Abstract
Background:
Identifying factors associated with adherence is of great value in clinical practice. The objective of this study was to investigate medication adherence, beliefs about medicines held by people with chronic illness and whether beliefs influence medication adherence.
Methods:
The study was carried out at primary health care clinic of the Palestinian Medical Military Services in Nablus, Palestine. The beliefs about medicines questionnaire was used to assess beliefs and Morisky medication adherence scale was used to assess adherence.
Results:
A total of 187 patients were interviewed. Most participants (79.6%) agreed or strongly agreed that their medications were necessary for their current health. However, 58.2% of the participants were concerned about having to take their medicines on a regular basis and 57.8% were concerned about becoming dependent on their medicines. None of the demographic and clinical variables was significantly associated with medication adherence. However, multivariate analysis showed that patients who had higher beliefs about medication necessity had higher odds (1.107 [1.023-1.197]) of being adherent. On the other hand, patients who had higher concern beliefs had lower odds (0.908 [0.845-0.975]) of being adherent.
Conclusions:
Beliefs about medicines are a major contributing factor to medication adherence.
Keywords: Adherence, beliefs about medicines, chronic illness, Palestine
Introduction
Medication adherence has important therapeutic and economic consequences.[1,2] Medication adherence is believed to be influenced by factors beyond the traditional demographic and clinical factors.[3,4] In the Arab world, beliefs about medicines and illnesses are supposed to be different than those in Asia and Europe due to differences in culture, religion and degree of public health awareness.[5] Studies about beliefs in medicines in general and particularly its association with medication adherence are very few in the Arab world.[6,7] Therefore, the objectives of this study were to (1) assess medication adherence and beliefs about medicines and to (2) assess potential association between beliefs and medication adherence in patients with chronic diseases.
Methods
Setting and study design
This cross-sectional study was carried out at the primary healthcare clinic of Military Medical Services in Nablus, Palestine. Nablus is a major city in Northern West-Bank of Palestine with approximately more than 200,000 inhabitants. The clinic where the study took place offers medical services and dispenses medications free of charge for Palestinian military personnel. Sample size was calculated using Raosoft sample size calculator (http://www.raosoft.com/samplesize.html) assuming a margin of error of 5%, a total population of patients with chronic illness of approximately 2000 and a response rate of 90% based on the researcher's observation during the pilot study. The estimated sample size will be a minimum of 130 patients. Convenience sampling method was used to recruit the required sample size. Recruitment was carried out by a pharmacist who works at the military medical services and is aware of the working system at the clinic. The recruitment process was carried out daily for 2 consecutive months in 2011. The pharmacist who was in charge of patient recruitment process and data collection visited the clinic daily and stayed in the clinic between 10 am and 1 pm. All patients attending the primary health care clinic during the study period were asked to participate if they report having the following characteristics: Having at least one chronic illness for at least 1 year, taking at least one medication on a regular basis and have not changed their medication in the past 3 months. The exclusion of patients whose prescription medications have been changed more than once in the past 3 months was based on the idea that too many changes in prescribed medicines during a short period of time suggest that patients’ therapeutic regimen has not been stabilized yet and the patient is not familiar with his medications yet. For the purpose of this study, chronic illness was defined as one or more of the followings: Diabetes mellitus (DM), cardiovascular diseases, rheumatoid arthritis (RA) or osteoarthritis. Median duration of chronic illness for the study sample was calculated based on the longest duration of chronic disease in each participant.
Ethical approval
The study objective and protocol was explained to patients and a verbal informed consent was obtained. All aspects of the study protocol, including access to, use of the patient clinical information and interview were authorized by the institutional review board (IRB) and the faculty of graduate studies before initiation of this study. The university IRB committee did not require the investigators to obtain a written consent because our study involved minimal risk and the research protocol did not involve any invasive intervention. However, the IRB required that the statement used to explain the purpose of this study is the same for all patients. The interview with the participants was carried out at a private space in the clinic with no interruption from people who work in the clinic.
Tools
Medication adherence was measured using Morisky medication adherence scale (MMAS-8©).[8] Approval to use and translate the MMAS-8© into Arabic language was obtained from the developer. The translation was carried out according to standard forward and backward method. In the forward translation process the scale was translated into Arabic by language experts. In the backward translation process, the Arabic-translated version was translated back into English language and the back-translated version was sent to the developer for approval. Details of the Arabic translation and its use were described previously.[9] The MMAS-8© is an eight items questionnaire designed to measure medication adherence. It is composed of seven Yes/No questions. The eighth question uses a 5-point Likert scale. For the purpose of this study, patients with a total MMAS-8© score <8 were considered to be non-adherent (poor/medium adherence) while those with a total MMAS-8© score = 8 were considered to be adherent. Beliefs about medicines was assessed using beliefs about medicines questionnaire (BMQ).[10] Approval to use and translate BMQ was obtained from the developer. Translation of BMQ was also carried out according to the standard forward and backward method. BMQ consists of two sections, general and specific. The specific section assesses patients’ beliefs about medications prescribed for a particular illness and comprises two scales assessing personal beliefs about the necessity of prescribed medication for controlling their illness (5 statements) and concerns about the potential adverse consequences of taking it (5 statements). The general section deals with more general beliefs about medicines and comprises two scales, the general-overuse scale addresses views about the way in which medicines are used by doctors (4 statements) and the general-harm scale which assesses beliefs about the degree to which they perceive medicines as essentially harmful. Each statement has a 5-point Likert scale answers (strongly disagree, disagree, uncertain, agree and strongly agree). The answers are scored from 1 (strongly disagree) to 5 (strongly agree). Points of each scale are summed to give a scale score. Higher scores indicate stronger beliefs in the concepts of the scale.
Specific-necessity and specific-concerns scales have 5 items and scores range from 5 to 25. Higher specific-necessity scores represent stronger perceptions of personal need for the medication to maintain health now and in the future. Higher specific-concerns scores represent stronger concerns about the potential negative effects of the medication. The general-overuse and the general-harm scales range from 4 to 20. Higher scores on the general-harm scale represent more negative views about medicines as a whole and a tendency to see medicines as fundamentally harmful, addictive poisons. Higher scores on the general-overuse indicate more negative views about the way in which medicines are prescribed and beliefs that they are overused by doctors.
The interview of each patient took to least 15 min. For patients with multiple chronic diseases, BMQ was applied to the chronic illness, which the patient had for the longest duration. A pilot test on 30 patients was carried out to optimize the Arabic phrasing of the BMQ and MMAS-8© questions. All other variables such as gender, age, marital status, level of education, duration and types of chronic illness and number of medications used regularly were obtained directly from the patient.
Data analysis
The data were coded; entered and analyzed using Statistical Package for Social Sciences (SPSS; SPSS Inc., Chicago, IL, USA) program version 17. Internal consistency was tested using Cronbach's alpha. A commonly accepted level of internal consistency using Cronbach's alpha is 0.7.[11] Descriptive analysis was carried out using median (lower-upper quartiles [Q1-Q3]) or mean ± standard deviation (SD). Categorical data were expressed as numbers with percentages. Association between demographic/clinical variables and level of adherence was tested using Pearson Chi-square test. Associations between individual BMQ items and medication adherence level were assessed with Mann-Whitney U-test and Wilcoxon Z scores were presented. Multivariable logistic regression was conducted using demographic variables which showed a P < 0.05 in bivariate analyses as well as subscales of BMQ. Unadjusted and adjusted odds ratios with 95% confidence intervals were calculated. The a priori level of significance for all analyses was <0.05.
Results
General characteristics of the study sample
During the study period, a total of 220 patients agreed to participate in the study. One hundred and eighty seven met the inclusion criteria while 33 were excluded mostly because they had a recent change in their medication regimen. Those who met the inclusion criteria were interviewed and their responses to belief and adherence scales were analyzed.
The mean ± SD age of the participants was 58.6 ± 10.5 with a median of 60 and a range of 30-87 years. Two-thirds of the participants were males (n = 123; 65.8%). Less than one-third of the participants (n = 56; 29.9%) were elderly. Participants reported an average of 1.9 ± 0.7 chronic illness (median = 2; Q1-Q3: 1-2); more than two-thirds (n = 128; 68.4%) had multiple chronic illnesses. Hypertension (HTN) (136; 72.7%), type 2 DM (98; 52.4%) and cardiac insufficiency (52; 27.8%) were the most frequently reported chronic illness in the study sample. There were 62 (32.6%) patients who had both DM and HTN. Patients reported an average of 5.6 ± 2.7 (median = 5; Q1-Q3: 4-7) medications taken on a regular basis. The mean ± SD and median (Q1-Q3) duration of chronic disease/s for all patients was 8.1 ± 6.9 and 6 (3-11) years respectively. More than half of the participants had less than high school education (n = 99; 52.9%).
Reported adherence of the study sample
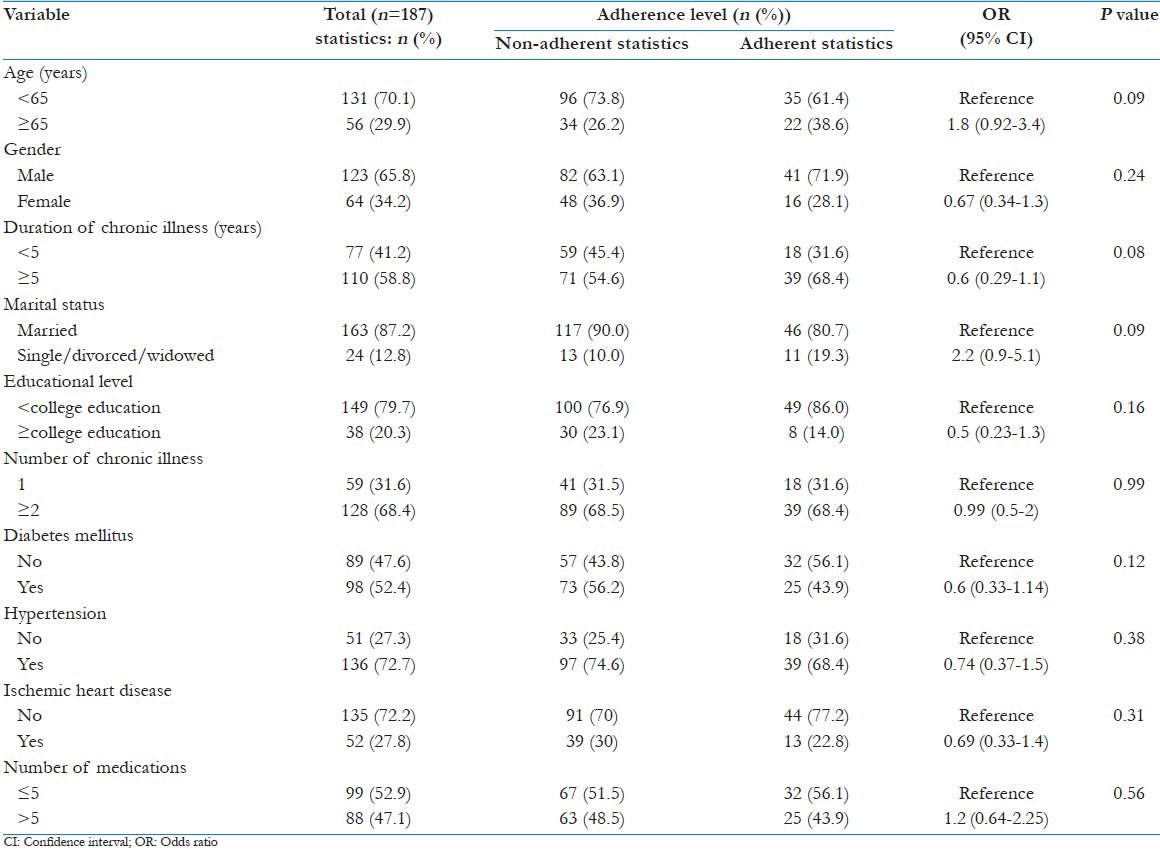
The internal consistency of the MMAS-8© in our study was satisfactory (α =0.7). Fifty-seven (30.5%) patients were adherent (MMAS-8© adherence score = 8) while 130 (69.5%) were non-adherent (MMAS-8© adherence score <8). Univariate analysis showed no significant association between adherence level and any of the tested demographic and clinical variables [Table 1].
Table 1.
Patient characteristic by adherence level
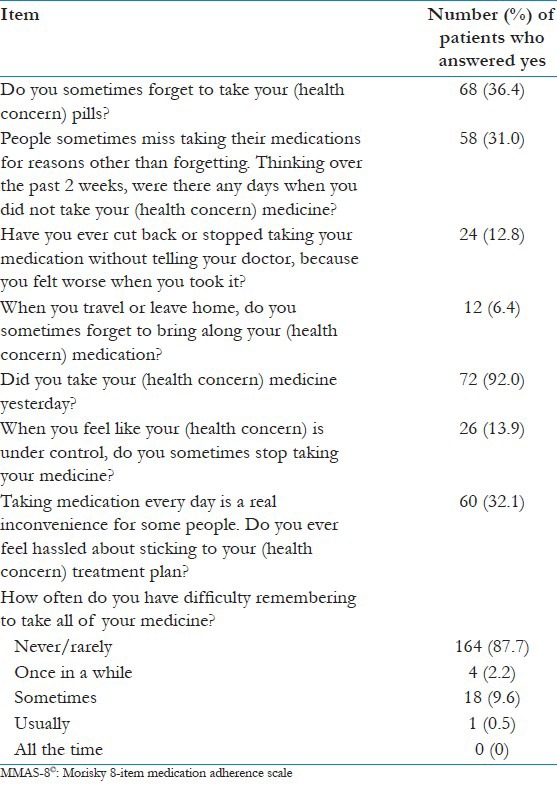
Reported answers to MMAS-8© are presented in Table 2. Slightly more than one-third (36.4%) of the participants reported that they sometimes forgot to take their medications; 31.0% of the participants reported that they did not take their medications on at least one occasion in the 2 weeks before the interview; 12.8% of the participants reported that they discontinued taking their medications without telling their doctor when they felt worse upon taking their medications; 6.4% of the participants reported that they sometimes forgot to take their medications with them when they traveled or left home; 92.0% of the participants reported taking all of their medications on the day before the interview; 13.9% of the participants reported that they stopped taking their medicines when they felt like their symptoms were under control; 32.1% of the participants reported feeling hassled by their treatment plans; and finally 87.7% reported that they never or rarely had difficulty remembering to take all their medicines.
Table 2.
Self-reported medication adherence behavior of study participants as determined by the MMAS-8©
Reported beliefs and its impact on medication adherence
Internal consistency for the BMQ four subscales showed values between α =0.7-0.8. The majority of the participants endorsed the beliefs that (1) their current health depended on their medication and that (2) their medications kept them from getting worse. Concerns about medicines were also reported. Many participants indicated that they are worried about being obliged to take their medicines and about becoming too much dependent on their medications. Many patients endorsed the belief that physicians have too much trust in medicines and that most medicines are addictive. However, few patients endorsed beliefs that medications were harmful [Table 3].
Table 3.
Response to BMQ items and participants’ scores for each item by adherence level
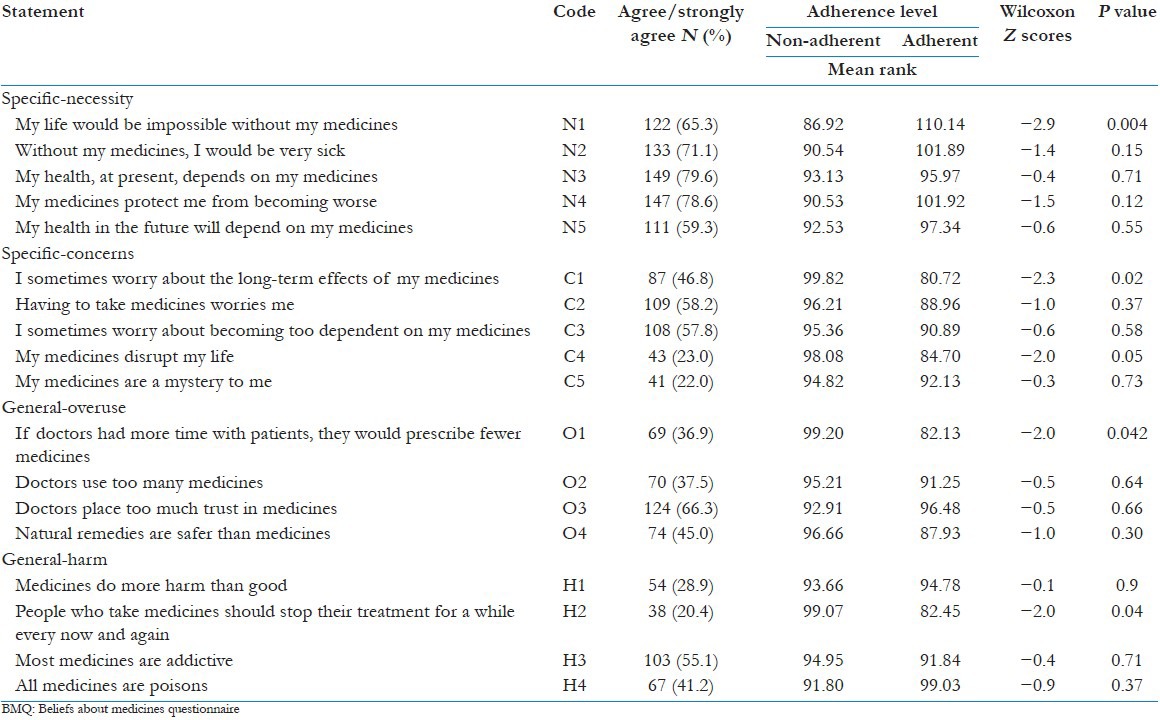
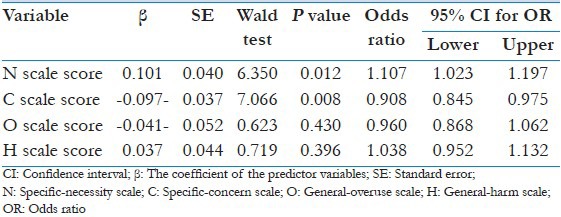
Analysis of belief scores using Mann-Whitney test showed that adherent participants had significantly higher specific-necessity belief (N1), lower specific-concern belief (C1) and lower general-overuse belief (O1) and lower general-harm belief (H2) compared with non-adherent participants [Table 3]. The overall specific-necessity score was higher than the concerns score (P < 0.001). None of the demographic and clinical variables was significantly associated with the level of adherence. However, multivariate analysis showed that patients who had higher necessity beliefs had higher odds (1.107 [1.023-1.197]) of being adherent. On the other hand, patients who had higher concern beliefs had lower odds (0.908 [0.845-0.975]) of being adherent [Table 4].
Table 4.
Independent factors associated with adherence using binary logistic regression analysis
Discussion
Over the past 30 years, a substantial number of reports have been published about medication adherence. In most of these studies, emphasis was made on the relationship between demographic/clinical variables and adherence. However, it seems that most demographic and clinical variables had no or limited predictive ability to explain variations in adherence.[12] The other approach which successfully explained a great portion of medication non-adherence among patients with chronic diseases was behavioral models. Several studies have successfully shown good correlation between beliefs about medicines and medication adherence. A study by Phatak et al., found that beliefs about medicines alone explained 22.4% of variation in non-adherence to chronic drug therapy.[12] A study in Japan by Iihara et al., concluded that beliefs on which individual Japanese patients with chronic diseases attach value were potential factors for intentional non-adherence.[13] A study by Mårdby et al., concluded that increased awareness of the patient's beliefs about medicines is needed and that health care providers should encourage patients to express their views about medicines in order to stimulate concordance and adherence to medication.[14] A study carried out in United States to examine the relationships between beliefs about medications, health literacy and self-reported medication adherence concluded that patients who had negative beliefs about medications reported low medication adherence.[15]
In our study, patients strongly endorsed beliefs that medications are necessary for their health, but also reported concerns about taking medications on a regular basis. Since 46.8% expressed concerns about long-term effects of taking medications, it is important for health care workers to be aware of these concerns and direct patients’ education and intervention to minimize such concerns and consequently minimize non-adherence. For example, patients who take medications for chronic illness like HTN or DM need to know that their medications are not addictive and that medication have an acceptable safety profile for long-term use. A study investigated beliefs about medications held by people with RA found that age and level of formal education had a weak negative association with specific-concern scores.[16] The authors of the study concluded that most people with RA have positive beliefs about the necessity of their medication. However, levels of concern were high and associated with helplessness and non-adherence.[16]
In our study, analysis showed significant association between adherence and specific-necessity and specific-concern. It was interesting to find that medication adherence was not associated with the number of medications used. This might emphasize the idea that it is not the number of medications that affects adherence; rather it is the belief that medicines are important for one's life which determines the level of adherence. Therefore, assessment of medication beliefs may be important for success of medication improvement strategies. Health care providers should address the patient's beliefs about medications in the hope of improving medication adherence.
Our study had some limitations. A self-report method was used to assess medication adherence. Although more precise estimates of medication adherence can be obtained through direct methods, the self-report assessment of medication adherence provided a practical measure for this study. The validity of the Arabic version of adherence and belief scales has not been tested and further studies are needed to confirm the validity of both scales among patients in the Arab world. Regardless, this is one of the few studies in the Arab world to investigate beliefs in medicines and to investigate the association between beliefs and adherence. Caution should be exercised in generalizing our study's findings due to the use of quota sample from one institution. Overestimation of adherence may have occurred because self-reporting was used for assessment. The presence of multiple chronic diseases in most participants in our study made it difficult for us to compare the level of adherence and beliefs in medicines for each category of chronic illness. Studies reported different values for specific-necessity and concerns when BMQ was used in different types of chronic diseases suggesting that the impact of medication belief on adherence is dependent on the nature of the disease.[17,18,19,20,21,22,23,24]
The sample size used in our study was relatively small. No priori calculation of power was conducted which might affect the generalization of our findings. All abovementioned limitations need to be considered when interpreting the findings of our study.
Conclusions
As a conclusion, stronger belief in the necessity or concern of one's medications is significantly associated with high adherence and that assessment of medication belief is important in understanding adherence of chronic medication users. The BMQ may identify people at risk of poor adherence providing opportunities to improve adherence. Our findings are consistent with those obtained by the analysis of 94 (N = 25,072) studies regarding adherence-related beliefs about medicines. The study concluded that higher adherence was associated with stronger perceptions of necessity of treatment, OR = 1.742, 95% CI [1.569, 1.934], P < 0.0001, and fewer concerns about treatment, OR = 0.504, 95% CI: [0.450, 0.564], P < 0.0001.[25]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 2.Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 3.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: Three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–42. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 4.Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 5.Al-Saeedi M, Elzubier AG, Bahnassi AA, Al-Dawood KM. Patterns of belief and use of traditional remedies by diabetic patients in Mecca, Saudi Arabia. East Mediterr Health J. 2003;9:99–107. [PubMed] [Google Scholar]
- 6.Fawzi W, Mohsen AM. Beliefs about medications predict adherence to antidepressants in older adults. (1-11).Int Psychogeriatr. 2012:24. doi: 10.1017/S1041610211001049. [DOI] [PubMed] [Google Scholar]
- 7.Shahin SH, Daly EB. Knowledge, attitudes and beliefs about psychotropic medication among Saudi hospitalized psychiatric patients. Int J Nurs Stud. 1999;36:51–5. doi: 10.1016/s0020-7489(98)00057-1. [DOI] [PubMed] [Google Scholar]
- 8.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Jamous RM, Sweileh WM, Abu-Taha AS, Sawalha AF, Zyoud SH, Morisky DE. Adherence and satisfaction with oral hypoglycemic medications: A pilot study in Palestine. Int J Clin Pharm. 2011;33:942–8. doi: 10.1007/s11096-011-9561-7. [DOI] [PubMed] [Google Scholar]
- 10.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. (1-24).Psychology and health. 1999:14. [Google Scholar]
- 11.Nunnally JC. 2nd ed. New York: McGraw-Hill; 1978. Psychometric Theory. [Google Scholar]
- 12.Phatak HM, Thomas J., 3rd Relationships between beliefs about medications and nonadherence to prescribed chronic medications. Ann Pharmacother. 2006;40:1737–42. doi: 10.1345/aph.1H153. [DOI] [PubMed] [Google Scholar]
- 13.Iihara N, Tsukamoto T, Morita S, Miyoshi C, Takabatake K, Kurosaki Y. Beliefs of chronically ill Japanese patients that lead to intentional non-adherence to medication. J Clin Pharm Ther. 2004;29:417–24. doi: 10.1111/j.1365-2710.2004.00580.x. [DOI] [PubMed] [Google Scholar]
- 14.Mårdby AC, Akerlind I, Jörgensen T. Beliefs about medicines and self-reported adherence among pharmacy clients. Patient Educ Couns. 2007;69:158–64. doi: 10.1016/j.pec.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 15.Gatti ME, Jacobson KL, Gazmararian JA, Schmotzer B, Kripalani S. Relationships between beliefs about medications and adherence. Am J Health Syst Pharm. 2009;66:657–64. doi: 10.2146/ajhp080064. [DOI] [PubMed] [Google Scholar]
- 16.Neame R, Hammond A. Beliefs about medications: A questionnaire survey of people with rheumatoid arthritis. Rheumatology (Oxford) 2005;44:762–7. doi: 10.1093/rheumatology/keh587. [DOI] [PubMed] [Google Scholar]
- 17.Aflakseir A. Role of illness and medication perceptions on adherence to medication in a group of Iranian patients with type 2 diabetes. J Diabetes. 2012;4:243–7. doi: 10.1111/j.1753-0407.2012.00183.x. [DOI] [PubMed] [Google Scholar]
- 18.Cook CL, Wade WE, Martin BC, Perri M., 3rd Concordance among three self-reported measures of medication adherence and pharmacy refill records. J Am Pharm Assoc. 2005;45:151–9. doi: 10.1331/1544345053623573. [DOI] [PubMed] [Google Scholar]
- 19.Jónsdóttir H, Friis S, Horne R, Pettersen KI, Reikvam A, Andreassen OA. Beliefs about medications: Measurement and relationship to adherence in patients with severe mental disorders. Acta Psychiatr Scand. 2009;119:78–84. doi: 10.1111/j.1600-0447.2008.01279.x. [DOI] [PubMed] [Google Scholar]
- 20.Khanderia U, Townsend KA, Erickson SR, Vlasnik J, Prager RL, Eagle KA. Medication adherence following coronary artery bypass graft surgery: Assessment of beliefs and attitudes. Ann Pharmacother. 2008;42:192–9. doi: 10.1345/aph.1K497. [DOI] [PubMed] [Google Scholar]
- 21.Kumar K, Gordon C, Toescu V, Buckley CD, Horne R, Nightingale PG, et al. Beliefs about medicines in patients with rheumatoid arthritis and systemic lupus erythematosus: A comparison between patients of South Asian and White British origin. Rheumatology (Oxford) 2008;47:690–7. doi: 10.1093/rheumatology/ken050. [DOI] [PubMed] [Google Scholar]
- 22.Mahler C, Hermann K, Horne R, Jank S, Haefeli WE, Szecsenyi J. Patients’ beliefs about medicines in a primary care setting in Germany. J Eval Clin Pract. 2012;18:409–13. doi: 10.1111/j.1365-2753.2010.01589.x. [DOI] [PubMed] [Google Scholar]
- 23.Menckeberg TT, Bouvy ML, Bracke M, Kaptein AA, Leufkens HG, Raaijmakers JA, et al. Beliefs about medicines predict refill adherence to inhaled corticosteroids. J Psychosom Res. 2008;64:47–54. doi: 10.1016/j.jpsychores.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 24.Saks EK, Wiebe DJ, Cory LA, Sammel MD, Arya LA. Beliefs about medications as a predictor of treatment adherence in women with urinary incontinence. J Womens Health (Larchmt) 2012;21:440–6. doi: 10.1089/jwh.2011.2952. [DOI] [PubMed] [Google Scholar]
- 25.Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the necessity-concerns framework. PloS One. 2013:8. doi: 10.1371/journal.pone.0080633. e80633. [DOI] [PMC free article] [PubMed] [Google Scholar]


