MS. (1999) Quality of life in allergic rhinitis. Ann Allergy Asthma Immunol 83, 449–54. [DOI] [PubMed] [Google Scholar]
- 21.Sublett JW, Bernstein DI. (2010) Occupational rhinitis. Curr Allergy Asthma Rep 10, 99–104. [DOI] [PubMed] [Google Scholar]
- 22.Krakowiak A, Szulc B, Pałczyński C, Górski P. (1996) [Laboratory animals as a cause of occupational allergy]. Med Pr 47, 523–31. [PubMed] [Google Scholar]
- 23.Heederik D, Venables KM, Malmberg P, Hollander A, Karlsson AS, Renström A, Doekes G, Nieuwenhijsen M, Gordon S. (1999) Exposure-response relationships for work-related sensitization in workers exposed to rat urinary allergens: results from a pooled study. J Allergy Clin Immunol 103, 678–84. [DOI] [PubMed] [Google Scholar]
- 24.Fuortes LJ, Weih L, Jones ML, Burmeister LF, Thorne PS, Pollen S, Merchant JA. (1996) Epidemiologic assessment of laboratory animal allergy among university employees. Am J Ind Med 29, 67–74. [DOI] [PubMed] [Google Scholar]
- 25.Elliott L, Heederik D, Marshall S, Peden D, Loomis D. (2005) Incidence of allergy and allergy symptoms among workers exposed to laboratory animals. Occup Environ Med 62, 766–71. [DOI] [PMC free article] [PubMed] [Google Scholar]