Abstract
While placed on different axes of the DSM classification system, borderline personality disorder (BPD) and posttraumatic stress disorder (PTSD) have important relationships with trauma, and overlap between these disorders has long been recognized. The current study is the first to examine comorbidity of PTSD and BPD in a large nationally representative sample using a reliable and valid method of assessing Axis I and II mental disorders. Data came from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Wave II (N=34,653; response rate 70.2%). Multiple regression models were used to examine differences in psychopathology, traumatic events and health-related quality of life across individuals with PTSD alone (n=1820), BPD alone (n=1290) and those with comorbid PTSD-BPD (n=643). The lifetime prevalence of PTSD and BPD were 6.6% and 5.9%, respectively. Of individuals with BPD, 30.2% were also diagnosed with PTSD, whereas 24.2% of individuals with PTSD were also diagnosed with BPD. Individuals with comorbid PTSD-BPD had a poorer quality of life, more comorbidity with other Axis I conditions, increased odds of a lifetime suicide attempt, and a higher prevalence of repeated childhood traumatic events than individuals with either condition alone. These results show that PTSD and BPD have a high degree of lifetime co-occurrence but are not entirely overlapping. Their concurrence is associated with poorer functioning compared to either diagnosis alone, emphasizing the clinical utility of diagnosing both conditions. Future research should explore the determinants of having either or both diagnoses with an aim toward improved identification, prevention, and intervention.
Keywords: posttraumatic stress disorder, borderline personality disorder, comorbidity, epidemiology, suicide attempt
Introduction
The overlap in phenomenological and conceptual aspects of borderline personality disorder (BPD) and posttraumatic stress disorder (PTSD) has been recognized since their initial inclusion in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III; Gunderson & Sabo, 1993; American Psychiatric Association, 1980). While placed on different axes of the DSM classification system, both disorders have important relationships with trauma. PTSD is an Axis I disorder characterized by persistent adverse reactions following exposure to a life-threatening traumatic event (American Psychiatric Association, 2000). Exposure to a traumatic event is not required for a diagnosis of BPD, but adverse experiences such as childhood physical and sexual abuse are commonly present in the life histories of individuals diagnosed with BPD, leading some authors to suggest that BPD be viewed as part of a posttraumatic stress “syndrome” (Zanarini et al. 1989; Goldman et al. 1992; Herman et al. 1989; Ogata et al. 1990). Further adding to the complexity in understanding the relationship between these disorders is the proposed construct of “complex PTSD,” which includes characterological alterations similar to those seen in BPD (Herman, 1992).
Existing studies of PTSD-BPD comorbidity have relied almost entirely on treatment-seeking clinical samples. These studies have suggested comorbid rates of PTSD among individuals with BPD ranging from 25% to 58% (Zanarini et al. 1998; Zlotnick et al. 2002; Zlotnick et al. 2003; Zimmerman & Mattia, 1999; Zanarini et al. 2004; Golier et al. 2003; Rusch et al. 2007; Famularo et al. 1991; Van Den Bosch et al. 2003; Yen et al. 2002; Harned et al. 2008; Linehan et al. 2006). Studies have reported similar rates of comorbid BPD among individuals with PTSD to range even more widely between 10% and 76% (Southwick et al. 1993; Heffernan & Cloitre, 2000; Shea et al. 1999; Zlotnick et al. 2002; Feeny et al. 2002; Clarke et al. 2008; Connor et al. 2002). Only two existing community studies have been able to assess PTSD-BPD comorbidity. One found that 10% of individuals with clinically significant PTSD symptoms also had BPD (Connor et al. 2002), while the second found that 34% of individuals with BPD had PTSD (Swartz et al. 1990). Although community samples, these studies were both conducted among adult respondents in North Carolina and to date, no findings generalizable to the general US population exist.
The literature on psychiatric correlates of PTSD-BPD comorbidity is far from consistent. Some studies have found general psychopathology (Rusch et al. 2007) and depressive symptoms (Bolton et al. 2006) to be more prevalent among individuals with comorbid PTSD-BPD relative to individuals with BPD alone, while alcohol problems (Connor et al. 2002) and a greater number of Axis I diagnoses (Zlotnick et al. 2003) have been found to to be more prevalent among individuals with comorbid PTSD-BPD relative to those with PTSD alone. Some studies have found no differences in Axis I or II characteristics between those with comorbid PTSD-BPD and BPD alone (Zlotnick et al. 2003). Although not inconsistent findings, it is important to note that an increased likelihood of suicide attempts has been found among individuals with comorbid PTSD-BPD relative to those with PTSD alone (Connor et al. 2002; Heffernan & Cloitre, 2000). This difference has not been found when comparing individuals with PTSD-BPD to those with BPD alone (Rusch et al. 2007).
Examination of the relationship between childhood trauma and PTSD-BPD has resulted in somewhat more consistent findings. Most (but not all; Zlotnick et al. 2003) studies have found a relationship between sexual trauma and PTSD-BPD comorbidity compared to either BPD alone (Zlotnick et al. 2003; Van Den Bosch et al. 2003) or PTSD alone (Connor et al. 2002; Feeny et al. 2002). Some studies have additionally found comorbid PTSD-BPD to be associated with earlier abuse onset (Heffernan & Cloitre, 2000), physical abuse (Clarke et al. 2008), and verbal abuse (Heffernan & Cloitre, 2000) relative to individuals with PTSD alone. However, one study found individuals with comorbid PTSD-BPD to be associated with physical abuse and a greater number of types of abuse (Zlotnick et al. 2003) relative to individuals with BPD alone, but did not find these differences relative to those with PTSD alone.
The literature regarding extent of PTSD symptoms has also been conflicting, with some studies finding differences between the comorbid PTSD-BPD group and individuals with PTSD only (Zlotnick et al. 2002; Clarke et al. 2008) and others finding no such differences (Heffernan & Cloitre, 2000). In terms of BPD traits, one study found a higher mean number among those with comorbid PTSD-BPD relative to those with PTSD alone (Zlotnick et al. 2002), but studies have not found this difference relative to BPD alone (Zlotnick et al. 2002; Zlotnick et al. 2003).
Quality of life has also been infrequently studied, but one study demonstrated that individuals with comorbid PTSD-BPD have worse physical quality of life than those with BPD only (Bolton et al. 2006). Other studies have examined related measures, however, and have found individuals with comorbid PTSD-BPD to have a significantly lower global assessment of functioning and a higher likelihood of lifetime hospitalization compared to those with BPD alone and those with PTSD alone (Zlotnick et al. 2003). In addition, the one community study of this comorbidity found that individuals with PTSD-BPD were more likely to have fair to poor health and increased impairment in social and occupational domains relative to those with PTSD alone (Connor et al. 2002).
Inconsistent findings regarding correlates of PTSD-BPD comorbidity most likely stem from methodological differences across surveys. As mentioned, most studies have focused on treatment-seeking samples, which is likely to have biased findings toward increased severity of the index disorder(s). In addition, many studies were restricted to females (Rusch et al. 2007; Heffernan & Cloitre, 2000; Clarke et al. 2008; Feeny et al. 2002; Van Den Bosch et al. 2003) and many focused on further sub-samples such as individuals who have experienced sexual trauma (Clarke et al. 2008; Heffernan & Cloitre, 2000) or individuals with at least one personality disorder (Zlotnick et al. 2003). Additionally, some studies compare the comorbid group to either individuals with PTSD only or individuals with BPD only, limiting the comprehensiveness of the examinations (Heffernan & Cloitre, 2000; Bolton et al. 2006; Connor et al. 2002; Rusch et al. 2007; Clarke et al. 2008).
The only previous community survey to have addressed PTSD-BPD comorbidity was limited to a particular region of the U.S. and, moreover, had only a small number (n=15) of respondents with both disorders (Connor et al. 2002). To date, no findings generalizable to the US population exist.
The current study is the first to examine the comorbidity of PTSD and BPD in a large, nationally representative sample using valid and reliable DSM-IV diagnoses. Not only does it provide the first general population estimate of the extent of PTSD-BPD comorbidity using DSM diagnoses, but it also explores a broad range of correlates of this comorbidity including presence of other psychiatric diagnoses, relationship to childhood traumatic events, age of onset of PTSD, extent of PTSD and BPD symptoms, and health-related quality of life. In addition, the current study provides the first opportunity for an examination of gender differences on the impact of this comorbidity. In order to comprehensively characterize the nature of PTSD-BPD comorbidity, three groups will be examined: respondents with PTSD only, respondents with BPD only and respondents with both PTSD and BPD. A better understanding of the discontinuity, overlap and consequences of overlap between PTSD and BPD holds great importance for clinicians.
Methods
Sample
The NESARC (Grant et al. 2003b; Grant & Kaplan, 2005) is a longitudinal nationally representative survey based on the civilian, non-institutionalized population of the 50 United States, age 18 and over. Data collection was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and was conducted in two waves using face-to-face interviews. Wave I interviews (N=43,093) were conducted between 2001 and 2002 by trained lay-interviewers who had an average of five years experience working on census and other health-related national surveys (Grant et al. 2003b). The current study utilized data from Wave II interviews which were conducted between 2004 and 2005 with 34,653 of the NESARC Wave I respondents (Grant & Kaplan, 2005). After accounting for those ineligible for the Wave II interview, there was a cumulative response rate of 70.2% for the Wave II survey. Informed consent was obtained from all participants before beginning the interviews. Detailed descriptions of methodology, sampling, and weighting procedures can be found elsewhere (Grant et al. 2003b; Grant & Kaplan, 2005).
Measures
Psychiatric Diagnoses
The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV; Grant et al. 2003a; Ruan et al. 2008), a fully structured diagnostic interview appropriate for use by trained lay interviewers as well as clinicians, was used to assess DSM-IV (American Psychiatric Association, 2000) Axis I and II disorders. Axis I disorders assessed include major depression, dysthymia, mania, hypomania, panic disorder with and without agoraphobia, agoraphobia without panic disorder, social phobia, specific phobia, generalized anxiety disorder, posttraumatic stress disorder (Wave II only), alcohol abuse and dependence, and drug abuse and dependence. For all Axis I disorders including PTSD, the age of onset of disorder was assessed. Although Axis I diagnoses were made for both past-year and lifetime time frames, the current study utilized lifetime diagnoses for most analyses, with the exception being the use of past-year PTSD in analyses examining health-related quality of life. The Axis II diagnosis of borderline personality disorder (Grant et al. 2008) was also assessed by the AUDADIS-IV at Wave II. The AUDADIS-IV attempts to establish the pervasiveness of personality disorders by indicating that symptoms should occur “most of the time throughout your life , regardless of the situation and who you were with.” Fair to good test-retest and inter-rater reliability have been demonstrated for Wave II Axis I and II AUDADIS-IV diagnoses using a subsample of 1899 respondents (Grant et al. 2003a; Ruan et al. 2008). Kappas were 0.77 and 0.64 for past-year and lifetime diagnoses of PTSD, respectively, and 0.71 for BPD, all indicating fair to good agreement. Internal consistencies for these diagnoses also fell in the good range (0.84 for PTSD, 0.83 for BPD).
Sociodemographics
Sociodemographic variables assessed in the NESARC Wave II include gender, age, ethnicity, education, marital status and household income. All sociodemographic variables were categorical, with the exception of sex, which was dichotomous. Age was divided into four groups (18–29, 30–44, 45–64, and 65+ years), ethnicity into five groups (Caucasian, African American, American Indian/Alaskan, Asian/Hawaiian/Pacific Islander and Hispanic), level of education into three groups (less than high school, high school, and some college or more), marital status into three groups (married/cohabiting, widowed/separated/divorced, never married) and household income into four groups ($0–19,999, $20,000–$34,999, $35,000–$59,999, and $60,000 or more).
Suicide Attempts
At Wave II, a question assessing lifetime suicide attempts was asked of all respondents. The question specifically asked, “In your entire life, did you ever attempt suicide?”
Health Related Quality of Life
Health related quality of life (HRQOL) in the past month was assessed using the Medical Outcomes Study Short Form (SF-12), a twelve-item self-report measure (Ware et al. 1996). Responses to items are used to from two component scores, a physical health related quality of life component score (PCS) and a mental health related quality of life component score (MCS), with higher scores indicating better HRQOL. This measure has demonstrated good reliability and validity (Ware et al. 1996).
Childhood Traumatic Events
Five childhood traumatic events were examined in the current study because of their possible relevance to BPD, including sexual abuse, physical abuse by a parent or caretaker, neglect by a parent or caretaker, witnessing violence in the home, and physical attack or abuse by someone other than a parent or caretaker. Respondents who endorsed lifetime occurrence of an event were then asked at what age this event first occurred. Childhood traumatic events were defined to occur before the age of 16. This cutoff has been used in previous literature (Connor et al. 2002; Van Den Bosch et al. 2003; Kessler et al. 1997). Repetition of the traumatic events was also assessed by asking respondents how many times the event had occurred. As done in previous research (Heffernan & Cloitre, 2000; Van Den Bosch et al. 2003), events that occurred more than once were also examined in the current study. These were combined into trichotomous variables reflecting no exposure to trauma (reference group), a single exposure to the given trauma, and repeated exposures to the given trauma. Two derived variables were also created based on these traumatic events. Since previous research has demonstrated an especially negative effect of three or more traumatic events (Kessler et al. 1997), one variable was derived that differentiated individuals who experienced three or more of the events from those who had experienced none, one or two of the traumatic events. The last derived variable differentiated sexual from non-sexual traumatic experiences, as sexual trauma has been hypothesized to have an etiological effect in BPD compared to non-sexual trauma (Murray, 1993).
Borderline Personality Disorder and Posttraumatic Stress Disorder Symptom Severity
Eighteen items were used to assess symptoms of BPD. These items correspond to the nine criteria used to assess BPD in DSM-IV (American Psychiatric Association, 2000). Two items correspond to the BPD criterion of frantic efforts to avoid abandonment, four items to the identity disturbance criterion, three items to the impulsivity criterion, two items to the suicidal behaviors/self-mutilation criterion, and three items to the inappropriate anger criterion. Each of the other four BPD criteria were assessed with one item. Nineteen items were used to assess symptoms of PTSD, corresponding to the five re-experiencing symptoms (6 items), the seven avoidance symptoms (8 items) and the five arousal symptoms (5 items) in DSM-IV (American Psychiatric Association, 2000). In order to examine BPD and PTSD symptom severity, two count variables were created based on the number of BPD criteria and PTSD criteria each respondent endorsed.
Analytic Strategy
All analyses were conducted using Taylor Series Linearization in the SUDAAN (Shah et al. 1995) program to account for the complex sampling methodology of the NESARC. This is a variance estimation procedure that utilizes NESARC stratification information. Appropriate statistical weights were also used to ensure that the data was representative of the national population.
Cross-tabulations were first used to determine the prevalence of PTSD and BPD and overlap between these diagnoses. Second, cross-tabulations and chi-squares were used to determine associations between three diagnostic groups (lifetime PTSD alone, BPD alone, and lifetime PTSD and BPD) and sociodemographic variables.
The three diagnostic groups were then compared using multiple logistic and linear regression models, as appropriate, with the independent variable of interest in all models being the trichotomous variable differentiating individuals with PTSD alone, BPD alone and comorbid PTSD-BPD. A lifetime diagnosis of PTSD was used in all analyses except for those examining HRQOL, a past-month measure. In this case, a past-year diagnosis of PTSD was utilized (as past-month diagnoses of PTSD were not made in the NESARC). Dependent variables included lifetime Axis I psychopathology, childhood traumatic events, HRQOL, number of BPD and PTSD symptoms, and age of onset of PTSD.
Logistic regression models were adjusted for sociodemographic factors significantly associated with diagnoses of PTSD, BPD and comorbid PTSD-BPD in chi-square analyses. Linear regression models were adjusted for sociodemographic factors and number of Axis I mental disorders, in order to account for the burden of comorbidity and increased severity of mental disorders. Interactions with gender were examined for each dependent variable. For those variables with significant gender interactions, regressions were repeated stratifying by gender.
Results
Prevalence
The prevalence of lifetime PTSD (n=2,463) was 6.6% (SE=0.18; 95% CI=6.27–7.00) and the prevalence of BPD (n=2,231) was 5.9% (SE=0.19; 95% CI=5.51–6.28). Twenty four percent of individuals with lifetime PTSD also had BPD, while 30.2% of individuals with BPD also had PTSD. Ninety percent of the sample had neither PTSD nor BPD (n=30,900, 95% CI=89.9–90.2), 5.0% had PTSD without BPD (n=1820, 95% CI=4.7– 5.3), 3.7% had BPD without PTSD (n=1290, 95% CI=3.4–4.0) and 1.6% had comorbid PTSD-BPD (n=643, 95% CI=1.4–1.8).
Sociodemographic Characteristics
Sociodemographic characteristics are presented by PTSD-BPD group in Table 1. All variables showed significant relationships with PTSD-BPD groups in chi-square analyses and all were used as covariates in the following adjusted odds ratios. Using sets of 2×2 chi-square analyses, the following general observations could be made. Individuals with PTSD alone were more likely to be female than those with BPD alone or comorbid PTSD-BPD. Individuals with BPD alone or comorbid PTSD-BPD tended to be younger than individuals with PTSD alone. More individuals with PTSD were Caucasian, while higher proportions of individuals with BPD and PTSD-BPD fell into the other race/ethnicity categories. Individuals with PTSD-alone tended to have a higher level of education than individuals with BPD or PTSD-BPD. Individuals with PTSD alone were most likely to be married or cohabiting, while individuals with BPD alone were most likely to never have been married, and those with comorbid PTSD-BPD were most likely to have been widowed, separated or divorced. Income was distributed fairly equally across all three PTSD-BPD groups, although more individuals with PTSD-BPD tended to have lower incomes, relative to the other two groups.
Table 1.
Demographic characteristics of the sample
| Characteristics | PTSD (n = 1820) |
BPD (n = 1290) |
PTSD + BPD (n = 643) |
|---|---|---|---|
| n (%) |
n (%) |
n (%) |
|
| Gender | |||
| Male | 473 (29.5) | 605 (52.7) | 201 (34.1) |
| Female | 1347 (70.5) | 685 (47.3) | 442 (65.9) |
| Age | |||
| 20–29 | 184 (12.4) | 302 (26.7) | 121 (22.4) |
| 30–44 | 571 (30.3) | 469 (35.8) | 234 (36.4) |
| 45–64 | 781 (42.8) | 398 (29.4) | 256 (36.6) |
| 65+ | 284 (14.6) | 121 (8.0) | 32 (4.7) |
| Ethnicity | |||
| Caucasian | 1060 (72.1) | 721 (68.3) | 313 (61.7) |
| African American | 380 (12.2) | 289 (14.7) | 175 (18.1) |
| American Indian/Alaskan | 35 (2.2) | 41 (4.0) | 28 (6.4) |
| Asian/Hawaiian/Pacific | 38 (2.4) | 31 (3.2) | 7 (1.6) |
| Islander | |||
| Hispanic | 307 (11.1) | 208 (9.8) | 120 (12.3) |
| Education | |||
| < High School | 308 (15.0) | 248 (18.8) | 139 (20.1) |
| High School | 463 (25.3) | 417 (33.1) | 183 (28.6) |
| Some College + | 1049 (59.7) | 625 (48.1) | 321 (51.4) |
| Marital Status | |||
| Married/Cohabiting | 903 (60.8) | 530 (49.9) | 241 (45.6) |
| Widowed/Separated/Divorced | 640 (26.8) | 389 (23.6) | 237 (31.4) |
| Never Married | 277 (12.4) | 371 (26.5) | 165 (23.0) |
| Household Income | |||
| $0 – $19,999 | 501 (23.9) | 379 (26.3) | 275 (39.0) |
| $20,000 – $34,999 | 419 (21.4) | 298 (23.4) | 140 (22.0) |
| $35,000 – $59,999 | 404 (22.3) | 328 (25.0) | 125 (20.2) |
| $60,000 + | 496 (32.4) | 285 (25.3) | 103 (18.7) |
Patterns of Comorbidity
Individuals with BPD alone were significantly more likely than those with PTSD alone to have the comorbid presence of most of the mood, anxiety and substance use disorders, the only exceptions being panic disorder and specific phobia (See Table 2). Furthermore, individuals with comorbid PTSD-BPD were significantly more likely than individuals with BPD-alone and individuals with PTSD-alone to have most lifetime mood, anxiety and substance use disorders. The only statistically significant PTSD-BPD group by gender interactions were for hypomanic episode and specific phobia. Identical regressions stratified by gender, revealed that among females, those with BPD and those with comorbid PTSD-BPD were significantly more likely than those with PTSD alone to have hypomanic episodes. Among males, those with BPD were significantly more likely to have hypomanic episodes than those with PTSD and those with comorbid PTSD-BPD were significantly less likely than those with BPD only to have hypomanic episodes. Examination of the gender interaction in specific phobia revealed that among males (but not females), those with BPD were less likely to have specific phobia compared to those with PTSD. Individuals with comorbid PTSD-BPD were more likely to have specific phobia compared to those with either PTSD alone or BPD alone among both males and females.
Table 2.
Lifetime psychiatric disorders associated with posttraumatic stress disorder (PTSD) and borderline personality disorder (BPD)
| PTSD (n = 1820) |
BPD (n = 1290) |
PTSD + BPD (n = 643) |
BPD vs. PTSD | (PTSD + BPD) vs. PTSD |
(PTSD + BPD) vs. BPD |
|
|---|---|---|---|---|---|---|
| n (%) |
n (%) |
n (%) |
AOR (95% CI) |
AOR (95% CI) |
AOR (95% CI) |
|
| Mood Disorders | ||||||
| Major Depressive Episode | 886 (48.6) |
749 (59.3) |
498 (77.5) |
1.76 (1.46–2.13)*** |
3.58 (2.72–4.71)*** |
2.03 (1.56–2.65)*** |
| Dysthymic Episode | 261 (13.8) |
236 (17.7) |
199 (31.7) |
1.59 (1.26–1.99)*** |
2.86 (2.13–3.84)*** |
1.80 (1.37–2.37)*** |
| Manic Episode | 189 (10.6) |
300 (23.8) |
277 (45.7) |
2.25 (1.77–2.87)*** |
6.02 (4.62–7.85)*** |
2.67 (2.07–3.45)*** |
| Hypomanic Episode | 122 (6.3) |
162 (13.2) |
82 (10.6) |
1.81 (1.30–2.51)** |
1.39 (0.90–2.16) |
0.77 (0.54–1.10) |
| Any Mood Disorder | 990 (53.5) |
864 (68.1) |
556 (86.5) |
2.01 (1.65–2.45)*** |
5.24 (3.70–7.43)*** |
2.61 (1.84–3.72)*** |
| Anxiety Disorders | ||||||
| Panic Disorder With or Without Agoraphobia |
352 (20.7) |
269 (22.0) |
235 (35.0) |
1.20 (0.93–1.54) |
1.94 (1.49–2.53)*** |
1.62 (1.25–2.11)*** |
| Agoraphobia Without Panic Disorder |
6 (0.3) |
15 (1.8) |
10 (1.8) |
6.23 (1.92–20.29)** |
5.82 (1.75–19.33)** |
0.93 (0.39–2.21) |
| Social Phobia | 239 (13.1) |
281 (23.3) |
239 (39.0) |
2.06 (1.62–2.62)*** |
3.99 (3.03–5.25)*** |
1.93 (1.48–2.53)*** |
| Specific Phobia | 580 (32.7) |
381 (29.6) |
315 (51.8) |
0.95 (0.76–1.20) |
2.14 (1.69–2.70)*** |
2.24 (1.74–2.89)*** |
| Generalized Anxiety Disorder |
381 (21.0) |
351 (27.5) |
303 (49.5) |
1.69 (1.34–2.14)*** |
3.95 (3.10–5.04)*** |
2.34 (1.85–2.96)*** |
| Any Anxiety Disorder | 955 (53.2) |
716 (57.7) |
498 (77.3) |
1.37 (1.13–1.67)*** |
3.03 (2.37–3.87)*** |
2.20 (1.71–2.84)*** |
| Substance Disorders | ||||||
| Alcohol Abuse/ Dependence |
655 (37.2) |
692 (56.9) |
344 (56.4) |
1.68 (1.38–2.04)*** |
2.08 (1.64–2.63)*** |
1.24 (0.97–1.58) |
| Drug Abuse/ Dependence |
287 (17.0) |
399 (34.8) |
223 (38.8) |
1.81 (1.42–2.31)*** |
2.55 (1.98–3.29)*** |
1.41 (1.11–1.80)*** |
| Any Substance Disorder |
718 (41.0) |
757 (61.5) |
388 (63.5) |
1.69 (1.39–2.05)*** |
2.33 (1.82–2.98)*** |
1.38 (1.06–1.80)*** |
|
Lifetime Suicide Attempt |
156 (8.0) |
256 (20.0) |
204 (32.4) |
3.29 (2.44–4.44)*** |
5.26 (3.85–7.19)*** |
1.60 (1.23–2.07)*** |
Adjusted Odds Ratios (AOR) are adjusted for gender, age, ethnicity, education, marital status, and household income.
p<.05
p<.01
p<.001
Suicidality
The likelihood of having made a lifetime suicide attempt was highest for the comorbid PTSD-BPD group, followed by the BPD alone group and then the PTSD alone group. All differences between the three groups were significant (See Table 2).
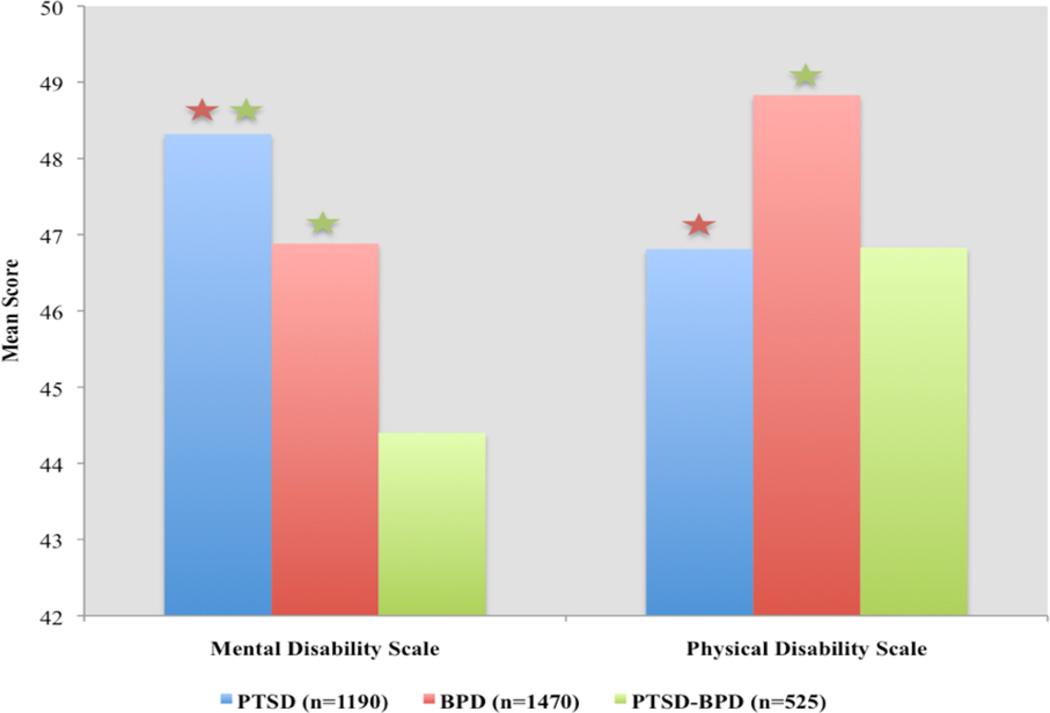
Health-Related Quality of Life
Results for analyses examining HRQOL among the three diagnostic groups are presented in Figure 1. Note that the PTSD-BPD groups for these analyses were calculated using past-year PTSD, hence the group n’s differ from the previously reported lifetime groups. Significant differences persisted after adjusting for sociodemographic factors and number of past-year Axis I mental disorders. Individuals with comorbid PTSD-BPD had the lowest mental HRQOL with individuals with BPD alone and then PTSD alone having significantly higher levels. All differences between the three groups were significant. Individuals with PTSD and comorbid PTSD-BPD had similar levels of physical HRQOL, which were significantly lower than the levels of individuals with BPD alone. Interactions between PTSD-BPD group and gender were not significant for mental or physical HRQOL.
Figure 1. Relationships between posttraumatic stress disorder (PTSD), borderline personality disorder (BPD) and their combination (PTSD + BPD) and health-related quality of life.
displays mean scores and differences between groups means derived from multiple linear regressions. The model is adjusted for gender, age, ethnicity, education, marital status, household income, and number of past-year Axis I mental disorders (none, 1 disorder, 2 disorders, 3+ disorders). Red stars indicate that the group mean is significantly different from the BPD alone group mean at p<.01 and green stars indicate that the group mean is significantly different from the PTSD-BPD group mean at p<.05.
Childhood Traumatic Events
The only difference between individuals with BPD alone and those with PTSD alone in terms of childhood traumatic events was that individuals with BPD alone were significantly more likely to experience sexual versus nonsexual trauma relative to individuals with PTSD alone (Table 3). Individuals with comorbid PTSD-BPD were significantly more likely than those with PTSD alone and BPD alone to have experienced each of the repeated childhood traumatic event variables examined. In terms of single occurrence traumatic events, individuals with comorbid PTSD-BPD were significantly more likely than those with PTSD alone and BPD alone to have experienced a single episode of neglect. Individuals with comorbid PTSD-BPD were significantly more likely to experience a single episode of sexual abuse than individuals with PTSD alone and significantly more likely to experience a single episode of physical attack or abuse by someone other than a parent or caretaker compared to those with BPD alone. When looking at the extent of traumatic events, individuals with PTSD-BPD were significantly more likely than those with PTSD alone and BPD alone to have experienced three or more of the childhood traumatic events examined.
Table 3.
Traumatic events associated with posttraumatic stress disorder (PTSD) and borderline personality disorder (BPD)
| PTSD (n = 1820) |
BPD (n = 1290) |
PTSD + BPD (n = 643) |
BPD vs. PTSD | (PTSD + BPD) vs. PTSD |
(PTSD + BPD) vs. BPD |
|
|---|---|---|---|---|---|---|
| n (%) |
n (%) |
n (%) |
AOR (95% CI) |
AOR (95% CI) |
AOR (95% CI) |
|
|
Childhood Traumatic Events (Before age 16) |
||||||
| No sexual abuse | 1547 (86.5) |
1073 (86.3) |
449 (73.1) |
1.00 | 1.00 | 1.00 |
| Single sexual abuse | 81 (4.6) |
73 (5.0) |
49 (8.5) |
1.30 (0.90–1.89) |
2.15 (1.26–3.65)* |
1.65 (0.97–2.81) |
| Repeated sexual abuse | 157 (8.7) |
115 (8.7) |
117 (18.4) |
1.31 (0.91–1.89) |
2.48 (1.82–3.38)*** |
1.90 (1.29–2.80)*** |
| No physical abuse by parent/caretaker |
1638 (92.3) |
1172 (92.7) |
512 (83.7) |
1.00 | 1.00 | 1.00 |
| Single physical abuse by parent/caretaker |
19 (1.1) |
15 (1.0) |
10 (1.7) |
0.87 (0.38–1.95) |
1.45 (0.51–4.10) |
1.67 (0.51–5.45) |
| Repeated physical abuse by parent/caretaker |
124 (6.6) |
79 (6.2) |
95 (14.7) |
0.89 (0.61–1.28) |
2.19 (1.52–3.15)*** |
2.46 (1.67–3.64)*** |
| No neglect by parent/caretaker |
1670 (93.8) |
1171 (93.0) |
511 (84.5) |
1.00 | 1.00 | 1.00 |
| Single neglect by parent/caretaker |
23 (1.3) |
21 (1.6) |
19 (3.7) |
0.95 (0.43–2.10) |
2.59 (1.16–5.76)* |
2.71 (1.34–5.50)** |
| Repeated neglect by parent/caretaker |
95 (4.9) |
73 (5.5) |
81 (11.8) |
1.00 (0.67–1.51) |
2.24 (1.53–3.28)*** |
2.24 (1.47–3.41)*** |
| Did not witness violence in the home |
1402 (80.5) |
989 (81.4) |
391 (68.3) |
1.00 | 1.00 | 1.00 |
| Single witnessed violence in home |
32 (1.9) |
40 (2.8) |
27 (3.0) |
1.57 (0.87–2.83) |
1.90 (0.92–3.92) |
1.21 (0.63–2.33) |
| Repeatedly witnessed violence in home |
318 (17.6) |
210 (15.8) |
181 (28.6) |
0.88 (0.69–1.11) |
1.68 (1.28–2.19)*** |
1.92 (1.46–2.51)*** |
| No physical attack/abuse by someone other than parent/caretaker |
1705 (93.2) |
1163 (90.2) |
539 (85.7) |
1.00 | 1.00 | 1.00 |
| Single physical attack/abuse by |
31 (2.6) |
35 (2.8) |
27 (4.6) |
0.75 (0.39–1.45) |
1.93 (0.97–3.87) |
2.58 (1.38–4.88)* |
| someone other than parent/caretaker |
||||||
| Repeated physical attack/abuse by someone other than parent/caretaker |
73 (4.3) |
78 (7.0) |
46 (9.8) |
1.11 (0.73–1.71) |
2.19 (1.36–3.51)** |
1.96 (1.25–3.09)** |
|
Number of Early Abuse Experiences |
||||||
| 0 to 2 | 1687 (93.2) |
1203 (94.1) |
523 (83.0) |
1.00 | 1.00 | 1.00 |
| 3 to 5 | 119 (6.8) |
75 (5.9) |
112 (17.0) |
0.84 (0.59–1.19) |
2.44 (1.76–3.38)*** |
2.91 (2.07–4.10)*** |
|
Type of Early Abuse Experience |
||||||
| Nonsexual Trauma | 389 (59.3) |
316 (60.5) |
196 (49.9) |
1.00 | 1.00 | 1.00 |
| Sexual | 266 (40.7) |
209 (39.6) |
189 (50.1) |
1.46 (1.03–2.08)** |
1.70 (1.18–2.45)** |
1.16 (0.77–1.75) |
Adjusted Odds Ratios (AOR) are adjusted for gender, age, ethnicity, education, marital status, and household income.
p<.05
p<.01
p<.001
Finally, individuals with comorbid PTSD-BPD were significantly more likely than those with PTSD alone, but not those with BPD alone, to have experienced sexual (vs. nonsexual) childhood trauma. The only significant interaction between the PTSD-BPD group and gender was for a single episode of childhood physical attack or abuse by someone other than a parent or caretaker. Among females, those with comorbid PTSD-BPD were significantly more likely to have experienced a single episode of physical attack or abuse relative to those with PTSD alone and BPD alone. There were no significant differences among males.
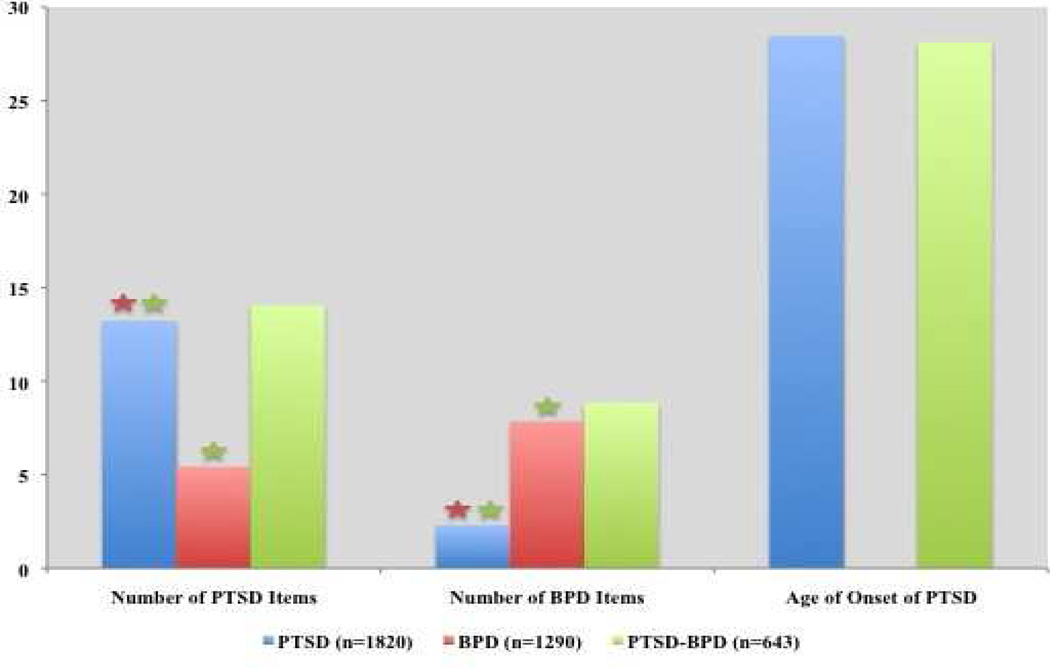
BPD and PTSD Symptom Severity and Age of Onset of PTSD
There were significant differences in the number of BPD and PTSD symptoms endorsed between all three PTSD-BPD diagnostic groups after adjusting for sociodemographic factors and number of lifetime Axis I mental disorders (Figure 2). Individuals with comorbid PTSD-BPD endorsed the highest number of BPD symptoms (unadjusted mean=9.44), followed by the BPD group (unadjusted mean=8.08) and finally the PTSD group (unadjusted mean=1.95). The interaction between PTSD-BPD group and gender in terms of number of BPD symptoms endorsed was not significant. Individuals with comorbid PTSD-BPD also endorsed the highest number of PTSD symptoms (unadjusted mean=14.58), followed by the PTSD alone group (unadjusted mean=13.03) and finally the BPD alone group (unadjusted mean=5.42). The interaction between PTSD-BPD group and gender in terms of number of PTSD symptoms endorsed was significant. Regressions stratified by gender showed that individuals with comorbid PTSD-BPD had a higher mean number of PTSD symptoms compared to those with PTSD only among females. Lastly, although individuals with comorbid PTSD-BPD had a significantly earlier age of onset of PTSD symptoms (unadjusted mean=25.29) than individuals with PTSD alone (unadjusted mean=29.77) in the unadjusted model and the model adjusted for sociodemographic factors only, this difference was no longer significant after adjusted for sociodemographic factors and number of lifetime Axis I disorders. The PTSD-BPD group by gender interaction for age of onset of PTSD was significant. There were no significant differences in the fully adjusted model, but in the unadjusted model and the model adjusted only for sociodemographics, those with comorbid PTSD-BPD had a significantly lower age of onset of PTSD compared to those with PTSD alone only among females.
Figure 2. Relationships between posttraumatic stress disorder (PTSD), borderline personality disorder (BPD) and their combination (PTSD + BPD) and number of PTSD and BPD symptoms endorsed and age of onset of PTSD.
displays mean scores and differences between group means derived from multiple linear regressions. The model is adjusted for gender, age, ethnicity, education, marital status, household income, and number of lifetime Axis I mental disorders (none, 1 disorder, 2 disorders, 3+ disorders). Red stars indicate that the group mean is significantly different from the BPD alone group mean at p<.001 and green stars indicate that the group mean is significantly different from the PTSD-BPD group mean at p<.01.
Discussion
This is the first study of PTSD-BPD comorbidity in a nationally representative sample using reliable and valid diagnoses of DSM-IV mental disorders. The principal finding is that individuals with comorbid PTSD-BPD carry a significantly greater burden of illness than individuals with either disorder alone. This was evident in terms of more symptoms, higher rates of comorbidity with other Axis I conditions, increased odds of suicide attempt(s), and poorer health-related quality of life. Importantly, PTSD-BPD comorbidity was also associated with an increased likelihood and severity of exposure to repeated childhood traumatic events.
The extent of overlap between PTSD and BPD seen in this general population-based study lies in the lower end of the range of previous estimates. This is to be expected, given that most prior estimates were derived from clinical samples. However, the prevalence of PTSD among individuals with BPD in the present study (30%) was strikingly similar to that reported in the only community study assessing this prevalence (34%; Swartz et al, 1990). Although there is significant symptomatic and possibly etiologic overlap between these disorders, the data make clear that they are not redundant. This is especially evident given that respondents with BPD alone were significantly more likely to have nearly every mental disorder examined as well as poorer quality of life than those with PTSD alone. Although some neurobiological evidence suggests common etiologic underpinnings for both disorders (hypothalamic-pituitary-adrenal (HPA) axis, as an example (Jogems-Kosterman et al. 2007; Wingenfeld et al. 2007a; Wingenfeld et al. 2007c; Wingenfeld et al. 2007b; Southwick et al. 2003; Lange et al. 2005; Rinne et al. 2002), the findings from this study indicate a differential impact when present alone and comorbid, and thus emphasize the importance of diagnosing both PTSD and BPD.
Our findings of a significantly greater number of both BPD and PTSD symptoms in the comorbid PTSD-BPD group have not been demonstrated in previous research (e.g., Zlotnick et al. 2002; Zlotnick et al. 2003; Heffernan & Cloitre, 2000). One possible explanation for this discrepancy is the fact that these previous studies came from clinical samples, while the current study was population-based. Clinical samples typically are more severe in general and this increased severity may have inflated all symptoms scores leaving less room for variance. These significant findings are also likely an effect of the higher power in this current study compared to previous smaller, clinical samples.
Previous studies have shown that both BPD (Zanarini et al. 2008; Kolla et al. 2008) and PTSD (Oquendo et al. 2005; Sareen et al. 2007; Sareen et al. 2005; Oquendo et al. 2003) are independently associated with a substantial risk of suicide attempts. The fact that individuals with comorbid PTSD-BPD were found to have increased odds of suicide attempts relative to individuals with either disorder alone is cause for concern. Findings of increased likelihood of suicide attempts in the histories of individuals with comorbid PTSD-BPD relative to individuals with PTSD alone are consistent with several previous studies, including the one previous community study (Connor et al. 2002; Heffernan & Cloitre, 2000). However, the current finding of a significantly higher prevalence of suicide attempts among individuals with comorbid PTSD-BPD relative to individuals with BPD alone has not been previously noted in the literature (Rusch et al. 2007). Our findings are especially important given that suicidal behaviors are included in the criteria for diagnosing BPD (American Psychiatric Association, 2000), and yet the presence of PTSD is associated with a much greater likelihood of suicide attempt(s) even among individuals with BPD. Given this association with suicide attempts and the potential for completed suicide (Owens et al. 2005; Suominen et al. 2004), it is especially important for clinicians to be aware of this increased risk and pay special attention to the assessment of suicidal behavior among individuals with comorbid PTSD-BPD.
As expected from diagnostic formulations and empirical literature, childhood trauma was prevalent across individuals with PTSD, BPD and PTSD-BPD comorbidity. However, the odds of experiencing all repeated traumas examined were significantly higher for individuals with comorbid PTSD-BPD. Sexual trauma in particular, relative to nonsexual trauma, was significantly more likely among individuals with PTSD-BPD compared to those with PTSD only (but not BPD only). Trauma appears to have a role in the etiology of both PTSD and BPD although the mechanisms by which trauma influences the genesis (and convergence) of these two disorders is uncertain (Sabo, 1997; Murray, 1993). Gunderson and Sabo propose that early trauma may affect personality development in a way that increases vulnerability for developing PTSD later in life (Gunderson & Sabo, 1993). Characterological traits may comprise an important part of the vulnerability that predisposes only a minority of individuals exposed to trauma to develop PTSD (Kessler et al. 1995). Previous studies have indeed shown childhood adversity to be a risk factor for subsequent PTSD (Bremner et al. 1993; Cabrera et al. 2007; Iversen et al. 2008; Widom, 1999). Multiple traumas and repetition of trauma early in life may be especially important in influencing the development of characterological vulnerabilities that may culminate in comorbid PTSD-BPD. It is important to remember, however, that most individuals who experience trauma do not develop PTSD and that although childhood trauma is common among individuals with BPD, it is not a prerequisite. As such, it is important for future longitudinal studies to examine the determinants of these disorders among individuals exposed to trauma.
Although BPD is more frequently diagnosed among females (American Psychiatric Association, 2000), a sizeable proportion of males met criteria for BPD in the current study and there was no difference in the prevalence of BPD across gender (Grant et al. 2008). The inclusion of males and our ability to examine interactions with gender is an important extension from previous studies, since most examinations of PTSD-BPD are confined to samples of females. Interestingly, few gender differences were observed in the current study. Despite the fact that fewer males may show up in clinical treatment settings it appears that PTSD-BPD comorbidity among men is associated with the same negative correlates as in women.
Several important limitations must be acknowledged in interpreting the findings of the current study. First, the NESARC Wave 2 data is cross-sectional, precluding any inferences of causality. This also makes it impossible to assess whether PTSD symptoms preceded BPD symptoms or vice versa. This also introduces the potential for recall bias in traumatic histories and lifetime psychopathology. Longitudinal studies in the general population where order of onset of disorders and potential determinants of comorbidity can be examined are necessary. Second, the lethality of suicide attempts was not assessed, precluding any distinction between parasuicidal gestures and more serious suicide attempts. Third, although the AUDADIS-IV is a valid and reliable method for lay interviewers to assess the presence of psychiatric disorders, personality disorders are difficult to assess and the role of clinical expertise may be more profound in Axis II diagnosis. The NESARC nonetheless provides the first opportunity to study the controversial overlap between PTSD and BPD in a nationally representative sample; as such, these limitations should temper rather than preclude inferential conclusions.
In summary, results of the current study confirm that the diagnoses of PTSD and BPD are not redundant and further emphasize the clinical utility of diagnosing both disorders for a comprehensive understanding of the impact of this comorbidity on mental health functioning. Whether or not the current DSM-IV criteria reflect the optimal configuration of these two diagnostic entities was not addressed by this study. This would be a potentially informative field trial for the framers of DSM-V to consider. Given the observed associations with childhood trauma – which provides a link to a growing literature on biological influences for PTSD – this seems like an important avenue for further investigation. Future research should further explore the determinants of having either or both diagnoses with an aim toward improved identification, prevention, and intervention.
Acknowledgements
The NESARC was supported by the National Institute on Alcohol and Related Conditions (NIAAA) and the National Institute on Drug Abuse. The research was supported by a Social Sciences and Humanities Research Council (SSHRC) Canada Graduate Scholarship (Pagura), a Manitoba Health Research Council (MHRC) operating grant (Bolton), the Canada Research Chairs program (Cox), a Canadian Institutes of Health Research (CIHR) New Investigator Award (Sareen), the Swampy Cree Suicide Prevention Team CIHR Operating Grant #82894, and MH64122 from the US National Institute of Mental Health (Stein).
Role of Funding Source
The NESARC was supported by the National Institute on Alcohol and Related Conditions (NIAAA) and the National Institute on Drug Abuse. The research was supported by a Social Sciences and Humanities Research Council (SSHRC) Canada Graduate Scholarship (Pagura), a Manitoba Health Research Council (MHRC) operating grant (Bolton), the Canada Research Chairs program (Cox), a Canadian Institutes of Health Research (CIHR) New Investigator Award (Sareen), the Swampy Cree Suicide Prevention Team CIHR Operating Grant #82894, and MH64122 from the US National Institute of Mental Health (Stein). These funding sources had no role in study design, analysis or interpretation of data, writing of the manuscript or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Author Sareen provided the initial conceptualization of the project. All authors contributed to the planning of statistical analyses. Author Pagura conducted the statistical analyses and wrote the initial draft of the manuscript. All authors provided ideas and feedback and to result in the final manuscript.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3 edn. Washington: American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR) Washington: American Psychiatric Association; 2000. [Google Scholar]
- Bolton EE, Mueser KT, Rosenberg SD. Symptom correlates of posttraumatic stress disorder in clients with borderline personality disorder. Comprehensive Psychiatry. 2006;47:357–361. doi: 10.1016/j.comppsych.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. American Journal of Psychiatry. 1993;150(2):235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Cabrera OA, Hoge CW, Bliese PD, Castro CA, Messer SC. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. American Journal of Preventive Medicine. 2007;33(2):77–82. doi: 10.1016/j.amepre.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT, Hughes DC, Swartz MS, Blazer DG, George LK. The impact of borderline personality disorder on post-traumatic stress in the community: A study of health status, health utilization and functioning. Comprehensive Psychiatry. 2002;43(1):41–48. doi: 10.1053/comp.2002.29846. [DOI] [PubMed] [Google Scholar]
- Famularo R, Kinscherff R, Fenton T. Posttraumatic stress disorder among children clinically diagnosed as borderline personality disorder. Journal of Nervous and Mental Disease. 1991;179(7):428–431. doi: 10.1097/00005053-199107000-00007. [DOI] [PubMed] [Google Scholar]
- Feeny NC, Zoellner LA, Foa EB. Treatment outcome for chronic PTSD among female assault victims with borderline personality characteristics: A preliminary examination. Journal of Personality Disorders. 2002;16(1):30–40. doi: 10.1521/pedi.16.1.30.22555. [DOI] [PubMed] [Google Scholar]
- Goldman SJ, D'Angelo EJ, DeMaso DR, Mezzacappa E. Physical and sexual abuse histories among children with borderline personality disorder. American Journal of Psychiatry. 1992;149(12):1723–1726. doi: 10.1176/ajp.149.12.1723. [DOI] [PubMed] [Google Scholar]
- Golier JA, Yehuda R, Bierer LM, Mitropoulou V, New AS, Schmeidler J, Silverman JM, Siever LJ. The relationship of borderline personality disorder to posttraumatic stress disorder and traumatic events. American Journal of Psychiatry. 2003;160:2018–2024. doi: 10.1176/appi.ajp.160.11.2018. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Smith SM, Dawson DA, Pulay AJ, Pickering RP, Ruan WJ. Prevalence, correlates, disability and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey of Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(4):533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003a;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda: National Institute on Alcohol Abuse and Alcoholism; 2003b. [Google Scholar]
- Grant BF, Kaplan KD. Source and accuracy statement for the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Rockville: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- Gunderson JG, Sabo AN. The phenomenological and conceptual interface between borderline personality disorder and PTSD. American Journal of Psychiatry. 1993;150(1):19–27. doi: 10.1176/ajp.150.1.19. [DOI] [PubMed] [Google Scholar]
- Harned MS, Chapman AL, Dexter-Mazza ET, Murray A, Comtois KA, Linehan MM. Treating co-occurring Axis I disorders in recurrently suicidal women with borderline personality disorder: A 2-year randomized trial of dialectical behavior therapy versus community treatment by experts. Journal of Consulting and Clinical Psychology. 2008;76(6):1068–1075. doi: 10.1037/a0014044. [DOI] [PubMed] [Google Scholar]
- Heffernan K, Cloitre M. A comparison of posttraumatic stress disorder with and without borderline personality disorder among women with a history of childhood sexual abuse: Etiological and clinical characteristics. Journal of Nervous and Mental Disease. 2000;188(9):589–595. doi: 10.1097/00005053-200009000-00005. [DOI] [PubMed] [Google Scholar]
- Herman JL. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress. 1992;5(3):377–391. [Google Scholar]
- Herman JL, Perry JC, van der Kolk BA. Childhood trauma in borderline personality disorder. American Journal of Psychiatry. 1989;146(4):490–495. doi: 10.1176/ajp.146.4.490. [DOI] [PubMed] [Google Scholar]
- Iversen AC, Fear NT, Ehlers A, Hacker Hughes J, Hull L, Earnshaw M, Greenberg N, Rona R, Wessely S, Hotopf M. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychological Medicine. 2008;38(4):511–522. doi: 10.1017/S0033291708002778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jogems-Kosterman BJM, de Knijff DWW, Kusters R, van Hoof JJM. Basal cortisol and DHEA levels in women with borderline personality disorder. Journal of Psychiatric Research. 2007;41:1019–1026. doi: 10.1016/j.jpsychires.2006.07.019. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kolla NJ, Eisenberg H, Links PS. Epidemiology, risk factors, and psychopharmacological management of suicidal behavior in borderline personality disorder. Archives of Suicide Research. 2008;12:1–19. doi: 10.1080/13811110701542010. [DOI] [PubMed] [Google Scholar]
- Lange W, Wulff H, Berea C, Beblo T, Saavedra AS, Mensebach C, Wingenfeld K, Driessen M. Dexamethasone suppression test in borderline personality disorder--Effects of posttraumatic stress disorder. Psychoneuroendocrinology. 2005;30:919–923. doi: 10.1016/j.psyneuen.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs. therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Murray JB. Relationship of childhood sexual abuse to borderline personality disorder, posttraumatic stress disorder, and multiple personality disorder. Journal of Psychology. 1993;127(6):657–676. doi: 10.1080/00223980.1993.9914905. [DOI] [PubMed] [Google Scholar]
- Ogata SN, Silk KR, Goodrich S, Lohr NE, Westen D, Hill EM. Childhood sexual and physical abuse in adult patients with borderline personality disorder. American Journal of Psychiatry. 1990;147(8):1008–1013. doi: 10.1176/ajp.147.8.1008. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Brent DA, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Burke AK, Firinciogullari S, Ellis SP, Mann JJ. Posttraumatic stress disorder comorbid with major depression: Factors mediating the association with suicidal behavior. American Journal of Psychiatry. 2005;162(3):560–566. doi: 10.1176/appi.ajp.162.3.560. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Friend JM, Halberstam B, Brodsky BS, Burke AK, Grunebaum MF, Malone KM, Mann JJ. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. American Journal of Psychiatry. 2003;160(3):580–582. doi: 10.1176/appi.ajp.160.3.580. [DOI] [PubMed] [Google Scholar]
- Owens D, Wood C, Greenwood DC, Hughes T, Dennis M. Mortality and suicide after non-fatal self-poisoning: 16-year outcome study. British Journal of Psychiatry. 2005;187:470–475. doi: 10.1192/bjp.187.5.470. [DOI] [PubMed] [Google Scholar]
- Rinne T, de Kloet ER, Wouters L, Goekoop JG, DeRijk RH, Van Den Brink W. Hyperresponsiveness of hypothalamic-pituitary-adrenal axis to combined dexamethasone/corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biological Psychiatry. 2002;52:1102–1112. doi: 10.1016/s0006-3223(02)01395-1. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch N, Corrigan PW, Bohus M, Kuhler T, Jacob GA, Lieb K. The impact of posttraumatic stress disorder on dysfunctional implicit and explicit emotions among women with borderline personality disorder. Journal of Nervous and Mental Disease. 2007;195:537–539. doi: 10.1097/NMD.0b013e318064e7fc. [DOI] [PubMed] [Google Scholar]
- Sabo AN. Etiological significance of associations between childhood trauma and borderline personality disorder: Conceptual and clinical implications. Journal of Personality Disorders. 1997;11(1):50–70. doi: 10.1521/pedi.1997.11.1.50. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJ. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine. 2007;69(3):242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- Sareen J, Houlahan T, Cox BJ, Asmundson GJG. Anxiety disorders associated with suicidal ideation and suicide attempts in the National Comorbidity Survey. Journal of Nervous and Mental Disease. 2005;193:450–454. doi: 10.1097/01.nmd.0000168263.89652.6b. [DOI] [PubMed] [Google Scholar]
- Shah BV, Barnswell BG, Bieler GS. Release 6.40 edn. Research Triangle Park: Research Triangle Institute; 1995. SUDAAN user's manual: Software for the analysis of correlated data. [Google Scholar]
- Shea MT, Zlotnick C, Weisberg RB. Commonality and specificity of personality disorder profiles in subjects with trauma histories. Journal of Personality Disorders. 1999;13(3):199–210. doi: 10.1521/pedi.1999.13.3.199. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Axelrod SR, Wang S, Yehuda R, Morgan CAI, Charney D, Rosenheck R, Mason JW. Twenty-four-hour urine cortisol in combat veterans with PTSD and comorbid borderline personality disorder. Journal of Nervous and Mental Disease. 2003;191(Suppl. 11):261–262. doi: 10.1097/01.NMD.0000061140.93952.28. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Yehuda R, Giller E. Personality disorders in treatment seeking Vietnam combat veterans with post-traumatic stress disorder. American Journal of Psychiatry. 1993;150:1020–1023. doi: 10.1176/ajp.150.7.1020. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, Smith SM, Ruan WJ, Pulay AJ, Saha TD, Pickering RP, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(7):1033–1045. doi: 10.4088/jcp.v69n0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: A 37-year follow-up study. American Journal of Psychiatry. 2004;161(3):562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- Swartz M, Blazer D, George L, Winfield I. Estimating the prevalence of borderline personality disorder in the community. Journal of Personality Disorders. 1990;4(3):257–272. [Google Scholar]
- Van Den Bosch LMC, Verheul R, Langeland W, Van Den Brink W. Trauma, dissociation, and posttraumatic stress disorder in female borderline patients with and without substance abuse problems. Australian and New Zealand Journal of Psychiatry. 2003;37:549–555. doi: 10.1046/j.1440-1614.2003.01199.x. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Kosinski M, Keller S. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. American Journal of Psychiatry. 1999;156(8):1223–1229. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- Wingenfeld K, Driessen M, Adam B, Hills A. Overnight urinary cortisol release in women with borderline personality disorder depends on comorbid PTSD and depressive psychopathology. European Psychiatry. 2007a;22:309–312. doi: 10.1016/j.eurpsy.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Wingenfeld K, Hill A, Adam B, Driessen M. Dexamethasone suppression test in borderline personality disorder: Impact of PTSD symptoms. Psychiatry and Clinical Neurosciences. 2007b;61:681–683. doi: 10.1111/j.1440-1819.2007.01728.x. [DOI] [PubMed] [Google Scholar]
- Wingenfeld K, Lange W, Wulff H, Berea C, Beblo T, Saavedra AS, Mensebach C, Driessen M. Stability of dexamethasone suppression test in borderline personality disorder with and without comorbid PTSD: A one-year follow-up study. Journal of Clinical Psychology. 2007c;63(9):843–850. doi: 10.1002/jclp.20396. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea R, Battle CL, Johnson DM, Zlotnick C, Dolan-Sewell R, Skodol AE, Grilo CM, Gunderson JG, Sanislow CA, Zanarini MC, Bender DS, Rettew JB, McGlashan TH. Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant and obsessive-compulsive personality disorders: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Nervous and Mental Disease. 2002;190(8):510–518. doi: 10.1097/00005053-200208000-00003. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, Reynolds V. Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry. 1998;155(12):1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. American Journal of Psychiatry. 2004;161:2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, Gunderson JG. The 10-year course of physically self-destructive acts reported by borderline patients and axis II comparison subjects. Acta Psychiatrica Scandinavica. 2008;117:177–184. doi: 10.1111/j.1600-0447.2008.01155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR. Childhood experiences of borderline patients. Comprehensive Psychiatry. 1989;30(1):18–25. doi: 10.1016/0010-440x(89)90114-4. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Mattia JI. Axis I diagnostic comorbidity and borderline personality disorder. Comprehensive Psychiatry. 1999;40(4):245–252. doi: 10.1016/s0010-440x(99)90123-2. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Franklin CL, Zimmerman M. Is comorbidity of posttraumatic stress disorder and borderline personality disorder related to greater pathology and impairment? American Journal of Psychiatry. 2002;159:1940–1943. doi: 10.1176/appi.ajp.159.11.1940. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Johnson DM, Yen S, Battle CL, Sanislow CA, Skodol AE, Grilo CM, McGlashan TH, Gunderson JG, Bender DS, Zanarini MC, Shea MT. Clinical features and impairment in women with borderline personality disorder (BPD) with posttraumatic stress disorder (PTSD), BPD without PTSD, and other personality disorders with PTSD. Journal of Nervous and Mental Disease. 2003;191(11):706–714. doi: 10.1097/01.nmd.0000095122.29476.ff. [DOI] [PubMed] [Google Scholar]