Abstract
Background:
Women between 12 and 50 years are in the reproductive age. The likelihood of or actual presence of pregnancy should be ruled out before they are exposed to medical ionizing radiation. Fetal exposure to ionizing radiation can either induce malformation (teratogenic) or cancer. They should be exposed only when it is safe for the fetus or when the benefit far outweighs the risk in urgent medical conditions. The radiation dose in medical imaging is generally below the threshold to induce malformation (100 mGy) in the fetus, but there is indeed no safe level as the risk of cancer induction later in life can occur at any dose. The referring physician must obtain the last menstrual period (LMP) and sometimes carry out pregnancy test before sending their patients for examinations using ionizing radiation. However, there are circumstances in which these rules are waived.
Objective:
The purpose of the study is to evaluate the role of the referring physician in the radiation protection of the fetus using the LMP. Subjects and Methods: This is a prospective study over a 2-month period. All the request forms of menstruating women aged 12-50 years sent for conventional radiography are included in the study.
Results:
One percent provided the LMP in the request forms. 0.6% (one) of our subjects was sure she is pregnant, but 13.7% (25) had an overdue menstruation.
Conclusion:
The level of compliance of the physicians with the referral guidelines for women of reproductive age is poor.
Keywords: Last menstrual period, radiation protection, referring physician, reproductive age
Introduction
The state of pregnancy is one associated with reduced immunity and increased susceptibility to infection than the rest of the healthy population. Pregnant women are also not spared from the different forms of trauma. Due to ill health or injury, the referring physician can inadvertently send a pregnant woman for a radiological examination that utilizes ionizing radiation, especially at the early stage. According to the International Commission on Radiological Protection (ICRP), thousands of pregnant women are exposed to medical ionizing radiation each year.[1] The knowledge of the possible hazards to patients and the fetus at doses used for different imaging procedures has been widely researched and safety measures have been recommended. Radiation safety is said to be a matter of taking appropriate actions to limit the risk to a level well-justified by the benefit.[2] Practice guidelines are developed to help achieve safety. One of the specific goals of the radiological practice guideline is to provide guidance on when and how to screen for pregnancy prior to imaging examinations using ionizing radiation.[2] A major part of the actions by the International Atomic Energy Agency (IAEA) prior to 2012 has been on the optimization process, which involved regulating the practice of imaging specialists rather than the referring physician.[3] This is partly achieved with quality assurance programs through regular analysis of repeated examinations using ionizing radiation which has been done in our center and this revealed that junior radiographers and underexposure are responsible for most of the repeats.[4] Member states of IAEA have expressed the desire to extend radiation protection actions to cover “unnecessary exposures” due to requests from physicians, which in some situations have been reported to be as much as 50% of radiation exposure from diagnostic imaging.[3] Also, there are reports that indicate a lack of awareness on the part of some referring physicians concerning the radiation dose involved in radiological examinations, the possible hazards, and practice guidelines. This situation, along with lack of formal training in most countries, requires actions with referring physicians similar to those the IAEA carried out with imaging specialists.[3] The risk of radiation induced cancer according to ICRP might be three times as high as for the average population.[5] In a tertiary center such as ours and indeed the country, there is no formal training of referring physicians on radiation safety and no literature exist evaluating the radiation protection of the fetus using the last menstrual period (LMP). Our study will assist the department, hospital management, and other relevant agencies to initiate steps to improve the level of awareness of the referring physicians concerning radiation safety and to develop a protocol for the radiological examination of women of reproductive age.
Subjects and Methods
This is a prospective study focused on women aged 12-50 years sent for conventional radiographic examinations over a 2-month period; April and May, 2013. One hundred and ninety-eight women were within the age group, but 13 were menopausal and two had not attained menarche, so only 183 were included in the study. Their request forms are assessed by the receptionist to see if the referring physician provided the LMP and other relevant information about pregnancy. If this information is not provided, this is obtained by the receptionist. She then enters the LMP into the request form to enable the radiographer decide if the examination is to be done that day, rescheduled, or if the radiologist need to informed. The information on the request forms is later analyzed and they are sorted into the different referring departments. The examinations are grouped based on those that involve direct or indirect irradiation of the uterus and those that deliver low dose or relatively higher dose to the uterus. The day of the menstrual cycle when the women were sent for the examination is also calculated from the LMP and the level of compliance with the 10-day and 28-day rules is assessed.
Results
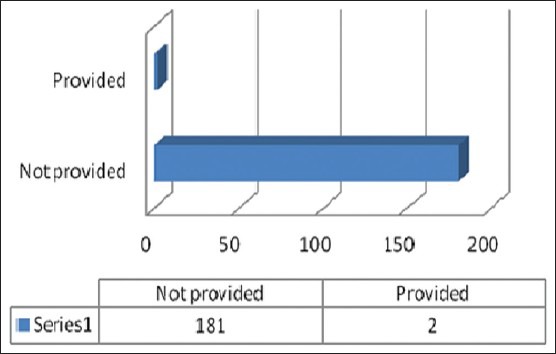
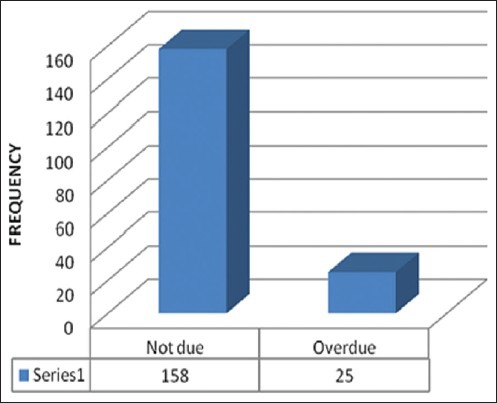
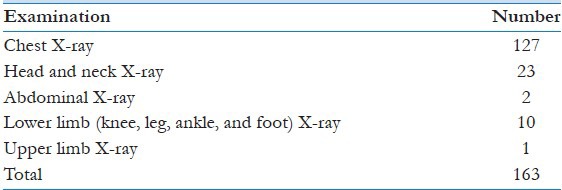
One hundred and eighty-three patients met the inclusion criteria. Table 1 shows the distribution of the referring departments. One hundred and eighty-one (98.9%) were sent for routine and two (1.1%) for contrast examinations. The different types of examinations and relative radiation dose are highlighted in Table 2. The referring physicians provided the LMP in the radiological request form of two (1.1%) of our subjects [Figure 1] and only one (0.6%) was sure she is pregnant. Figure 2 shows the menstrual status of the subjects. The “10-day rule” was not obeyed in 28 (15.5%) cases and the “28-day rule” in two (100%). Twenty-one (11.5%) of our subjects were sent for examinations that directly irradiate the uterus, but amongst those with overdue menses, four (16%) involved low dose exposure to the uterus and two (8%) relatively higher dose contrast examinations (intravenous urography (IVU) and hysterosalpingography (HSG)). Table 3 shows the examinations that directly irradiate the uterus, while Table 4 show examinations that do not irradiate and indirectly irradiates the uterus.
Table 1.
Distribution of the referring departments
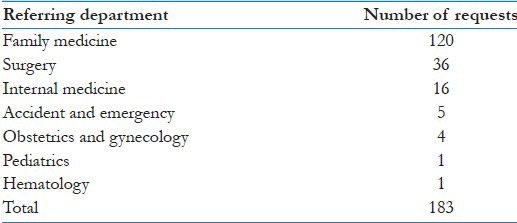
Table 2.
Radiation dose to the uterus
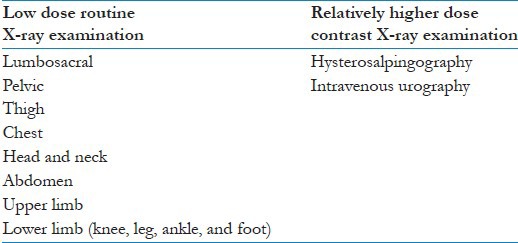
Figure 1.
Provision of last menstrual period (LMP) or pregnancy status in the request forms
Figure 2.
Menstruation status
Table 3.
Examinations that directly irradiate the uterus
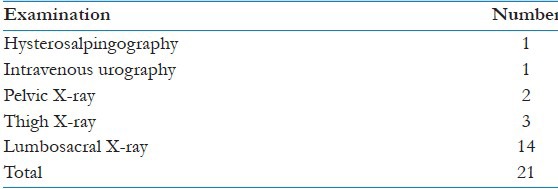
Table 4.
Examinations that do not irradiate and indirectly irradiate the uterus
Discussion
According to the different guidelines, the referring physicians play an important role in screening patients and in proper documentation of the information gathered before sending them for appropriate radiological investigation. They have the prime responsibility to identify pregnant patients.[6] They have to provide the practitioners (radiologist and radiographer) with all relevant information as part of the examination request.[7] This includes supply of the LMP.[8] Patients usually can supply adequate information to assess the possibility of pregnancy.[5] From our study, most of the referring physicians did not supply the LMP (98.9%) or rule out pregnancy before sending women of reproductive age for ionizing radiological examinations. This is probably due to lack of awareness of the possible risk of this type of radiation to a developing embryo or fetus. This level of awareness is contrary to the observation of Ratnapalan et al., who carried out a survey on 400 family physicians and 100 obstetricians, and found that these doctors had a perception of a high teratogenic risk associated with radiation, so they exercised restrain in sending pregnant patient for ionizing radiological examinations.[9]
Though only one (0.6%) woman in our study was sure of pregnancy, another 25 (13.7%) could be pregnant based on an overdue menses ranging from 29 to 71 days. In a bid to protect the developing embryo or fetus from being exposed to the harmful effects of ionizing radiation, examinations of women of child-bearing age are restricted to certain days of their menstrual cycle. Based on the knowledge of the variable radiation dose of different examinations and organogenesis, the “10-day and 28-day rules” are used whenever possible to confine exposure of women in the reproductive age to ionizing radiation to within these days following the onset of menstruation. Generally, for examinations that deliver low radiation dose to the uterus, that is, non-contrast X-rays of the proximal thigh, pelvis and abdomen and examinations at remote sites (head and neck, upper limbs, lower limbs except the upper thigh and chest), the “28-days rule” is applied; while the “10-days rule” is applicable to relatively high radiation dose examinations (>10 mGy to fetus) such as pelvic computed tomography (CT) and diagnostic fluoroscopy of the abdomen and pelvis such as barium enema and IVU.[10] HSG also falls into the latter category. The 25 patients with overdue menses should have been tested for pregnancy before being sent for examinations using ionizing radiation, especially those involving direct irradiation of the uterus because the focus of radiation protection in early pregnancy has shifted to a missed menstrual period.[3] Because of inadvertent exposure of the conceptus, some facilities insist on documenting the pregnancy status before an order for radiological examination in women of reproductive age is accepted.[2] This seems justified by the study carried out by Mossan et al., who observed that 1% of women of child bearing age who underwent abdominal X-ray examination were unknowingly pregnant in the first trimester.[11]
A similar study in trauma patients demonstrated that 2.9% were pregnant and the unidentified pregnancy rate was 0.3%.[12] There are, however, conditions in which the rules and the enquiry about pregnancy status are waived (not sexually active, using an effective form of birth control, or biologically incapable of conceiving).[5,8] A waiver can also be requested in urgent medical situations and the radiologist must document the referring physician who requested for it[1] and the reason for the waiver.[13] Though the LMP was not provided in 99% of the request forms in our study, most of the examinations rendered low radiation dose to and do not involve direct irradiation of the uterus. One hundred and eighty-one (98.9%) patients in our study were sent for routine X-ray examinations and 16 (8.7%) of these involved the back, hip, and pelvis, which according to the American College of Radiology are not likely to pose a serious risk to the child.[14] When the patient is known to be pregnant, the radiographer informs the radiologist who then informs the referring physician and the patient about possible limited radiation risk to fetus based on the gestational age, radiation dose, and region of the body to be examined. The examination can be cancelled and replaced with a nonionizing alternative, rescheduled, or modified to reduce the likelihood of direct radiation exposure to the conceptus. If the examination with ionizing radiation is the best option, the referring physician gives a waiver and the patient signs the consent form.[1] The medical physicist is then invited to discuss the means by which the risk can be reasonably limited and to estimate the absorbed radiation dose received by the fetus using the exposure factors and additional external dose monitoring devices placed above and below the patient's pelvis.[2] A vast majority of routine diagnostic studies deliver less than 20 mGy to the uterus and a single-phase acquisition CT of the abdomen including pelvis usually deliver less than 35 mGy.[15] These doses are not teratogenic[16] because they are below the threshold radiation dose for induced fetal malformation (100-200 mGy). However, cancer induction can occur later in life at any dose if the women were not screened in our department.[1]
Conclusion
Most of the referring physicians are currently not playing their role in preventing exposure of the developing embryo/fetus to ionizing radiation. A lot needs to be done to raise their level of awareness on the radiation dose, possible risks, and practice/referral guidelines for the various imaging modalities. As part of the awareness campaign, regular seminars should be organized for the physicians and every radiological facility should return the request forms of women in the reproductive age group that do not provide the LMP, pregnancy status, or a waiver from the referring physician.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Vol. 84. ICRP Publication; 2000. International commission on radiological protection. Pregnancy and medical radiation; pp. 1–43. [DOI] [PubMed] [Google Scholar]
- 2.ACR practise guideline for imaging pregnant or potentially pregnant adolescents and women with ionising radiation. 2008 Res 26. [Google Scholar]
- 3.Pregnancy and radiation protection in diagnostic radiology. IAEA Radiation protection of patients (RPOP) 2012 [Google Scholar]
- 4.Akintomide AO, Egbe NO, Bassey DE, Eduwem DU, Oyama EA. An analysis of repeated examinations in conventional film-screen radiography (FSR) J Assoc Radiographers Nigeria. 2011;25:14–20. [Google Scholar]
- 5.ICRP Publication 60; 1991. International commission of radiological protection. 1990. Recommendations of the international commission of radiological protection. [Google Scholar]
- 6.Referral guidelines for imaging. Radiation protection 118. (c) European communities. 2001 [Google Scholar]
- 7.Radiological protection institute of Ireland; 2010. Guidelines on the protection of the unborn child during diagnostic medical exposures. [Google Scholar]
- 8.London: HMSO; 1972. Department of health and social security, code of practise for the protection of persons against ionising radiations arising from medical and dental use. [Google Scholar]
- 9.Ratnapalan S, Bona N, Chandra K, Koen G. Physician's perceptions of teratogenic risk associated with radiography and CT during early pregnancy. AJR AM J Roentgenol. 2004;182:1107–9. doi: 10.2214/ajr.182.5.1821107. [DOI] [PubMed] [Google Scholar]
- 10.National radiation protection board. Board statement on diagnostic medical exposure to ionising radiation during pregnancy and estimate of late radiation risks to the UK population. Document NRPB. 1993;4:1–14. [Google Scholar]
- 11.Mossan KL, Hill LT. Radiation risks in pregnancy. Obstet Gynecol. 1982;60:237–42. [PubMed] [Google Scholar]
- 12.Bochicchio GV, Napolitano LM, Haan J, Champion H, Scalea T. Incidental pregnancy in trauma patients. J Am Coll Surg. 2001;192:566–69. doi: 10.1016/s1072-7515(01)00818-3. [DOI] [PubMed] [Google Scholar]
- 13.Thompson SK, Goldman SM, Shah KB, Chen PC, Wagner LK, Corl FM, et al. Acute non traumatic maternal illness in pregnancy: Imaging approaches. Emerg Radiol. 2005;11:199–212. doi: 10.1007/s10140-004-0385-9. [DOI] [PubMed] [Google Scholar]
- 14.Radiologyinfo.org; 2010. American College of Radiology/Radiological society of North American. Pregnancy and X-rays. [Google Scholar]
- 15.Mccollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, et al. Radiation exposure and pregnancy: When should we be concerned? Radiographics. 2007;27:909–17. doi: 10.1148/rg.274065149. [DOI] [PubMed] [Google Scholar]
- 16.Cohen-Kerem R, Nulman I, Abramow-Newerly M, Medina D, Maze R, Brent RL, et al. Diagnostic radiation in pregnancy: Perception versus true risks. J Obstet Gynaecol Can. 2006;28:43–8. doi: 10.1016/S1701-2163(16)32039-4. [DOI] [PubMed] [Google Scholar]


