Abstract
Background:
Settings-based approach for health promotion includes conducting risk factor surveillance as one of its component. It was aimed to estimate the prevalence of CVD risk factors among group C employees of tertiary care hospital in south India.
Materials and Methods:
A cross-sectional survey was conducted among 400 group C employees aged ≥20 years using the WHO “STEPwise approach to surveillance of non-communicable diseases” (STEPS) methodology. Standardized international protocols were used to measure behavioral risk factors (smoking, alcohol consumption, fruit and vegetable consumption, physical activity) and physical characteristics (weight, waist and hip circumferences, height, and blood pressure). Multivariate analysis was done to predict the factors, which carry independent risk of hypertension. Risk factor profiling of the staff was done using WHO/ISH risk prediction chart to calculate the 10-year risk of a fatal or non-fatal major cardiovascular events (myocardial infarction or stroke), according to age, gender, blood pressure, smoking status, and presence or absence of diabetes mellitus.
Results:
Mean age in years was 40.9 (±10.4), and men constituted 81.3% of study population. Prevalence of major cardiovascular risk factors was as follows: Current smokers 12.3% men, regular alcohol intake 33.2% among men, overweight (≥23 kg/m2) 74.5%, central obesity 78.7%, hypertension 38.8%, and history of diabetes mellitus 13.2%. Age, gender, physical inactivity, obesity, and family history of hypertension were found to be independently associated with hypertension. Four percent participants had a >10% risk of developing CVD in next 10 years.
Conclusion:
The prevalence of CVD risk factors is high in the sample population. Employee wellness program should be started in the institute to combat the burden of cardiovascular diseases.
Keywords: Cardio-vascular disease, employee, risk factor profile
Introduction
Cardiovascular diseases (CVD) will be the largest cause of death and disability in India by 2020.[1] Much of this enormous burden is already evident in urban as well as semi-urban and slum dwellings across India, where increasing lifespan and rapid acquisition of adverse lifestyles related to demographic transition are thought to have contributed to rising prevalence of chronic disease determinants like smoking, physical inactivity, improper diet, stress and their ensuing outcomes such as obesity, hypertension, and type 2 diabetes.[2,3,4,5]
The workplace is increasingly being used as a setting for health promotion and preventive health activities; not only to prevent occupational injury, but to assess and improve worker's overall health.[6,7]
Settings-based approach for health promotion has been proposed by World Health Organization for improving the population health. One of the components of this approach is to focus on health of employees’ workplaces by conducting risk factor surveillance.[8] Tertiary care hospitals with their intramural resources and healthcare infrastructure are ideal for initiating preventive and promotional activities, for which baseline data on prevalence of CVD risk factors is essential.[9] Group C staffs are public servants in non-supervisory/non-administrative roles e.g., clerks, assistants, typist, stenographer, telephone operator etc., While being vulnerable for cardiovascular diseases, risk factor assessment in this group is limited as compared to group A and B staffs. So, we estimated the prevalence of CVD risk factors among group C employees of JIPMER, a tertiary care hospital in Puducherry, South India.
Materials and Methods
Study setting
A cross-sectional study was carried out in JIPMER, Puducherry in July and August 2011. At 95% CI and 80% power, for 20% prevalence of hypertension,[10] minimum sample to be covered was 384 considering 20% relative precision. Accounting for the non-response rate of 4%, it was decided to cover 400 group C staff. Group C staffs of ≥20 years and have been working in JIPMER for more than 1 year were included in the study after taking informed written consent. The study was approved by institute ethics committee.
Study procedure
Out of 1706 group C staff members who were employed during the study period, 400 employees were selected purposively from 35 departments of JIPMER, Pondicherry. After obtaining administrative clearance from institute, study subjects were interviewed using adapted WHO STEPS instrument (Step 1),[11] after obtaining written informed consent. STEPS instrument is a standard tool proposed by WHO for surveillance of NCD risk factors and seeks information on core socio-demographic information (education, occupation, and income), core behavioral measures (self-reported tobacco use, alcohol intake, diet, and physical activity), and physical measurements (weight, height, blood pressure, waist and hip circumference). The investigator was trained in the interview techniques and conducting anthropometric measurements (height, weight, waist and hip circumference, and blood pressure) as per standard protocols.[12,13]
Risk factor profiling of the staff was done using WHO/ISH risk prediction Chart.[14] WHO/ISH risk prediction charts indicate 10-year risk of a fatal or non-fatal major cardiovascular events (myocardial infarction or stroke), according to age, gender, blood pressure, smoking status, total blood cholesterol, and presence or absence of diabetes mellitus. The charts provide approximate estimates of CVD risk in people who do not have established coronary heart disease, stroke, or other atherosclerotic disease.
Statistical analysis
Statistical package SPSS (version 16.0) was used for the analyses. Prevalence rates were calculated for the risk factors and presented as percentages. Continuous data are given as mean (± standard deviation). Categorical variables have been compared using Fisher's exact test or Chi-square test for difference of proportion. We investigated association of risk factors for hypertension by calculating odds ratio (95% CI) in the univariate logistic regression. Age, gender, marital status, physical activity, obesity, waist hip ratio, family history of hypertension, and current alcohol use showed significantly association with hypertension. These variables were tested for independent association in multivariate logistic regression model using backward method. All analyses were two-tailed, and P < 0.05 was considered statistically significant.
Results
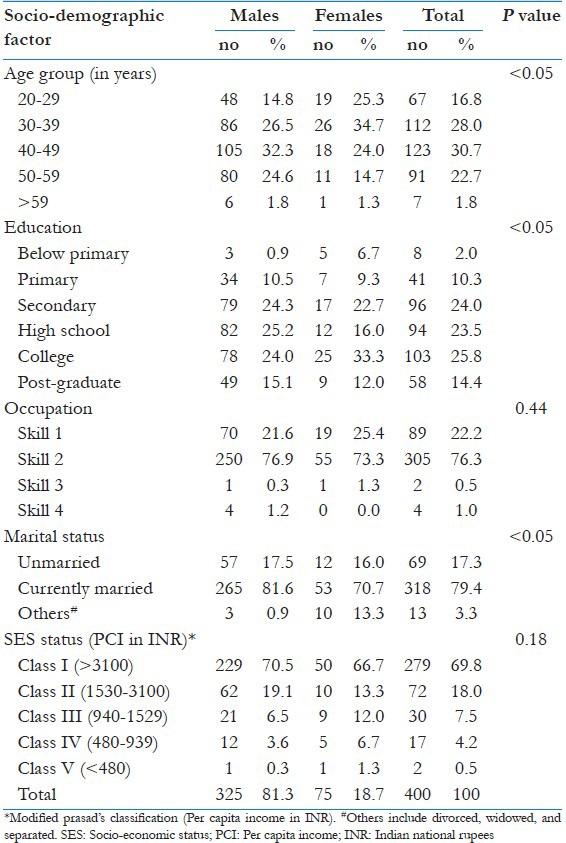
The survey comprised of 400 participants, of whom all consented for participation. The mean age of study population was 40.9 (±10.4) years with majority being males 81.3% (n = 325). Selected socio-demographic parameters of the participants are presented in Table 1.
Table 1.
Socio-demographic profile of study subjects
Prevalence of behavioral risk factors
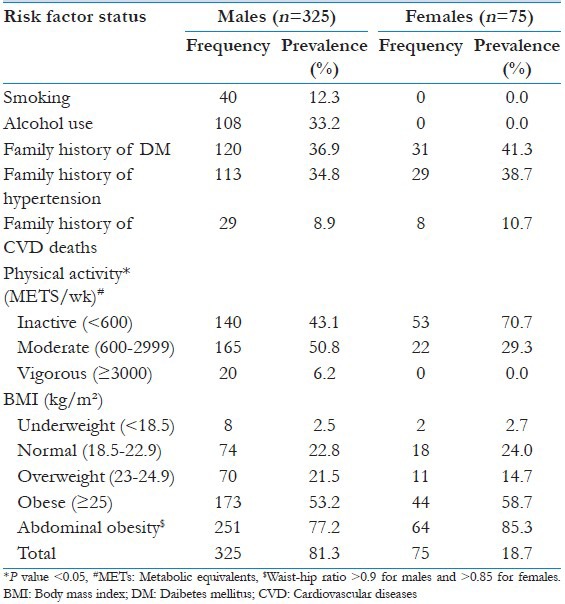
The distribution of behavioral risk factors for cardiovascular risk factors is shown in Table 2. In the study population, none of the women were using alcohol or any form of tobacco. Among men, prevalence of current smoking was 12.3% (95% CI: 9.1-16.2), of whom two-third (9.2%) smoked daily. About one-third men (n = 108) consumed alcohol at least once in the past 12 months, of whom 9 (2.8%) consumed it daily.
Table 2.
Prevalence of risk factors in the study population
On an average, participants ate fruits and vegetables 3.4 (±2.5) and 6.5 (±1.4) days per week, respectively (not shown in table). Sixteen percent didn’t eat fruits at all, while only 25% ate fruits daily in the last week. Almost everyone took at least one serving of vegetable each day. One, two, and three servings of vegetable were taken by 58.5%, 38.2%, and 2.8% participants, respectively. When asked to the subjects to describe about their salt intake, 8.8% reported that they took extra helpings of salt. The per capita per day oil consumption in milliliters ranged from 143-2500 with mean consumption of 893.5 (±360.7). Twenty percent subjects consumed more than recommended oil amount (1000 ml/day).
Of the 400 subjects, 37.8%, 35.5%, and 9.3% have had family history of diabetes, hypertension, and CVD mortality, respectively [Table 2]. Physical inactivity was found to be more among women than men (70.7% Vs 43.2%) with difference being statistically significant (P < 0.001).
Three-fourth [74.5% (95% CI: 70.1%-78.6%)] of the study group were overweight or obese, almost equally in men and women. Of total subjects, 54.2% were obese, 20.3% were overweight, and 2.3% were underweight. Only 23% of the study population was normal weight. Central obesity as measured by waist circumference was quite prevalent [79.5% (95% CI 74.53%-82.55%)] in group C staff with higher prevalence among women than men (85.3% Vs 77.2%).
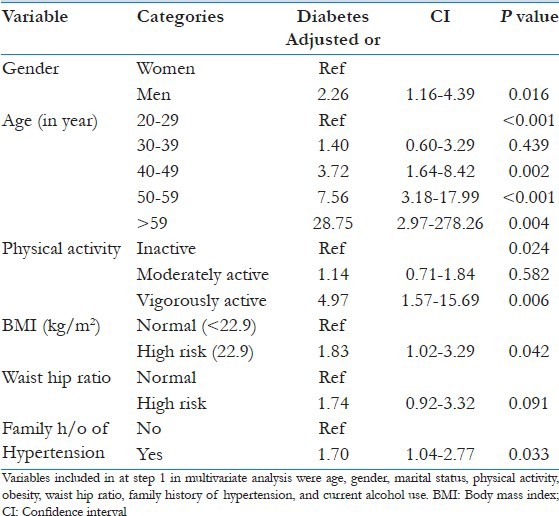
There was significant difference among men and women regarding diseased status [Table 3]. Higher proportion of men than women had a personal history of diabetes [13.2% Vs 2.7% (P < 0.009)] and hypertension [25.5% Vs 14.7% (P = 0.045)]. Around half of the study population had pre-hypertension, and only 27.2% had normal blood pressure. The prevalence of hypertension was 38.8% (95% CI: 34.1%-43.6%)], of whom 40% were newly diagnosed. Men had two times higher prevalence than women, the difference being statistically significant [42.8% Vs 21.3% (P < 0.001)]. Multivariate logistic regression showed that age, gender, physical inactivity, obesity, and family history of hypertension were independently associated with hypertension [Table 4].
Table 3.
Prevalence of morbidities among study subjects
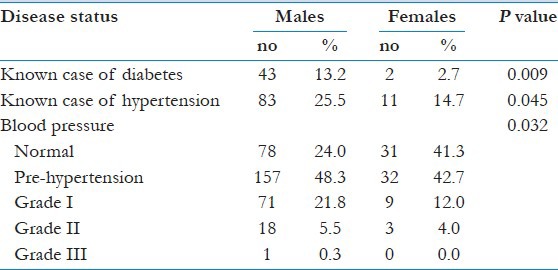
Table 4.
Multivariate analysis of risk factors of hypertension by backward logistic regression
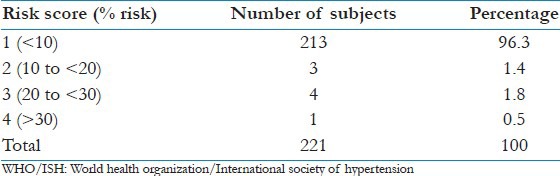
Risk profiling of group C employee
WHO/ISH risk assessment chart was used to predict the CVD risk among group C employee with more than 40 years age, which constituted 55% (n = 221) of total population [Table 5]. Risk score was based on the age, tobacco use, gender, and blood pressure level of the individual. Risk assessment showed that 3.7% subjects had >10% risk of developing cardiovascular disease in next 10 years.
Table 5.
10 year risk of cardiovascular disease according to WHO/ISH risk prediction chart
Discussion
NCDs are becoming of serious concern, accounting for 52% of deaths and 38% of disease burden in the WHO South East Asia Region. Eighty percent of total deaths due to non-communicable diseases occur in the low income countries.[15] Our study provided an opportunity to study the influence of socio-economic factors on the prevalence of cardiovascular risk factors among group C staff of tertiary care center in South India. We found high prevalence of obesity, abdominal obesity, and hypertension in this working group.
Nearly 10% men were daily smokers. This prevalence was lower than that observed from other studies in non-hospital work settings and population-based studies where it ranged from 13-36%.[9,16,17,18,19] This might be due to the awareness in the hospital-based setting. None of the females use tobacco products in our study population, which is common practice in traditional Indian society.
Fifty percent of the subjects were having sedentary lifestyle with high prevalence among women and higher age groups. As compared to other studies from industrial setting, the prevalence was very high where it ranged from 3-17%.[9,16,17,18] Prevalence of physical inactivity was higher in study group. The clustering of other NCD risk factors was seen in the inactive population. Accordingly, prevalence of overweight, obesity, and abdominal obesity was higher in our population as compared to other industrial settings.[9,16,17,18,19] This could be due to better socio-economic status and better work profile.
We observed that for only one in four consumed fruits daily, and the quantity consumed was lower than recommended. This is in accordance with findings from study on south Asians.[20] This emphasizes need to improve awareness among staffs to increase fruit and vegetable intake.
High prevalence of hypertension (25.5%) was observed in our study. Similar findings are reported from other work setting-based studies.[9,16,17,18,21,22] A cross-sectional survey was conducted among a total of 453 individuals aged 30 years and above among administrative staffs of AIIMS, New Delhi reported a high prevalence of major cardiovascular risk factors - current smoking 58 (12.8%), tobacco consumption 26 (5.7%), family history of coronary artery disease 79 (17.4%), diabetes mellitus 25 (5.8%), and hypertension 94 (20.7%).[22] But, prevalence was higher than that of general population[19] where it was 15.7%. Of all the hypertensives detected in the study, 40% were newly diagnosed. And among known hypertensives, 40% had uncontrolled blood pressure. This might be due to the less awareness level among employees about NCDs and absence of regular screening program even in tertiary care center. Thus, health education among employees and also sensitizing physicians for advocating screening can improve early detection and management.
It was found that the almost 4% participants had a >10% risk of developing CVD in next 10 years and majority (96.3%) belonged to low (<10%) risk of developing cardiovascular disease. But, low risk does not mean “no” risk. So, conservative management focusing on lifestyle interventions are advised, which can have a positive health impact. Another study reported the prevalence of WHO/ISH “high CVD risk” (≥20% chance of developing a cardiovascular event over 10 years) of 6%, 2.3%, and 1.3% in Mongolia, Malaysia, and Cambodia, respectively.[23] Our findings were similar to a study using similar methodology to classify cardiovascular risk was categorized in a cross-sectional study of 8,625 randomly selected people aged 40-80 years (mean age, 54.6 years) from defined geographic regions of Nigeria, Iran, China, Pakistan, Georgia, Nepal, Cuba, and Sri Lanka. The study reported a large fraction (90.04.6 years) from defined population has a 10-year cardiovascular risk <20%.[24]
The strength of the study was a comprehensive survey of risk factors using WHO stepwise approach using standardized tools. Data collection was done by single trained investigator, and subjects were interviewed under adequate privacy and comfortable situation to avoid information bias. We included group C staffs who constitute vulnerable and probably least health conscious population in health care setting. In the study group, males constituted 80% population. In limitation, sampling was purposive and may not be representative of the group C staffs working in hospital. Biochemical parameters like fasting blood glucose and lipid profile were not tested due to logistic reasons.
The group C employees of the tertiary care hospital in south India have high prevalence of cardiovascular risk factors. This might put them at the risk of increased cardiovascular morbidity and mortality in near future. There is need to take measures to promote healthy lifestyle, regular screening for NCDs and its risk factors, and appropriate management of the diseased hospital staff population. Policy measures that create conducive environments for quitting tobacco, engaging in physical activity, and consuming healthy diets are necessary to promote behavioral change, which will benefit this working population.
The study has relevance to all primary care physicians; first to screen and adopt appropriate methods of lifestyle modification among the staffs and second to carry out screening program for risk stratification in different settings as proposed under settings-based approach by World Health organization for prevention and control of non-communicable diseases.
Screening of group C staffs in a sample population gave us an idea about the prevalence of CVD risk factors distribution. We educated the staff members regarding various lifestyle parameters for prevention and control of cardiovascular diseases. Our results reinforce the need for low-cost workplace intervention programs. An intervention is being planned to promote healthy lifestyle among the JIPMER group C staff members.
Acknowledgment
This project was carried out under the aegis of ICMR-STS 2011 project. We would like to acknowledge ICMR for the opportunity and financial support. We would like to thank all the participants for their cooperation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.World Health Organization. Geneva: WHO; 2002. The World Health Report 2002. [Google Scholar]
- 2.Reddy KS. Rising burden of cardiovascular disease in Indians. In: Sethi KK, editor. Coronary Artery Disease in Indians. A Global Perspective. Mumbai: Cardiological Society of India; 1998. [Google Scholar]
- 3.Kar SS, Thakur JS, Jain S, Kumar R. Cardiovascular disease risk management in a primary health care setting of North India. Indian Heart J. 2008;60:19–25. [PubMed] [Google Scholar]
- 4.Gupta R, Gupta VP, Sarna M, Bhatnagar S, Thanvi J, Sharma V, et al. Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J. 2002;54:59–66. [PubMed] [Google Scholar]
- 5.Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, et al. Are the urban poor vulnerable to non-communicable diseases? A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Natl Med J India. 2007;20:115–20. [PubMed] [Google Scholar]
- 6.World Health Organization. Geneva: WHO; 2010. [Last accessed on 2011 Jun 15]. Healthy Workplaces: A Model For Action: For Employers, Workers, Policymakers and Practitioners. Available from: http://www.whoindia.org/LinkFiles/NMH_Resources_Healthy_Workplaces_a_ model_for_action.pdf . [Google Scholar]
- 7.World Health Organization. Geneva: WHO; 2005. [Last accessed on 2012 Jun 15]. The Bangkok Charter for health promotion in a globalized world. Available from: http://www.who.int/healthpromotion/conferences/6gchp/hpr_050829_‥20BCHP.pdf . [Google Scholar]
- 8.World Health Organization. Geneva: WHO; 2009. 2008-2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. [Google Scholar]
- 9.Prabhakaran D, Shah P, Chaturvedi V, Ramakrishnan L, Manhapra A, Reddy KS. Cardiovascular risk factor prevalence among men in a large industry of northern India. Natl Med J India. 2005;18:59–65. [PubMed] [Google Scholar]
- 10.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai: The Chennai Urban Rural Epidemiology Study (CURES-52) J Assoc Physicians India. 2007;55:326–32. [PubMed] [Google Scholar]
- 11.World Health Organization. Geneva: WHO; 2003. [Last accessed on 2011 Jan 26]. The WHO STEP Wise Approach to Chronic Disease Risk Factor Surveillance (STEPS)-Instrument v2.1. Available from: ncd_surveillance@who.int . [Google Scholar]
- 12.Rose GA, Blackburn H, Gillum RF, Prineas RJ. Geneva: World Health Organization; 1982. Physical Examination: Cardiovascular Survey Methods; pp. 85–7. [Google Scholar]
- 13.Beevers G, Lip GY, O’Brien E. ABC of hypertension: Blood pressure measurement: Part II-conventional sphygmomanometry: Technique of auscultatory blood pressure measurement. BMJ. 2001;322:1043–7. doi: 10.1136/bmj.322.7293.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Geneva: WHO; 2007. Prevention of Cardiovascular Disease-Guidelines for Assessment and Management of Cardiovascular Risk. [Google Scholar]
- 15.Mathers CD, Bernard C, Iburg KM, Inoue M, Ma Fat D, Shibuya K, et al. Geneva: World Health Organization; 2003. Global Burden of Disease in 2002: Data Sources, Methods and Results. Global Programme on Evidence for Health Policy Discussion Paper No. 54. revised 2004. [Google Scholar]
- 16.Kaur P, Rao TV, Sankarasubbaiyan S, Narayanan AM, Ezhil R, Rao SR, et al. Prevalence and distribution of cardiovascular risk factors in an urban industrial population in South India: A cross-sectional study. J Assoc Physicians India. 2007;55:771–6. [PubMed] [Google Scholar]
- 17.Mehan MB, Srivastava N, Pandya H. Profile of non communicable diseaserisk factors in an industrial setting. J Postgrad Med. 2006;52:167–71. [PubMed] [Google Scholar]
- 18.Reddy KS, Prabhakaran D, Chaturvedi V, Jeemon P, Thankappan KR, Ramakrishnan L, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–9. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah B, Narender K, Menon GR. India: WHO India-ICMR; 2002. Assessment of Burden of Noncommunicable Diseases. 3. [Google Scholar]
- 20.Goyal A, Yusuf S. The burden of cardiovascular diseases in the Indian subcontinent. Indian J Med Res. 2006;124:235–44. [PubMed] [Google Scholar]
- 21.Mohan V, Deepa M, Farooq S, Prabhakaran D, Reddy KS. Surveillance for risk factors of cardiovascular disease among an industrial population in southern India. Natl Med J India. 2008;21:8–13. [PubMed] [Google Scholar]
- 22.Sharma D, Vatsa M, Lakshmy R, Narang R, Bahl VK, Gupta SK. Study of cardiovascular risk factors among tertiary hospital employees and their families. Indian Heart J. 2012;64:356–63. doi: 10.1016/j.ihj.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dugee O, Oum S, Buckley BS, Bonita R. Assessment of total cardiovascular risk using WHO/ISH risk prediction charts in three low and middle income countries in Asia. BMC Public Health. 2013;13:539. doi: 10.1186/1471-2458-13-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mendis S, Lindholm LH, Anderson SG, Alwan A, Koju R, Onwubere BJ, et al. Total cardiovascular risk approach to improve efficiency of cardiovascular prevention in resource constrain settings. J Clin Epidemiol. 2011;64:1451–62. doi: 10.1016/j.jclinepi.2011.02.001. [DOI] [PubMed] [Google Scholar]


