Abstract
[Purpose] Patients with severe bilateral knee osteoarthritis (KOA) often suffer from low back pain (LBP). However, few studies have examined the relationship between LBP and KOA in downward reach and pick-up movements. [Subjects] Eight KOA patients with LBP (LBP group), 8 KOA patients without LBP (NLBP group), and 7 healthy participants (Control group), without osteoarthritis or low back pain, were recruited for this study. [Methods] All subjects were asked to pick up a bottle with one hand, placed at the diagonal on the opposite side of the body. A 3D motion analysis system was used to record trunk and lower limb movements. [Results] The knee flexion angle on the side ipsilateral to the bottle was significantly smaller in both KOA groups than in the controls in the downward reach and pick-up movements. KOA patients showed a significantly lower trunk flexion angle and greater pelvis anterior tilt angle than the controls. In addition, no significant differences were found between the LBP and NLBP group. [Conclusion] We suspect that severe knee pain due to OA determines the priority of movement in strategic planning for the execution of pick-up movements. The knee strategy was abandoned by our severe knee OA patients, even when they had mild LBP.
Key words: Knee osteoarthritis, Low back pain, Pick-up movement
INTRODUCTION
Stooping, crouching, or kneeling movements are an important component of many daily living movements, such as in reaching down to low shelves, picking up an object from the floor, or cleaning. Stooping, crouching, or kneeling difficulty is prevalent among knee osteoarthritis (OA) patients1) and it can significantly affect their daily lives. The most obvious clinical sign of knee OA is pain. To reduce pain, patients try to reduce the load on the painful knee joint2), or change the movement pattern, for example by reducing walking speed3, 4), shortening of stride length5), or reducing pelvic rotation during walking6). However, few studies have explored the reasons behind downward reaching and pick up difficulty. Accurate control of the center of mass (COM) is expected in the maintenance of balance during downward reaching and pick up movements. However, previous studies have shown increased knee forces when kneeling in high flexion and squatting7, 8). Therefore, knee joints affected by OA have a restricted range of movement. We hypothesized that reduced knee flexion angle would result in increased trunk flexion when performing reaching and pick-up movements. However, it is a clinical observation that patients with severe knee OA often suffer low back pain (LBP) and this pain is also directly associated with increases in pain, depression, and anxiety in OA patients. Past research has reported that back pain was present in 54.6% of patients with knee OA9). This has been linked to bone demineralization, muscle atrophy, inflexibility, and loss of functional ability following knee OA10). It is also reported that subjects with multiple joint problems involving either the knee or the back are 12 times more likely to have pain than those with problems in only one of those joints11). To the best of our knowledge, little research has as yet been conducted to analyze back pain interference in the knee function of OA knee patients. Therefore, this study quantified the effects of body configuration changes in the downward reaching and pick-up movements of OA knee patients with and without LBP.
SUBJECTS AND METHODS
Subjects
Eight severe bilateral knee OA patients with chronic nonspecific low back pain (LBP group), aged 69.00 (65.50/72.50) years, and 8 severe bilateral knee OA patients without LBP (NLBP group), aged 72.00 (64.00/74.50) years were recruited for this study. Subjects were diagnosed as having OA at Kaohsiung Medical Hospital. Radiographically detected OA of the knee according to the Kellgren and Lawrence classification method was grade 4 for all patients. Patients in the LBP group had a chief complaint of low back pain for a minimum of three months. In addition, 7 healthy participants aged 23.00 (20.00/24.00) years, without osteoarthritis, low back pain, or other musculoskeletal symptoms, were recruited as the control group. All the participants provided their written informed consent prior to their participation in this study, and all procedures were reviewed and approved by the Institutional Review Board for the Use of Human Subjects in Research of Kaohsiung Medical Hospital.
Methods
A 6-camera Qualisys 3D motion analysis system was used to record trunk and lower limb movements of the subjects at a sampling frequency of 100 Hz for 5 seconds. Three cameras were positioned in front of the subjects and three behind the subjects. Qualisys Track Manager 2.0.387 (Qualisys Motion Capture Systems, Qualisys AB, Sweden) and Visual3D 3.79.0 (C-Motion Inc., USA) software were used to analyze the motion data. In addition, Lequesne’s Index was used to evaluate the pain and functional disability of the patients with knee OA. This 10-question survey has five questions pertaining to pain or discomfort, one question deals with maximum total ranging from walking distance, and four questions are about the activities of daily living. The responses are scored to give a 0 to 24 scale. Lower scores indicate lower functional impairment. The Roland-Morris disability questionnaire (RDQ)12) was used to assess physical disability due to back pain as experienced by these knee OA patients. The RDQ comprises 24 yes/no items specifically related to physical functions which are scored to assess disability due to LBP. The physical functions considered include walking, bending over, sitting, lying down, dressing, sleeping, self-care and daily activities. In the RDQ, one point is given for each “yes” answer. The RDQ score is obtained by adding up the number of items checked. The final score ranges from 0 (no disability) to 24 (severe disability). In addition, the Oswestry low back pain disability index (ODI) was used in this study to measure individuals’ levels of back pain intensity. The ODI covers 1 item on pain and 9 items on activities of daily living. In this study, only the pain item was used in the analysis. This pain item is scored from 0–5, 0 meaning “no pain” and 5 meaning the “worst possible pain”.
All subjects were asked to pick up an empty plastic bottle (height = 30 cm) from the floor with one hand. The bottle was placed at the diagonal on the opposite side of the body, within the arm’s reach. Both hands were examined three times, respectively. A cycle of trunk flexion-extension constituted one trial. One cycle included a self-paced flexion to attain the deepest trunk flexion by touching and picking up the bottle, followed by a self-paced extension to the starting position. At the beginning of each trial, the participants were asked to stand with their feet shoulder-width apart and lower the torso while bending the knees. They were told to rotate and slowly lower their torso to the required angle using the bottle guides, and then slowly elevate and rotate their torso to the upright position. They did not need to maintain the required rotational angle at the deepest trunk flexion position, and did not have to maintain straight knees during trunk flexion. To become accustomed to the testing procedure, subjects performed three warm-up practices in each direction.
For kinematic analysis, a modified Helen-Hayes marker set was used with the addition of markers on the C7, T6, L1 and L3 of the spine. After the static posture recording, the markers on the medial side were removed for the testing procedure. For the purpose of describing the rotational kinematics of the trunk, pelvis, and knee, the other markers were used to reconstruct each body segment, the trunk, pelvis, thighs and legs.
Qualisys Track Manager software was used to track the markers in space. All marker data were low-pass filtered using a Butterworth filter with a cut-off frequency of 6 Hz, and interpolated with a maximum gap fill of 10 frames using a 3rd-order polynomial. The joint angles of the trunk were calculated relative to a pelvis coordinate system in flexion-extension, lateral bending, and rotation. Pelvis anterior tilt and trunk inclination angles were calculated relative to a global coordinate system to determine the pelvis and trunk anterior/posterior tilt angles. These angles at final downward pick-up movement were averaged over both directions of movement. However, the knee flexion angles of the sides ipsilateral and contralateral to the bottle were separately observed during asymmetric trunk flexion motion.
The statistical significance of the differences in joint angles was calculated using the Kruskal-Wallis H test for independent measures of each group. The Mann-Whitney test was further used to determine the significance of differences in the angles fbetween pairs of groups, and the differences in the Lequesne’s Index and RDQ scores between the LBP and NLBP groups. All analyses were carried out using the SPSS 19.0 program. The results were considered statistically significant when the p-value was less than 0.05.
RESULTS
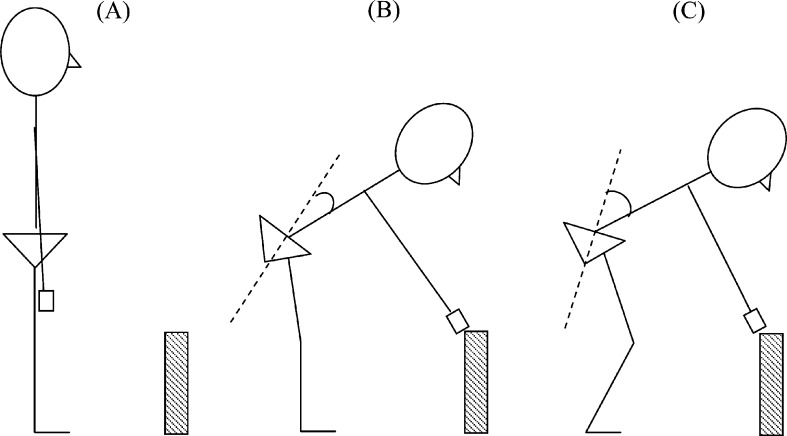
The baseline characteristics of the three groups are shown in Table 1. The RDQ and ODI pain scores were highest in the LBP group. There was no statistically significant difference in the Lequesne’s index scores between the LBP and NLBP groups. The descriptive statistics and statistical significance of the knee, trunk and pelvis movement data are presented in Table 2 and the movement is illustrated in Fig. 1. Knee flexion angles were smaller in both the LBP and NLBP groups than that of the controls on the side ipsilateral to the bottle. The OA patients in the LBP and NLBP groups showed significantly smaller trunk flexion angles than that of the control, and the rotation angle of the NLBP group was smaller than that of the controls. A significantly greater pelvis anterior tilt angle was found in the OA patients of both the LBP and NLBP groups. No significant differences were found among the seen for trunk anterior tilt angles.
Table 1. Baseline characteristics of the knee OA patients (LBP group and NLBP group) and the control group (median and interquartile range in parentheses).
| LBP group | NLBP group | Control group | |
|---|---|---|---|
| Case No. (Male/Female) | 8 (2/6) | 8 (1/7) | 7 (4/3) |
| Age (years) | 69.0 (65.5/72.5) | 72.0 (64.0/74.5) | 23.0 (20.0/24.0) |
| Height (cm) | 156.3 (147.8/162.2) | 151.2 (142.3/154.1) | 170.0 (167.0/174.0) |
| Weight (kg) | 65.2 (58.6/79.0) | 56.7 (52.3/63.4) | 66.0 (58.0/70.0) |
| Lequesne’s index | 11.0 (9.3/15.0) | 13.0 (10.0/14.0) | N/A |
| RDQ | 9.0 (7.3/10.8)* | 3.5 (2.0/5.8) | N/A |
| ODI (pain score) | 1.0 (1.0/2.0)* | 0.5 (0.0/1.0) | N/A |
* denotes a significant difference from the control group, p value < 0.05
Table 2. Descriptive statistics and statistical significances of the knee, trunk and pelvis movements at the end of the downward pick-up movement (median and interquartile range in parentheses).
| LBP | NLBP | Control | |
|---|---|---|---|
| Knee flexion angle (°) Contralateral | −9.11 (−12.16/−5.75) | −8.99 (−22.17/−5.75) | −15.45 (−40.39/−4.96) |
| Ipsilateral | −7.54 (−12.31/−3.78)* | −6.39 (−12.95/−4.05)* | −19.89 (−31.63/−6.50) |
| Trunk flexion (°) | −27.65 (−33.07/−20.10)* | −27.44 (−32.83/−24.30)* | −40.43 (−46.46/−36.44 ) |
| Trunk lateral bending (°) | 7.46 (4.95/10.20) | 7.96 (5.59/15.08) | 8.01 (4.41/9.76) |
| Trunk rotation (°) | 6.79 (5.12/9.12) | 6.01 (3.89/8.23)* | 9.15 (6.57/10.25) |
| Pelvis anterior tilt (°) | −44.68 (−50.18/−40.52) * | −45.83 (−48.56/−39.38) * | −32.61 (−37.05/−28.47) |
| Trunk anterior tilt (°) | −82.13 (−89.33/−73.23) | −83.96 (−88.80/−74.07) | −85.05 (−85.96/81.92) |
* denotes a significant difference from the control group, p < 0.05
Fig. 1.
Illustration of the trunk movement in the sagittal plane at the end of the downward pick-up movement. (A) starting position; (B) knee OA patient; and (C) control subject. The knee OA patients showed significantly smaller trunk flexion angles and greater pelvis anterior tilt angles than the controls.
DISCUSSION
In both the LBP and NLBP groups, the knee OA patients showed significantly smaller knee flexion angles in the limb ipsilateral to the bottle than that of the controls when doing the downward pick-up movement. The downward pick-up movement designed for this study included flexion, extension, and rotation of the trunk and knee joints. To avoid pain in or around the knee and to complete this task smoothly, the knee OA patients reduced the flexion of the knee joint and tilted the pelvis more to move the center of body weight backward to balance the trunk. However, it is common knowledge that one should bend the knees when lifting heavy objects because this makes full use of the strongest set of leg muscles, and this shifts most of the heavy load onto the hips and thighs, instead of directly loading the low back. Therefore, it is likely that knee OA patients are highly vulnerable to low back injuries if they use the strategy observed in this study to lift a heavy object.
In the present study, the knee OA patients showed smaller trunk flexion angles than the control subjects. The OA patients also displayed greater pelvic anterior tilt than the control subjects. Overall, this had no influence on the anterior trunk inclination angle. This confounds our hypothesis that reducing knee flexion angle would result in increased trunk flexion when performing reaching and pick-up movements. Instead, in clinical observation, we found the subjects in the control group could pick-up the bottle at a greater distance away from the body by increasing the forward lean of the trunk. Therefore, there was no significant difference in anterior trunk inclination angle between the knee OA patients and the controls. Figure 1 provides an illustration of how the trunk movement in the sagittal plane at the final downward pick-up movement was performed by the knee OA patients and control subjects.
No significant differences were found between the LBP and NLBP group. We suspect this is because: the empty bottle was not heavy enough to change the trunk movement patterns of the knee OA patients with LBP; our LBP patients had a mean RDQ score of 9.00 which was not severe enough to affect trunk movement; and severe knee pain due to OA determined the priority of movement in the strategic planning of the execution of pick-up movements. The knee strategy was abandoned by our severe knee OA patients, even when they had mild LBP, and the pain reported by most of our LBP patients (median ODI pain score of 1) was very mild. Future research should examine the effects of a heavy-load pick-up movement and also investigate its effect on patients with more severe LBP and higher levels of disability.
Acknowledgments
The author gratefully acknowledges the grant support from the National Science Council, Taiwan (NSC 99-2314-B037-004).
REFERENCES
- 1.Gelber AC, Hochberg MC, Mead LA, et al. : Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med, 2000, 133: 321–328 [DOI] [PubMed] [Google Scholar]
- 2.Hurwitz DE, Ryals AR, Block JA, et al. : Knee pain and joint loading in subjects with osteoarthritis of the knee. J Orthop Res, 2000, 18: 572–579 [DOI] [PubMed] [Google Scholar]
- 3.Messier SP, DeVita P, Cowan RE, et al. : Do older adults with knee osteoarthritis place greater loads on the knee during gait? A preliminary study. Arch Phys Med Rehabil, 2005, 86: 703–709 [DOI] [PubMed] [Google Scholar]
- 4.Mündermann A, Dyrby CO, Hurwitz DE, et al. : Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis Rheum, 2004, 50: 1172–1178 [DOI] [PubMed] [Google Scholar]
- 5.McGibbon CA, Krebs DE: Compensatory gait mechanics in patients with unilateral knee arthritis. J Rheumatol, 2002, 29: 2410–2419 [PubMed] [Google Scholar]
- 6.Tanaka K, Miyashita K, Urabe Y, et al. : Relationship between pelvic rotation and trunk lean motion during walking in patients with symptomatic knee osteoarthritis. J Biomech, 2007, 40: S508 [DOI] [PubMed] [Google Scholar]
- 7.Nagura T, Dyrby CO, Alexander EJ, et al. : Mechanical loads at the knee joint during deep flexion. J Orthop Res, 2002, 20: 881–886 [DOI] [PubMed] [Google Scholar]
- 8.Komistek RD, Kane TR, Mahfouz M, et al. : Knee mechanics: a review of past and present techniques to determine in vivo loads. J Biomech, 2005, 38: 215–228 [DOI] [PubMed] [Google Scholar]
- 9.Wolfe F, Hawley DJ, Peloso PM, et al. : Back pain in osteoarthritis of the knee. Arthritis Care Res, 1996, 9: 376–383 [DOI] [PubMed] [Google Scholar]
- 10.Goerres GW, Häuselmann HJ, Seifert B, et al. : Patients with knee osteoarthritis have lower total hip bone mineral density in the symptomatic leg than in the contralateral hip. J Clin Densitom, 2005, 8: 484–487 [DOI] [PubMed] [Google Scholar]
- 11.Keenan AM, Tennant A, Fear J, et al. : Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Rheum, 2006, 55: 757–764 [DOI] [PubMed] [Google Scholar]
- 12.Stratford PW, Binkley JM, Riddle DL, et al. : Sensitivity to change of the Roland-Morris Back Pain Questionnaire: part 1. Phys Ther, 1998, 78: 1186–1196 [DOI] [PubMed] [Google Scholar]