Abstract
Background:
Population aging has evolved gradually. Polypharmacy to control disease associated with age-related physiological changes increases the risk of adverse drug reactions, including drug interactions among the elderly population. Objective: This study was intended to assess the medications used by the elderly population, aiming at identifying the potentially inappropriate medications according to the Beers Criteria.
Materials and Methods:
We conducted a cross-sectional study on medical records to assess the use of medications by elderly patients admitted to the Hospital Nossa Senhora da Conceição in 2011. The variables included gender, age, reasons for admission, comorbidities, and medications used by the elderly patients.
Results:
In total, we reviewed 440 medical records. Patients were predominantly male (51.6%). The total number of medications used was 5904, with an average of 13.4 per person. The three most commonly used drugs were dipyrone, omeprazole, and metoclopramide. The most frequently used drugs according to the Anatomical Therapeutic Chemical Classification (ATC) system were those of the alimentary tract and metabolism, nervous system, and cardiovascular system. Of the 255 types of drugs used, 42 (16.4%) were included in the Beers list, and the three most often used were metoclopramide, ketoprofen, and aspirin.
Conclusion:
The number of medications used per patient was substantial, and potentially inappropriate medications according to the Beers Criteria were significant as well.
Keywords: Adverse effects, drug interactions, drug prescription, elderly, inappropriate use of prescription drugs, inpatients, medication assessment, medication use
Introduction
The proper use of medicines, polypharmacy, and adverse effects are important factors in the treatment of elderly patients. Medication use is the most common intervention in health care for older adults, being able to increase survival time and improve quality of life.[1] Although there is no consensus for the definition of polypharmacy, Bushardt et al.[2] defined as polypharmacy as the presence of six or more concurrent medications. Polypharmacy in the elderly is due to the number of prescribed medications, but the use of drugs as self-medication is extremely common as well.[3,4] In addition, aging is associated with a reduction in first-pass metabolism, bioavailability, and distribution of drugs, which increases the risk of adverse effects,[5] and the risks grow exponentially with the number of different drugs being used.[6] Adverse effects tend to be more severe in the elderly patients.[7] Polypharmacy and potentially inappropriate use of medications in elderly are under-recognized cause of readmissions to the hospital.[8]
Because of the potentially serious consequences of exaggerated or incorrect prescriptions, screening tools have been created to detect inadequacies in drug prescriptions. Currently, the best-known screening tool is the Beers Criteria. In 1991, Beers and colleagues listed 30 drugs that should not be used in elderly patients independently of diagnosis.[9] In 2003, Fick and colleagues updated these criteria and divided them into two categories. First, a list of medications to avoid in older adults, due to the high risk of adverse effects; these should be replaced by safer medications already available. Second is a list of medications to avoid in older adults in certain clinical circumstances.[9,10] In 2012, the American Geriatrics Society (AGS) and an interdisciplinary panel of experts in geriatric care and pharmacotherapy reach consensus on the 2012 AGS Beers Criteria. Fifty-three medications or medication classes encompass the final updated criteria, which are divided into three categories: Potentially inappropriate medications or classes to avoid in older adults, potentially inappropriate medications or classes to avoid in older adults with certain diseases, and syndromes that the drugs listed can exacerbate, and medications to be used with caution in older adults.[11]
The purpose of this study was to determine the prevalence of medication use, and identify potentially inappropriate drugs, according to Beers Criteria, for use in older adults admitted to a hospital in southern Brazil.
Materials and Methods
This study was approved by the Research Ethics Committee of the University of Southern Santa Catarina, under registration number 12.136.4.01.III.
We conducted an epidemiological cross-sectional study to assess medication use in older adults hospitalized at Hospital Nossa Senhora da Conceição, located in the state of Santa Catarina, southern Brazil, covering the period between 1 January and 31 December 2011. During the study period, approximately 5000 hospitalizations of elderly people occurred. We calculated a sample of 360 admissions, considering an unknown prevalence of 50% of elderly that used potentially inappropriate medications, with a 95% confidence interval. The sample was randomly selected from the total admissions for the period, by using a table of random numbers. A 20% addition was made to compensate for losses, totaling a final sample size of 440 records.
All hospitalizations of elderly people aged 60 years and over (completed in 2011) were included in the study. In case of hospital readmission, the records were excluded. No record was excluded for poor quality or lack of accuracy reasons.
Tasy®, particular software used by the hospital, was engaged to collect the data from the electronic medical records. The following variables were included within the data extraction process: Gender, date of birth, age, reason for hospital admission, comorbidities, use of medications during hospitalization by generic name and the Anatomical Therapeutic Chemical Classification (ATC) system, and polypharmacy. The Beers Criteria for potentially inappropriate medication in older adults were used to assess the medication use in the study population.
The collected data were entered into the EpiData software, version 3.1. Statistical analysis was performed using the Statistical Package for the Social Sciences version 20.0. We used the Chi-square test to assess the association between variables of interest, and the Student's t-test for mean comparison. The statistical significance level was set at 95%.
Results
We examined the medical records of 440 elderly patient, of whom 227 (51.6%) were men. The mean age was 69.7 years (SD = 6.0). The total number of medications used for these patients during the study period was 5904, with an average of 13.4 (SD = 7.4) drugs per patient. There were no gender-related differences regarding the number of medications used by men or women (P = 0.995).
Table 1 shows the 20 most common drugs used by the elderly patients, percentage out of the total number of drugs used, and percentage out of the total hospital admissions.
Table 1.
Main medications used by elderly patients (n=440)
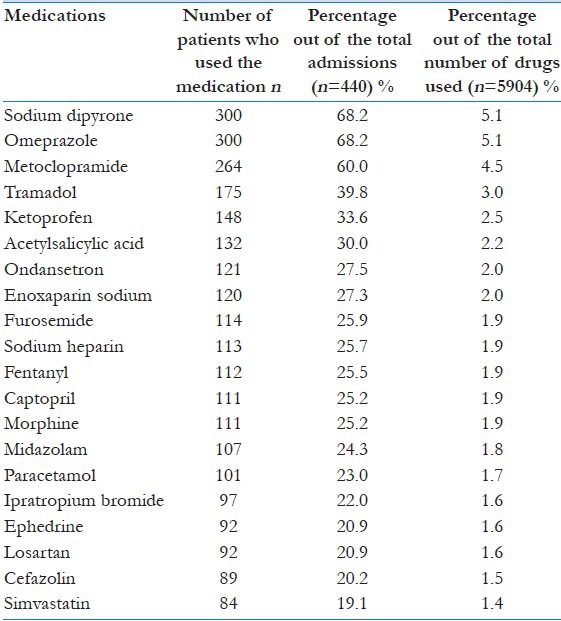
There was a high prevalence of medications used for pain, inflammation, and vomiting. In addition, approximately 70% of hospitalized patients had dipyrone, omeprazole, and metoclopramide as part of their prescriptions, which suggests a pattern of medication use.
Of the surveyed patients, 350 (79.5%) had comorbidities registered in their medical records. Most frequent comorbidities were hypertension (42.3%), diabetes mellitus (13%), cancer (8.9%), and congestive heart failure (4.3%). There was no significant gender-related difference in the number of comorbidities (P = 0.804). The number of medications used by those with at least one comorbidity was significantly higher than those that had no comorbidities. Patients with comorbidities used 14.4 (SD = 7.5) different drugs on average, whereas patients without comorbidity used 9.8 (SD = 5.5) different drugs (P = 0.018). Table 2 shows the reasons for hospitalization in the study sample.
Table 2.
Main reasons for hospitalization of the elderly (n=440)
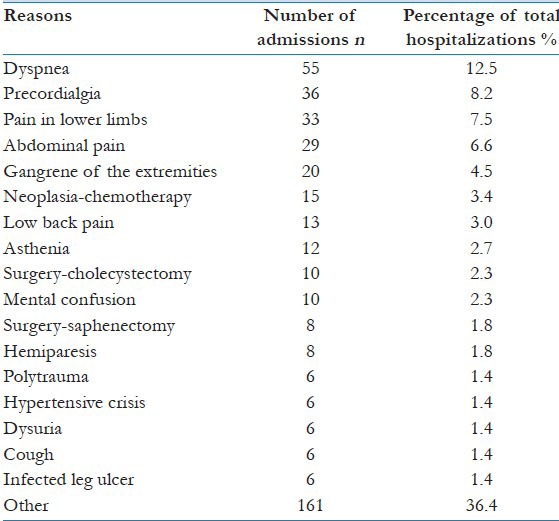
The data showed that the main reasons for hospitalization were due to respiratory and cardiovascular disorders, and that the causes of admissions were multiple because it is a referral hospital with various medical specialties.
Table 3 shows the ATC classification of drugs and amount of medications used.
Table 3.
ATC classification of drugs (n=5904)
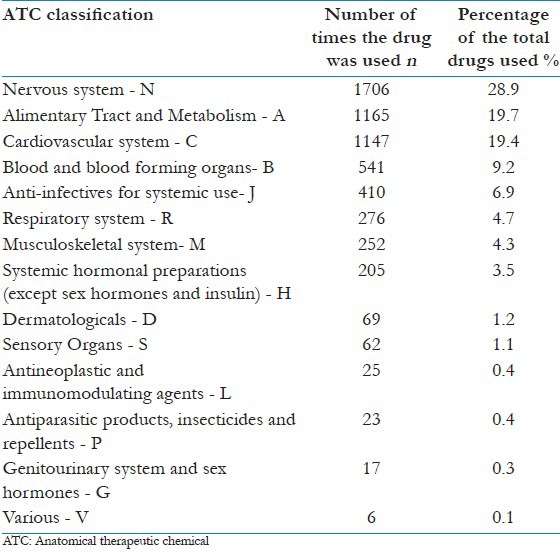
In this study, the classes of drugs most commonly used among the elderly inpatients, according to the ATC classification, were “N,” “A,” and “C”, which correspond to the nervous system, alimentary tract and metabolism, and cardiovascular system, accounting for 68.0% of the medications used.
Beers criteria-based review of medications use
Our data showed that of the 440 patients evaluated, 420 (95.5%) used at least one of the potentially inappropriate medications on the Beers list. Furthermore, the average of potentially inappropriate medications per patient was 3.01 (SD = 1.64), and the amount varied from 1 to 9 drugs per patient.
Of the 255 different types of drugs used by the elderly patient in the study, 42 (16.4%) were potentially inappropriate medications. Table 4 lists all drugs identified as potentially inappropriate for elderly patients, according to the Beers Criteria.
Table 4.
Classification of potentially inappropriate medications, according to the beers criteria, prescribed to the elderly patients
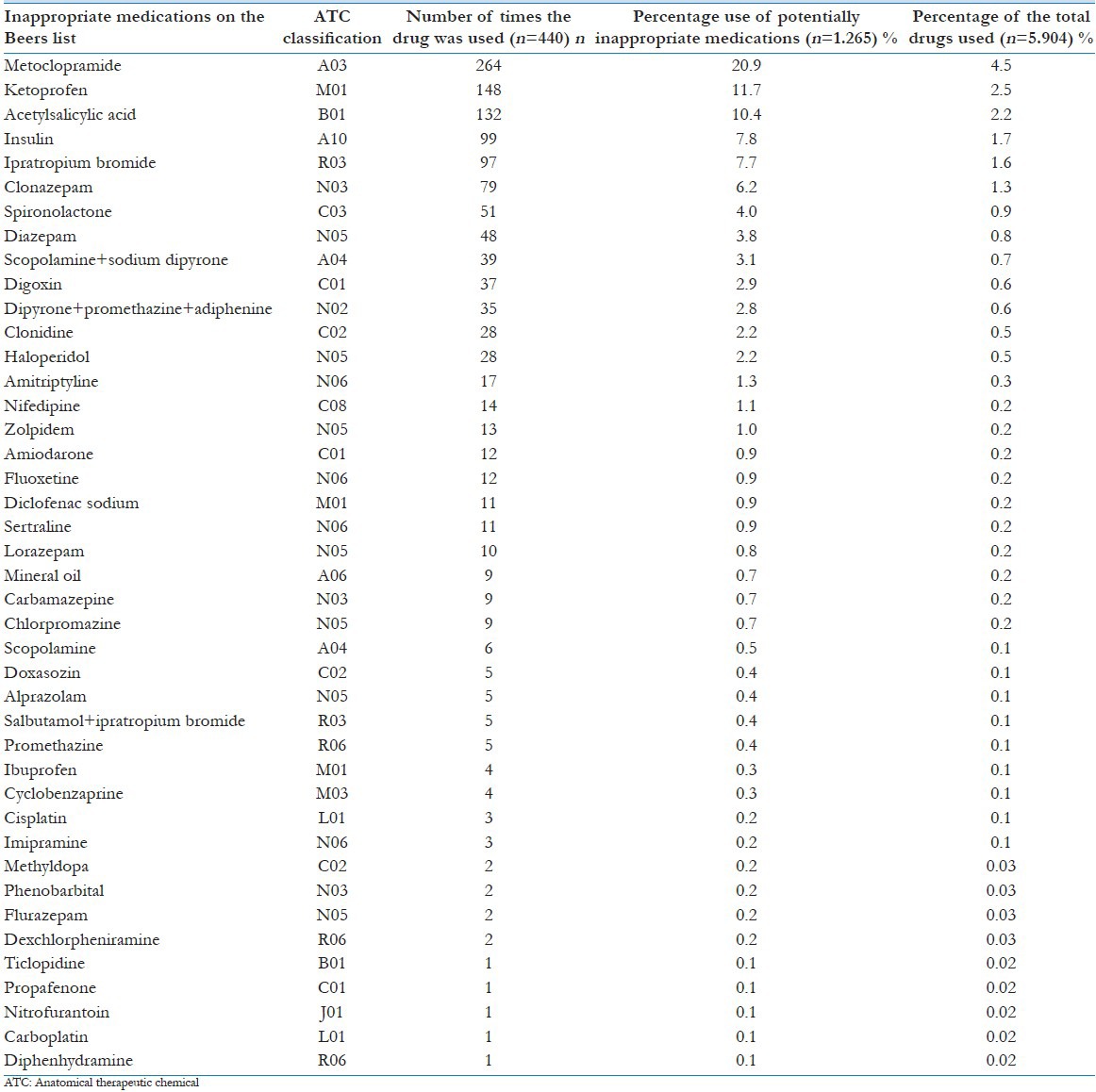
Our data revealed that metoclopramide, acetylsalicylic acid, and ketoprofen accounted for 43% of the potentially inappropriate medications and 9.2% of all drugs used in the study period. Inappropriate medications on the Beers list most commonly used among the elderly inpatients in this study were the ATC classes “A,” “N,” and “M”, which correspond to the alimentary tract and metabolism, nervous system and musculoskeletal system, accounting for 15.1% of the total drugs used and 68.5% of all potentially inappropriate medications for the elderly patients.
Discussion
Our data showed that 5904 drugs were used in 440 surveyed patients during their hospital stay, an average of 13.4 drugs per patient. Studies conducted in southern states of Brazil[12,13] showed a lower prevalence, between 7.0 and 7.8 medications per patient, whereas in our study, the prevalence was almost two times higher. Our data showed that of the 440 patients evaluated, 420 (95.5%) used at least one of the potentially inappropriate medications on the Beers list. Of the 255 different types of drugs used by the elderly patients in the study, 42 (16.4%) were potentially inappropriate medications.
The most widely used drugs were dipyrone, omeprazole, and metoclopramide. Braga et al.[14] demonstrated that dipyrone and metoclopramide had a prevalence of use of 35.7% and 25.0%, respectively, in older adults, whereas in this study, we observed a two-fold higher prevalence of these drugs. Dipyrone is not commonly used in the United States and is not included in the Beers list. Even so, it is widely used in other countries, like Brazil, and should be included in the Beers Criteria of potentially inappropriate medications, because it poses a risk of adverse outcomes for the elderly.[3,4,5]
This study revealed that omeprazole, which is also not listed in the Beers Criteria, was widely used in the elderly patients. It should be noted that studies conducted in Japan provided evidence that the most serious adverse effects of this drug are related to hypomagnesaemia,[15,16] bone fractures, deficient absorption of calcium, vitamin B12, and iron.[16] Along the same line, metoclopramide has been linked to a 2.5% of the possible drug interactions[17] and cause adverse reactions such as extrapyramidal effects (29.0%), dizziness (18.2%), and tremor (9.9%).[18]
Approximately, 150 medications and medication classes are listed on the Beers Criteria[11] of potentially inappropriate medications for elderly patients. Of these, 42 were used at least once in the study population during the study period. The top six medications of the Beers list most commonly used by the elderly in this study were metoclopramide, ketoprofen, acetylsalicylic acid, insulin, ipratropium bromide, and clonazepam, which accounted for more than 64.0% of the total use of potentially inappropriate medications for older adults.
Metoclopramide was listed in the Beers Criteria because of the risk of causing extrapyramidal adverse effects, including tardive dyskinesia, a risk that may be even greater in the elderly patients. Ketoprofen and acetylsalicylic acid were included in the Beers Criteria due to increased risk of gastrointestinal bleeding and peptic ulcer. Insulin was listed due to the increased risk of hypoglycemia, in the absence of improved management of hyperglycemia. Ipratropium bromide was listed due to reduced clearance with advancing age, thus increasing the anticholinergic effects from the medication. Clonazepam and benzodiazepines in general were included in the Beers Criteria due to increased sensitivity of the elderly to these drugs, thereby increasing the risk of cognitive impairment, falls, fractures, delirium, and car accidents.[11]
With regard to potentially inappropriate drugs according to Beers, the result of this study was similar to other published studies on the elderly population. One of them, conducted in the metropolitan area of São Paulo,[19] found that the use of potentially inappropriate medications accounted for 15.1% of the prescriptions among the elderly. Another study, conducted in outpatient clinics of the Geriatrics Service, University of São Paulo,[20] found a 26.9% prevalence of potentially inappropriate medications among older adults, which shows that there is a certain pattern followed by the Brazilian health care centers in this respect.
Importantly, the Beers Criteria is meant to serve as a guide for clinicians and health care providers. It does not prohibit the use of drugs, but restricts them on occasion, depending on the possible interactions between the drugs and the disease or syndrome presented by the individual. Thus, the Beers Criteria must be carefully analyzed, identifying medications that pose potential risks outweighing potential benefits for elderly people.
Using a list of potentially inappropriate medications for older adults is of great importance. Therapy practices should align with these guidelines and create treatment protocols that include the particularities of the elderly population.[21] Switching to drugs with less risk of adverse reactions and drug interactions should be considered.
This study allowed us to analyze the use of potentially inappropriate medications in the elderly people, as well as provide suggestions for replacing medicines that could reduce possible harm to patients.[11] Some of the limitations to this study are related to loss of data due to incomplete filling of the medical records, mainly those related to previous comorbidities. Moreover, some prescriptions read “if necessary,” which impaired adequate assessment, whether the drug was used at some point during the hospital stay. It was assumed that medicines prescribed as “if necessary” were used.
Nevertheless, this is a groundbreaking study because published works on the subject are scarce. Our study allowed us to alert health managers and provide data to researchers, health care professionals, particularly drug prescribers for the use of potentially inappropriate medications for the elderly.
This study was conducted in a hospital setting on inpatient elderly people; and so, all medications were prescribed by physicians. Particular care must be taken in prescribing medications for older adults. The possibility of adverse events and drug interactions should always be borne in mind. Findings from this study indicated a considerable amount of potentially inappropriate medications being used, which should be avoided and replaced by other medications with less potential for adverse effects.
In conclusion, the number of drugs used by the surveyed elderly patients was 5904, encompassing 255 different medications. The average number of medications used per person was relatively high, totaling 13.4 medications per patient. The average number of medications taken by men and women showed no significant difference. The most frequently used drugs according to the ATC system were those of the alimentary tract and metabolism, nervous system, and cardiovascular system. The most commonly used drugs were dipyrone, omeprazole, and metoclopramide.
Of the total number of medications used, 16.4% were potentially inappropriate according to the Beers Criteria, and the most commonly used were metoclopramide, acetylsalicylic acid and ketoprofen.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dal Pizzol T da S, Pons E da S, Hugo FN, Bozzetti MC, Sousa Md L, Hilgert JB. Use of medication by the elderly in urban and rural areas in southern Brazil: A population-based study. Cad Saúde Pública. 2012;28:104–14. doi: 10.1590/s0102-311x2012000100011. [DOI] [PubMed] [Google Scholar]
- 2.Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN. Polypharmacy: Misleading, but manageable. Clin Interv Aging. 2008;3:383–9. doi: 10.2147/cia.s2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santos TR, Lima DM, Nakatani AY, Pereira LV, Leal GS, Amaral RG. Medicine use by the elderly in Goiania, Midwestern Brazil. Rev Saude Publica. 2013;47:94–103. doi: 10.1590/s0034-89102013000100013. [DOI] [PubMed] [Google Scholar]
- 4.de Oliveira MA, Francisco PM, Costa KS, Barros MB. Self-medication in the elderly population of Campinas, São Paulo State, Brazil: Prevalence and associated factors. Cad Saúde Pública. 2012;28:335–45. doi: 10.1590/s0102-311x2012000200012. [DOI] [PubMed] [Google Scholar]
- 5.Guaraldo L, Cano FG, Damasceno GS, Rozenfeld S. Inappropriate medication use among the elderly: A systematic review of administrative databases. BMC Geriatr. 2011;11:79. doi: 10.1186/1471-2318-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi S, Morike K, Klotz U. The clinical implications of ageing for rational drug therapy. Eur J Clin Pharmacol. 2008;64:183–99. doi: 10.1007/s00228-007-0422-1. [DOI] [PubMed] [Google Scholar]
- 7.Laroche ML, Charmes JP, Nouaille Y, Picard N, Merle L. Is inappropriate medication use a major cause of adverse drug reactions in the elderly? Br J Clin Pharmacol. 2007;63:177–86. doi: 10.1111/j.1365-2125.2006.02831.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sehgal V, Bajwa SJ, Sehgal R, Bajaj A, Khaira U, Kresse V. Polypharmacy and potentially inappropriate medication use as the precipitating factor in readmissions to the hospital. J Family Med Prim Care. 2013;2:194–9. doi: 10.4103/2249-4863.117423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 10.Gorzoni ML, Fabbri RM, Pires SL. Beer-Fick criteria and generic drugs in Brazil. Rev Assoc Med Bras. 2008;54:353–6. doi: 10.1590/s0104-42302008000400022. [DOI] [PubMed] [Google Scholar]
- 11.American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616–31. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cruciol-Souza JM, Thomson JC. A pharmacoepidemiologic study of drug interactions in a Brazilian teaching hospital. Clinics (Sao Paulo) 2006;61:515–20. doi: 10.1590/s1807-59322006000600005. [DOI] [PubMed] [Google Scholar]
- 13.Sehn R, Camargo AL, Heineck I, Ferreira MB. Potential drug interactions in prescriptions at the Hospital de Clinicas de Porto Alegre. Infarma. 2003;15:9–10. [Google Scholar]
- 14.Braga TB, Pfaffenbach G, Weiss DP, Barros MB, Bergsten-Mendes G. Point prevalence of drug prescriptions for elderly and non-elderly inpatients in a teaching hospital. Sao Paulo Med J. 2004;122:48–52. doi: 10.1590/S1516-31802004000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tamura T, Sakaeda T, Kadoyama K, Okuno Y. Omeprazole- and esomeprazole-associated hypomagnesaemia: Data mining of the public version of the FDA Adverse Event Reporting System. Int J Med Sci. 2012;9:322–6. doi: 10.7150/ijms.4397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ito T, Jensen RT. Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium. Curr Gastroenterol Rep. 2010;12:448–57. doi: 10.1007/s11894-010-0141-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pereira GJ, Costa LC, Oliveira AR, Barbosa JA, Silva ED, Júnior, Belém LF, et al. Assessment of drugs prescribed to medical in-patients in a public hospital. Rev Ciênc Farm Básica Apl. 2011;32:239–44. [Google Scholar]
- 18.Orta IA, López GJ, Cardeso AC, Pérez JA. The metoclopramide and its adverse reactions on the nervous central system. Rev Cubana Med Gen Integr. 2011;27:197–206. [Google Scholar]
- 19.Carvalho MF, Romano-Lieber NS, Bergsten-Mendes G, Secoli SR, Ribeiro E, Lebrão ML, et al. Polypharmacy among the elderly in the city of São Paulo, Brazil-SABE Study. Rev Bras Epidemiol. 2012;15:817–27. doi: 10.1590/s1415-790x2012000400013. [DOI] [PubMed] [Google Scholar]
- 20.Faustino CG, Passarelli MC, Jacob-Filho W. Potentially inappropriate medications among elderly Brazilian outpatients. Sao Paulo Med J. 2013;131:19–26. doi: 10.1590/S1516-31802013000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Costa SC, Pedroso ER. Drug prescription for inpatient treatment of elderly people at primary care centers: An update. Rev Med Minas Gerais. 2011;2:201–14.21. [Google Scholar]


