Abstract
Objectives:
(1) To measure the crestal bone levels around implants immediately, and one month, three months, and six months after immediate implant placement, to evaluate the amount of bone level changes in six months. (2) To measure the initial stability in immediate implant placement.
Materials and Methods:
Ten patients were selected and a total of ten implants were placed in the immediate extraction sites. The change in the level of crestal bone was measured on standardized digital periapical radiographs taken at baseline, first month, third month, and sixth months for each patient, using the SOPRO imaging software. The initial stability of implants was measured with resonance frequency analysis (RFA) and an engine-driven torque. The measurements were statistically analyzed. The student's t-test was used, to identify the significance of the study parameters.
Results:
When mesial and distal bone losses were averaged, the radiographic evaluation with the SOPRO imaging software showed an average of 0.80 mm, with a standard deviation of ± 0.18 mm bone loss at the first month, followed by 1.03 mm with a standard deviation of ± 0.19 mm at the third month, and 1.23 mm with standard deviation of ± 0.6 mm at the sixth month. The initial stability with the RFA instrument showed a mean of 55 implant stability quotient (ISQ) values and the torque showed a value of 36.50 Nm.
Conclusions:
The implant has to be placed 2 mm below the crestal bone level to compensate the crestal bone loss. The initial stability is achieved by apical preparation of the socket wall and use of straight screw implants. When the defect is more than 2 mm, autogenous grafts with membranes are the best choice.
Keywords: Crestal bone loss, immediate implants, initial stability in immediate implants
INTRODUCTION
The advent of implants has revolutionized the field of dentistry. Nearly 40 years ago, Branemark discovered that fully edentulous patients could be dentally rehabilitated using machined screws made of commercially pure titanium, which osseointegrated to the jawbone, enabling the attachment of a fixed prosthesis. Since then, endosseous dental implants of various shapes and surface textures have been used in partially edentulous patients. According to him a waiting period of 12 months following tooth extraction was necessary before an endosseous dental implant could be placed and loaded with a prosthesis. The rationale for this waiting was to allow resolution of any hard or soft tissue pathology in the proposed recipient site.[1]
Several studies conducted to know the effects of tooth extraction on the dimensional changes observed with both the hard and soft tissues revealed that after extraction, during the first four months of healing, the buccolingual ridge underwent a reduction of approximately 5 to 7 mm, with a 2- to 4.5-mm loss of vertical bone height. Schroop and colleagues measured the intraoperative dimensional changes in 46 healing sockets. in 46 patients, confined to only the premolars and molars, in both arches. They reported a reduction in the buccolingual width of nearly 50% over an observation period of 12 months and two-thirds of the change occurred within the first three months following tooth extraction, with the greatest changes observed in the molar sites.
This resorption post extraction could adversely affect the availability of bone for implant placement, hence, clinicians began to insert dental implants immediately following tooth extraction. The first reported case was described by Schulte in 1976.[1] Since then, numerous clinical case reports have been published, and at various times, review articles have appeared to update this surgical technique.[1] With this background we have planned our study to analyze the initial stability and crestal bone loss around the implants immediately, and one month, three months, and six months after immediate implant placement and to evaluate the amount of bone level changes in six months.
MATERIALS AND METHODS
Ten patients were selected among the patients who visited the Department of Oral Surgery, at the Meenakshi Ammal Dental College and Hospital, who were found to have at least one maxillary or mandibular single-rooted tooth indicated for extraction. The inclusion criteria included, patients aged between 20 and 25 years requiring extraction of teeth for reasons such as, caries without any periapical pathology, trauma without affecting the alveolar bone, root stumps, and root-fractured tooth. Multi-rooted teeth, teeth with any bony defects, and teeth with acute or chronic periapical pathology were excluded.
The study protocol was approved by the Ethical Committee of the Meenakshi University, Chennai. All the patients were informed about the procedure being conducted and informed consent was obtained. The implant system used for the study was the Pitt-easy implant system. Preoperative diagnostic casts were obtained to know the interarch relationship and preoperative photographs and radiographs were taken. The implant diameter was selected based on the bone available in the mesio-distal distance between the adjacent root tips and the length was selected 2 mm beyond the socket wall to be restored using a preoperative radio visio graph (RVG) [Figure 1].
Figure 1.

Preoperative picture showing partial edentulism and root stumps in relation to region around 11
Surgical procedure
Complete blood investigations were performed to evaluate the fitness of the patient for implant placement. After local anesthesia the tooth was atraumatically extracted using periotomes. Once the extraction was completed, the site was thoroughly degranulated using curettes. Manual probing was done and an intraoral periapical (IOPA) radiograph was taken to verify that the socket wall was intact and there were no root remnants. The length and width of the extracted tooth was measured to determine the width and diameter of the implant [Figure 2].
Figure 2.

(a) Extracted root stump using periotomes (b) Completely extracted root stump
Initiation of osteotomy was performed in the standard fashion, with the drilling speed at 800 rpm for the initial pilot drill along with both internal and external irrigation with normal saline. An IOPA was taken with a 2.0 mm initial drill for identifying the angulation and length. Then it was drilled 2 mm above the socket wall. Sequential drilling was carried out with 2.2, 2.8, 3.2, and 3.65 drills. Following this, the sequential drilling implant was placed into the socket wall with a motor-driven handpiece about 35-40 Nm torque. Using a radio frequency analyzer (RFA) the Implant Stability Quotient (ISQ) value of the implant was noted.[2] The SmartPeg was placed into the abutment screw hole and tightened. Next, using hand-held probe, the initial stability was noted from the reading on the RFA screen [Figure 3]. Finally, the cover screw was placed and the surgical area was thoroughly irrigated and debrided. Buccal and lingual flaps were well-approximated and sutured to cover and protect the implant site. A three-day postoperative antibiotic regime was prescribed for the patient. A final IOPA was taken and sutures were removed after seven days.
Figure 3.
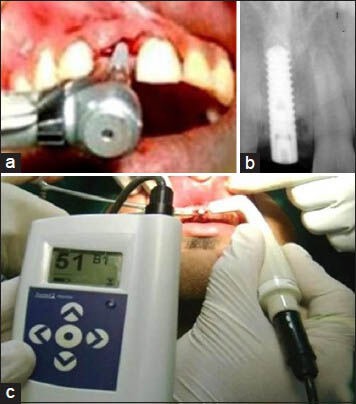
(a and b) Implant placed using motor-driven handpiece (c) RFA to verify initial stability
Follow up
Recall appointments were made after one month, three months, and six months, after immediate implant placement and after all the clinical and radiological parameters were recorded [Figure 4]. After six months of follow-up with good osseointegration and following the completion of soft tissue sculpting, the healing screw was exposed and the abutment was tightened to a torque of 35 Ncm and was customized into the desired shape. A closed tray impression technique was performed and the definitive restoration delivered with cementation of the prosthesis, with a permanent cement like glass ionomer cement (GIC) type-I [Figure 5]. The patient was followed-up for one year.
Figure 4.
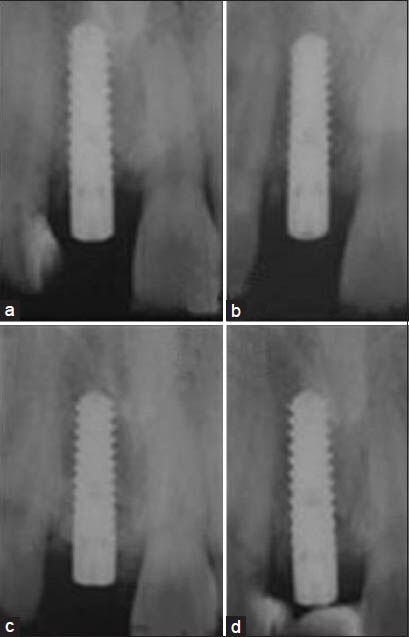
IOPAs taken (a) Immediate (b) first month (c) third month (d) sixth month
Figure 5.

Picture showing restored implant prosthesis
Statistical analysis
The Statistical Package for Social Sciences Software (SPSS 11) was used for computations. Microsoft Word and Excel were used to generate graphs and tables [Table 1 and Figure 6]. To find the significance of the study parameters, the student's t test was used and a P ≤ 0.05 was considered as statistically significant, at 95% C.I.
Table 1.
The results
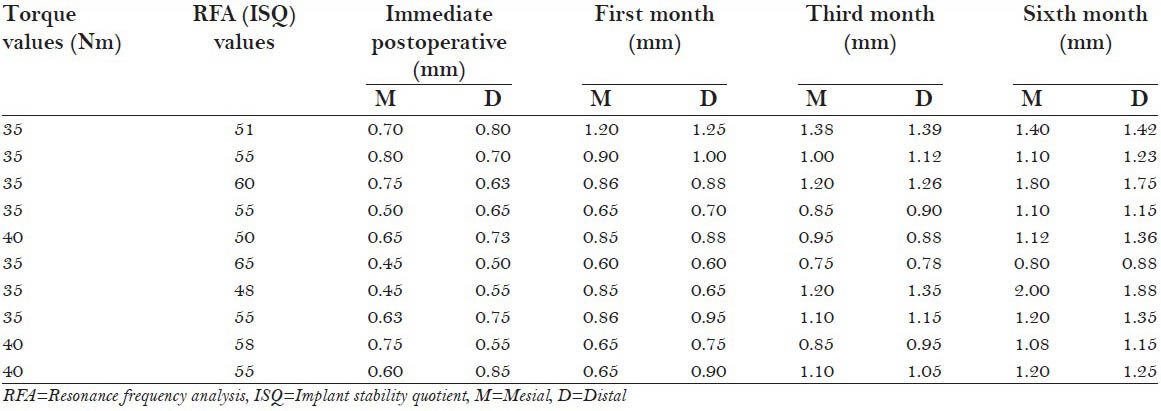
Figure 6.

Evaluating the crestal bone loss using SOPRO imaging software
RESULTS
Ten implants were placed in ten patients with a mean age of 30.4 years, with a minimum age of 20 years and a maximum age of 55 years. All implants included in the study functioned well during the mean follow-up period of six months.
The initial stability with the RFA instrument showed a mean of 55 ISQ values and the torque showed a value of 36.50 Nm. The radiographic evaluation exhibited no peri-implant radiolucency, which indicated good osseointegration. When the mesial and distal bone losses were averaged, the radiographic evaluation with the SOPRO imaging software showed an average of 0.80 mm with a standard deviation of ± 0.18 mm bone loss at the first month, followed by 1.03 mm with a standard deviation of ± 0.19 mm at third month, and 1.23 mm with a standard deviation ± 0.6 mm at the sixth month.
DISCUSSION
The original protocol of a dental implant placement requires a period of six months following extraction, to allow for healing of the extraction socket. Several studies have revealed that during this waiting period, there is a definitive post-extraction resorption of bone, which will adversely affect the availability of bone for implant placement. To reduce this problem of bone loss, implants have been placed immediately into fresh extraction sockets. In 1989, Lazzara first reported immediate implant placement at an extraction socket. The success of dental implant treatment of partially and fully edentulous patients has been documented extensively.[3,4] This healing pattern has been termed ‘Type 1’ implant installation at a consensus conference.[5,6]
In the present study, all the 10 implants were placed successfully, showing good osseointegration at the end of six months, with no signs of pain, discomfort or periapical radiolucency. This could be due to the proper care taken during implant placement and the optimal plaque control followed by the patients postoperatively.
Stability is the most important factor for the loading of an implant with prosthesis and for its success. In immediate implant cases there is a customized socket wall for attaining good initial stability and in the present study also all the cases had good socket walls. To analyze the socket wall continuity we used manual probing along the socket walls on all sides and also used RVG for identifying any defect.
To attain good initial stability we selected implants 2 mm longer than the socket length and excess preparation was done 2 mm beyond the socket, with initial drilling followed by sequential drilling, which was in concordance with the previous studies.[7] Therefore, the initial stability attained in our study cases might be primarily due to the contact of the implant bone interface (IBI), only in the apical one-third.
Selection of the implant body contour is very important to attain good initial stability. As the socket wall is tapered toward the apex, it is best to use cylindrical or straight screw implants. Drilling with drills that have exact angulation is also primarily important, as always, if the root is slightly curved the drill goes toward the path of least resistance. Therefore, a firm grip is necessary to prepare a 2-mm implant site apically.
During the process of healing of the extracted socket there is bone resorption followed by remodeling, usually in the implant collar area, to compensate for this crestal bone loss. In the current study, implants are placed into an extraction socket with the implant shoulder margin at least 2 mm below the crestal bone level, which is in correlation with other studies. This demonstrates that vertical resorption can be limited by placing the implant shoulder below the level of the crestal bone.[7] Evaluation of the crestal bone level has been performed using standardized digital periapical radiographs with the long-cone paralleling technique in conformation with studies evaluating marginal bone loss.[8,9] Even though histometry serves as the gold standard to assess the crestal bone level accurately, a study by Hermann, et al., comparing histometry and standardized periapical radiographs has shown that the precision of the radiographs is within 0.1 mm of the histometry in 73.4% and between 0.1 and 0.2 mm in 15.9% of the evaluations. The prevention of the cover screw exposure is also minimized, as it attains a good tissue biotype. The incremental suture technique is followed for an easy flow of exudates during the process of healing by primary intention.
In one case, there was a loss of the labial cortical plate and this area was grafted using an autogenous bone graft, harvested from chin of the patient. It was made into a bone blend and grafted using the membrane. Postoperative healing after six months gave a satisfactory result.[10]
Advantages for immediate placement include, reduced surgical time, preservation of the alveolar bone, easy maintenance of soft tissues, and a simplified prosthetic design. The disadvantages include, secondary infections in the grafted sites and recession in the thin tissue biotype areas.[11]
Radiographic evaluation is done by measuring the distance from the apex of the implant to the collar of the implant, and the distance from the apex of the implant to the mesial and distal alveolar bone crest immediately, and at one month, three months, and six months. The differences have been calculated and the crestal bone loss evaluated using the SOPRO imaging software.
In the present study, when the mesial and distal bone losses were radiographically evaluated with the SOPRO imaging software, they showed a mean of 0.80 mm with a standard deviation of ± 0.18 mm bone loss at the first month, followed by 1.03 mm with a standard deviation ± 0.19 mm at the third month, and 1.23 mm with a standard deviation of ± 0.6 mm at the sixth month. This showed a marked reduction in bone loss when compared to the conventional implant placement. Therefore, the results of the present study confirmed the hypothesis that immediate implant placement reduced alveolar resorption.
CONCLUSION
In the present study, immediate implant placement showed a marked reduction in bone resorption when compared with conventional implant placement. The implant length had to be 2 mm more than the socket length. The straight screw implant body was the best to use. A 2-mm sunken implant of the shoulder into the socket was a must. If the jumping distance was more than 2 mm between the implant shoulder and the socket wall, it was best restored with an autograft.
ACKNOWLEDGMENTS
No financial interests, direct or indirect, for any of the authors exist for this article. There are no sources of outside support for the project of this article.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Beagle JR. The immediate placement of endosseous dental implants in fresh extraction sites. Dent Clin North Am. 2006;50:375–89. doi: 10.1016/j.cden.2006.03.003. vi. [DOI] [PubMed] [Google Scholar]
- 2.Valderrama P, Oates TW, Jones AA, Simpson J, Schoolfield JD, Cochran DL. Evaluation of two different resonance frequency devices to detect implant stability: A clinical trial. J Periodontol. 2007;78:262–72. doi: 10.1902/jop.2007.060143. [DOI] [PubMed] [Google Scholar]
- 3.Karoussis IK, Salvi GE, Heitz-Mayfield LJ, Brägger U, Hämmerle CH, Lang NP. Long-term implant prognosis in patients with and without a history of chronic periodontitis: A 10-year prospective cohort study of the ITI dental implant system. Clin Oral Implants Res. 2003;14:329–39. doi: 10.1034/j.1600-0501.000.00934.x. [DOI] [PubMed] [Google Scholar]
- 4.Kwon KR, Sachdeo A, Weber HP. Achieving immediate function with provisional prostheses after implant placement: A clinical report. J Prosthet Dent. 2005;93:514–7. doi: 10.1016/j.prosdent.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G. Long-term survival and success of oral implants in the treatment of full and partial arches: A 7-year prospective study with the ITI dental implant system. Int J Oral Maxillofac Implants. 2004;19:247–59. [PubMed] [Google Scholar]
- 6.Hämmerle CH, Chen ST, Wilson TG., Jr Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004;19(Suppl):26–8. [PubMed] [Google Scholar]
- 7.Cordaro L, Torsello F, Roccuzzo M. Clinical outcome of submerged vs. non-submerged implants placed in fresh extraction sockets. Clin Oral Implants Res. 2009;20:1307–13. doi: 10.1111/j.1600-0501.2009.01724.x. [DOI] [PubMed] [Google Scholar]
- 8.Appleton RS, Nummikoski PV, Pigno MA, Cronin RJ, Chung KH. A radiographic assessment of progressive loading on bone around single osseointegrated implants in the posterior maxilla. Clin Oral Implants Res. 2005;16:161–7. doi: 10.1111/j.1600-0501.2004.01089.x. [DOI] [PubMed] [Google Scholar]
- 9.Pirker W, Kocher A. Immediate, non-submerged, root-analogue zirconia implants placed into single-rooted extraction sockets: 2-year follow-up of a clinical study. Int J Oral Maxillofac Surg. 2009;38:1127–32. doi: 10.1016/j.ijom.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Carmagnola D, Adriaens P, Berglundh T. Healing of human extraction sockets filled with Bio-Oss. Clin Oral Implants Res. 2003;14:137–43. doi: 10.1034/j.1600-0501.2003.140201.x. [DOI] [PubMed] [Google Scholar]
- 11.Rosenquist B, Ahmed M. The immediate replacement of teeth by dental implants using homologous bone membranes to seal the sockets: Clinical and radiographic findings. Clin Oral Implants Res. 2000;11:572–82. doi: 10.1034/j.1600-0501.2000.011006572.x. [DOI] [PubMed] [Google Scholar]


