Abstract
[Purpose] Knee joint proprioception combines sensory input from a variety of afferent receptors that encompasses the sensations of joint position and motion. Poor proprioception is one of the risk factors of anterior cruciate ligament injury. Most studies have favored testing knee joint position sense in the sagittal plane and non-weight-bearing position. One of the most common mechanisms of noncontact anterior cruciate ligament injury is dynamic knee valgus. No study has measured joint position sense in a manner relevant to the mechanism of injury. Therefore, the aim of this study was to measure knee joint position sense in the noncontact anterior cruciate ligament injury risk position and normal condition. [Subjects and Methods] Thirty healthy male athletes participated in the study. Joint position sense was evaluated by active reproduction of the anterior cruciate ligament injury risk position and normal condition. The dominant knees of subjects were tested. [Results] The results showed less accurate knee joint position sense in the noncontact anterior cruciate ligament injury risk position rather than the normal condition. [Conclusion] The poorer joint position sense in non-contact anterior cruciate ligament injury risk position compared with the normal condition may contribute to the increased incidence of anterior cruciate ligament injury.
Key words: Anterior cruciate ligament, Proprioception, Injury risk position
INTRODUCTION
Knee joint proprioception combines different sensory inputs from a variety of receptors. Proprioception involves joint position sense (JPS) and detection of motion1). JPS refers to the awareness of joint position and is mediated through various receptors called mechanoreceptors2). Mechanoreceptors, including Ruffini endings, Pacinian corpuscles, and Golgi tendon organ-like receptors, have been found in the human anterior cruciate ligament (ACL). These mechanoreceptors convert applied mechanical loads into afferent impulses to regulate the stability of the knee joint and possibly prevent ligament injury3, 4). Recently, much attention has been devoted to the role of proprioception as a contributing factor to functional stability of the knee joint5).
ACL injury is one of the most common severe sport-related knee injuries. The majority of ACL injuries occur with a noncontact mechanism. The rate for noncontact ACL injuries ranges from 70 to 84% of all ACL tears in both female and male athletes6,7,8). Noncontact ACL injuries frequently occur in the weight-bearing (WB) phase. Loading of the ACL may occur in multiple planes, as anterior tibial translation, knee valgus, and lower extremity rotational motions all increase the amount of load on the ACL9,10,11,12,13). The relative orientation of the thigh to the shank is thought to be a factor contributing to ACL rupture. Knee joint valgus is often implicated as a hazardous position for the ACL and has recently been linked to ACL injury risk14,15,16,17). Current research suggests that a combined loading pattern is most detrimental with respect to ACL injury. Movement patterns that appear to increase ACL injury risk include a valgus and extension moments, especially during slight knee flexion (dynamic knee valgus)6).
In recent years, interest in assessment, prevention, and treatment of proprioceptive deficits has been increased. In addition, increasing numbers of authors have recommended that future examinations are necessary to more fully characterize the differential proprioceptive acuity in the constrained planes of movement (both frontal and transverse planes) compared with the primary plane of movement at the knee, and a test of proprioception is needed that involves movements similar to the mechanism of injury18, 19).
Most studies have tested knee proprioception in the sagittal plane and non-weight-bearing (NWB) position. As it has been revealed that the ACL is not only the primary restraint of posteroanterior motion of the tibia on the femur, but it also controls and induces valgus/rotation movement during WB activities, the limb alignment during high-risk WB activities may be more relevant in assessment of proprioception. To the authors’ best knowledge, no study has measured proprioception in a manner relevant to the mechanism of injury. Therefore, the aim of this study was to measure knee JPS in the noncontact ACL injury risk position and normal WB condition in healthy subjects.
SUBJECTS AND METHODS
Thirty healthy male volunteer athletes (age, 24.19 ± 5.27 years; height, 177.9 ± 7.7 cm; weight, 78.03 ± 11.7 kg) participated in the study. The study’s exclusion criteria for subjects included: 1) clinical signs of an impairment or abnormality in the knee (such as abnormal range of motion, muscle weakness, or malalignment), 2) injury to the knee that required medical attention, 3) previous surgery on the knee, or 4) current pain in the knee. All of the subjects were familiarized with the procedure by explanation, demonstration, and one practice repetition. The subjects wore loose-fitting shorts. The dominant knees of the subjects (defined as the leg used for kicking) were tested. All the subjects signed an informed consent form, and the study was approved by the Tehran University of Medical Sciences.
Biometrics’ “SG” series twin axis electrogoniometer (Biometrics Ltd, UK) was used to measure JPS. Participants were asked to wear shorts for ease of attachment of the electrogoniometer to the lateral side of the knee joint. The electrogoniometer was attached to the knee joint in the neutral knee position, which was defined based on the relationship between the thigh and the leg in the anatomical position20). The telescopic block was placed in parallel to an imaginary line between the head of the fibula and the lateral malleolus. The fixed end block was placed in parallel to an imaginary line between the greater trochanter and the lateral condyle of the femur. The electrogoniometer was zeroed when the subject was standing motionless in the anatomic position, and this was confirmed with a hand held goniometer. To prevent slippage during knee joint motion, the end blocks were adhered to the test leg with double-sided adhesive tape and further secured in place with adhesive tape. Electrogoniometer readings recorded knee joint angular displacements relative to zero. The test procedure included active reproduction of the angles in the ACL injury risk position and normal WB condition. The ACL injury risk position was executed in a standing position, with the feet slightly wider than shoulder-width apart and the toes pointed slightly outward (knee in and toe out; Fig. 1). The normal position was executed in a standing position, with the feet shoulder-width apart (Fig. 2)21, 22).
Fig. 1.
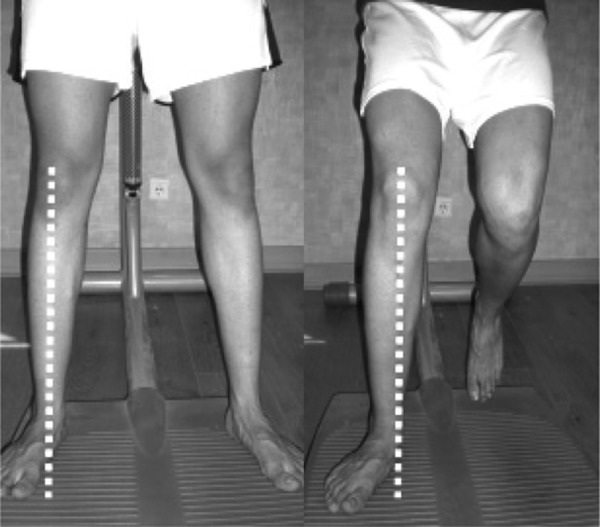
Risk position The ACL injury risk position was executed in a standing position, with the feet slightly wider than shoulder-width apart and the toes pointed slightly (knee in and toe out).
Fig. 2.

Normal position The Normal position was executed in a standing position, with the feet shoulder-width apart.
The foot of the untested limb was lifted from the floor. The knee was straight in the starting position (0 degrees). The subject stood with eyes closed, and was instructed to 1) lift the unexamined foot from the floor; 2) slowly flex the WB limb until told to stop (30 degrees), 3) identify (sense) the knee position while isometrically holding the test position for approximately 5 seconds, 4) return to the erect bilateral WB stance (for 7 seconds), and 5) reproduce the previous unilateral flexed position while concentrating on the knee. The holding times used in this study were the same as those used in previous studies23,24,25).
The test and replicated angles were measured using the electrogoniometer. Measurement of knee JPS was repeated three times, and the average was taken for the limb. By subtracting the test angle (TA) from the reproduced angle (RA), the absolute angular error (AAE) was calculated as a dependent variable25). This variable represented the accuracy of the replication.
All the collected data were analyzed using the Statistical Package for the Social Sciences (SPSS) (V.17). The Kolmogorov–Smirnov test was used for determination of the normal distribution of the data. The paired samples t-test was used for comparison within the ACL injury risk and normal positions. The test-retest reliability was measured using the two-way random effects model of intraclass correlation coefficient (ICC2,1) with the 95% confidence interval (95% CI). An ICC equal or greater than 0.70 is considered acceptable for test-retest reliability26, 27). Significance was set at p<0.05.
RESULTS
The Kolmogorov–Smirnov test showed that there was a normal distribution for the AEs in the two positions. Reliability values obtained for the risk and normal positions are shown in Table 1. JPS measurements demonstrated moderately high reliability for the risk position (with ICC = 0.74) and high reliability for the normal position (ICC = 0.88), according to the classifications of Feinstein28). Mean (SD) values of the AEs for the ACL injury risk and normal positions are presented in Table 2. A significant difference was found between the ACL injury risk and normal positions (p<0.001).
Table 1. Reliability statistics for the normal and risk positions.
| Measures | Mean (degrees) for test session (SD) |
Mean (degrees) for retest session (SD) |
ICC (95%CI) |
|---|---|---|---|
| RP | 3.80 (0.98) | 3.56 (0.88) | 0.74 |
| NP | 1.87 (0.94) | 1.83 (0.95) | 0.88 |
SD: standard deviation, ICC: intraclass correlation coefficient, RP: risk position, NP: normal position
Table 2. Mean (SD) values of AE for the ACL injury risk and normal positions.
| Testing Condition |
AAE (degrees), mean (SD) |
|---|---|
| RP | 3.99 (1.15)* |
| NP | 1.80 (0.83) |
AAE: absolute angular error, RP: risk position, NP: normal position. *: Statistically significant
DISCUSSION
Proprioception contributes to the development of motor control and plays a major role in the reflex protection of joints against potentially harmful forces1). It is important in the prevention of injuries, as reduced proprioception is one of the factors contributing to injury in the knee, particularly injury of the ACL. Although there are multiple risk factors associated with noncontact ACL injuries, poor proprioception is one of the key causative factors29,30,31). Therefore, proprioception appears not only important for regaining full function after ACL reconstruction but also for the prevention of ACL injuries.
Recently, it has been recommended that knee proprioception in high-risk positions should be examined. Thus, results of studies using NWB and normal WB positions may not correspond with those using high-risk positions. Assessment of JPS in WB risk positions potentially provides clinicians with more information on the status of the knee, thus giving a more precise picture for screening methods and prevention strategies. In the current study, JPS of the knee was compared between the noncontact ACL injury risk position and normal WB conditions in healthy subjects. The results showed less accurate knee JPS in the noncontact ACL injury risk position than in the normal WB condition.
Muaidi et al. examined knee proprioception in movements similar to the mechanism of injury during active internal and external rotations of the knee in healthy subjects. Their study reported that proprioceptive acuity of internal rotation was significantly lower than for external rotation19).
Several possible hypotheses for the different levels of JPS in the ACL injury risk and normal positions may be suggested. One hypothesis is that knee joint proprioception combines sensory input from a variety of afferent receptors in muscles, tendons, ligaments, and skin. The differential contributions of each of these structures could vary with joint position and direction/plane of loading18). Another possible reason for the difference in JPS between the ACL injury risk and normal positions may relate to altered proprioceptive input caused by incorrect functional alignment in the risk position. Therefore, the knee positions used during testing may have confounded our interpretation of the differential proprioceptive acuity across positions in the test. In conclusion, the poorer JPS in the noncontact ACL injury risk position compared with the normal WB condition identified in this study may contribute to the increased incidence of ACL injury. One of the most common mechanisms of noncontact ACL injury is dynamic knee valgus. It is possible that people with less accurate proprioception in the noncontact ACL injury risk position may be at greater risk of ACL injury. However, further prospective studies are required to confirm this hypothesis. From a clinical perspective, knee joint proprioception assessment in the high-risk position may have implications in understanding the development of knee sport pathologies, such as noncontact ACL injury and patellofemoral pain.
References
- 1.Riemann BL, Lephart SM: The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train, 2002, 37: 71–79 [PMC free article] [PubMed] [Google Scholar]
- 2.Grob KR, Kuster MS, Higgins SA, et al. : Lack of correlation between different measurements of proprioception in the knee. J Bone Joint Surg Br, 2002, 84: 614–618 [DOI] [PubMed] [Google Scholar]
- 3.Schultz RA, Miller DC, Kerr CS, et al. : Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am, 1984, 66: 1072–1076 [PubMed] [Google Scholar]
- 4.Schutte MJ, Dabezies EJ, Zimny ML, et al. : Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am, 1987, 69: 243–247 [PubMed] [Google Scholar]
- 5.Riemann BL, Lephart SM: The sensorimotor system. Part II: The role of proprioception in motor control and functional joint stability. J Athl Train, 2002, 37: 80–84 [PMC free article] [PubMed] [Google Scholar]
- 6.Griffin LY, Albohm MJ, Arendt EA, et al. : Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med, 2006, 34: 1512–1532 [DOI] [PubMed] [Google Scholar]
- 7.Boden BP, Dean GS, Feagin JA, Jr, et al. : Mechanisms of anterior cruciate ligament injury. Orthopedics, 2000, 23: 573–578 [DOI] [PubMed] [Google Scholar]
- 8.Faunø P, Wulff Jakobsen B: Mechanism of anterior cruciate ligament injuries in soccer. Int J Sports Med, 2006, 27: 75–79 [DOI] [PubMed] [Google Scholar]
- 9.Markolf KL, Gorek JF, Kabo JM, et al. : Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am, 1990, 72: 557–567 [PubMed] [Google Scholar]
- 10.Renström P, Arms SW, Stanwyck TS, et al. : Strain within the anterior cruciate ligament during hamstring and quadriceps activity. Am J Sports Med, 1986, 14: 83–87 [DOI] [PubMed] [Google Scholar]
- 11.Bendjaballah MZ, Shirazi-Adl A, Zukor DJ: Finite element analysis of human knee joint in varus-valgus. Clin Biomech (Bristol, Avon), 1997, 12: 139–148 [DOI] [PubMed] [Google Scholar]
- 12.Markolf KL, Burchfield DM, Shapiro MM, et al. : Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res, 1995, 13: 930–935 [DOI] [PubMed] [Google Scholar]
- 13.Berns GS, Hull ML, Patterson HA: Strain in the anteromedial bundle of the anterior cruciate ligament under combination loading. J Orthop Res, 1992, 10: 167–176 [DOI] [PubMed] [Google Scholar]
- 14.Olsen OE, Myklebust G, Engebretsen L, et al. : Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med, 2004, 32: 1002–1012 [DOI] [PubMed] [Google Scholar]
- 15.McLean SG, Huang X, Su A, et al. : Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon), 2004, 19: 828–838 [DOI] [PubMed] [Google Scholar]
- 16.Ford KR, Myer GD, Toms HE, et al. : Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sports Exerc, 2005, 37: 124–129 [PubMed] [Google Scholar]
- 17.Withrow TJ, Huston LJ, Wojtys EM, et al. : The effect of an impulsive knee valgus moment on in vitro relative ACL strain during a simulated jump landing. Clin Biomech (Bristol, Avon), 2006, 21: 977–983 [DOI] [PubMed] [Google Scholar]
- 18.Cammarata ML, Dhaher YY: Proprioceptive acuity in the frontal and sagittal planes of the knee: a preliminary study. Eur J Appl Physiol, 2011, 111: 1313–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muaidi QI, Nicholson LL, Refshauge KM: Proprioceptive acuity in active rotation movements in healthy knees. Arch Phys Med Rehabil, 2008, 89: 371–376 [DOI] [PubMed] [Google Scholar]
- 20.Gerhardt JJ: Documentation of joint motion: international standard neutral-zero measuring S.F.T.R. recording and application of goniometers, inclinometers and calipers, 3rd ed. Portland: Isomed Inc., 1992 [Google Scholar]
- 21.Myer GD, Ford KR, Hewett TE: The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J Electromyogr Kinesiol, 2005, 15: 181–189 [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi H, Kanamura T, Koshida S, et al. : Mechanisms of the anterior cruciate ligament injury in sports activities: a twenty-year clinical research of 1,700 athletes. J Sports Sci Med, 2010, 9: 669–675 [PMC free article] [PubMed] [Google Scholar]
- 23.Marks R, Quinney HA, Wessel J: Proprioceptive sensibility in women with normal and osteoarthritic knee joints. Clin Rheumatol, 1993, 12: 170–175 [DOI] [PubMed] [Google Scholar]
- 24.Marks R: The reliability of knee position sense measurements in healthy women. Physiother Can, 1994, 46: 37–41 [Google Scholar]
- 25.Hopper DM, Creagh MJ, Formby PA, et al. : Functional measurement of knee joint position sense after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil, 2003, 84: 868–872 [DOI] [PubMed] [Google Scholar]
- 26.Terwee CB, Bot SD, de Boer MR, et al. : Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol, 2007, 60: 34–42 [DOI] [PubMed] [Google Scholar]
- 27.Atkinson G, Nevill AM: Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med, 1998, 26: 217–238 [DOI] [PubMed] [Google Scholar]
- 28.Feinstein AR: Clinimetrics. New Haven: Yale University Press, 1987 [Google Scholar]
- 29.Beynnon BD, Johnson RJ: Anterior cruciate ligament injury rehabilitation in athletes. Biomechanical considerations. Sports Med, 1996, 22: 54–64 [DOI] [PubMed] [Google Scholar]
- 30.Griffin LY, Agel J, Albohm MJ, et al. : Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg, 2000, 8: 141–150 [DOI] [PubMed] [Google Scholar]
- 31.Taimela S, Kujala UM, Osterman K: Intrinsic risk factors and athletic injuries. Sports Med, 1990, 9: 205–215 [DOI] [PubMed] [Google Scholar]


