Abstract
OBJECTIVE:
To examine pediatrician weight-management communication with overweight Latino children and their parents and whether communication differs by pediatrician-patient language congruency.
METHODS:
Mixed-methods analysis of video-recorded primary care visits with overweight 6- to 12-year-old children. Three independent reviewers used video/transcript data to identify American Academy of Pediatrics–recommended communication content and establish communication themes/subthemes. Language incongruence (LI) was defined as pediatrician limited Spanish proficiency combined with parent limited English proficiency (LEP). Bivariate analyses examined associations of LI with communication content/themes.
RESULTS:
The mean child age (N = 26) was 9.5 years old; 81% were obese. Sixty-two percent of parents had LEP. Twenty-seven percent of pediatricians were Spanish-proficient. An interpreter was used in 25% of LI visits. Major themes for how pediatricians communicate overweight included BMI, weight, obese, chubby, and no communication (which only occurred in LI visits). The pediatrician communicated child overweight in 81% of visits, a weight-management plan in 50%, a culturally relevant dietary recommendation in 42%, a recommendation for a follow-up visit in 65%, and nutrition referral in 50%. Growth charts were used in 62% of visits but significantly less often in LI (13%) versus language-congruent (83%) visits (P < .001).
CONCLUSIONS:
Many overweight Latino children do not receive direct communication of overweight, culturally sensitive dietary advice, or follow-up visits. LI is associated with a lower likelihood of growth chart use. During primary care visits with overweight Latino children, special attention should be paid to directly communicating child overweight, formulating culturally sensitive weight-management plans, and follow-up. With LEP families, vigilance is needed in providing a trained interpreter and using growth charts.
Keywords: childhood obesity, primary care, communication, Latino health
What’s Known on This Subject:
Little is known about how pediatricians communicate with overweight Latino children and their parents regarding overweight and obesity.
What This Study Adds:
Findings suggest that many overweight Latino children and their parents do not receive direct communication that the child is overweight, weight-management plans, culturally relevant dietary recommendations, or follow-up visits.
Latinos are among the most overweight racial/ethnic groups of US children,1 and are the largest minority group of children in the United States, comprising 16% of children <18 years old.2 In addition, 26 million Americans, or ∼9%, have limited English proficiency (LEP), including 20 million adults.3 It is unclear, however, how pediatricians communicate regarding childhood overweight with parents of overweight Latino children and whether language barriers affect communication of a child’s high weight status during primary care visits.
Well-child visits are an important opportunity to assess and treat childhood overweight/obesity among Latino children. During these visits, pediatricians can engage parents in conversations regarding weight and weight management. The American Academy of Pediatrics (AAP) recommends that clinicians screen for overweight, assess medical/behavior risk (by performing a history and physical examination and ordering screening laboratory tests), and use a staged treatment approach, including structured primary care weight management and referrals for multidisciplinary treatment.4,5 Although obesity management has been studied with the use of retrospective chart review,6 field notes by observers,7 and software documenting time and broad content areas,8 to our knowledge no study has video-/audio-recorded pediatrician-patient communication to examine specific clinical practice and communication strategies used by pediatricians during primary care visits with overweight children in general (the subject of a separate study) or specifically with Latino children.
It also is unclear whether language barriers affect either communication of children’s high weight status or recommended weight-related clinical practices during primary care visits with overweight Latino children. Previous studies document that, during outpatient visits with LEP Latinos, language barriers affect medical care,9 many pediatricians do not use professional interpreters,10 and, even during visits in which a medical interpreter is present, interpretation errors are common and have potential clinical consequences.11,12 The impact of language incongruence (LI), defined as pediatrician limited Spanish proficiency combined with parent LEP, on communication and clinical practices related to addressing childhood overweight is unknown.
The study objectives, therefore, were to examine pediatrician communication with overweight Latino children and their families and to determine whether differences exist in communication between language-congruent (LC) and LI parent-pediatrician interactions.
Methods
The study design was a cross-sectional mixed-methods analysis. A convenience sample of pediatricians, participants, and parents was recruited from 2 primary care clinics in academic and community settings. The sample consisted of equal numbers of pediatrician-patient interactions conducted in English and Spanish. At the academic center, resident/attending dyads were recruited; at the community clinic, only attending physicians were recruited. Written informed consent was obtained from pediatricians and parents (in their preferred language), written assent was obtained from 7- to 12-year-old participants, and verbal assent was obtained from 6-year-old children. The study protocol was approved by the Institutional Review Board of the University of Texas Southwestern Medical Center.
Eligibility criteria were aged between 6 and 12 years, Latino race/ethnicity (by parent self-identification), and overweight, with a directly measured BMI of ≥85th percentile for age and gender. English and Spanish surveys were verbally administered by a trained bilingual research assistant.
Previsit surveys assessed sociodemographic characteristics (of the child/parent and pediatrician), language proficiency, and LI, defined as a parent with LEP combined with a pediatrician with limited Spanish proficiency. LEP was measured by using the standard US Census Bureau question on the participant’s self-rated ability to speak English.13 LEP was defined as anything less than “very well.” Pediatricians were asked about Spanish proficiency by using a similar question, with limited Spanish proficiency defined as speaking Spanish less than “very well.”
Sociodemographic characteristics assessed for the child included age, gender, and race/ethnicity (all children were Latino by study design). Parental characteristics assessed included age, English proficiency, parental weight and height (by self-report for the parent/guardian present at the visit, who also reported the weight and height of the other biological parent/guardian if he/she was not present at the visit), marital status, highest educational attainment among adults in the child’s household, and annual household income. Pediatrician characteristics (by self-report) included race/ethnicity, gender, and weight and height (ascertained via a series of other questions to mask the study focus on weight).
Child weight and height were measured in the clinic by trained clinical staff with the use of standardized clinical protocols and calibrated instruments. BMI was calculated as weight in kilograms divided by height in meters squared. BMI percentiles were determined by using age- and gender-specific Centers for Disease Control and Prevention growth charts.14 BMI-percentile categories were defined by using AAP-recommended cutoffs,4 including healthy weight, overweight, and obesity, defined as the ≥5th to <85th, ≥85th to <95th, and ≥95th BMI percentiles for age and gender, respectively. With the use of self-reported parent and pediatrician weight and height from the previsit surveys, healthy weight, overweight, and obesity were defined by using BMI cutoffs of 18.5 to <25, ≥25 to <30, and ≥30, respectively.15
Pediatricians and participants were not told that the study was about weight but that it focused on pediatrician-patient communication regarding preventive health topics. Digital video- and audio-recorders were placed in discrete locations in examination rooms by research staff before visits. Participants were recruited from May through October 2012, and $10 honoraria were provided to participating families and pediatricians.
Qualitative Analysis
All recorded visits were viewed (or for audiotapes, listened to) and transcribed. Visits conducted in Spanish or through Spanish interpreters were reviewed, transcribed, and corrected twice by a bilingual medical student and a bilingual research assistant trained in medical Spanish. Transcripts were analyzed by using margin coding and grounded theory.16 Thematic coding and the constant-comparison method were used to identify communication themes within and between visits.17 Constant comparison provided a means to group similar codes into themes and subthemes. Three trained coders independently reviewed transcripts, listed major themes and subthemes in the margins, and identified dialogue that best illustrated major themes. To validate thematic coding, coders met to compare results and develop a taxonomy of themes/subthemes. Differences among coders were resolved using consensus. The 3 reviewers also were trained to identify prespecified communication content recommended by the AAP,18 including the following: determine/interpret child’s BMI-for-age, assessed as pediatrician communication of weight status by using the growth chart and direct communication that the child was overweight; address culture, assessed as use of a trained medical interpreter (when indicated) and discussion of traditional foods/culturally relevant dietary recommendations (broadly defined as any mention of traditional or culturally relevant Latino foods); perform a comprehensive physical assessment, assessed as communication of weight-related physical examination findings (eg, acanthosis); identify whether high weight status is accompanied by another disorder, assessed as discussion of family history and weight-related laboratory studies; set treatment goal, assessed as discussion of a goal for weight maintenance or loss; encourage healthy eating behaviors, regular physical activity, and reduced sedentary behaviors, assessed as discussion of changes in sedentary activity, physical activity, and diet; target both parents and children for behavior change, assessed as discussion of parent/family diet/lifestyle changes; and maintain treatment program over a long period of time, assessed as communication referring to a nutrition or a weight-management program and scheduling a follow-up visit with the pediatrician to address weight (Supplemental Fig 2). Coder agreement was excellent (average pairwise agreement: 85%–100%); κ scores, calculated by using the SAS macro MAGREE (SAS Institute, Cary, NC), ranged from 0.71 (for discussion of parent/family diet/lifestyle changes) to 1.0 (for discussion of physical activity and diet).
Quantitative Analysis
Descriptive statistics were used to summarize sample characteristics, proportions receiving each communication-content area, and the proportion of parents who reported that the pediatrician communicated with them regarding their child’s weight status. Pearson’s χ2 statistic was used to compare proportions receiving the communication-content areas and reporting pediatrician communication of child overweight between LI and LC groups. Statistical analyses were conducted by using SAS version 9.2.
Results
For children, the mean age was 9.5 years, more than half were female, and most were obese (Table 1). For parents, the mean age was 35 years, approximately two-thirds were LEP, and most were overweight/obese, married, and not high school graduates. The mean annual household income was $24 000. For pediatricians, most were female, the plurality was white, approximately one-quarter were Spanish proficient, and less than half were overweight or obese.
TABLE 1.
Participant Characteristics
| Characteristic | Proportion (%) |
|---|---|
| Child (N = 26) | |
| Age, mean (95% CI), y | 9.5 (7–12) |
| Female, % | 58 |
| Weight status, % | |
| Overweight | 19 |
| Obese | 81 |
| Parent (N = 26) | |
| Age, mean (95% CI), y | 35 (30–41) |
| LEP, % | 62 |
| Weight status, % | |
| Mother overweight/obese | 81 |
| Father overweight/obese | 54 |
| Marital status, % | |
| Married | 65 |
| Separated or divorced | 19 |
| Never married | 16 |
| Household (N = 26), % | |
| Highest educational attainment | |
| Not high school graduate | 58 |
| High school graduate/GED | 15 |
| Technical school or some college | 27 |
| College graduate or higher | 0 |
| Annual household income, mean (95% CI), $ | 24 000 (4500–50 000) |
| Pediatrician (N = 15) | |
| Female, % | 73 |
| Race/ethnicity, % | |
| African American | 13 |
| Asian | 33 |
| Latino | 13 |
| White | 40 |
| Spanish proficiency, % | |
| Speaks very well (versus well/not well/not at all) | 27 |
| Pediatrician weight status, % | |
| Healthy weight | 60 |
| Overweight | 27 |
| Obese | 12 |
CI, confidence interval; GED, General Educational Development.
Pediatricians used growth charts to communicate weight status in almost two-thirds of visits and directly communicated that the child was overweight in >80% of visits (Table 2). Only 1 in 4 pediatricians used trained medical interpreters (when indicated), and less than half discussed traditional Latino foods. Physical examination findings were communicated in less than half of visits, family history was assessed in one-third of visits, and laboratory study orders or results were communicated in less than two-thirds of visits. Pediatricians communicated weight-management goals and discussed sedentary activity behaviors in half of visits, recommended physical activity in 4 in 5 visits, encouraged dietary changes in almost all visits, and counseled with regard to parental role-modeling/family/household lifestyle changes in less than one-third of visits. Parents/children received a plan for long-term weight-management treatment, via referral to nutrition, a weight-management program, or physician follow-up, in half to two-thirds of visits.
TABLE 2.
Communication Content Areas Recommended for Screening and Assessing Overweight and Obesity During Health Supervision Visits
| Content Area | Measure by Which Content Deemed Present | Proportion of Visitsa, % |
|---|---|---|
| Screening and assessment | ||
| Determine and interpret child’s BMI-for-age | • Growth chart used to communicate weight status | 62 |
| • Child overweight directly communicated | 81 | |
| Address culture | • Trained medical interpreter used, when indicatedb | 25 |
| • Traditional Latino foods discussed/culturally relevant dietary recommendation made | 42 | |
| Perform comprehensive physical assessment | • Abnormal physical examination findings communicated (eg, acanthosis nigricans) | 42 |
| Identify whether “weight status accompanied by any other disorder” | • Family history discussed | 35 |
| • Laboratory studies related to elevated weight recommended/discussed | 62 | |
| Treatment | ||
| Set treatment goal | • Goal for weight maintenance or loss discussed | 50 |
| Encourage healthy eating behaviors, regular physical activity, and reduced sedentary behaviors | • Sedentary activity behavior changes discussed | 50 |
| • Physical activity changes discussed | 81 | |
| • Dietary changes discussed | 96 | |
| Target both parents and children for behavior change | • Parent/family diet/lifestyle changes discussed | 31 |
| Maintain treatment program over long period of time | • Referral to nutritionist or weight-management program discussed | 50 |
| • Follow-up visit for overweight discussed | 65 |
N = 26.
One-third of visits were audio-recorded only.
During visits in which pediatrician and parent languages were incongruent (n = 8).
Growth charts were used significantly less often in LI (13%) than in LC (83%) visits (P = .001), and the only LI visit in which the growth chart was reviewed was conducted in English (Table 3). Discussion of traditional foods/culturally relevant dietary recommendations and nutrition referrals occurred in almost twice as many LI as LC visits; however, these differences were not statistically significant. There were no significant differences between LI and LC visits for any other content areas.
TABLE 3.
Communication-Content Areas by LC Between Pediatrician and Parent
| Content Area | Proportion Meeting Content-Area Recommendation, % | P | |
|---|---|---|---|
| LI (n = 8) | LC (n = 18) | ||
| Growth chart used | 13 | 83 | .001 |
| Discuss traditional foods/culturally relevant diet recommendations made | 63 | 33 | .2 |
| Referral to nutrition | 75 | 39 | .2 |
| Physician directly communicated child overweight | 63 | 89 | .3 |
| Dietary changes discussed | 88 | 100 | .3 |
| Family history discussed | 50 | 28 | .4 |
| Laboratory studies recommended | 75 | 56 | .4 |
| Weight-related physical examination findings discussed | 50 | 39 | .7 |
| Weight-status improvement plan communicated | 38 | 56 | .7 |
| Sedentary activity discussed | 50 | 50 | .99 |
| Physical activity discussed | 88 | 78 | .99 |
| Parent/family diet/lifestyle changes discussed | 25 | 33 | .99 |
| Physician follow-up visit recommended | 63 | 67 | .99 |
The qualitative analysis of how pediatricians communicate that a child is overweight yielded 5 major themes, 9 subthemes (Table 4), and unique and overlapping themes/subthemes by LC (Fig 1). Major communication themes included BMI, weight, obese, chubby, and no communication regarding weight status. During a visit in which BMI was the communication theme, 1 pediatrician said, “I’m worried about the weight. In children, we start to look at their weight in proportion to their height, their body mass index; her BMI is off the charts.” For visits in which communication of weight status was organized around “weight,” an illustrative pediatrician quote was, “I’m sure you probably are aware of her weight. She was going along—dot, dot, dot, and then boom, she just jumped right up. That’s a big concern. I don’t want her to stay up there, it’s not healthy.” During some visits, the terms “obese” or “chubby” were used in isolation to convey a child’s high weight status. One physician stated, “He is obese and running the risk of developing high blood pressure, diabetes, and all the problems that come with obesity.” Communication themes/subthemes noted in both LC and LI visits were as follows: “not healthy,” “high weight,” “weight going up,” “heavy,” and “fat.” Unique to LI visits was a lack of any weight discussion; among LC visits, unique themes/subthemes included BMI, overweight, obese/obesity, and muscle mass (Fig 1).
TABLE 4.
How Pediatricians Communicate That a Child Is Overweight: Themes and Subthemes
| Theme | Subtheme |
|---|---|
| BMI | Weight |
| Overweight or obese | |
| Muscle mass (“un cálculo de la masa muscular”) | |
| Weight | Not healthy |
| High | |
| Going up | |
| Heavy (“un poquito pesadito”) | |
| Fat | |
| Overweight | |
| Obese | |
| Chubby | |
| No communication |
FIGURE 1.
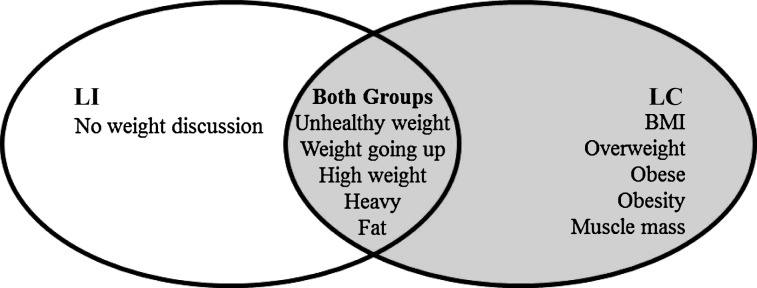
Qualitative analysis of how pediatricians communicate regarding child’s high weight status: themes/subthemes by LC. Common and unique communication themes/subthemes regarding how pediatricians communicate a child’s high weight status in LI and LC visits are shown. Unique to LI visits was a lack of any weight discussion.
In the qualitative analysis of how pediatricians communicate weight-management treatment goals (Table 5), 2 major themes (no weight goal and weight goal) and 6 subthemes were identified. For visits in which no goal was given, an illustrative pediatrician quote was, “We are going to see her back in 3 months for a weight follow-up, and we’ll see where her weight is going.” Underscoring the subtheme “weight deemphasized,” another pediatrician stated, “It’s not so much about losing weight, it’s about changing habits.” The following exchange occurred during a visit in which the weight goal was agreed upon collaboratively:
Physician: “I want to see him in 3 months to see how he’s doing.”
Parent: “How many pounds in 3 months? Two? One?”
Child: “Twenty.”
Physician: “Too much.”
Child: “Ten?”
Physician: “We’ll say 7. His goal is 7 pounds.”
TABLE 5.
How Pediatricians Communicate Weight-Management Treatment Goals: Themes and Subthemes
| Theme | Subtheme |
|---|---|
| No weight goal | Follow weight |
| Weight deemphasized | |
| Referred to nutrition only | |
| Weight goal | Collaborative goal setting |
| Lose weight slowly | |
| Maintain weight |
Another pediatrician who provided a weight goal stated, “Since he gained weight slowly, he should lose weight slowly. If we make him lose weight suddenly, it might not work. Our goal is to lose 5 pounds in 3 months.” Regarding the subtheme “maintain weight,” a pediatrician said, “Our goal is not to necessarily lose weight, but for the weight to stay stable.”
The qualitative analysis of culturally relevant dietary communication included 3 major themes and 11 subthemes (Table 6). Major communication themes included limit portions, use healthy substitutes, and culturally relevant foods discussed but no advice given. An illustrative exchange about limiting portions was as follows:
Parent: “If he’s given beans and soup, he eats a lot. He eats adult plates.”
Physician: “Big plates?”
Parent: “Yes.”
Physician: “Why don’t we choose to make 1 change, for example, portions.”
TABLE 6.
Culturally Relevant Dietary Communication: Themes and Subthemes
| Theme | Subtheme |
|---|---|
| Limit portions | Tortillas |
| Beans | |
| Use healthy substitutes | Low-calorie/low-carbohydrate tortillas |
| Fruit instead of tacos | |
| Calorie-free sweeteners instead of sugar in agua naturalesa | |
| Beans instead of pizza | |
| Cultural foods discussed, no advice given | Burrito |
| Beans | |
| Chorizo | |
| Quesadillas | |
| Pozole |
Agua naturales is water mixed with natural fruit or fruit juice plus an added sweetner (typically sugar).
Regarding healthy substitutes, a pediatrician remarked, “Do you like tortillas? I love tortillas. I get ones called ‘carb-free.’ Look at the back and each tortilla is 80 calories. The kind I used to buy were 130 calories.” A dialogue illustrating a discussion of traditional Latino foods without advice was as follows:
Physician: “Let’s talk about the diet .…”
Parent: “He has tortilla de horneo, a burrito.”
Physician: “And what is in the burrito, beans?”
Child: “Potatoes and chorizo.”
Physician: “So nothing more? One burrito?”
Parent: “Yes.”
In postvisit surveys, 8% of parents reported that the pediatrician did not communicate that their child was overweight (half had direct communication observed in the video-/audio-recording), and 12% reported that their pediatrician stated that their child was at a healthy weight (all had direct communication of overweight observed in the recordings) (Table 7). There was a nonsignificant trend (P = .07) toward LI parents more often reporting no pediatrician communication of the child’s overweight and LC parents more often reporting pediatricians describing their child as having a healthy weight.
TABLE 7.
Postvisit Parental Reports of Pediatrician Communication Regarding Their Child’s Weight Status
| Postvisit Survey | Proportion, % | Pa | ||
|---|---|---|---|---|
| Overall (N = 26) | LI (n = 8) | LC (n = 18) | ||
| Postvisit parental report that pediatrician | .07 | |||
| Did not communicate that child was overweight | 8b | 25 | 0 | |
| Communicated child was healthy weight | 12c | 0 | 17 | |
| Communicated child was overweight | 81 | 75 | 83 | |
All children were overweight or obese.
For comparison of LI versus LC groups.
Half had direct communication of overweight observed in the video-/audio-recording.
One hundred percent had direct communication of overweight observed.
Discussion
This is the first study, to our knowledge, to directly video-/audio-record pediatrician-patient communication regarding weight among overweight Latino children. Findings of particular concern include the use of terms that people with obesity consider “very undesirable,”19,20 such as “fat”; the low proportions of parents directly informed of their child’s overweight, weight-management plans, and follow-up visits; and the lack of any weight discussion in LI visits. For effective weight management, patients/parents first must recognize the child’s overweight, and BMI screening and communication increase parental recognition of overweight in children.21 This is important because, in general, ∼60% of parents do not recognize that their overweight school-age child is overweight.22 Pediatricians are encouraged to screen for overweight in all children ≥6 years old and offer children moderate- to high-intensity interventions.4,5 Many studies suggest that overweight children and their parents want primary care guidance regarding overweight, weight-related health risks, behaviors that help improve children’s weight, and follow-up for overweight.23,24 Our study indicates, however, that many pediatricians do not communicate that overweight Latino children are overweight. This finding complements other studies of BMI screening among children of other races/ethnicities.8,25,26 Follow-up visits also are crucial, because experimental studies of primary care weight-management interventions in a general population suggest that more frequent, higher-intensity behavioral counseling results in small-to-moderate BMI improvements.5
A particularly noteworthy finding is that LI is associated with a significantly lower likelihood of the use of growth charts during primary care visits with overweight Latino children. Although the reason for this disparity could not be determined, it is possible that communication barriers led pediatricians with limited Spanish proficiency not to review the growth charts, particularly because a medical interpreter was used in only one-quarter of LI visits, and the only visit in which the growth chart was reviewed was conducted in English. These findings underscore the importance of having appropriate language services available in primary care and performing high-quality weight-management clinical practices when caring for LEP patients.27
Another notable finding was the low frequency of communication regarding traditional Latino foods or culturally relevant dietary plans. Previous research has documented that Latino parents welcome suggestions regarding how to make traditional Latino foods healthier, such as substituting whole-wheat for flour tortillas, water with lemon for sugary beverages, and fish for red meat, and including more vegetables in meals28; and culturally tailored obesity interventions have been shown to effectively reduce BMI and improve target health behaviors among Latino-American and Mexican-American children.29–31 Also noteworthy, although not significant, was the higher frequency of communication regarding traditional foods among LI versus LC groups. It is possible that LI underscored cultural differences, and perhaps the need to address culturally relevant dietary plans. The implications of these study findings are that instead of simply mentioning burritos, pediatricians might suggest substituting low-calorie, high-fiber whole-grain tortillas filled with nonstarchy vegetables (eg, grilled bell peppers instead of potatoes) and grilled fish instead of chorizo. The findings and previous studies also suggest that by paying particular attention to communicating with patients regarding culturally relevant dietary plans, pediatricians may be particularly effective in improving the health and weight status of overweight Latino children.
Certain study limitations should be noted. Participants were Latino (because a primary objective was to examine communication by LC), not differentiated by subgroup, and recruited from urban clinics in academic and community medical centers in Dallas, Texas. The study findings, therefore, may not necessarily generalize to non-Latinos, particular subgroups, private practices, nonurban regions, other parts of the country, or regions with a different subgroup composition. Participants, on average, had lower educational attainment, and so the findings may not generalize to populations with higher parental educational attainment. The sample size was relatively small, which may account for the lack of statistical significance in proportions receiving specific communication content between LI and LC groups, despite larger-magnitude differences (eg, postvisit parental reports of pediatrician communication regarding their child’s weight status); the focus of the study, however, was on videotaping pediatrician-patient interactions and describing specific communication content, because this method of direct observation and communication analysis has not been used before.
This study has several strengths, including being the first to use video-/audio-recordings to directly observe/examine pediatrician-patient communication regarding weight during primary care visits; use of a sample of Latino participants with and without LEP; and inclusion of a particularly high-risk group, parents from low-income, low-educational-attainment households with public insurance. High proportions of children from such households are affected by overweight/obesity and have substantial need for effective primary care weight-management solutions.32
Conclusions
The study findings suggest that during primary care visits with overweight Latino children, special attention should be paid to direct communication that the child is overweight with the use of patient-preferred terms (eg, too much weight for his/her health or “demasiado peso para su salud”), providing weight-management plans, making culturally relevant dietary recommendations, and scheduling follow-up visits. During primary care visits with LEP families with overweight children, vigilance is needed in providing a trained medical interpreter or bilingual provider and using the growth chart to communicate that the child is overweight.
Supplementary Material
Glossary
- AAP
American Academy of Pediatrics
- LC
language congruence/congruent
- LEP
limited English proficiency
- LI
language incongruence/incongruent
Footnotes
Dr Turer designed the study and data collection instruments, supervised data collection at each of the study sites, assisted with analyses and interpretation of data, and drafted the manuscript; Mr Montaño assisted with designing the study and data collection instruments, video-/audio-recorded primary care visits at the study sites, assisted with analyses and interpretation of data, and contributed to drafting the manuscript; Drs Lin and Hoang assisted with analyses and interpretation of data and contributed to drafting the manuscript; Dr Flores oversaw the study design, development of data collection instruments, and analyses and interpretation of data and critically revised the manuscript; and all authors approved the final manuscript as submitted.
This work was presented in part as a platform presentation at the annual meeting of the Pediatric Academic Societies; May 6, 2013; Washington, DC.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by award K23HL118152-01A1 from the National Heart, Lung, and Blood Institute (to Dr Turer). The content is solely the responsibility of the authors and does not necessarily represent the official views of National Heart, Lung, and Blood Institute or the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307(5):483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Census Bureau. The Hispanic population in the United States: 2012. Available at: www.census.gov/population/hispanic/data/2012.html. Accessed July 14, 2014
- 3.US Census Bureau. Language spoken at home: 2012 American community survey 1-year estimates. Available at: www.census.gov/compendia/statab/cats/population/ancestry_language_spoken_at_home.html. Accessed July 14, 2014
- 4.Barlow SE, Expert Committee . Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192 [DOI] [PubMed] [Google Scholar]
- 5.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of primary care interventions for weight management in children and adolescents: an updated, targeted systematic review for the USPSTF. Evidence synthesis no. 76. Rockville, MD: Agency for Healthcare Research and Quality; January 2010. AHRQ publication 10-05144-EF-1 [PubMed]
- 6.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114(2). Available at: www.pediatrics.org/cgi/content/full/114/2/e154 [DOI] [PubMed] [Google Scholar]
- 7.Scott JG, Cohen D, DiCicco-Bloom B, et al. Speaking of weight: how patients and primary care clinicians initiate weight loss counseling. Prev Med. 2004;38(6):819–827 [DOI] [PubMed] [Google Scholar]
- 8.Martin LA, Ariza AJ, Thomson JS, Binns HJ, Pediatric Practice Research Group . Seconds for care: evaluation of five health supervision visit topics using a new method. J Pediatr. 2008;153(5):706–711, e1–e2 [DOI] [PubMed] [Google Scholar]
- 9.Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19(2):60–67 [DOI] [PubMed] [Google Scholar]
- 10.Kuo DZ, O’Connor KG, Flores G, Minkovitz CS. Pediatricians’ use of language services for families with limited English proficiency. Pediatrics. 2007;119(4). Available at: www.pediatrics.org/cgi/content/full/119/4/e920 [DOI] [PubMed] [Google Scholar]
- 11.Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111(1):6–14 [DOI] [PubMed] [Google Scholar]
- 12.Flores G, Abreu M, Barone CP, Bachur R, Lin H. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;60(5):545–553 [DOI] [PubMed] [Google Scholar]
- 13.US Census Bureau. 2010 Census summary file 1: technical documentation. Available at: www.census.gov/prod/cen2010/doc/sf1.pdf. Accessed July 14, 2014
- 14.Centers for Disease Control and Prevention. Growth charts. Available at: www.cdc.gov/growthcharts/percentile_data_files.htm. Accessed July 14, 2014
- 15.National Institutes of Health . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;6(suppl 2):51S–209S [PubMed] [Google Scholar]
- 16.Glaser BG, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, NY: Aldine Publishing; 1967 [Google Scholar]
- 17.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications; 2009 [Google Scholar]
- 18.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(suppl 4):S193–S228 [DOI] [PubMed] [Google Scholar]
- 19.Knierim S, Rahm A, Haemer M, et al. Hispanic parents’ preferences for terms used in pediatric weight counseling. E-PAS2014:2953.735. Available at www.abstracts2view.com/pas/view.php?nu=PAS14L1_2953.735. Accessed July 14, 2014.
- 20.Volger S, Vetter ML, Dougherty M, et al. Patients’ preferred terms for describing their excess weight: discussing obesity in clinical practice. Obesity (Silver Spring). 2012;20(1):147–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chomitz VR, Collins J, Kim J, Kramer E, McGowan R. Promoting healthy weight among elementary school children via a health report card approach. Arch Pediatr Adolesc Med. 2003;157(8):765–772 [DOI] [PubMed] [Google Scholar]
- 22.West DS, Raczynski JM, Phillips MM, Bursac Z, Heath Gauss C, Montgomery BEE. Parental recognition of overweight in school-age children. Obesity (Silver Spring). 2008;16(3):630–636 [DOI] [PubMed] [Google Scholar]
- 23.Borra ST, Kelly L, Shirreffs MB, Neville K, Geiger CJ. Developing health messages: qualitative studies with children, parents, and teachers help identify communications opportunities for healthful lifestyles and the prevention of obesity. J Am Diet Assoc. 2003;103(6):721–728 [DOI] [PubMed] [Google Scholar]
- 24.Turer CB, Mehta M, Durante R, Wazni F, Flores G. Parental perspectives regarding primary-care weight-management strategies for school-age children [published online ahead of print April 10, 2014]. Matern Child Nutr. doi:10.1111/mcn.12131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barlow SE, Bobra SR, Elliott MB, Brownson RC, Haire-Joshu D. Recognition of childhood overweight during health supervision visits: does BMI help pediatricians? Obesity (Silver Spring). 2007;15(1):225–232 [DOI] [PubMed] [Google Scholar]
- 26.Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. Medical evaluation of overweight children and adolescents: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110(1 pt 2):222–228 [PubMed] [Google Scholar]
- 27.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–299 [DOI] [PubMed] [Google Scholar]
- 28.Flores G, Maldonado J, Durán P. Making tortillas without lard: Latino parents’ perspectives on healthy eating, physical activity, and weight-management strategies for overweight Latino children. J Acad Nutr Diet. 2012;112(1):81–89 [DOI] [PubMed] [Google Scholar]
- 29.Barkin SL, Gesell SB, Po’e EK, Escarfuller J, Tempesti T. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children. Pediatrics. 2012;130(3):445–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bender MS, Nader PR, Kennedy C, Gahagan S. A culturally appropriate intervention to improve health behaviors in Hispanic mother-child dyads. Child Obes. 2013;9(2):157–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Branscum P, Sharma M. A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: lessons learned from the previous decade. Obes Rev. 2011;12(5):e151–e158 [DOI] [PubMed] [Google Scholar]
- 32.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84(4):707–716 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


