Abstract
Importance
While the enthusiasm for the Affordable Care Act (ACA) revolves around its impact on access to preventive and primary care services, the effect of this reform on surgical care remains undefined.
Objective
Using Massachusetts (MA) healthcare reform as a natural experiment, we estimate the differential impact of insurance expansion on the utilization of discretionary versus non-discretionary inpatient surgery.
Design
We used the State Inpatient Databases from MA and two control states to identify nonelderly patients (19–64 years) who underwent discretionary (DS) versus non-discretionary surgery (NDS) during the years 2003–2010. We defined DS as elective, preference-sensitive procedures (e.g., joint replacement, back surgery), and NDS as imperative and potentially lifesaving procedures (e.g., cancer surgery, hip fracture repair). Using July 2007 as the transition point between pre and post-reform periods, we performed a difference-in-differences (DID) analysis to estimate the effect of insurance expansion on rates of DS vs NDS among the entire study population, and for subgroups defined by race, income and insurance status. We then extrapolated our results from MA to the entire US population.
Main Outcome(s) and Measure(s)
Rate of DS and NDS performed before and after the healthcare reform in Massachusetts.
Results
We identified a total of 836,311 surgeries during the study period. In contrast to NDS, post-reform rates of DS increased more in MA than in control states. Based on our DID analysis, insurance expansion was associated with a 9.3% increase in the use of DS in MA (p=0.021). Conversely, the rate of NDS decreased by 4.5% (p=0.009). We found similar effects for DS in all subgroups, with the greatest increase observed for non-whites (19.9%, p<0.001). Based on the findings in MA, we estimated that full implementation of national insurance expansion would yield an additional 465,934 discretionary surgeries by 2017.
Conclusions and Relevance
Insurance expansion in Massachusetts was associated with increased rates of discretionary surgery, and a concurrent decrease in utilization of nondiscretionary surgery. If similar changes are seen nationally, the value of insurance expansion for surgical care may depend on the relative balance between increased expenditures and potential health benefits of greater access to elective inpatient procedures.
INTRODUCTION
Once implemented fully, it is anticipated that the Patient Protection and Affordable Care Act (ACA) will provide coverage for up to 25 million previously uninsured individuals in the United States. By virtue of new insurance exchanges, expansion of Medicaid, and individual requirements for insurance, proponents of the ACA believe that the legislation will enhance access to physicians and necessary health care services, thereby improving population health outcomes and potentially reducing costs over the long term.1–5
While much of the enthusiasm for the ACA revolves around providing patients with previously inaccessible preventive and primary care services, the effect of this reform on complex and expensive hospital-based care, including inpatient surgery, remains undefined. For instance, it is plausible that, due to a large unmet need, insurance expansion will yield greater use of surgery across the board. An alternative scenario, however, is that rates of surgery will change mainly for certain procedures and patient populations. Supporting the latter hypothesis, existing data suggest that access to imperative surgical procedures like hip fracture repair and colectomy for cancer may not be affected by insurance status. 6,7 Conversely, decisions about the use of other, more discretionary, procedures (e.g., joint replacement, back surgery) may be strongly influenced by insurance coverage, 6–12 and utilization of such surgeries could change most prominently among populations who are at highest risk for being currently uninsured.13,14
Previous investigators have used the outcomes of healthcare reform in Massachusetts to forecast the ACA’s impact on racial disparities with inpatient surgery.13,14 Herein, we build on this work by examining the impact of the Massachusetts insurance expansion on utilization of discretionary versus non-discretionary surgical procedures. We specifically compare the pre- and post-reform rates of discretionary and non-discretionary procedures in Massachusetts to those for two control states where no similar reform was implemented. In addition, we assess whether the impact of insurance expansion varies across subgroups that differed in their baseline (i.e., pre-reform) risk of being uninsured. By virtue of this approach, our findings will provide policymakers with more nuanced insight regarding the potential impact of national insurance expansion for utilization of inpatient surgery.
METHODS
Data Sources
Our primary datasets were the State Inpatient Databases (SID) for Massachusetts and two Northeastern control states (New York and New Jersey). 15 We selected New Jersey and New York as controls because both states: 1) are in close geographic proximity to Massachusetts; 2) had a steady nonelderly uninsured rate during the study period;16 3) had data available in the SID before and after implementation of health care reform in Massachusetts. In addition to the SID, we used U.S. Census data to account for population growth during the study interval, and to obtain county level measures of insurance status and household income.16–18 Because we used publically available data, this study was deemed exempt from review by the University of Michigan Institutional Research Board.
Study population and primary outcome
Our study population included all nonelderly patients (ages 19–64) who underwent selected surgeries from January 1, 2003 through December 31, 2010. We excluded patients who did not reside in Massachusetts or the control states.
Our outcome of interest was the rate of discretionary and non-discretionary inpatient surgeries in Massachusetts and in control states. For this analysis, we defined discretionary procedures as inpatient surgeries with high levels of preference sensitivity, potential medical management alternatives, and a large degree of geographic variation.6–8 We hypothesized that the rate of these surgeries will increase with insurance expansion. Based on this framework, we decided a priori to include knee replacement, hip replacement, transurethral resection of the prostate, back surgery, and inguinal hernia repair as discretionary surgeries. We removed all patients undergoing “emergent” surgery from the discretionary group.
As a comparison group, we also identified a set of non-discretionary inpatient procedures. We defined these as imperative surgical procedures that address an immediately threatening diagnosis (e.g., cancer, acute appendicitis). A priori, we specifically classified major cancer surgeries19, appendectomy and hip fracture repair as non-discretionary surgeries (eTable I). In addition to clinical judgment, our selection of these procedures was based existing literature suggesting that they have relatively lower levels of preference and insurance sensitivity.6–8,20–22 We hypothesized that, compared with discretionary procedures, rates of non-discretionary surgeries will be affected less by insurance expansion. Ultimately, our analysis included 5 discretionary and 10 non-discretionary surgeries (eTable 1).
Reform period
We assigned July 2007 as the transition point between the pre- and post-reform eras in Massachusetts. We selected this date for several reasons. First, although the law was enacted in April 2006, its provisions were implemented in a staggered fashion from July 2006 through July 2007, and the number of uninsured individuals did not decline significantly until 2007.16,23 Second, significant components of the reform (i.e., the individual and employer mandates) did not take effect until July 2007.24 Third, this approach is consistent with that used by other investigators evaluating the impact of health care reform in Massachusetts. 23,25,26
Statistical Analyses
In our first analytic step, we compared the characteristics of patients who underwent surgery in Massachusetts versus control states from 2003 through 2010. Next, we calculated the mean (unadjusted) rates of discretionary and non-discretionary surgery in Massachusetts and control states before and after July 2007.
We then performed a difference-in-differences (DID) analysis to estimate the effect of healthcare reform on rates of discretionary versus non-discretionary surgery. DID analysis is a widely used empirical strategy that allows adjustment for secular changes that may under or overestimate the true effect of the reform.13,14,27–30 We implemented the DID analysis by fitting separate ordinary least square regression models for discretionary and non-discretionary procedures. The dependent variable for each model was the total number of surgeries in each state per quarter per 10,000 individuals. We included variables specifying the state where the surgery was performed, as well as reform status (i.e., whether the surgery was performed before or after July 2007). Our models also included an interaction term for the state and reform status variables. The coefficient on this interaction term represents the difference-in-differences estimator. Finally, we included an unemployment variable in the models to account for the five percentage point rise in unemployment from 2006 through 2009 (a result of economic recession),26 and we adjusted for seasonal differences in rates of surgery.31
Subgroup analyses
Because the implications of insurance expansion may vary across patient populations, we decided a priori to perform separate analyses for the following patient subgroups: 1) non-Hispanic whites; 2) non-whites; 3) low income; and 4) newly insured. We identified the first two groups using the race variable in the SID. The non-white category included blacks and patients of Hispanic origin. Using county-level data as a proxy, we defined low-income patients as those living in the tercile of counties in Massachusetts with the lowest median income (Suffolk, Berkshire, Dukes, Franklin, Hampden). We also specified a subgroup of patients with the greatest likelihood of being newly-insured after the implementation of healthcare reform. This group included patients living in the five Massachusetts counties with the greatest number of individuals gaining insurance from 2006 through 2008 (Norfolk, Worcester, Essex, Suffolk, Middlesex). 16 After defining these subgroups, we applied the DID framework described above to compare rates of discretionary and non-discretionary surgery.
Sensitivity analyses
We performed sensitivity analyses to examine the robustness of our findings to several key assumptions. First, we excluded patients who had surgery during the reform implementation period prior to our transition point (i.e., from January 2006 through June 2007).13,14 This step removed from analysis newly insured patients who had surgery after parts of the reform were enacted, but prior to our transition point (July 2007). Including such patients may attenuate the effects of reform. Second, we repeated our analyses after excluding patients who were aged 19–64 and covered by Medicare (e.g., disabled, end stage renal disease) since these individuals should have not experienced a substantive change in their insurance status during the reform period. Third, we performed the DID analysis for each of the individual surgeries comprising the discretionary and non-discretionary groups to assess whether changes in the rates of single procedures might be driving our overall results. Finally, using 2003 as the reference year, we fit models that estimated the change in surgery rates in Massachusetts relative to the comparison states in each year as if there were a reform in that year (i.e., a placebo analysis). We expected that there would be no change in the rate of surgery for 2004, 2005, 2006 (i.e., “placebo” years prior to the reform) relative to 2003. All analyses were performed using computerized software (STATA 13/SE, College Station, TX), and at the 5% significance level.
Calculation of national estimates for inpatient surgeries
To arrive at national estimates for the effect of insurance expansion on the utilization of inpatient surgery, we first determined the number of new procedures performed in Massachusetts. Assuming that these new procedures were due to insurance gains, we calculated the percentage of newly insured individuals who underwent surgery. We then used a recent Congressional Budget Office (CBO) estimate of the number of individuals who will be newly insured through national insurance expansion (25 million by 2017) to yield corresponding estimates for the entire United States population.32
RESULTS
We identified a total of 836,311 nonelderly patients who underwent surgery (22% MA, 55% NY, 23% NJ) from January 1, 2003 through December 31, 2010. Table 1 presents the pre- and post-reform characteristics of patients from Massachusetts and control states. While the percentage of surgical patients receiving free care in Massachusetts declined from 4.7% to 2.1% after reform, no similar change was observed in control states. During the entire study interval, percentage of patients in Massachusetts receiving free care for non-discretionary surgery exceeded that for discretionary surgery (eFigure 1).
Table 1.
Demographics of patients undergoing surgery before and after Massachusetts healthcare reform
| Massachusetts | Control | ||||
|---|---|---|---|---|---|
| Pre-reform | Post-reform | Pre-reform | Post-reform | ||
| Surgery (%) | Discretionary | 65.4 | 69.1 | 60.8 | 62.6 |
| Non-discretionary | 34.6 | 30.9 | 39.2 | 37.4 | |
| Age (%) | 19–40 | 23.8 | 20.3 | 26.9 | 24.5 |
| 40–64 | 76.1 | 79.7 | 73.1 | 75.5 | |
| Female (%) | 50.1 | 51.4 | 50.4 | 51.5 | |
| Race (%) | White | 87.4 | 85.9 | 72.3 | 69.7 |
| Black | 4.3 | 5.0 | 10.2 | 10.6 | |
| Hispanic | 4.8 | 6.0 | 10.1 | 11.2 | |
| Other | 3.5 | 3.1 | 7.4 | 8.5 | |
| Payer (%) | Medicare | 7.5 | 9.1 | 6.7 | 7.6 |
| Medicaid | 8.1 | 9.8 | 8.5 | 10.5 | |
| Private | 75.2 | 72.1 | 70.5 | 67.3 | |
| Self-pay | 1.4 | 0.7 | 5.6 | 5.8 | |
| Free care | 3.3 | 1.4 | 0.1 | 0.1 | |
| Other | 4.5 | 7.0 | 8.6 | 8.8 | |
Patients undergoing surgery during pre and post-reform periods in Massachusetts and control periods are compared. The pre and post-reform transition point is defined as July 2007. In the payer categories, “Other” includes worker’s compensation, Health Safety Net, other government payment, other non-managed care plans, and CommCare (a free or subsidized health care insurance program)
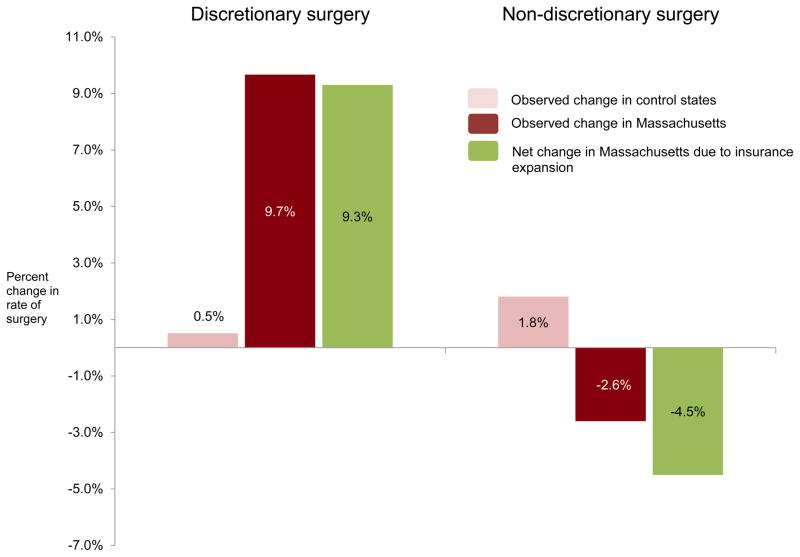
In Massachusetts, the unadjusted mean rate of discretionary surgery increased by 9.7% from before (35.6 cases/year/10,000 individuals) to after (39.2 cases/year/10,000 individuals) reform (Table 2). In contrast, the mean rate of discretionary surgery in the control states increased by only 0.5%. The mean rate of non-discretionary surgery decreased slightly in Massachusetts after reform, and increased slightly in the control states (Table 2). The difference-in-differences analysis demonstrated that insurance expansion was associated with a 9.3% net increase in the rate of discretionary surgery and a 4.5% net decrease in the rate of non-discretionary surgery (Figure 1).
Table 2.
Pre and post-reform annual rates of discretionary and non-discretionary surgery
| Discretionary | Non-discretionary | ||||
|---|---|---|---|---|---|
| Pre-reform | Post-reform | Pre-reform | Post-reform | ||
| All | MA | 35.8 | 39.2 | 18.5 | 18.0 |
| Control | 28.9 | 29.0 | 18.3 | 18.7 | |
| White | MA | 35.9 | 40.4 | 16.7 | 16.6 |
| Control | 27.2 | 28.0 | 14.6 | 14.8 | |
| Non-white | MA | 17.5 | 21.7 | 15.2 | 17.0 |
| Control | 14.6 | 15.3 | 13.6 | 14.8 | |
| Low Income | MA | 35.9 | 39.2 | 22.8 | 21.8 |
| Control | 22.8 | 23.8 | 16.6 | 17.0 | |
| Newly Uninsured | MA | 32.5 | 36.0 | 18.5 | 17.5 |
| Control | 28.9 | 29.0 | 18.3 | 18.7 | |
Abbreviations: MA, Massachusetts. Values represent unadjusted mean rates of surgery per year per 10,000 individuals in each subgroup. The pre and post-reform transition point is defined as July 2007. Low income refers to patients residing in Massachusetts counties with low median income. Newly insured refers to patients residing in Massachusetts counties with high numbers of individuals gaining insurance from 2006–2008. Control states are New York and New Jersey.
Figure 1. Changes in discretionary and non-discretionary surgery after insurance expansion in Massachusetts.
Bar graphs represent percent change in the mean rate of discretionary and non-discretionary surgery from before to after Massachusetts healthcare reform (July 2007). Control states are New Jersey and New York. Net change in Massachusetts due insurance expansion was determined using multivariable difference-in-differences analysis and represents change in rate of surgery attributed to insurance expansion.
Subgroup analyses
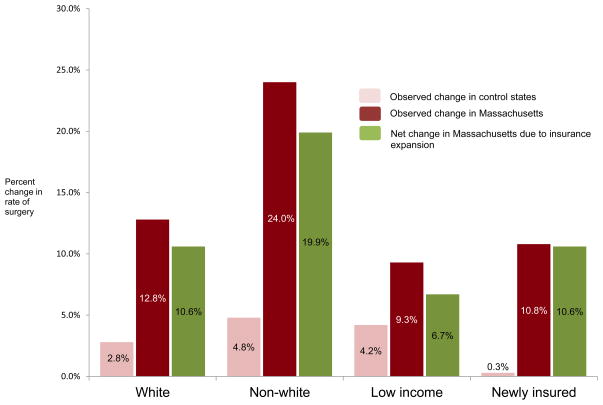
For each subgroup, we observed an increase in the unadjusted mean rates of discretionary procedures in Massachusetts versus control states; concurrently, rates of non-discretionary surgery remained either stable or decreased during the same time period (Table 2). Based on the DID analysis, the effect of insurance expansion was greatest for the non-white population, for whom health care reform was associated with a 19.9% increase in the rate of discretionary surgery (Figure 2). Although variable in magnitude, insurance expansion yielded analogous increases in discretionary surgery for all other subgroups of interest (Figure 2). Table 3 presents the difference-in-differences estimators for discretionary and non-discretionary surgery for both the entire study population and specific subgroups of interest. Our sensitivity analyses revealed no substantive changes in the principal findings (eTables 2–5). When we analyzed procedures individually, utilization increased for all discretionary surgeries with statistically significant results observed for knee and hip replacement, and inguinal hernia repair (eTable 4). Among non-discretionary surgeries, a statistically significant 6% reduction in appendectomy was noted.
Figure 2. Changes in discretionary surgery after insurance expansion in Massachusetts, by subgroups.
Bar graphs represent percent change in the mean rate of discretionary surgery from before to after Massachusetts healthcare reform (July 2007). Non-white population includes blacks and patients of Hispanic origin. Low income refers to patients residing in Massachusetts counties with low median income. Newly insured refers to patients residing in Massachusetts counties with high numbers of individuals gaining insurance from 2006–2008. Control states are New Jersey and New York. Net change in Massachusetts due insurance expansion was determined using multivariable difference-in-differences analysis and represents the change in rate of surgery attributable to insurance expansion.
Table 3.
Net change in the rates of discretionary and non-discretionary surgery resulting from Massachusetts healthcare reform
| All | White | Non-white | Low income | Newly insured | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| coefficient | p-value | %change | coefficient | p-value | %change | coefficient | p-value | %change | coefficient | p-value | %change | coefficient | p-value | %change | |
| Discretionary | 0.83 | 0.021 | 9.3% | 0.95 | 0.003 | 10.6% | 0.87 | <0.001 | 19.9% | 0.60 | 0.004 | 6.7% | 0.86 | 0.017 | 10.6% |
| Non-discretionary | −0.21 | 0.009 | −4.5% | −0.09 | 0.142 | −2.2% | 0.15 | 0.401 | 3.9% | −0.36 | <0.001 | −6.3% | −0.32 | <0.001 | −6.9% |
Results of the multivariable difference-in-differences (DID) analysis showing change in rates of discretionary and non-discretionary surgery in Massachusetts compared to control states. Reform transition point is defined as July 2007. Coefficient refers to the DID estimator and % change refers to coefficient divided by pre-reform rate. Low income refers to patients residing in Massachusetts counties with low median income. Newly insured refers to patients residing in Massachusetts counties with high numbers of individuals gaining insurance from 2006–2008.
Calculation of national estimates for inpatient surgeries
Using the DID estimator from our primary analysis, we determined that insurance expansion led to 2,202 more discretionary surgeries in Massachusetts. Assuming that these additional procedures were provided solely to patients with new insurance coverage, we calculated that1.86% of newly insured individuals in Massachusetts underwent a discretionary inpatient procedure. This corresponds to an additional 4,659 elective surgeries performed nationally per 1% increase in insurance coverage. If national insurance expansion provisions in ACA are fully implemented, we estimate that up to 465,934 discretionary surgeries will be performed by 2017 (eTable 6).
DISCUSSION
Insurance expansion in Massachusetts led to greater use of discretionary inpatient surgeries. Not surprisingly, this effect was greatest for populations at highest risk for being uninsured in Massachusetts before reform. By translating the Massachusetts experience to the national level, we estimated that insurance expansion will result in up to 500,000 new discretionary surgeries (i.e., knee replacement, hip replacement, back surgery, inguinal hernia repair, transurethral resection of prostate) by 2017.
Previous investigators have demonstrated convincingly that healthcare utilization rises when previously uncovered patients acquire health insurance.10,33–35 The current study clarifies this broader relationship by demonstrating that, for inpatient surgical care, the effect of policies aimed at increasing coverage is not uniform. Instead, it appears that patients in need of imperative or non-discretionary inpatient surgery tend to get this care whether or not they have insurance. In contrast, insurance expansion is an important driver of utilization for the relatively large population of patients who are potential candidates for discretionary or elective procedures. Once coverage is available, many of these move forward with surgical treatment. Similar findings have been observed in patients newly eligible for the Medicare program.10,36
We also observed lower rates of non-discretionary surgery in Massachusetts relative to control states after healthcare reform. This change was most apparent for patients from counties with high rates of low-income and newly insured individuals. There are several potential explanations for this finding. First, it is plausible that better access to primary and specialty care in Massachusetts contributed to some reduction in the need for non-discretionary surgery (e.g., increased use of colonoscopy may have led to lower rates of surgically treated cancer). However, the time needed to see such a change is likely longer than our study period.37 Second, while insurance expansion did not appear to “crowd out” access to hospitalization for Medicare beneficiaries, this effect may be significant for surgical procedures, particularly if greater use of elective surgeries competes for finite hospital resources.31 Finally, in the case of appendectomy, the observed reduction in post-reform rates may indicate that insured patients are presenting early and surgeons are able to perform uncomplicated procedures that do not require an inpatient stay. 20,22,38–40 Ultimately, a better understanding of these issues will be needed to clarify the relationship between insurance expansion and non-discretionary surgical care.
For discretionary procedures, our finding that the non-white population was most strongly impacted by insurance expansion is also consistent with findings reported by other investigators.13,14,24 Taken together, these data suggest that insurance expansion may achieve an intended consequence of attenuating racial disparities in access to care, at least for certain inpatient surgeries. It is unclear, however, whether greater access to such procedures will ultimately close existing gaps between white and non-white populations with respect to overall health status.
Our study does have several limitations. First, there is no standard definition for discretionary and non-discretionary surgery. Thus, we while classified procedures a priori based on both the existing literature and clinical experience, we cannot know with certainty whether any one surgery was truly discretionary or not. Second, because we looked only at utilization of surgical procedures, we do not know whether insurance expansion affected other factors such as the timing or quality of surgery.41,42 Third, our analysis did not include outpatient surgical procedures. Accordingly, we could not examine trends in the utilization of cataract surgery, cystoscopy, gastrointestinal endoscopy, and other procedures for which utilization may be particularly sensitive to changes in insurance status or supply of providers. 43,44 Finally, because our outcome variable was a state-level rate, we did not adjust for patient-level variables in our regression models. Nonetheless, while there were some baseline differences in age, race, and payer mix between patients in the control states and Massachusetts, at the state-level these demographic differences were stable at over time and therefore unlikely to affect our estimates.
These limitations notwithstanding, our findings may help many stakeholders anticipate the effects of national insurance expansion through the ACA. Relevant to policymakers, our results suggest that expected long-term cost savings from national insurance expansion may be dampened to some extent by increased use of certain expensive inpatient elective surgeries.5,35 To this point, healthcare spending in Massachusetts has grown substantially in the last 5 years. 45–47 From a policy perspective, the value of such expenditures will depend on whether, and to what extent, greater access to such procedures actually improves quality and/or quantity of life for newly insured individuals.
Many payers anticipate that insurance expansion will save money by providing access to care that prevents expensive hospitalizations.25 Our findings suggest that such savings that could be offset by greater expenditures for elective inpatient procedures. Given this possibility, payers arguably have strong incentives to work with and support surgeons in their efforts to define optimal selection criteria for many elective surgical procedures.48 Our findings are also relevant to physicians and specialty societies because they suggest that some surgical disciplines (e.g., orthopedic surgery) could experience a rapid growth in demand with implementation of the ACA. This could have important implications for both post-graduate training programs and for patients seeking access to such care, particularly in areas with fewer surgical specialists.49,50 Finally, for patients who currently lack coverage, insurance expansion offers the promise of secondary improvements in overall health status and quality of life through access to procedures that treat debilitating conditions such as severe osteoarthritis.51 However, as seen in Massachusetts, if payers ultimately experience greater expenditures as a consequence of covering more elective inpatient surgeries, then all patients may ultimately face higher premiums.52
Our collective findings suggest that insurance expansion leads to greater utilization of discretionary inpatient procedures that are often performed to improve quality of life rather than to address immediately life-threatening conditions. Moving forward, research in this area should focus on whether greater utilization of such procedures represents a response to unmet need or changes in treatment thresholds driven by patients, providers, or some combination of the two. In addition, it will be important to examine and define the individual and societal-level returns (e.g., better health outcomes, increased productivity, reduced rates of disability) achieved with such surgical interventions. In the end, the value of insurance expansion for surgical care may depend on the relative balance between increased expenditures and the measurable health benefits derived from greater access to elective inpatient surgery.
Supplementary Material
Acknowledgments
Matthew Davis, M.D., M.P.P
Professor of Pediatrics and Communicable Diseases, Internal Medicine, University of Michigan Medical School
Professor of Public Policy, Gerald R. Ford School of Public Policy
Contribution: Review of manuscript (no compensation)
FINANCIAL SUPPORT:
This research was supported by the Agency for Healthcare Research and Quality (K08 HS018346-01A1 to Dr. Miller), Urology Care Foundation (Astellas Rising Star in Urology Research Award to Dr. Miller) and the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney (T32 DK 7782-14 to Dr. Ellimoottil)
Footnotes
CONFLICTS OF INTEREST:
Chandy Ellimoottil, M.D: None
Sarah Miller, Ph.D: None
John Z. Ayanian, M.D., M.P.P: None
David C. Miller, M.D: None
ACCOUNTABILITY:
Chandy Ellimoottil, MD had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis
References
- 1.Baker DW, Sudano JJ, Durazo-Arvizu R, Feinglass J, Witt WP, Thompson J. Health insurance coverage and the risk of decline in overall health and death among the near elderly, 1992–2002. Med Care. 2006;44(3):277–82. doi: 10.1097/01.mlr.0000199696.41480.45. [DOI] [PubMed] [Google Scholar]
- 2.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med. 2007;357(2):143–53. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- 3.McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Health insurance coverage and mortality among the near-elderly. Health Aff (Millwood) 2004;23(4):223–33. doi: 10.1377/hlthaff.23.4.223. [DOI] [PubMed] [Google Scholar]
- 4.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Health of previously uninsured adults after acquiring Medicare coverage. JAMA. 2007;298(24):2886–94. doi: 10.1001/jama.298.24.2886. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Hidden costs, value lost: uninsurance in America. Washington, DC: National Academy Press; 2003. Jun, 2003. [PubMed] [Google Scholar]
- 6.Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery. 1998;124(5):917–23. [PubMed] [Google Scholar]
- 7.Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121–9. doi: 10.1016/S0140-6736(13)61215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinstein JN, Bronner KK, Morgan TS, Wennberg JE. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood) 2004;(Suppl Vari):VAR81–9. doi: 10.1377/hlthaff.var.81. [DOI] [PubMed] [Google Scholar]
- 9.Lurie JD, Bell JE, Weinstein J. What rate of utilization is appropriate in musculoskeletal care? Clin Orthop Relat Res. 2009;467(10):2506–11. doi: 10.1007/s11999-009-0889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Card D, Dobkin C, Maestas N. The Impact of Nearly Universal Insurance Coverage on Health Care Utilization: Evidence from Medicare. Am Econ Rev. 2008;98(5):2242–2258. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mota REM, Tarricone R, Ciani O, Bridges JFP, Drummond M. Determinants of demand for total hip and knee arthroplasty: a systematic literature review. BMC Health Serv Res. 2012;12:225. doi: 10.1186/1472-6963-12-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hanchate AD, Zhang Y, Felson DT, Ash AS. Exploring the determinants of racial and ethnic disparities in total knee arthroplasty: health insurance, income, and assets. Med Care. 2008;46(5):481–8. doi: 10.1097/MLR.0b013e3181621e9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanchate AD, Lasser KE, Kapoor A, et al. Massachusetts reform and disparities in inpatient care utilization. Med Care. 2012;50(7):569–77. doi: 10.1097/MLR.0b013e31824e319f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loehrer AP, Song Z, Auchincloss HG, Hutter MM. Massachusetts Health Care Reform and Reduced Racial Disparities in Minimally Invasive Surgery. JAMA Surg. 2013;02114:1–7. doi: 10.1001/jamasurg.2013.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. [Accessed December 4, 2013.];Healthcare Cost and Utilization Project. http://www.hcup-us.ahrq.gov.
- 16.United States Census Bureau. [Accessed October 1, 2013];Small Area Health Insurance Estimates. http://www.census.gov/did/www/sahie/
- 17.United States Census Bureau. [Accessed October 1, 2013.];Population Estimates. http://www.census.gov/popest/data/intercensal.
- 18.United States Census Bureau. [Accessed October 1, 2013.];Small Area Income and Poverty Estimates. http://www.census.gov/did/www/saipe.
- 19.Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280(20):1747–51. doi: 10.1001/jama.280.20.1747. [DOI] [PubMed] [Google Scholar]
- 20.Livingston EH, Fairlie RW. Little effect of insurance status or socioeconomic condition on disparities in minority appendicitis perforation rates. Arch Surg. 2012;147(1):11–7. doi: 10.1001/archsurg.2011.746. [DOI] [PubMed] [Google Scholar]
- 21.Nwomeh BC, Chisolm DJ, Caniano Da, Kelleher KJ. Racial and socioeconomic disparity in perforated appendicitis among children: where is the problem? Pediatrics. 2006;117(3):870–5. doi: 10.1542/peds.2005-1123. [DOI] [PubMed] [Google Scholar]
- 22.Gadomski a, Jenkins P. Ruptured appendicitis among children as an indicator of access to care. Health Serv Res. 2001;36(1 Pt 1):129–42. [PMC free article] [PubMed] [Google Scholar]
- 23.Long SK. On the road to universal coverage: impacts of reform in massachusetts at one year. Health Aff (Millwood) 2008;27(4):w270–84. doi: 10.1377/hlthaff.27.4.w270. [DOI] [PubMed] [Google Scholar]
- 24.Courtemanche Charles, Zapata Daniela. Does Universal Coverage Improve Health? The Massachusetts Experience (July 1, 2012) Andrew Young School of Policy Studies Research Paper Series No. 12-19. doi: 10.1002/pam.21737. [DOI] [PubMed] [Google Scholar]
- 25.Kolstad JT, Kowalski AE. The Impact of Health Care Reform on Hospital and Preventive Care: Evidence from Massachusetts(☆) J Public Econ. 2012;96(11–12):909–929. doi: 10.1016/j.jpubeco.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Long SK, Stockley K. Sustaining health reform in a recession: an update on Massachusetts as of fall 2009. Health Aff (Millwood) 2010;29(6):1234–41. doi: 10.1377/hlthaff.2010.0337. [DOI] [PubMed] [Google Scholar]
- 27.Long BSK, Stockley K, Yemane A. Another Look at the Impacts of Health Reform in Massachusetts : Evidence Using New Data and a Stronger Model. American Economic Review: Papers & Proceedings. 2009;99(2):508–511. doi: 10.1257/aer.99.2.508. [DOI] [PubMed] [Google Scholar]
- 28.Miller S. The effect of insurance on emergency room visits: An analysis of the 2006 Massachusetts health reform. J Public Econ. 2012;96(11–12):893–908. [Google Scholar]
- 29.Miller S. Findings from Massachusetts Health Reform : Lessons for Other States The Effect of the Massachusetts Reform on Health Care Utilization. Inquiry. 2013;49:1–10. [Google Scholar]
- 30.Miller S. The Impact of the Massachusetts Health Care Reform on Health Care Use Among Children. Am Econ Rev. 2012;102(3):502–507. doi: 10.1257/aer.102.3.502. [DOI] [PubMed] [Google Scholar]
- 31.Joynt KE, Chan D, Orav EJ, Jha AK. Insurance expansion in Massachusetts did not reduce access among previously insured Medicare patients. Health Aff (Millwood) 2013;32(3):571–8. doi: 10.1377/hlthaff.2012.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Congressional Budget Office. [Accessed December 4, 2013.]; www.cbo.gov/sites/default/files/cbofiles/attachments/44190_EffectsAffordableCareActHealthInsuranceCoverage_2.pdf.
- 33.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med. 2007;357(2):143–53. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- 34.Baicker K, Finkelstein A. The effects of Medicaid coverage--learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–5. doi: 10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hadley J. Sicker and Poorer—The Consequences of Being Uninsured: A Review of the Research on the Relationship between Health Insurance, Medical Care Use, Health, Work, and Income. Med Care Res Rev. 2003;60(2):3–75. doi: 10.1177/1077558703254101. [DOI] [PubMed] [Google Scholar]
- 36.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Medicare spending for previously uninsured adults. Ann Intern Med. 2009;151(11):757–66. doi: 10.7326/0003-4819-151-11-200912010-00149. [DOI] [PubMed] [Google Scholar]
- 37.Van Der Wees PJ, Zaslavsky AM, Ayanian JZ. Improvements in health status after massachusetts health care reform. Milbank Q. 2013;91(4):663–89. doi: 10.1111/1468-0009.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331(7):444–9. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 39.Smink DS, Fishman SJ, Kleinman K, Finkelstein Ja. Effects of race, insurance status, and hospital volume on perforated appendicitis in children. Pediatrics. 2005;115(4):920–5. doi: 10.1542/peds.2004-1363. [DOI] [PubMed] [Google Scholar]
- 40.Ponsky TA, Huang ZJ, Kittle K, et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292(16):1977–82. doi: 10.1001/jama.292.16.1977. [DOI] [PubMed] [Google Scholar]
- 41.Ayanian JZ, Kohler BA, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993;329(5):326–31. doi: 10.1056/NEJM199307293290507. [DOI] [PubMed] [Google Scholar]
- 42.Billmeier SE, Ayanian JZ, Zaslavsky AM, Nerenz DR, Jaklitsch MT, Rogers SO. Predictors and outcomes of limited resection for early-stage non-small cell lung cancer. J Natl Cancer Inst. 2011;103(21):1621–9. doi: 10.1093/jnci/djr387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hollenbeck BK, Hollingsworth JM, Dunn RL, Zaojun Ye, Birkmeyer JD. Ambulatory surgery center market share and rates of outpatient surgery in the elderly. Surg Innov. 2010;17(4):340–5. doi: 10.1177/1553350610377211. [DOI] [PubMed] [Google Scholar]
- 44.Hollingsworth JM, Krein SL, Ye Z, Kim HM, Hollenbeck BK. Opening of ambulatory surgery centers and procedure use in elderly patients: data from Florida. Arch Surg. 2011;146(2):187–93. doi: 10.1001/archsurg.2010.335. [DOI] [PubMed] [Google Scholar]
- 45.Steinbrook R. Controlling health care costs in Massachusetts with a global spending target. JAMA. 2012;308(12):1215–6. doi: 10.1001/2012.jama.11322. [DOI] [PubMed] [Google Scholar]
- 46.Song Z, Landon BE. Controlling health care spending--the Massachusetts experiment. N Engl J Med. 2012;366(17):1560–1. doi: 10.1056/NEJMp1201261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ayanian JZ, Van der Wees PJ. Tackling rising health care costs in Massachusetts. N Engl J Med. 2012;367(9):790–3. doi: 10.1056/NEJMp1208710. [DOI] [PubMed] [Google Scholar]
- 48.Share Da, Campbell Da, Birkmeyer N, et al. How a regional collaborative of hospitals and physicians in Michigan cut costs and improved the quality of care. Health Aff (Millwood) 2011;30(4):636–45. doi: 10.1377/hlthaff.2010.0526. [DOI] [PubMed] [Google Scholar]
- 49.Etzioni Da, Liu JH, Maggard Ma, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238(2):170–7. doi: 10.1097/01.SLA.0000081085.98792.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams TE, Satiani B, Ellison EC. A comparison of future recruitment needs in urban and rural hospitals: the rural imperative. Surgery. 2011;150(4):617–25. doi: 10.1016/j.surg.2011.07.047. [DOI] [PubMed] [Google Scholar]
- 51.Ravi B, Croxford R, Austin PC, et al. The relation between total joint arthroplasty and risk for serious cardiovascular events in patients with moderate-severe osteoarthritis: propensity score matched landmark analysis. BMJ. 2013;347(October):f6187. doi: 10.1136/bmj.f6187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cogan JF, Hubbard RG, Kessler D. The Effect of Massachusetts’ Health Reform on Employer-Sponsored Insurance Premiums. Forum Health Econ Policy. 2010;13(2):1075–1077. doi: 10.2202/1558-9544.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.