Abstract
Objective:
To evaluate and compare the oral health status and the impact of supervised toothbrushing and oral health education among school children of urban and rural areas of Maharashtra, India.
Materials and Methods:
A total of 200 school children in the age group 12-15 years were selected by stratified random sampling technique from two schools and were further divided into two groups: Group A (urban school) and Group B (rural school). Both the groups were again subdivided into control group and study group. Supervised toothbrushing was recommended for both the groups. The toothbrushing teaching program included session on oral health education, individual toothbrushing instructions, and supervised toothbrushing. Dental caries increment, plaque scores, and gingival status were assessed as per the World Health Organization (WHO) criteria (1997), Turesky-Gilmore-Glickman modification of the Quigley Hein Plaque Index, and Loe-Silness Gingival Index (1963), respectively. Cronbach's alpha, Chi-square test, paired t-test, and unpaired t-test were utilized for data analysis.
Results:
The mean plaque and gingival score reduction was significantly higher in the study groups as compared to the control groups. An increase in the mean of Decayed, missing, filled teeth (DMFT) and Decayed, missing, filled teeth and surfaces (DMFS) scores throughout the study period was seen in children who participated in study.
Conclusion:
Oral health education was effective in establishing good oral health habits among school children and also in enhancing the knowledge of their parents about good oral health.
Keywords: Dental caries, dental health education, oral hygiene status, school children, toothbrushing
INTRODUCTION
Dental caries and periodontal diseases exert tremendous social, economic, and financial burden on a global scale. Despite a plethora of preventive measures available, dental plaque, the precursor of dental caries and periodontal disease, remains an enigma. The mechanical removal of dental plaque, if effectively carried out, can be the most effective method of maintaining good oral hygiene, reducing tooth decay, and promoting better gingival health.[1] Various methods are employed to maintain oral hygiene, of which the most common is toothbrushing.[2] It is an effective way of removing plaque, preventing gingivitis, and also managing dental caries.[3] However, the value of uncontrolled toothbrushing in prevention of dental caries has always been questioned.[4] Effective plaque removal depends not only on the type of toothbrush but also on the proper brushing technique.[5] It is obvious that manual dexterity and motivation of an individual are of paramount importance in maintaining oral hygiene.[6] The plethora of literature is enormous on the effectiveness of the toothbrushing for achieving good oral hygiene; however, no study has been carried out exclusively to evaluate the efficacy of supervised toothbrushing by parents and the impact of oral health education on improving the oral hygiene status of school children. More so, no study exclusively has been conducted in the Indian environment. The obscurity in achieving a satisfactory standard of oral hygiene among the rural and few urban areas is of paramount significance when the child is not assisted or supervised by an adult.[7]
Thus, to explore this aim, the present study was designed with the objectives to evaluate and compare the effectiveness of supervised toothbrushing and its impact on oral health in school children of urban and rural communities.
MATERIALS AND METHODS
Study population and methodology
This comparative study was carried out by the Department of Pediatric and Preventive Dentistry, Nair Hospital Dental College, Mumbai. The research protocol outlining the purpose and precise methodology of this study of 3 months duration was reviewed and approved prior to its implementation by the institutional ethics committee as well as by the administrative authorities of Municipal Corporation of Greater Mumbai and Thane Administration. Two schools, Gilderlane Municipal School of Mumbai Central (urban) and D. J. Galvankar High School, Arnala (rural), were selected for the study. The fluoride level of drinking water samples of the study area is 0.03 mg/l.
The children who were in good general health as well as the permanent residents of the area were included. Children with physical limitation or motor incoordination, medically compromised children, and children with any evidence of significant oral soft tissue pathology other than gingivitis were not included. A total of 200 school children in the age group 12-15 years were selected by stratified random sampling technique from two schools and were further divided into two groups: Group A (urban school; Mumbai - 100 children) and Group B (rural school; Arnala - 100 children). Both the groups were again subdivided into control group and study group having 50 children (25 girls and 25 boys).
The children of the study groups were taught toothbrushing as per bass methodology, using models, charts, and also by live demonstrations under the supervision of parents, and were instructed to brush their teeth twice daily for 2 min using a peanut size of study dentifrice (containing 1000 ppm of fluoride, standardized for all). They were asked to refrain from all other oral hygiene measures during the course of the study. Oral care instructions were specified, which included the topics on importance of oral health, etiology and pathogenesis of oral diseases, methods of oral hygiene maintenance, etc., No intervention was provided to the children in the control groups and routine oral hygiene maintenance procedures were continued. The dentifrices and toothbrushes were provided to all the children who participated in the study, at regular intervals. The children were further instructed to maintain a 3-day diet diary, provided in local language as well as in English. The diet of the children was analyzed for sugar exposure as per the recommendation of Nizel.[8] At each subsequent visit, the feedback regarding the dentifrice usage was recorded.
The recording procedures of decayed, missing, filled teeth and surfaces (DMFT/DMFS), plaque scoring, and gingival index were standardized by sessions of calibration between the investigator and the supervisor. Single examiner recorded all the parameters. Intra-examiner reliability of the recorded data was assessed by re-examining 10% of the children after 2 weeks of the initial examination. The detailed oral health examination was carried out in their respective schools where they were seated on an ordinary chair ensuring adequate daylight, supplemented with a torch (3.0 V DC) to facilitate the examination. The dental caries, plaque score, and gingival status were assessed as per the World Health Organization (WHO) criteria (1997), Turesky–Gilmore–Glickman modification of the Quigley Hein Plaque Index, and Loe–Silness Gingival Index, respectively. Clinical examination after 1 month of baseline examination and further at 3 months interval was carried out to evaluate the plaque scores, gingival status, and dental caries. Data collected were then subjected to statistical analysis using Cronbach's alpha, Chi-square test, paired t-test, and unpaired t-test.
RESULTS
At the end of 3 months examination, 197 children (99 of urban school and 98 of rural school) completed the study. The overall dropout rate was 1.50%.
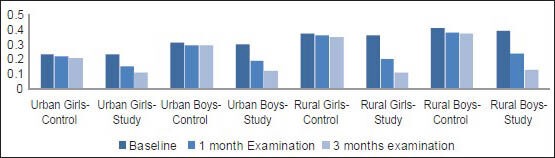
The mean DMFT scores for girls and boys at baseline and at the end of 1 and 3 months for the urban and rural areas are depicted in Table 1 and Graph 1. The mean DMFS scores for girls and boys at baseline and at the end of 1 and 3 months for the urban and rural areas are depicted in Table 2 and Graph 2.
Table 1.
DMFT score in children at baseline and at the end of 1 and 3 months
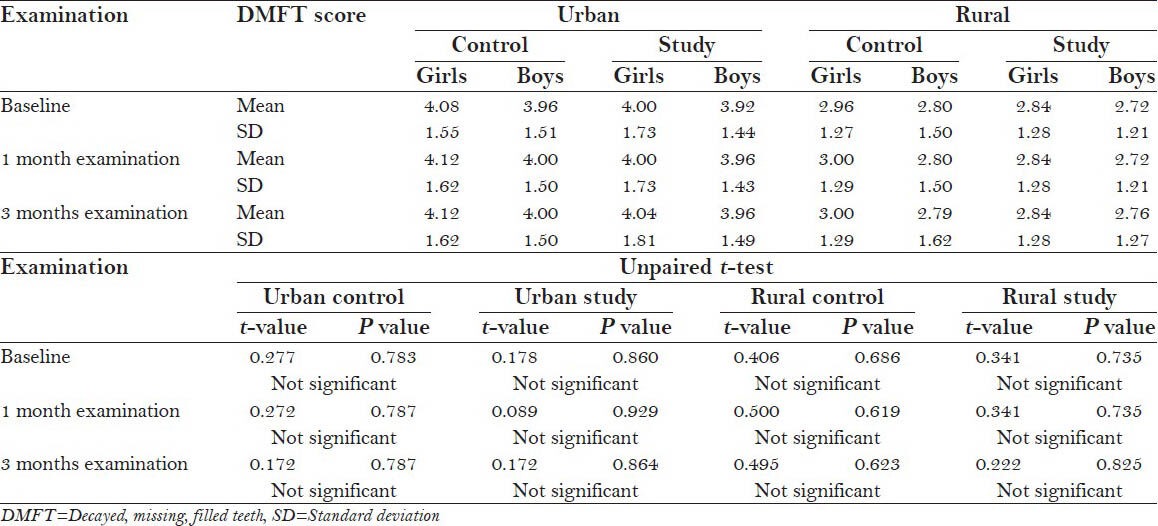
Graph 1.

Mean DMFT score in children at baseline and at the end of 1 and 3 months
Table 2.
DMFS score in children at baseline and at the end of 1 and 3 months

Graph 2.

Mean DMFS score in children at baseline and at the end of 1 and 3 months
Although the overall mean DMFT and DMFS scores were higher in girls as compared to boys in all the four groups at baseline and at the end of 3 months, the results were not statistically significant (P > 0.05) [Tables 1 and 2, respectively]. Furthermore, no statistically significant difference was observed between both the groups of urban and rural areas in regards to mean DMFT and DMFS score at baseline and at 3 months examination. An increase in mean DMFT and DMFS scores throughout the study period was seen among all the children who participated in the study [Tables 1 and 2, Graphs 1 and 2].
The mean plaque scores for girls and boys at baseline and at the end of 1 and 3 months for the urban and rural areas are given in Table 3 and Graph 3. The mean gingival index scores for girls and boys at baseline and at the end of 1 and 3 months for the urban and rural areas are given in Table 4 and Graph 4.
Table 3.
Plaque score in children at baseline and at the end of 1 and 3 months

Graph 3.

Mean plaque score in children at baseline and at the end of 1 and 3 months
Table 4.
Gingival index score in children at baseline and at the end of 1 and 3 months

Graph 4.
Mean gingival index score in children at baseline and at the end of 1 and 3 months
Baseline values of the mean plaque score and gingival score revealed no significant difference between all the four groups. At 3 months examination, the reduction in mean plaque and mean gingival index scores was significantly higher in the study groups as compared to the control groups in both the schools. No statistically significant difference was observed between the rural control and urban control groups with respect to mean plaque and gingival index score reduction at 1 and 3 months examination. However, reduction in both the parameters was observed to be significantly higher in the rural study group as compared to the urban study group. Moreover, reduction in mean plaque score was seen to be higher in girls in both the control groups at 3 months examination and reverse interpretation was true for gingival index score representing higher reduction in boys in both the control groups and in the urban study group [Tables 3 and 4, Graphs 3 and 4].
DISCUSSION
Oral health habits, attitudes, and behavior are best established during childhood. It is believed that visualization, active participation, skill training, and reinforcement are of paramount importance in establishing and altering behavior in a child. Also, the largest and the most significant group accessible for oral health education is always seen in school systems. For that reason, in the present study, classroom was considered an ideal setting to conduct supervised toothbrushing program, especially in rural areas where oral health facilities are meager and rarely parents are concerned of their children's toothbrushing behavior. However, a study by Lindhe and Koch,[9] concluded the impracticability of prolonged careful supervision of toothbrushing behavior.
The present study was carried out in a rural area of Arnala in Thane district of Maharashtra. Thane is the largest district in Maharashtra, comprising mainly tribal population, who are away from modern life of civilization, even though it is just 70 km away from Mumbai. The tribal population of Thane including Arnala is deprived of modern amenities. The children are motivated by dedicated social workers to attend school, as most of the students do not attend school regularly. As far as oral hygiene habits are concerned, it was surprising to know that the children were not brushing their teeth regularly and even some of the parents including their children were using neem, babool, or kikar twig. Few of them were also using charcoal, burnt cow dung cake powder, etc., Parents too in the study area were found to be with neglected attitude and practice regarding oral hygiene. Therefore, parents were sensitized by giving oral hygiene instructions and demonstration on brushing technique, and were instructed to supervise child's toothbrushing at home. The rural school population of Arnala was specially targeted for this. To have proper control over the brushing regime, supervised brushing was initiated. Even though in Mumbai it could have been without parents’ supervision, the children studying in municipal school are from weaker sections and most of them live in slums, hence supervised toothbrushing was initiated.
The selected age group was from 12 to 15 years, since 12 years (as per WHO recommendations) is regarded as an age for international comparison and global monitoring of disease trends including dental caries, while 15 years is considered the last age from which a reliable sample may be easily obtained through the school system in most countries. The children selected from the municipal and rural schools in a metropolitan city like Mumbai with diversity of religions and languages were obviously expected to be from varied socioeconomic status. In view of the family characteristics, a strong influence of mothers on their children's toothbrushing habit has been documented.[10] Moreover, the implication of oral hygiene sessions and its compliance could only be ensured by parents’ supervision at their home.
The duration of the study was 3 months, sufficient for plaque to accumulate as supported by a study in which clinical signs of gingivitis were observed within 10-21 days.[11] The assessment of dental caries increment was in accordance with WHO criteria (1997), as it allows comparison of results with other national and international investigations using the same recording criteria.[12] The plaque scores were recorded using Turesky-Gilmore-Glickman modification of the Quigley Hein plaque index,[13] which has an advantage of clear objective definitions of each numerical score included in the index. For recording the gingival index score, gingival index system as proposed by Loe and Silness was used[14] which is entirely confined to qualitative changes in the gingival soft tissue.[15] Duration of toothbrushing is known to produce the strongest effect on plaque removal and should be emphasized in dental health education.[16] Hence, children were advised to brush twice daily for 2 min with bass method, thereby controlling the type of toothbrush and dentifrice, and the frequency and method of toothbrushing. The prime objective of the study was to boost proper oral health through supervised brushing among students selected in two different locations, i.e., the rural area of Arnala (one of the tribal and backward areas) in Thane district and a Municipal School in Mumbai Central. The bass technique was preferred over modified bass technique as it is simpler and easier for children to learn. As the children were not brushing at all, to encourage brushing habits, we preferred the simple technique, i.e., bass technique, as the initial measure.
The 3-day diet diary of every child was assessed to find out the nutritional status and hidden sugar in the diet. The diet history was taken which revealed that intake of carbohydrate was more and protein was less and the child had four to five sugar intake per day, including tuck shop sweets, etc., and the same was observed with the Mumbai school children (the first response was with whatever money they had, they bought sweets). The diet chart revealed that most of children did not receive proper food with proper nutrition value.
Evaluation of DMFT and DMFS scores
No statistically significant difference in caries increment was seen in children in the study group as compared to the control group, which is in accordance with the previous studies on oral health education[17,18] in which supervised toothbrushing sessions in the study groups were carried out and no significant reduction in caries increments was observed. However, the present study results are not in accordance with the study confirming reduced caries increment in the study population.[19]
Evaluation of mean plaque and gingival index scores
The difference in relation to the mean plaque and gingival index scores from baseline to 3 months in the study and control groups of both urban and rural areas was statistically significant. The results are in accordance with various studies.[9,20,21,22,23] A study carried out to determine the impact of an educational oral health program conducted within a club of America in Chicago also reported a statistically significant difference in plaque and gingival scores between study and control groups.[24] The results of the present study are not in agreement with the outcome of a 3-year school-based study carried out in a rural non-fluoridated community of East Hampton, Connecticut, in which lesser mean plaque and gingival scores were observed in the study group at the first follow-up examination and the scores were nearly at baseline levels at the second follow-up examination.[25]
In the present study, reduction in plaque and gingivitis was observed among children in the control group, which is attributed to the Hawthorne effect,[26] i.e., by virtue of participating in the study and undergoing frequent oral examinations, the children became self-motivated to improve their brushing technique.
Although the present study has yielded similar outcome to that of many other studies, it differs in relation to the manner of motivation. Simpler methods such as dental education programs and supervised toothbrushing have been adopted in this study without the use of expensive aids. Other studies have used frequent prophylaxis for longer duration along with supervised toothbrushing, which is impractical in an Indian scenario, as dental professionals will be able to attend a limited number of children and immense manpower also will be required. In contrast to this, the present study method can be employed on a larger scale with minimum expenditure and manpower.
CONCLUSION
The school-based caries preventive program comprised oral hygiene instructions and supervised toothbrushing education was effective in imparting oral health knowledge and establishing good oral hygiene habits in school children and in improving their oral hygiene status and the attitudes of their parents. With these positive findings, it is recommended that similar programs be supported and implemented with a larger sample size to determine the long-term effect of such programs and to improve the poor oral health situation among school children.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lindhe J, Axelsson P, Tollskog G. Effect of proper oral hygiene on gingivitis and dental caries in Swedish schoolchildren. Community Dent Oral Epidemiol. 1975;3:150–5. doi: 10.1111/j.1600-0528.1975.tb00299.x. [DOI] [PubMed] [Google Scholar]
- 2.Dale JW. Toothbrushing frequency and its relationship to dental caries and periodontal disease. Aust Dent J. 1969;14:120–3. doi: 10.1111/j.1834-7819.1969.tb04290.x. [DOI] [PubMed] [Google Scholar]
- 3.Tucker GJ, Andlaw RJ, Burchell CK. The relationship between oral hygiene and dental caries incidence in 11-year-old children. A 3-year study. Br Dent J. 1976;141:75–9. doi: 10.1038/sj.bdj.4803790. [DOI] [PubMed] [Google Scholar]
- 4.Ainamo J. Current basis for the prevention of dental caries. J Indian Dent Assoc. 1976;48:117–24. [PubMed] [Google Scholar]
- 5.Saxer UP, Yankell SL. Impact of improved toothbrushes on dental diseases. I. Quintessence Int. 1997;28:513–25. [PubMed] [Google Scholar]
- 6.Claydon N, Addy M. Comparative single-use plaque removal by toothbrushes of different designs. J Clin Periodontol. 1996;23:1112–6. doi: 10.1111/j.1600-051x.1996.tb01812.x. [DOI] [PubMed] [Google Scholar]
- 7.Bellini HT, Arneberg P, von der Fehr FR. Oral hygiene and caries. A review. Acta Odontol Scand. 1981;39:257–65. doi: 10.3109/00016358109162287. [DOI] [PubMed] [Google Scholar]
- 8.Nizel AE. Nutrition counseling for dental caries prevention: A step by step procedure. In: Nizel AE, editor. Nutrition in Preventive Dentistry. Philadelphia, PA: WB Saunders Company; 2013. p. 356. [Google Scholar]
- 9.Lindhe J, Koch G. The effect of supervised oral hygiene on the gingiva of children. Progression and inhibition of gingivitis. J Periodontal Res. 1966;1:260–7. doi: 10.1111/j.1600-0765.1966.tb01870.x. [DOI] [PubMed] [Google Scholar]
- 10.Blinkhorn AS. Influence of social norms on toothbrushing behavior of preschool children. Community Dent Oral Epidemiol. 1978;6:222–6. doi: 10.1111/j.1600-0528.1978.tb01154.x. [DOI] [PubMed] [Google Scholar]
- 11.Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177–87. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. 4th ed. Geneva: WHO; 1997. Oral Health Surveys-Basic Methods. [Google Scholar]
- 13.Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962;65:26–9. doi: 10.14219/jada.archive.1962.0184. [DOI] [PubMed] [Google Scholar]
- 14.Loe H, Silness J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 15.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 16.Honkala E, Nyyssönen V, Knuuttila M, Markkanen H. Effectiveness of children's habitual toothbrushing. J Clin Periodontol. 1986;13:81–5. doi: 10.1111/j.1600-051x.1986.tb01418.x. [DOI] [PubMed] [Google Scholar]
- 17.Ashley FP, Sainsbury RH. The effect of a school-based plaque control programme on caries and gingivitis. A 3-year study in 11 to 14-year-old girls. Br Dent J. 1981;150:41–5. doi: 10.1038/sj.bdj.4804533. [DOI] [PubMed] [Google Scholar]
- 18.Van Palenstein Helderman WH, Munck L, Mushendwa S, van’t Hof MA, Mrema FG. Effect evaluation of an oral health education programme in primary schools in Tanzania. Community Dent Oral Epidemiol. 1997;25:296–300. doi: 10.1111/j.1600-0528.1997.tb00943.x. [DOI] [PubMed] [Google Scholar]
- 19.Moorhead JE, Conti AJ, Marks RG, Cancro LP. The effect of supervised brushing on caries inhibition in school age children. J Clin Dent. 1991;2:97–102. [PubMed] [Google Scholar]
- 20.Agerbaek N, Melsen B, Lind OP, Glavind L, Kristiansen B. Effect of regular small group instruction per se on oral health status of Danish schoolchildren. Community Dent Oral Epidemiol. 1979;7:17–20. doi: 10.1111/j.1600-0528.1979.tb01179.x. [DOI] [PubMed] [Google Scholar]
- 21.Englander HR. Supervised deplaquing and improved gingival health in a school program. J Periodontol. 1979;50:394–6. doi: 10.1902/jop.1979.50.8.394. [DOI] [PubMed] [Google Scholar]
- 22.Sutcliffe P, Rayner JA, Brown MD. Daily supervised toothbrushing in nursery schools. Br Dent J. 1984;157:201–4. doi: 10.1038/sj.bdj.4805460. [DOI] [PubMed] [Google Scholar]
- 23.Hartono SW, Lambri SE, van Palenstein Helderman WH. Effectiveness of primary school-based oral health education in west Java, Indonesia. Int Dent J. 2002;52:137–43. doi: 10.1111/j.1875-595x.2002.tb00618.x. [DOI] [PubMed] [Google Scholar]
- 24.Biesbrock AR, Walter PA, Bartizek RD. Short-term impact of a national dental education program on children's oral health and knowledge. J Clin Dent. 2004;15:93–7. [PubMed] [Google Scholar]
- 25.Horowitz AM, Suomi JD, Peterson JK, Voglesong RH, Mathews BL. Effects of supervised daily dental plaque removal by children: First- year results. J Public Health Dent. 1976;36:193–200. doi: 10.1111/j.1752-7325.1976.tb02596.x. [DOI] [PubMed] [Google Scholar]
- 26.Jeffcoat M. Chemical plaque control: How do you advise your patients? Int Dent J. 1993;43(Suppl 1):415–21. [PubMed] [Google Scholar]


