Abstract
Penicillin allergy remains the most common drug allergy, with a reported prevalence of 10% in the United States. Epidemiology of penicillin allergy in outpatient populations is relatively scarce. This study sought to determine the prevalence and characteristics of reported penicillin allergy in an urban outpatient population and to identify trends in clinical evaluation and management from a tertiary center serving a large inner-city population. A retrospective review of electronic medical records was performed of adult patients seen in the Internal Medicine Associates Clinic of Mount Sinai Hospital between January 31, 2012, and July 31, 2012. Medical records were selected based on the documentation of penicillin in patient's allergy section. Of the 11,761 patients seen in the clinic, 1348 patients (11.5%) reported a history of penicillin allergy. The most common allergic reactions were rash (37%), unknown/undocumented (20.2%), hives (18.9%), swelling/angioedema (11.8%), and anaphylaxis (6.8%). There was an increased prevalence of penicillin allergy in female patients compared with male patients (odds ratio [OR] = 1.82; 95% CI = 1.60, 2.08; p < 0.0001), and there were significantly fewer Asians with penicillin allergy compared with Caucasians (OR = 0.51; 95% CI = 0.32, 0.83; p = 0.007). However, only 78 (6%) of the patients reporting penicillin allergy had a referral to an allergy specialist. Overall, improved referral to an allergist will help to identify patients who have penicillin allergy requiring avoidance.
Keywords: Adverse drug reactions, anaphylaxis, drug allergy, electronic medical record, epidemiology, outpatient, penicillin
Penicillin allergy remains the most common drug allergy reported, with a prevalence of ∼8–12% depending on the specific population evaluated.1–3 Higher rates are noted in individuals receiving more health care, including female patients and with increasing age.2,3 Symptoms associated with reported penicillin allergy classically include rash and/or itching, nausea, vomiting, shortness of breath, and anaphylaxis. However, often reported symptoms are either classified as unknown or representative of non–IgE-mediated reactions, such as nonurticarial rashes resulting from underlying viral illnesses.4 The Choosing Wisely campaign recommends appropriate evaluation of patients with a history of penicillin allergy rather than avoidance or use of alternative antibiotics that can increase medical costs, patient morbidity, and potentially contribute to further antibiotic resistance.5,6 After a complete evaluation, up to 90% of individuals with a history of penicillin allergy are able to tolerate penicillins.1 Despite these favorable statistics, drug allergies are very rarely confirmed or removed from the medical record, and penicillin allergy is overdiagnosed with the antibiotic class avoided as part of a “safe rather than sorry” approach.2,4,7
It is therefore important to study the epidemiology of penicillin allergy, because it may help practitioners better identify the patients at risk for true drug allergy. Relatively few studies have examined the characteristics of penicillin allergy in various patient populations. A 20-year retrospective study published by Ponvert et al. is the largest to report on β-lactam allergy in children. They showed that a history of severe skin symptoms such as acute generalized Stevens–Johnson Syndrome (SJS), serum sickness-like reactions, and anaphylaxis were risk factors for β-lactam allergy, although age, gender, and a history of atopy were not contributing factors.8 In contrast, the largest retrospective study of both children and adults with self-reported antibiotic allergy by Macy et al. found that female gender and older age were associated with a higher rate of self-reported allergy, albeit without confirmation by skin and challenge testing.2 Despite these reports, there are still few published data on the epidemiology of penicillin allergy in the outpatient population of the United States.2
Beyond epidemiology, it is also important to study the management of penicillin allergy given the drug's efficacy and cost-effectiveness, particularly in diseases such as group A streptococcal pharyngitis and syphilis.9 The Joint Task Force on Practice Parameters has stated that the “evaluation of patients with penicillin allergy by skin testing leads to reduction in the use of broad-spectrum antibiotics and may decrease costs.”1 Current evaluation includes skin-prick testing, intradermal testing, in vitro testing for IgE, and oral drug challenge, all of which should be precluded by a thorough history to help determine the likelihood of true clinical allergy. In terms of the reliability of testing for penicillin allergy, studies have shown a large discrepancy in specificity and sensitivity for in vitro detection of penicillin-specific IgE.10,11 One such study showed that the specificity of fluorenzymeimmunoassay (CAP-FEIA; Phadia, Uppsala, Sweden) for penicillin ranged from 83.3 to 100% and sensitivity ranged from 0 to 25%.10 Another prospective study showed that commercially available anti–penicillin IgE fluorenzymeimmunoassays were not useful in diagnosing penicillin allergy in patients with remote histories of penicillin allergy.12 With data supporting such low sensitivity, immediate hypersensitivity skin testing is considered the most useful test for detecting IgE-mediated reactions to penicillin. A recent consensus document supports that skin-prick testing is advised as an initial screen in patients with a history of immediate reaction to penicillin, because it is simple, rapid, cost-effective, and highly specific.13 Studies show that skin testing with both penicilloyl-poly-lysine (major determinant) and penicillin G (minor determinant) can identify up to ∼95% of patients with positive reactions, and 98% of patients with a negative result will tolerate penicillin without any serious reaction.14 Additional studies indicate that penicillin skin testing using only penicilloyl-poly-lysine and penicillin, followed by an oral amoxicillin challenge, is a safe way to determine clinically significant IgE-mediated penicillin allergy.15 However, despite the availability and endorsement of various clinical tests, there are many patients who continue to carry a diagnosis of penicillin allergy as a result of poor testing use and application.
In this study we sought to determine the prevalence and characteristics of reported penicillin allergy in a general internal medicine practice serving an urban population in New York City. We further aimed to identify trends in clinical evaluation and management to establish more concise recommendations toward improvement in the clinical care of patients with a history of penicillin allergy.
METHODS
Study Design
A retrospective review of electronic medical records (Epic; Epic Systems Corp., Verona, WI) was performed of adult patients seen in the Internal Medicine Associates Clinic of Mount Sinai Hospital, New York, NY, between January 31, 2012, and July 31, 2012. This clinic serves an urban population of East Harlem, NY. We queried electronic medical records for patients with any of the following listed in the allergy section at the time of chart review (October 2012): penicillin, penicillin G, penicillin G benzathine, penicillin G potassium, penicillin G procaine, penicillin G sodium, penicillin V, and penicillin V potassium. Demographics, clinical history, and details of penicillin reaction were collected from the medical record and analyzed. This study was approved by the Institutional Review Board of Mount Sinai Hospital with a waiver of consent.
Demographic Information and Study Variables
The following data were recorded for each subject: age at the time of chart review, race, gender, documented symptoms of allergic reaction to penicillin, referral to allergy, the presence of additional atopic conditions including asthma and allergic rhinitis, and the coexistence of a diagnosis best treated with penicillin including syphilis (ICD9 090.* to 097.*), group A Streptococcus infection (ICD9 041.01), or streptococcal sore throat (ICD9 034.0).
A more detailed review of the medical record was performed for patients with a documented history of anaphylaxis to penicillin by reviewing the entire medical record, including progress notes. The information recorded included details of anaphylaxis history, documenting physician, additional antibiotic allergy, and historical antibiotics prescribed.
Statistical Analysis
Statistical analysis was performed using GraphPad (GraphPad Software, La Jolla, CA). Categorical variables were summarized using frequencies and percentages. Age across groups was compared with one-way ANOVA (Kruskal-Wallis test), and gender and race across groups was compared with a chi-square test. Odds ratios (ORs) and CIs of 95% were calculated where applicable. All tests were performed using a level of significance of p <0.05.
RESULTS
Eleven thousand seven hundred sixty-one patients were seen in the Internal Medicine Associates Clinic from January 31, 2012, to July 31, 2012, of which 1348 (11.5%) met study criteria of documented penicillin allergy. Characteristics of patients without a penicillin allergy, patients with a reported nonanaphylactic penicillin allergy, and patients with reported penicillin anaphylaxis are presented in Table 1. There was an increased prevalence of penicillin allergy (of any type) in female patients (OR = 1.82; 95% CI = 1.60, 2.08; p < 0.0001) compared with male patients. The most common race with penicillin allergy was African American (although this was the most common documented race among all clinic patients), and there were significantly fewer Asians with penicillin allergy compared with Caucasians (OR = 0.51; 95% CI = 0.32, 0.83; p = 0.007; Table 2).
Table 1.
Patient characteristics
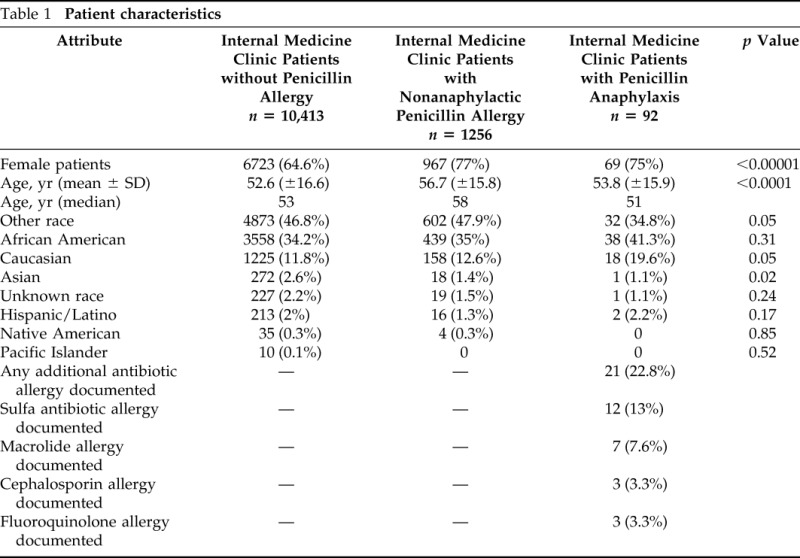
Table 2.
Likelihood of reported penicillin allergy based on race
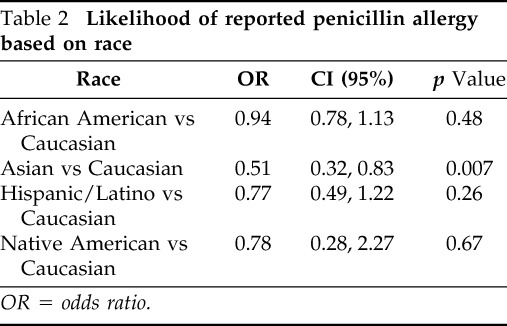
OR = odds ratio.
Among all patients with penicillin allergy, the most common documented reactions included rash (37%), hives (18.9%), and swelling/angioedema (11.8%; Table 3); 6.8% (n = 92) of patients had documented anaphylaxis. For patients with a history of penicillin anaphylaxis, the vast majority (92.4%) had no documentation of the details of the reaction, including age of anaphylaxis; 20.2% of patients were documented as having an “unknown” or an “undocumented” reaction. Seventy-eight (6%) of the 1348 penicillin-allergic patients had a documented referral to an allergy specialist, of which 56 (72%) were evaluated in our allergy clinic.
Table 3.
Historical reactions associated with reported penicillin allergy
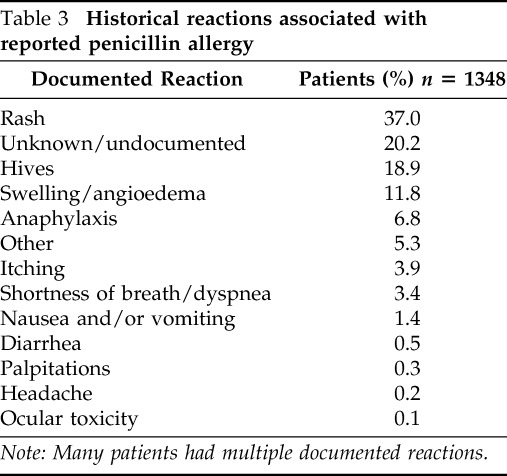
Note: Many patients had multiple documented reactions.
In terms of comorbidities, slightly less than one-third of the patients with penicillin allergy had asthma (30.6%) or allergic rhinitis (27.5%). Five patients had documentation of streptococcal pharyngitis and five other patients had syphilis; all of the patients with either pharyngitis or syphilis who received treatment were prescribed azithromycin. Regarding additional drug allergy in populations with reported penicillin allergy, 21 patients also had reported cephalosporin allergy, 3 of whom had a history of penicillin anaphylaxis. The cephalosporin-allergic patients otherwise had documentation of hives and/or rash (n = 11), swelling (n = 2), or unknown reaction (n = 5) with penicillin.
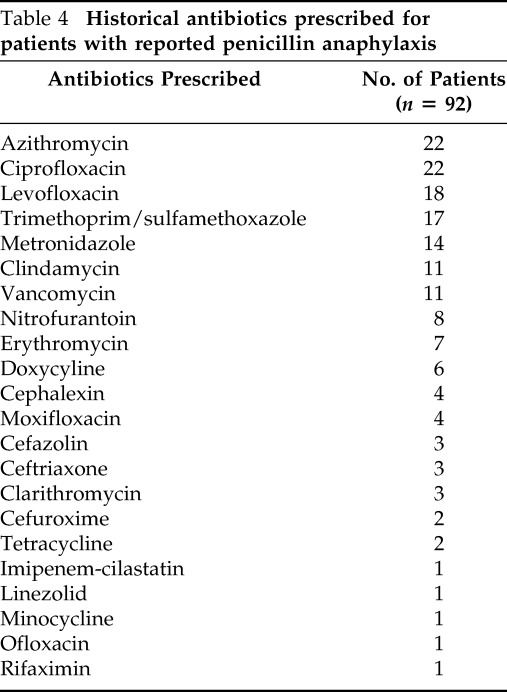
Subgroup analysis of patients with reported anaphylaxis was performed (n = 92). Primary care physicians were the most frequent providers to document penicillin anaphylaxis (42.4%), followed by physicians transcribing documentation from paper to electronic records through chart abstraction (23.9%) and physicians documenting in the emergency room (18.5%). Physicians in allergy, cardiology, endocrinology, geriatrics, gynecology, hepatology, nephrology, pain management, and pulmonary subspecialties each accounted for <3% of the providers documenting penicillin anaphylaxis; 22.8% of this patient subgroup had additional antibiotic allergies documented, of which sulfa-based antibiotics and macrolides were the most common (Table 1). Interestingly, although there were 3 patients labeled as cephalosporin allergic within the penicillin anaphylaxis subgroup, 11 of the patients had documentation of receiving a cephalosporin without clinical reaction. Of these 11 patients, 9 were prescribed the cephalosporin after the chart documentation of penicillin allergy. A full listing of antibiotics prescribed to patients with documented penicillin anaphylaxis is provided in Table 4.
Table 4.
Historical antibiotics prescribed for patients with reported penicillin anaphylaxis
DISCUSSION
In this study, we found a significant increase in documented penicillin allergy in female patients versus male patients, a finding that has been borne out in multiple studies looking at gender differences in the reporting of adverse drug reactions.3,16 Because this study did not prospectively test for penicillin allergy in the identified study patients, it remains unclear whether this difference is because of reporting bias or actual biological/pharmacokinetic factors. We also found that Asian race may be protective in penicillin allergy when compared with Caucasian race, and, to our knowledge, this is the first time such a racially protective finding has been reported. Although this study did not examine allergy trends in age in the selected population, other studies have shown that increasing age may be a risk factor for penicillin allergy.2
Another important finding to come from this study relates to the technical documentation of allergic reaction. Close to one-half of all anaphylactic penicillin allergies were recorded by primary care physicians, and we presume that many of the overall penicillin allergies were also recorded by primary care physicians. A meaningful number (20.2%) of general reaction histories were recorded as “unknown” or “undocumented.” Although this description may represent a segment of patients who could not provide an accurate history of penicillin reaction, it may also represent a segment of patients who were not formally asked about the details of penicillin reaction.
Additionally, none of the recorded histories distinguished between an immediate and delayed reaction. For all physicians, including primary care physicians, the documentation of a drug allergy should include (at a minimum) the nature and timing of the reaction, because this can be used to determine a pretest likelihood for true drug allergy.17 This is particularly true when it comes to the documentation of rash, the most commonly reported reaction in our patient group. In a publication by Scherer and Bircher, they highlight the importance of documenting exact morphology, distribution, and speed of evolution of skin symptoms in a suspected drug hypersensitivity reaction. They report that “danger signs” for immediate-type reactions include extensive pruritus (particularly on palmoplantar and scalp surfaces) as well as a flush on the face and neck with conjunctivitis and rhinitis, and that “danger signs” for delayed-type reactions include erythroderma, pain, purpura, hemorrhage, necrosis, and erosive stomatitis.18 There is significant difference in the testing and management of a patient who has skin symptoms consistent with a mild maculopapular eruption versus SJS or toxic epidermal necrolysis, and none of our patients had such detailed descriptors. Similarly, the vast majority (92.4%) of patients with reported anaphylaxis to penicillin did not have details of the anaphylactic reaction. Current practice recommends avoidance of testing and challenge to penicillin in those patients with a history of SJS/ toxic epidermal necrolysis. Patients with a history of anaphylaxis should be evaluated by skin testing before any challenge in a monitored setting. Therefore, it is essential to clarify and obtain a complete history to determine whether a patient's reaction meets the criteria for these diagnoses. In the era of electronic medical records, efforts should be made toward improved documentation of drug allergy to aid in a multidisciplinary understanding of accurate patient drug histories.
As for the question of cephalosporin use in penicillin-allergic patients, relatively few patients (1.6%) with documented penicillin allergy also had documented cephalosporin allergy. This supports practice guidelines that most patients with a history of penicillin allergy can tolerate cephalosporins, and when severe reactions are excluded, the rate of reactions after giving a cephalosporin (without skin testing) to a patient with a history of penicillin allergy is ∼0.1%.1 Within the group of patients with reported penicillin anaphylaxis, 11 were uneventfully prescribed cephalosporins including cephalexin, cefazolin, cefuroxime, and ceftriaxone. These were prescribed for various infections including cellulitis, pneumonia, and bacteremia as well as prophylaxis for spinal intervention, valve replacement, and intestinal surgery. It is interesting that the first-generation cephalexin was prescribed more than the second- and third-generation cephalosporins, given that the original study quoting 10% cross-reactivity between penicillins and cephalosporins was referencing first-generation cephalosporins.19
Finally, our study reveals low numbers of referral to allergy for penicillin reactions. With such low referral numbers, there likely is a role for educating primary care physicians on the availability of standard methods for evaluating penicillin allergy, as well as the important role they can play in promoting successful antimicrobial stewardship through working up penicillin allergy. Allergy evaluation should also be stressed as an economical decision; a recent study in the setting of selected inpatient wards estimated that the avoidance of β-lactam antibiotics on only 55 occasions incurred an additional cost of $15,672 (Canadian dollars).20 Overall, penicillin testing and challenge is a well-tolerated, effective service that should be offered in an elective manner before patients are in a critical condition requiring specific antibiotic regimens.
The limitations of this study include that it is a retrospective chart review without prospective confirmation of penicillin allergy through standardized testing. The patients identified as penicillin allergic were largely through self-report, although the histories were filtered through health-care professionals during the process of labeling the electronic medical record. We may have missed some patients with penicillin allergy, because we looked only for patients with listed allergies to penicillin, penicillin G, and penicillin V. However, our assumption is that most providers entered the allergy as “penicillin” to cover the entire family of medications. Additionally, our chart review could be missing patients who had a diagnosis of penicillin allergy that was cleared by the allergy service and therefore removed from the electronic medical record. In this case, the referrals to and workups by the allergy service may be higher than reported.
In summary, this study adds to the relatively small repository of information on patients with penicillin allergy in the outpatient population. We note significantly higher penicillin allergy prevalence in female patients, and we identify that Asian race may be protective against penicillin allergy. Many patients had vague or distant histories of penicillin reaction, most commonly rash, and the majority of such patients may tolerate penicillin after allergy evaluation. It is therefore justifiable from the perspective of health-care costs, as well as the benefit to the individual patient, that an increased focus be placed on clarifying penicillin allergy in the outpatient setting. Improved documentation of penicillin allergy is called for by all practitioners, and patients should be referred to allergists for well-established and validated methods of penicillin allergy evaluation.
Footnotes
Presented at the 2013 American Academy of Allergy, Asthma, and Immunology Conference, February 2013, San Antonio, Texas
Funded by The Institutes for Translational Sciences at Mount Sinai School of Medicine and by Grant UL1TR000067 from the National Center for Advancing Translational Sciences, National Institutes of Health
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: An updated practice parameter. Ann Allergy Asthma Immunol 105:259–273, 2010.20934625 [Google Scholar]
- 2. Macy E, Poon K-Y T. Self-reported antibiotic allergy incidence and prevalence: Age and sex effects. Am J Med 122:778.e1–7, 2009. [DOI] [PubMed] [Google Scholar]
- 3. Macy E, Ho NJ. Multiple drug intolerance syndrome: Prevalence, clinical characteristics, and management. Ann Allergy Asthma Immunol 108:88–93, 2012. [DOI] [PubMed] [Google Scholar]
- 4. Caubet JC, Kaiser L, Lema∧itre B, et al. The role of penicillin in benign skin rashes in childhood: A prospective study based on drug rechallenge. J Allergy Clin Immunol 127:218–222, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. ABIM Foundation. Choosing wisely. American Academy of Allergy, Asthma and Immunology: 10 Things physicians and patients should question. Available online at www.choosingwisely.org/doctor-patient-lists/american-academy-of-allergy-asthma-immunology/; accessed May 21, 2014.
- 6. Macy E, Contreras R. Health care use and serious infection prevalence associated with penicillin “allergy” in hospitalized patients: A cohort study. J Allergy Clin Immunol 133:790–796, 2014. [DOI] [PubMed] [Google Scholar]
- 7. Stevenson DD, Kowalski ML. An epidemic of over diagnosing drug allergies. Allergy Asthma Proc 35:92–94, 2014. [DOI] [PubMed] [Google Scholar]
- 8. Ponvert C, Perrin Y, Bados-Albiero A, et al. Allergy to betalactam antibiotics in children: Results of a 20-year study based on clinical history, skin and challenge tests. Pediatr Allergy Immunol 22:411–418, 2011. [DOI] [PubMed] [Google Scholar]
- 9. Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 Update by the Infectious Diseases Society of America. Clin Infect Dis 55:1279–1282, 2012. [DOI] [PubMed] [Google Scholar]
- 10. Fontaine C, Mayorga C, Bousquet PJ, et al. Relevance of the determination of serum-specific IgE antibodies in the diagnosis of immediate beta-lactam allergy. Allergy 62:47–52, 2007. [DOI] [PubMed] [Google Scholar]
- 11. Blanca M, Mayorga C, Torres MJ, et al. Clinical evaluation of Pharmacia CAP System RAST FEIA amoxicilloyl and benzylpenicilloyl in patients with penicillin allergy. Allergy 56:862–870, 2001. [DOI] [PubMed] [Google Scholar]
- 12. Macy E, Goldberg B, Poon KY. Use of commercial anti-penicillin IgE fluorometric enzyme immunoassays to diagnose penicillin allergy. Ann Allergy Asthma Immunol 105:136–141, 2010. [DOI] [PubMed] [Google Scholar]
- 13. Demoly P, Adkinson NF, Brockow K, et al. International consensus on drug allergy. Allergy 69:420–437, 2014. [DOI] [PubMed] [Google Scholar]
- 14. Salkind AR, Cuddy PG, Foxworth JW. The rational clinical examination. Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy. JAMA 285:2498–2505, 2001. [DOI] [PubMed] [Google Scholar]
- 15. Macy E, Ngor EW. Safely diagnosing clinically significant penicillin allergy using only penicilloyl-poly-lysine, penicillin, and oral amoxicillin. J Allergy Clin Immunol Pract 1:258–263, 2013. [DOI] [PubMed] [Google Scholar]
- 16. Zopf Y, Rabe C, Neubert A, et al. Women encounter ADRs more often than do men. Eur J Clin Pharmacol 64:999–1004, 2008. [DOI] [PubMed] [Google Scholar]
- 17. Khan DA. Treating patients with multiple drug allergies. Ann Allergy Asthma Immunol 110:2–6, 2013. [DOI] [PubMed] [Google Scholar]
- 18. Scherer K, Bircher AJ. Danger signs in drug hypersensitivity. Med Clin North Am 94:681–689, xv–x, 2010. [DOI] [PubMed] [Google Scholar]
- 19. Dash CH. Penicillin allergy and the cephalosporins. J Antimicrob Chemother 1:107–118, 1975. [DOI] [PubMed] [Google Scholar]
- 20. Picard M, Bégin P, Bouchard H, et al. Treatment of patients with a history of penicillin allergy in a large tertiary-care academic hospital. J Allergy Clin Immunol Pract 1:252–257, 2013. [DOI] [PubMed] [Google Scholar]


