Abstract
OBJECTIVE:
This study was designed to determine whether living in a neighborhood in which poverty levels increase across adolescence is associated with heightened levels of allostatic load (AL), a biological composite reflecting cardiometabolic risk. The researchers also sought to determine whether receipt of emotional support could ameliorate the effects of increases in neighborhood poverty on AL.
METHODS:
Neighborhood concentrations of poverty were obtained from the Census Bureau for 420 African American youth living in rural Georgia when they were 11 and 19 years of age. AL was measured at age 19 by using established protocols for children and adolescents. When youth were 18, caregivers reported parental emotional support and youth assessed receipt of peer and mentor emotional support. Covariates included family poverty status at ages 11 and 19, family financial stress, parental employment status, youth stress, and youths’ unhealthful behaviors.
RESULTS:
Youth who lived in neighborhoods in which poverty levels increased from ages 11 to 19 evinced the highest levels of AL even after accounting for the individual-level covariates. The association of increasing neighborhood poverty across adolescence with AL was not significant for youth who received high emotional support.
CONCLUSIONS:
This study is the first to show an association between AL and residence in a neighborhood that increases in poverty. It also highlights the benefits of supportive relationships in ameliorating this association.
Keywords: African Americans, allostasis, physiology, human development, poverty
What’s Known on This Subject:
Allostatic load (AL), a biomarker of cardiometabolic risk, predicts the onset of the chronic diseases of aging including cardiac disease, diabetes, hypertension, and stroke. Socioeconomic-related stressors, such as low family income, are associated with AL.
What This Study Adds:
African American youth who grow up in neighborhoods in which poverty levels increase across adolescence evince high AL. The study also highlights the benefits of emotional support in ameliorating this association.
Life in a low socioeconomic status (SES) rural environment and the stressors that accompany it are associated with a host of detrimental biological profiles that contribute to racial disparities in health across the life span.1,2 The concept of allostatic load (AL) suggests that adaptation to SES-related stress can “weather” tissues and organs that lie downstream of stress response systems, creating wear and tear on the body as a consequence of frequent or prolonged activation of these pathways.3–7 AL is a biomarker of cardiometabolic risk characterized by multisystem dysregulation. It is operationally defined by composite indicators that reflect the activity of stress response systems, such as the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis, and bodily processes influenced by their outflow, such as lipid metabolism, fat deposition, and immune functioning.8 AL predicts the onset of chronic diseases including hypertension, cardiac disease, diabetes, stroke, and all-cause mortality.9 A hypothesis proposed in the pediatric health disparities literature that has not received empirical attention concerns the possibility that living in a high-poverty neighborhood during childhood, adolescence, or both will engender heightened levels of AL in youth, with downstream health consequences.2
Little is known about the health of youth, African American or not, who experience changes in neighborhood contexts. Neighborhood socioeconomic conditions shift over time as a consequence of broader socioeconomic upheavals such as the recession of 2007–2010. Even without moving out of a neighborhood, many African American children still reside in progressively lower SES areas over time.10 The process of change in neighborhoods over time is called neighborhood dynamics. A primary aim of this study was to determine the effects that changes in neighborhood poverty levels have on rural African American youths’ AL in a cohort followed from ages 11 to 19.
The current study also addressed protective effects. Research involving children and adolescents suggests that receipt of emotional support from parents11–13 and peers14,15 is capable of offsetting some of the risky neuroendocrine, metabolic, inflammatory, and cardiovascular profiles that tend to develop after exposure to adversity.1,2 We investigated the possibility that the receipt of emotional support during adolescence has a protective effect, reducing the impact of increases in neighborhood poverty on AL in rural African American youth.
Methods
Sample
The sample comprised African American target youth and their primary caregivers, who participated in 9 annual data collections. Youths’ mean age was 11.2 years at the beginning of the larger study in 2000–2001 and 19.2 years at the last assessment in 2009–2010. The families resided in 9 rural counties in Georgia, in small towns and communities in which poverty rates are among the highest in the nation and unemployment rates are above the national average.16 Of the youth in the sample, 53% were girls and 47% were boys. At baseline, 78% of the caregivers had completed high school or earned a general equivalency diploma. Although the primary caregivers in the sample worked an average of 39.4 hours per week, 46.3% lived below federal poverty standards, with a median family income of $1655 per month. At the last assessment, the proportion was 49.1% with a median income of $1169. The increase in the proportion of families living in poverty and the decrease in family income over time may have resulted from the economic recession that was occurring during 2009 and 2010, when the last wave of data were collected.
At the first assessment, 667 families were selected randomly from lists that schools provided of their fifth-grade students; Brody and colleagues17 described the recruitment process in detail. From a sample of 561 at the age 18 data collection (a retention rate of 84%), 500 adolescents were selected randomly to participate in the assessment of AL; of this subsample, 489 agreed to participate. The current study was based upon the 420 participants (193 men and 227 women) who agreed to participate in the assessment of AL and provided data on all measures at the age 19 data collection. Comparisons, using independent t tests and χ2 tests, of the 420 youth who provided data at age 19 with the 69 who did not revealed no differences on any demographic or study variable.
Procedure
All data were collected in participants’ homes by 2 African American field researchers using a standardized protocol. At each data collection wave, participants were compensated $100 and informed consent was obtained. Caregivers consented to minor youths’ participation in the study, and minor youth assented to their own participation. Youth age 18 and older consented to their own participation.
Measures
Childhood Neighborhood Poverty
Childhood data were collected at the first wave, when the target youth were 11 years of age. Neighborhood poverty concentrations were assessed by using the 2000 STF3A census tract data, which was geocoded with each participant’s residential address in 2000. The mean of the proportion of households in a census tract below the federal poverty level was 20.2 (SD = 7.7).
Neighborhood Poverty in Adolescence
At age 19, neighborhood poverty concentration was assessed by using the US Census Bureau’s American Community Survey. This nationwide survey is taken every year to collect data about the demographic, social, economic, and housing characteristics of the American population.18 The mean percentage of households in participants’ tract-level neighborhoods whose income fell below the federal poverty level was 23.4 (SD = 9.1).
AL
Youths’ AL was measured at age 19 by using protocols established for field studies involving children and adolescents.12,19–21 Resting blood pressure was monitored with Dinamap Pro 100 (Critikon; Tampa, FL) while the youth sat reading quietly. Three readings were taken every 2 minutes, and the average of the last 2 readings was used as the resting index. This procedure yields highly reliable indices of resting blood pressure.22 Overnight urine samples were collected for assays of catecholamines and cortisol. Beginning on the evening of data collection, all urine that a youth voided from 8 pm to 8 am was stored on ice in a container with metabisulfite as a preservative. Total volume was recorded, and four 10-mL samples were randomly extracted and deep frozen at −80°C until assays were completed. The frozen urine was delivered to the Emory University Hospital medical laboratory in Atlanta, Georgia, for assaying. Total unbound cortisol was assayed with a radioimmune assay.23 Epinephrine and norepinephrine were assayed with high-pressure liquid chromatography with electrochemical detection.24 Creatinine was assayed to control for differences in body size and incomplete urine voiding.25 Technicians blind to the study assayed the samples. BMI was calculated as weight in kilograms divided by the square of height in meters. In the current study, mean BMI was 27.5 (SD = 7.9), with 51.7% of the participants classified as overweight (BMI ≥25).
We calculated AL by summing the number of physiologic indicators on which each emerging adult scored in the top quartile of risk; possible scores ranged from 0 to 6. The AL indicators included overnight cortisol, epinephrine, and norepinephrine; resting diastolic and systolic blood pressure; and BMI (weight in kilograms divided by the square of height in meters). Previous studies of AL in adults26 and adolescents14 have included similar metrics, combining multiple physiologic indicators of risk into 1 total AL index. The mean number of indicators that were above the top quartile of risk was 1.5.
Emotional Support
Emotional support included assessments of parent, peer, and mentor support at the age 18 data collection. Each youth’s primary caregiver responded to the 11-item Family Support Inventory.27 Cronbach’s α for the scale was 0.94. Peer support was measured by using youth reports on the 4-item Emotional Support subscale from the Carver Support Scale.28 Support from an adult mentor was assessed with the Mentor Relationship Index29; an adult mentor reported on positivity with the youth in the study. Cronbach’s α was 0.74. The parent, peer, and mentor indicators were standardized and summed to form a composite of emotional support for which Cronbach’s α was 0.98.
Covariates
Covariates examined in the current study included gender; family poverty status at age 11, age 19, and their interaction; family financial stress; primary caregiver employment status; and youths’ diet, smoking, alcohol use, and perceived life stress at age 19. Family poverty status was categorized by using US government criteria of an income-to-needs ratio ≤1.5. Youths’ primary caregivers were categorized as unemployed if the caregiver did not have a job. Family financial stress was operationalized through unmet material needs such as inadequate food and clothing, an inability to pay bills, and inadequate resources for obtaining health insurance and medical care.30 An unhealthful diet, smoking, and alcohol use were measured with items from the Youth Risk Behavior Survey.31 Youths’ perceptions of life stress were measured by using the Life Stress scale from the MacArthur Successful Aging Battery.32
Analytic Strategy
The first aim was to determine whether adolescents who remained in the same neighborhoods over time and whose neighborhood poverty levels increased would evince higher AL levels. The second aim was to examine the protective effects of emotional support. These research aims pose 2 data analytic challenges. First, the data are hierarchically nested (individual participants nested within neighborhoods), and participants living in the same neighborhoods will be influenced by common neighborhood environments. Because observations are potentially interdependent, traditional regression models will not control for this multilevel data structure. In this study, to avoid this problem with AL, a dependent measure that is a count variable, Models 1 through 3 were undertaken. These multilevel Poisson models33 were executed by using the Stata 12 statistical software (Stata Corp, College Station, TX) on a sample of participants who resided in the same neighborhood across time.
To determine whether the results obtained would change when participants who moved during the course of the study were included in the analyses and to address selection bias, we executed a cross-classified multilevel Poisson model.33 This model enabled us to examine the poverty status of more than 1 neighborhood for participants who moved between 2000 and 2010. The selection bias issue (do participants who move differ from those who do not move) was addressed in the data analytic scheme by using inverse probability of treatment weights.34 We included residential stability as the selection bias variable in the first part of the analysis. A propensity score was then calculated for the likelihood of a participant’s staying in his or her neighborhood until 2010 from a logistic regression equation including neighborhood poverty level at age 11; youth gender; family poverty at ages 11 and 19; caregiver employment status; youth perceived stress; family financial stress; and youth diet, smoking, and alcohol use at age 19. Differences between participants with similar propensity values are considered to be a function of staying in the year 2000 neighborhood rather than potential confounds.35 Thus, a model was executed (Model 4 in Table 1) that included all study participants: those who resided in the same neighborhood across time and those who did not, using the inverse of a propensity score weighting to adjust for selection out of age 11 neighborhoods.
TABLE 1.
Descriptive Statistics for Individual- and Neighborhood-Level Measures
| Variables | Mean | SD | Minimum | Maximum | % |
|---|---|---|---|---|---|
| Individual measures | |||||
| Age, y (baseline) | 11.65 | 0.36 | 10.83 | 12.78 | — |
| AL | 1.48 | 1.24 | 0.00 | 5.00 | — |
| BMI | 27.52 | 7.91 | 15.36 | 55.31 | — |
| Emotional support at age 18 | 0.00 | 1.00 | −3.95 | 1.93 | — |
| Diet at age 19 | 5.08 | 1.63 | 0.00 | 8.00 | — |
| Perceived stress at age 19 | 27.25 | 5.98 | 10.00 | 45.00 | — |
| Financial stress at age 19 | 10.81 | 2.91 | 4.00 | 16.00 | — |
| Family below poverty line at age 11, mean % | 43.10 | 49.58 | — | — | — |
| Family below poverty line at age 19, mean % | 54.76 | 49.83 | — | — | — |
| Male | — | — | — | — | 46.00 |
| Smoking at age 19 | — | — | — | — | 25.70 |
| Binge drinking at age 19 | — | — | — | — | 21.00 |
| Unemployment at age 19 | — | — | — | — | 66.20 |
| Neighborhood measures (census tract level), mean % | |||||
| Stayed in the same neighborhoods from 2000 to 2010 (n = 284; census tracts = 41) | |||||
| Below poverty (census 2000) | 21.45 | 7.41 | — | — | — |
| Below poverty (American Community Survey 2010) | 24.80 | 7.86 | — | — | — |
N = 420.
Results
Descriptive Statistics
Table 1 reveals descriptive statistics for the sample. Among the 420 participants, 284 nested in 41 census tracts remained in their childhood neighborhoods until 2010. Of these 41 census tracts, the mean proportion of households that in the aggregate were below the federal poverty level was 21.5% (SD = 7.4) in 2000 and 24.8% (SD = 7.9) in 2010. A paired t test revealed that neighborhood poverty rates in adolescence were significantly higher than in childhood.
Data Analyses
The data analyses are presented in Table 2. Model 1 was designed to identify the main effects of neighborhood poverty at ages 11 and 19 on AL. After adjustments for individual-level covariates, the results indicated that neighborhood poverty levels at age 19 predicted AL at age 19. An increase of 1 SD in neighborhood poverty in adolescence was associated with a 23% increase in AL, odds ratio = 1.23, P < .05. Family-level poverty at both time points, their interaction, the other covariates, and childhood neighborhood poverty were not related to AL. This analysis was re-executed (not shown in Table 2) to determine whether childhood neighborhood poverty forecast AL without current neighborhood poverty in the equation. Again, childhood neighborhood poverty did not forecast AL.
TABLE 2.
Multilevel Poisson Regression Models Using AL at Age 19 as the Outcome
| Model 1a | Model 2a | Model 3a | Model 4b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | P | B | SE | P | B | SE | P | B | SE | P | ||
| Constant | 0.21 | 0.42 | .63 | 0.26 | 0.43 | .55 | 0.21 | 0.43 | .63 | 0.37 | 0.35 | .29 | |
| Between-neighborhood | |||||||||||||
| Neighborhood poverty (2000) | −0.14 | 0.09 | .12 | −0.10 | 0.09 | .30 | −0.17 | 0.10 | .09 | −0.06 | 0.05 | .21 | |
| Neighborhood poverty (2010) | 0.20 | 0.10 | .05 | 0.17 | 0.10 | .09 | 0.17 | 0.10 | .10 | 0.08 | 0.05 | .11 | |
| NP (2000) × NP (2010) | −0.12 | 0.06 | .03 | −0.19 | 0.06 | .00 | −0.11 | 0.04 | .01 | ||||
| ES × NP (2000) | 0.20 | 0.09 | .04 | 0.08 | 0.06 | .17 | |||||||
| ES × NP (2010) | −0.07 | 0.10 | .49 | 0.03 | 0.05 | .61 | |||||||
| NP (2000) × NP (2010) × ES | 0.19 | 0.07 | .01 | 0.10 | 0.05 | .04 | |||||||
| Between-person | |||||||||||||
| Family poverty at age 11 | 0.17 | 0.11 | .13 | 0.13 | 0.18 | .46 | 0.14 | 0.18 | .45 | 0.05 | 0.15 | .72 | |
| Family poverty at age 19 | 0.03 | 0.12 | .79 | 0.01 | 0.16 | .93 | 0.02 | 0.16 | .89 | 0.01 | 0.12 | .93 | |
| FP (age 11) × FP (age 19) | 0.03 | 0.23 | .90 | 0.04 | 0.23 | .86 | 0.11 | 0.19 | .57 | ||||
| Emotional support at age 18 | −0.02 | 0.06 | .68 | −0.02 | 0.05 | .62 | |||||||
| Male | 0.08 | 0.10 | .44 | 0.10 | 0.11 | .36 | 0.13 | 0.11 | .24 | 0.11 | 0.09 | .20 | |
| Diet at age 19 | −0.01 | 0.03 | .89 | −0.01 | 0.03 | .98 | 0.01 | 0.03 | .86 | −0.01 | 0.02 | .56 | |
| Smoking at age 19 | −0.08 | 0.13 | .54 | −0.08 | 0.13 | .55 | −0.03 | 0.13 | .84 | −0.07 | 0.11 | .50 | |
| Binge drinking at age 19 | −0.08 | 0.14 | .57 | −0.03 | 0.14 | .83 | −0.05 | 0.14 | .74 | 0.02 | 0.11 | .86 | |
| Perceived stress at age 19 | −0.01 | 0.01 | .69 | −0.01 | 0.01 | .70 | −0.01 | 0.01 | .61 | −0.01 | 0.01 | .62 | |
| Unemployment at age 19 | 0.03 | 0.12 | .78 | 0.02 | 0.12 | .86 | −0.03 | 0.12 | .79 | 0.05 | 0.10 | .64 | |
| Financial stress at age 19 | 0.02 | 0.02 | .40 | 0.02 | 0.02 | .36 | 0.02 | 0.02 | .23 | 0.01 | 0.02 | .73 | |
| Residential stability | 0.03 | 0.09 | .73 | ||||||||||
| Random effect: | |||||||||||||
| τ (same census tract between 2000 and 2010) | 3.72e-07 | 8.00e-10 | 3.51e-11 | ||||||||||
| τ (2000 census tract) | 8.39e-06 | ||||||||||||
| τ (2010 census tract) | 4.1e-05 | ||||||||||||
| Deviance | 884.96 | 879.85 | 863.44 | 1289.64 | |||||||||
Neighborhood poverty and emotional support were standardized by z transformation. ES, emotional support; FP, family poverty; NP, neighborhood poverty.
Multilevel Poisson regression model with participants who evinced residential stability between 2000 and 2010, n(person) = 284 and n(neighborhood) = 41.
Cross-Classified Multilevel Poisson regression model with the inverse of a propensity score weighting with the entire sample, n(person) = 420, n(neighborhood 2000) = 48, and n(neighborhood 2010) = 88.
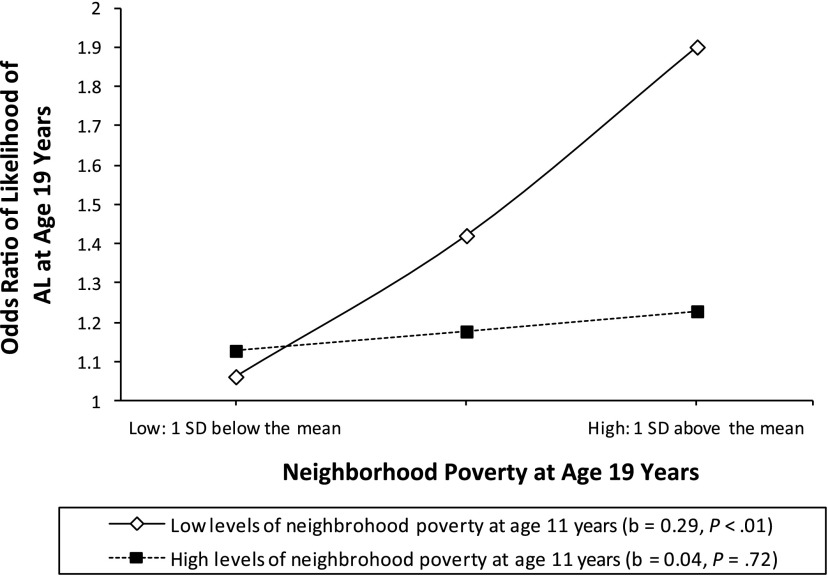
Model 2 estimated the contribution of changes in neighborhood poverty to AL. With the individual-level covariates, including family-level poverty status at ages 11 and 19 and their interaction controlled, the results of Model 2 revealed a significant interaction effect for neighborhood poverty at ages 11 and 19 on AL, odds ratio = 0.88, P < .05. To interpret the interaction of neighborhood poverty at 2000 and 2010, we plotted estimated AL at low (1 SD below the mean) and high (1 SD above the mean) levels of neighborhood poverty in adolescence. Low neighborhood poverty in childhood was also defined as 1 SD below the sample mean (−1 SD), and high neighborhood poverty in childhood was defined as 1 SD above the sample mean (+1 SD). As Fig 1 reveals, the highest levels of AL at age 19 occurred among African American youth who lived in low-poverty neighborhoods during childhood and high-poverty neighborhoods during adolescence (b = 0.21, P < .05). Thus, African American youth for whom neighborhood poverty levels increased over time evinced the highest AL levels, even when accounting for the individual-level covariates.
FIGURE 1.
The effects of neighborhood poverty at age 19 years on predicted AL by level of neighborhood poverty at age 11 years by using a multilevel Poisson regression model. The analysis controlled for family poverty, gender, diet, smoking, binge drinking, perceived stress, unemployment, and financial stress. The lines represent the regression lines for different levels of neighborhood poverty (low: 1 SD below the mean; high: 1 SD above the mean). Numbers in parentheses refer to simple slope test.
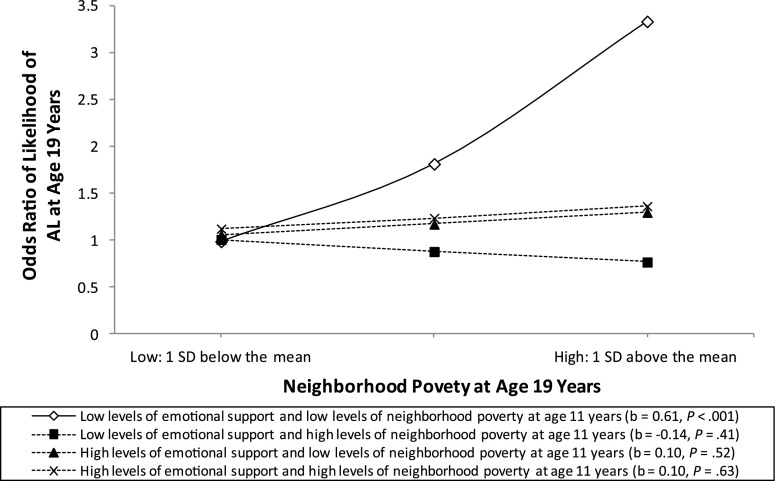
The protective effects of emotional support were addressed in Model 3 in Table 2. Emotional support was added to the multiplicative interaction of neighborhood poverty at 2000 and 2010 as a predictor of AL at age 19 while accounting for all the individual-level covariates. Consistent with the study hypothesis, this 3-way interaction was significant (odds ratio = 1.20, P < .05); Fig 2 illustrates the interaction effect. Figure 2 reveals that the highest levels of AL at age 19 emerged for youth who both lived in neighborhoods in which poverty levels increased across adolescence and received low levels of protective emotional support (b = 0.61, P < .001). Youth receiving high levels of emotional support did not evince an association between increases in neighborhood poverty and AL.
FIGURE 2.
The effect of neighborhood poverty at age 19 years on predicted AL by level of neighborhood poverty at age 11 years and emotional support by using a multilevel Poisson regression model. The analysis controlled for family poverty, gender, diet, smoking, binge drinking, perceived stress, unemployment, and financial stress. The lines represent the regression lines for different levels of neighborhood poverty (low: 1 SD below the mean; high: 1 SD above the mean) and emotional support (low: 1 SD below the mean; high: 1 SD above the mean). Numbers in parentheses refer to simple slope for each group.
The analysis presented in Model 3 was repeated by using a cross-classified multilevel Poisson model with propensity score weighting to adjust for selection out of age 11 neighborhoods. As depicted in Model 4, Table 2, the results of this analysis were identical to the ones depicted in Models 2 and 3, indicating that, after adjustments were made for potential selection biases and individual-level covariates, the study findings did not change.
Discussion
The current study is the first to examine the ways in which changes in neighborhood poverty are associated with AL. Rural African American youth who resided in a low-poverty neighborhood at age 11 and a high-poverty neighborhood at age 19 evinced the highest levels of AL. This finding persisted after we accounted for gender; family-level poverty status at age 11, at age 19, and their interaction; primary caregiver employment status; adolescent perceived stress; and youth diet, smoking, and alcohol use at age 19. The results also demonstrated the protective effects of emotional support from others in the adolescents’ social networks in ameliorating neighborhood effects on AL.
The results are consistent with previous literature that has identified protective effects of emotional support on physiologic responses to stress.13 Of relevance to pediatric clinical practice, efficacious family-centered prevention programs that are designed to enhance emotional support are available for rural African American children and youth.36 Participation in these programs has demonstrated stress-buffering effects on adolescent cytokine levels,37 catecholamine levels,38 and telomere lengths.39 Encouraging participation in prevention programs like these, along with helping children and adolescents living in high-poverty neighborhoods find a primary source of medical care, which pediatric health professionals term a medical home, could mitigate the effects of chronic neighborhood stress on AL.
The study findings signify that living in neighborhoods characterized by increasing levels of poverty has biological significance across multiple physiologic systems. At present, the mechanisms responsible for the neighborhood dynamics effects are unknown. Increasing exposure to crime, violence, and drug use, along with lack of safe recreational areas, transportation systems, and limited health care options are factors through which living in increasingly poor rural neighborhoods may influence AL.10 Future research should investigate whether exposure to increases in these neighborhood-level stressors account for this study’s findings.
Some aspects of the study constitute possible limitations. An expanded AL composite, covering additional physiologic systems that can be assessed by using blood draws, would be important for future research. Second, the study did not account for pubertal timing or development. Because assessments of pubertal maturation such as the Tanner scales40–42 are associated with sex steroid levels that influence neuroendocrine responses to stress,43 the inclusion of Tanner assessments in future research may facilitate more refined conclusions about neighborhood poverty and AL. Third, the use of inverse probability of treatment weighting to minimize selection bias does not rule out selection bias entirely; precision will increase as additional factors are measured and included. Fourth, it is not known whether the results of this study are generalizable to urban African Americans or to individuals of other ethnicities living in either rural or urban communities. Finally, although we accounted for a range of individual-level covariates, others, such as major life events and acute financial occurrences, should be included in future research. Despite these limitations, the study provides evidence that living in neighborhood environments that become poorer over time is reflected in rural African American youths’ AL, but only when they do not receive high levels of emotional support.
Conclusions
The results of this study reveal that AL, a measure of cardiometabolic risk, is associated with living, across childhood and adolescence, in neighborhoods in which poverty levels increase. This association did not emerge when youth received high levels of emotional support. This underscores the importance of relational support to youths’ stress reactivity.
Glossary
- AL
allostatic load
- SES
socioeconomic status
Footnotes
Dr Brody conceptualized and designed the analysis, drafted and revised the manuscript, approved the final manuscript as submitted, and takes full responsibility for the final submission; Dr Lei conceptualized and conducted the data analyses, made substantial intellectual contributions to the manuscript, and critically reviewed the manuscript; Drs Chen and Miller made substantial intellectual contributions to the manuscript and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by NIH grants R01 HD030588 and P30 DA027827. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137(6):959–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259 [DOI] [PubMed] [Google Scholar]
- 3.McEwen BS. Sex, stress and the hippocampus: allostasis, allostatic load and the aging process. Neurobiol Aging. 2002;23(5):921–939 [DOI] [PubMed] [Google Scholar]
- 4.Sterling P, Eyer J. Allostasis: a new paradigm to explain arousal pathology. In: Fisher S, Reason J, eds. Handbook of Life Stress, Cognition and Health. Oxford, UK: Wiley; 1988:629–649 [Google Scholar]
- 5.Theall KP, Drury SS, Shirtcliff EA. Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. Am J Epidemiol. 2012;176(suppl 7):S164–S174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juster R-P, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16 [DOI] [PubMed] [Google Scholar]
- 7.McCaffery JM, Marsland AL, Strohacker K, Muldoon MF, Manuck SB. Factor structure underlying components of allostatic load. PLoS ONE. 2012;7(10):e47246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA. 2001;98(8):4770–4775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68(3):500–507 [DOI] [PubMed] [Google Scholar]
- 10.Braveman P, Egerter S. Overcoming Obstacles to Health. Princeton, NJ: Robert Wood Johnson Foundation; 2008 [Google Scholar]
- 11.Chen E, Miller GE, Kobor MS, Cole SW. Maternal warmth buffers the effects of low early-life socioeconomic status on pro-inflammatory signaling in adulthood. Mol Psychiatry. 2011;16(7):729–737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evans GW, Kim P, Ting AH, Tesher HB, Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev Psychol. 2007;43(2):341–351 [DOI] [PubMed] [Google Scholar]
- 13.Chen E, Miller GE. “Shift-and-persist” strategies: why low socioeconomic status isn’t always bad for health. Perspect Psychol Sci. 2012;7(2):135–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brody GH, Yu T, Chen YF, et al. Cumulative socioeconomic status risk, allostatic load, and adjustment: a prospective latent profile analysis with contextual and genetic protective factors. Dev Psychol. 2013;49(5):913–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams RE, Santo JB, Bukowski WM. The presence of a best friend buffers the effects of negative experiences. Dev Psychol. 2011;47(6):1786–1791 [DOI] [PubMed] [Google Scholar]
- 16.Proctor BD, Dalaker J. Poverty in the United States: 2002 (Current Population Reports, P60-222). Washington, DC: US Census Bureau; 2003 [Google Scholar]
- 17.Brody GH, Murry VM, Gerrard M, et al. The Strong African American Families program: translating research into prevention programming. Child Dev. 2004;75(3):900–917 [DOI] [PubMed] [Google Scholar]
- 18.US Census Bureau. American Community Survey information guide. Washington, DC: US Census Bureau; 2013
- 19.Evans GW. A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev Psychol. 2003;39(5):924–933 [DOI] [PubMed] [Google Scholar]
- 20.Evans GW, Kim P. Childhood poverty and young adults’ allostatic load: the mediating role of childhood cumulative risk exposure. Psychol Sci. 2012;23(9):979–983 [DOI] [PubMed] [Google Scholar]
- 21.Doan SN, Dich N, Evans GW. Childhood cumulative risk and later allostatic load: mediating role of substance use [published online ahead of print November 25, 2013]. Health Psychol. doi:10.1037/a0034790 [DOI] [PubMed] [Google Scholar]
- 22.Kamarck TW, Jennings JR, Debski TT, et al. Reliable measures of behaviorally-evoked cardiovascular reactivity from a PC-based test battery: results from student and community samples. Psychophysiology. 1992;29(1):17–28 [DOI] [PubMed] [Google Scholar]
- 23.Contreras LN, Hane S, Tyrrell JB. Urinary cortisol in the assessment of pituitary-adrenal function: utility of 24-hour and spot determinations. J Clin Endocrinol Metab. 1986;62(5):965–969 [DOI] [PubMed] [Google Scholar]
- 24.Riggin RM, Kissinger PT. Determination of catecholamines in urine by reverse-phase liquid chromatography with electrochemical detection. Anal Chem. 1977;49(13):2109–2111 [DOI] [PubMed] [Google Scholar]
- 25.Tietz NW, ed. Fundamentals of Clinical Chemistry. 2nd ed. Philadelphia, PA: Saunders; 1976 [Google Scholar]
- 26.Seeman TE, Singer BH, Ryff CD, Dienberg Love G, Levy-Storms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med. 2002;64(3):395–406 [DOI] [PubMed] [Google Scholar]
- 27.Wills TA, Blechman EA, McNamara G. Family support, coping, and competence. In: Hetherington EM, Blechman EA, eds. Stress, Coping, and Resiliency in Children and Families. Mahwah, NJ: Erlbaum; 1996:107–133 [Google Scholar]
- 28.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283 [DOI] [PubMed] [Google Scholar]
- 29.Kogan SM, Brody GH, Chen YF. Natural mentoring processes deter externalizing problems among rural African American emerging adults: a prospective analysis. Am J Community Psychol. 2011;48(3-4):272–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Conger RD, Elder GH., Jr Families in Troubled Times: Adaptation to Change in Rural America. New York, NY: Aldine de Gruyter; 1994 [Google Scholar]
- 31.Youth Risk Behavior Surveillance System Youth Risk Behavior Survey. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2009 [Google Scholar]
- 32.Taylor SE, Seeman TE. Psychosocial resources and the SES-health relationship. Ann N Y Acad Sci. 1999;896(1):210–225 [DOI] [PubMed] [Google Scholar]
- 33.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modelling Using Stata. 2nd ed. College Station, TX: Stata Press; 2008 [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79(387):516–524 [Google Scholar]
- 35.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55 [Google Scholar]
- 36.Brody GH, Kogan SM, Grange CM. Translating longitudinal, developmental research with rural African American families into prevention programs for rural African American youth. In: King RB, Maholmes V, eds. The Oxford Handbook of Poverty and Child Development. New York, NY: Oxford University Press; 2012:553–570 [Google Scholar]
- 37.Miller GE, Brody GH, Yu T, Chen E. A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proc Natl Acad Sci USA. 2014;111(31):11287–11292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brody GH, Yu T, Chen E, Miller GE. Prevention moderates associations between family risks and youth catecholamine levels [published online ahead of print March 3, 2014]. Health Psychol. doi:10.1037/hea0000072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brody GH, Yu T, Beach SRH, Philibert RA. Prevention effects ameliorate the prospective association between nonsupportive parenting and diminished telomere length [published online ahead of print March 6, 2014]. Prev Sci. 2014. doi:10.1007/s11121-014-0474-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanner JM. Growth at Adolescence. 2nd ed. Oxford, UK: Blackwell; 1962 [Google Scholar]
- 41.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45(239):13–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434–445 [DOI] [PubMed] [Google Scholar]