Abstract
OBJECTIVE:
We sought to determine the prevalence of initial computed tomography (CT) utilization and to identify regions in the United States where CT is highly used as the first imaging study for children with nephrolithiasis.
METHODS:
We performed a cross-sectional study in 9228 commercially insured children aged 1 to 17 years with nephrolithiasis who underwent diagnostic imaging in the United States between 2003 and 2011. Data were obtained from MarketScan, a commercial insurance claims database of 17 827 229 children in all 50 states. We determined the prevalence of initial CT use, defined as CT alone or CT performed before ultrasound in the emergency department, inpatient unit, or outpatient clinic, and identified regions of high CT utilization by using logistic regression.
RESULTS:
Sixty-three percent of children underwent initial CT study and 24% had ultrasound performed first. By state, the proportion of children who underwent initial CT ranged from 41% to 79%. Regional variations persisted after adjusting for age, gender, year of presentation, and insurance type. Relative to children living in West South Central states, the highest odds of initial CT utilization were observed for children living in the East South Central US Census division (odds ratio: 1.27; 95% confidence interval: 1.06–1.54). The lowest odds of initial CT were observed for children in the New England states (odds ratio: 0.48; 95% confidence interval: 0.38–0.62).
CONCLUSIONS:
Use of CT as the initial imaging study for children with nephrolithiasis is highly prevalent and shows extensive regional variability in the United States. Current imaging practices deviate substantially from recently published guidelines that recommend ultrasound as the initial imaging study.
Keywords: nephrolithiasis, computed tomography, ultrasound, children
What’s Known on This Subject:
Professional organizations recommend ultrasound as the initial diagnostic imaging modality for children with suspected nephrolithiasis. Computed tomography utilization for children with nephrolithiasis treated at freestanding children’s hospitals is common and varies substantially by hospital.
What This Study Adds:
The high prevalence and regional variability of CT as the first imaging study for children with nephrolithiasis who presented to emergency departments, outpatient clinics, and hospitals throughout the United States indicate that current imaging practices deviate substantially from guidelines.
Computed tomography (CT) localizes kidney stones with 96% sensitivity and 100% specificity.1 However, CT delivers ionizing radiation, which is associated with an increased risk of cancer, particularly in children.2–4 Because of concern for medical radiation exposure among children with kidney stones, the American Urological Association and the European Society of Pediatric Radiology developed imaging recommendations for children with suspected nephrolithiasis. Both organizations recommend using ultrasound as the initial imaging study for children with suspected kidney stones and reserving CT when ultrasound is nondiagnostic and suspicion of stones remains high.5,6 Additionally, the Image Gently Alliance, a consortium of radiologic professional societies, began its campaign in 2007 to lower radiation exposure among children who need diagnostic imaging.7,8
Currently, CT is the imaging modality used most commonly to evaluate children with nephrolithiasis9,10 and abdominal pain11 in the United States. Within the Pediatric Hospital Information System (PHIS), the hospital where the child is seen is the strongest predictor of imaging modality choice,9 which suggests that there is undesirable variation in imaging utilization for children with nephrolithiasis in the United States.12 However, previous studies did not determine the order in which imaging studies were obtained. Additionally, it is possible that these results are not generalizable to practices at non–children’s hospitals or children’s hospitals not in PHIS. To determine how current imaging practices at all types of US clinics and hospitals deviate from recently published guidelines, we determined the prevalence of initial CT utilization and identified US regions where CT is highly used as the first imaging study for children with nephrolithiasis. We hypothesized that there is regional variability in initial CT utilization for children with nephrolithiasis that is not explained by patient characteristics or by trends in CT utilization. We also examine temporal trends of overall utilization of CT, ultrasound, kidney, ureter, and bladder x-ray (KUB), intravenous pyelogram (IVP), and MRI at any point during a kidney stone episode.
Methods
Data Source
We conducted this study in MarketScan (Truven Health Analytics, Ann Arbor, Michigan), which includes patients enrolled in >100 nongovernmental health insurance plans in all states. MarketScan contains longitudinal patient-level data for inpatient, outpatient, and procedure claims from all types of hospitals and clinics where patients received care. The databases contain patient demographics, zip code of residence, dates of services, International Classification of Diseases, Ninth Revision, diagnostic codes, and Common Procedural Terminology codes.
Study Design
We performed a cross-sectional study in 17 827 229 children in MarketScan aged 1 to 17 years with at least 1 full calendar year of continuous medical benefits between 2003 and 2011. We identified patients with stone events among this population by using International Classification of Diseases, Ninth Revision, and Common Procedural Terminology codes for nephrolithiasis and stone procedures, respectively.13 A patient must have met at least 1 of the following criteria to be considered to have a kidney stone: (1) ≥2 primary diagnosis codes for nephrolithiasis in the outpatient setting <180 days apart or a primary diagnosis in the emergency department (ED), (2) surgical procedures for nephrolithiasis, and/or (3) stone diagnoses in the inpatient setting. We chose these criteria to maximize specificity of identifying clinically important new stone events and minimize misclassifying care received for a previous history of nephrolithiasis as a kidney stone event. For patients with kidney stones, we defined the duration of the kidney stone episode to extend from 1 month before to 6 months after the first kidney stone claim to capture the initial diagnosis, treatment, and follow-up imaging that would be obtained after spontaneous stone passage or surgical removal.9,14
We identified all ultrasound, CT, KUB, IVP, and MRI performed during the kidney stone episode by using imaging billing codes. The order of imaging was defined by the imaging claim dates. Outcomes among unique individuals with >1 kidney stone event during the study period were limited to the earliest occurrence.
Outcome Definition
The primary outcome was the use of CT as the first imaging study during the kidney stone episode. Initial CT was defined as CT alone or CT performed before ultrasound in the ED, inpatient unit, or outpatient clinic. Ultrasounds were classified as the initial imaging study when they had the same claim date as a CT.
The secondary outcome was overall use of CT, ultrasound, KUB, IVP, and MRI at any point within the kidney stone episode irrespective of the order in which it was obtained.
Predictor Variable and Covariates
The primary predictor of initial CT utilization was geographic location. We analyzed location as the US Census division15 and state of the patient’s residence to allow assessment of variation in CT utilization within and across regions. Covariates included age, gender, year of presentation, and insurance type. Age was defined into 3 strata (2–5 years, 6–11 years, and 12–17 years) to reflect early childhood, prepubescence, and adolescence. Insurance type included the following: exclusive provider organization, health maintenance organization, point of service, preferred provider organization with and without capitation, consumer-driven health plans, and point of service. Race and ethnicity were missing for more than half the patients in MarketScan and thus were not evaluated.
Statistical Analysis
We estimated the odds of initial CT utilization for each census division by using logistic regression. We built 2 models to estimate the proportion of geographic variability explained by patient characteristics. The base model included the 9 divisions and indicator variables for year of presentation to adjust for temporal trends in CT utilization. The second, fully adjusted model, included age, gender, year of presentation, and insurance type to adjust a priori for patient characteristics that may be independently associated with CT utilization.
All variables were analyzed as categorical variables. Year of presentation was analyzed as a categorical variable to avoid the assumption that changes in imaging utilization were equal between calendar years. Insurance types were collapsed on the basis of similarities in coverage and plan structure. The insurance categories included in the models were exclusive provider organization, health maintenance organization, consumer-driven or high-deductible health care plans, point of service, and preferred provider organization. The proportion of children who underwent CT scan as the first imaging study during a kidney stone episode was mapped by state. We excluded states in which <10 children had kidney stones during the study period due to potential imprecise estimates of CT utilization.
Analyses were performed in patients for whom complete data were available by using SAS 9.2 (SAS Institute, Cary, NC). Tests were 2-sided, and P < .05 was the threshold for statistical significance. This study was exempt from institutional review board approval per Department of Health and Human Services regulation 45 CFR 46.101, category 4.
Results
From 2003 to 2011, 17 827 229 children were included in MarketScan and 9642 children had codes for nephrolithiasis that met criteria for a kidney stone episode. Of these, 9228 children (96%) had imaging studies during a stone episode (Table 1). We excluded Vermont, Rhode Island, North Dakota, South Dakota, Wyoming, and Alaska because <10 children living in these states had stones during the study period.
TABLE 1.
Characteristics of Children With Nephrolithiasis Who Underwent Diagnostic Imaging in the United States from 2003 to 2011
| Total Pediatric Population in MarketScan (N = 17 827 229) | Children With Nephrolithiasis Who Underwent Imaging (N = 9228) | |
|---|---|---|
| Median age, y (IQR) | 10 (6–14) | 15 (12–17) |
| Gender, n (%) | ||
| Male | 9 111 328 (51.1) | 3834 (41.5) |
| Female | 8 715 901 (48.9) | 5394 (58.5) |
| Plan type, n (%) | ||
| POS | 1 578 897 (8.9) | 976 (10.6) |
| CDHP/HDHP | 863 370 (4.8) | 418 (4.5) |
| PPO | 11 749 236 (65.9) | 6302 (68.3) |
| EPO | 217 788 (1.2) | 118 (1.3) |
| HMO | 3 417 938 (19.2) | 1414 (15.3) |
CDHP, consumer-driven health plan; EPO, exclusive provider organization; HDHP, high-deductible health plan; HMO, health maintenance organization; IQR, interquartile range; POS, point of service; PPO, preferred provider organization.
Utilization of CT as the Initial Imaging Study
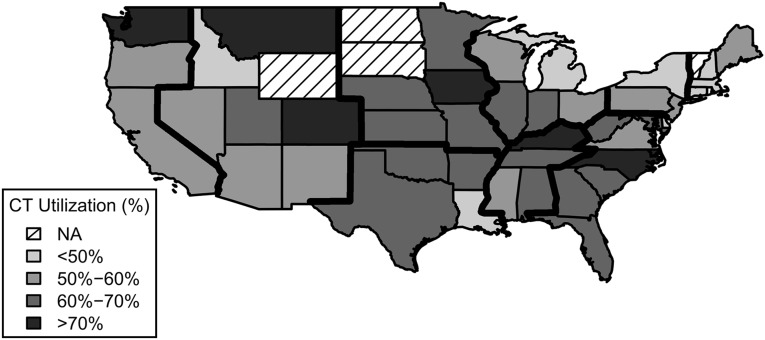
From 2003 to 2011, an average of 63% of children in the United States underwent CT as the first imaging study during a kidney stone episode. By state, the proportion of children who underwent initial CT during a kidney stone episode varied from 41% to 79% (Fig 1). Averaged over the study period, 24% underwent ultrasound as the first imaging study. KUB and IVP comprised the remaining 13% of initial imaging studies.
FIGURE 1.
Geographic variability in utilization of CT as the first imaging study for children with nephrolithiasis in the United States from 2003 to 2011. Census divisions are outlined by thick dark lines. NA, not applicable due to low prevalence of kidney stones.
The final model included census division, age, gender, year of presentation, and insurance type (Table 2). The odds of initial CT utilization associated with census divisions were similar between the base and fully adjusted models. The inclusion of patient characteristics changed the odds ratios (ORs) from the base model by <3% for any division.
TABLE 2.
Association Between Census Division, Patient Characteristics, and Utilization of CT as the First Imaging Study for Children With Nephrolithiasis
| Base Model | Fully Adjusted Model | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Census division | ||||
| South region | ||||
| West South Central | Referent | Referent | Referent | Referent |
| East South Central | 1.30* | 1.09–1.56 | 1.27* | 1.06–1.54 |
| South Atlantic | 0.96 | 0.84–1.10 | 0.93 | 0.80–1.07 |
| Northeast Region | ||||
| New England | 0.50* | 0.40–0.64 | 0.48* | 0.37–0.62 |
| Middle Atlantic | 0.70* | 0.58–0.84 | 0.69* | 0.57–0.83 |
| Midwest region | ||||
| East North Central | 0.97 | 0.84–1.12 | 0.95 | 0.81–1.10 |
| West North Central | 1.24 | 0.99–1.54 | 1.22 | 0.98–1.53 |
| West region | ||||
| Mountain | 0.86 | 0.68–1.09 | 0.86 | 0.68–1.10 |
| Pacific | 0.69* | 0.57–0.82 | 0.71* | 0.59–0.86 |
| Year of evaluation | ||||
| 2003 | Referent | Referent | Referent | Referent |
| 2004 | 1.19 | 0.89–1.60 | 1.18 | 0.88–1.60 |
| 2005 | 1.36* | 1.03–1.79 | 1.30 | 0.98–1.73 |
| 2006 | 1.62* | 1.22–2.14 | 1.59* | 1.19–2.12 |
| 2007 | 1.68* | 1.29–2.19 | 1.62* | 1.23–2.13 |
| 2008 | 1.44* | 1.11–1.86 | 1.42* | 1.09–1.86 |
| 2009 | 1.40* | 1.09–1.80 | 1.35* | 1.04–1.76 |
| 2010 | 1.23 | 0.96–1.56 | 1.19 | 0.91–1.54 |
| 2011 | 1.01 | 0.79–1.3 | 0.96 | 0.74–1.24 |
| Age | ||||
| 2–5 years | Referent | Referent | ||
| 6–11 years | 3.68* | 2.81–4.81 | ||
| 12–17 years | 8.61* | 6.66–11.13 | ||
| Gender | ||||
| Male | Referent | Referent | ||
| Female | 1.13* | 1.03–1.24 | ||
| Insurance type | ||||
| HMO | Referent | Referent | ||
| POS | 1.15 | 0.96–1.38 | ||
| PPO | 1.11 | 0.98–1.26 | ||
| EPO | 0.83 | 0.57–1.24 | ||
| CDHP/HDHP | 1.15 | 0.90–1.46 | ||
West South Central: Arkansas, Louisiana, Oklahoma, and Texas; East South Central: Alabama, Kentucky, Mississippi, and Tennessee; South Atlantic: Delaware, District of Columbia, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, and West Virginia; New England: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont; Middle Atlantic: New Jersey, New York, and Pennsylvania; East North Central: Illinois, Indiana, Michigan, Ohio, and Wisconsin; West North Central: Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota; Mountain: Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, and Wyoming; Pacific: Alaska, California, Hawaii, Oregon, and Washington. *P < .05. CDHP, consumer-driven health plan; EPO, exclusive provider organization; HDHP, high-deductible health plan; HMO, health maintenance organization; POS, point of service; PPO, preferred provider organization.
Relative to the West South Central US Census division (Arkansas, Louisiana, Oklahoma, and Texas), the highest odds of initial CT utilization were observed for children living in the East South Central division (Alabama, Kentucky, Mississippi, and Tennessee; OR: 1.27; 95% confidence interval [CI]: 1.06–1.54). The lowest odds of initial CT were observed for children in New England states (Connecticut, Maine, Massachusetts, and New Hampshire; OR: 0.48; 95% CI: 0.38–0.62).
Older children were more likely to undergo initial CT. Adolescents were nearly 9 times more likely to undergo initial CT than were 2- to 5-year-olds (OR: 8.75; 95% CI: 6.78–11.30). Girls were more likely to undergo CT than boys (OR: 1.13; 95% CI: 1.03–1.23). There was no significant association between initial CT utilization and insurance type.
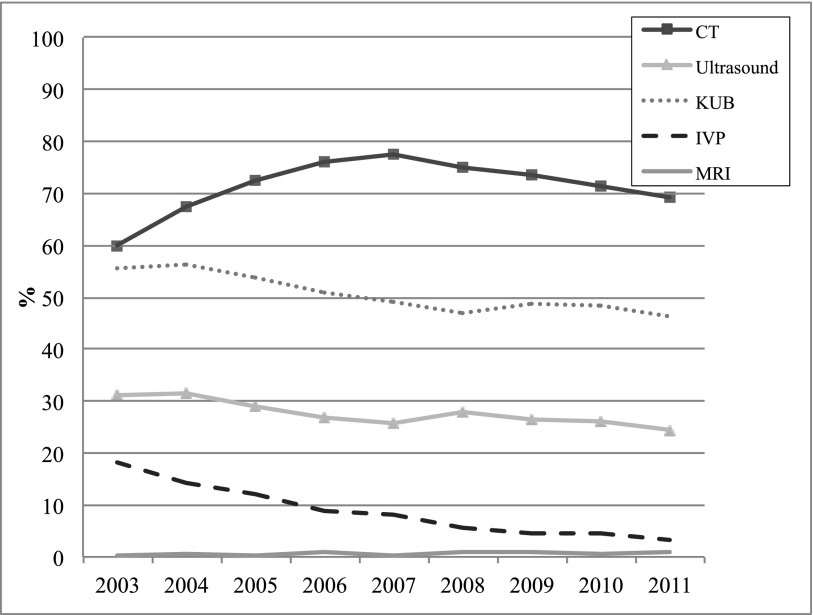
Overall Diagnostic Imaging Utilization
CT was the imaging study ordered most frequently during a stone episode. Across the United States, CT use anytime during the kidney stone episode increased from 60% in 2003 to 77% in 2007, and then gradually declined. Overall ultrasound utilization during a stone episode remained stable at 24% to 31% throughout the study period. IVP use decreased steadily and, by 2011, only 3% of children with nephrolithiasis were evaluated with IVP at any point during the stone episode (Fig 2).
FIGURE 2.
Proportion of children evaluated by CT, ultrasound, KUB, IVP, and MRI during a kidney stone episode between 2003 and 2011. Utilization of diagnostic imaging modalities is not mutually exclusive. KUB, .
Discussion
In this cross-sectional study that included clinics and hospitals throughout the United States, CT was the most frequently ordered initial imaging study for children during a kidney stone episode. On average, >60% of children had CT as the initial imaging study during a kidney stone episode. In some states, nearly 80% of children underwent CT as the first or only imaging study. Girls, in whom abdominal and pelvic radiation has a higher lifetime attributable risk of cancer than boys, were more likely to have CT.16 Only 24% of children with nephrolithiasis underwent ultrasound as the initial study. The high prevalence of initial CT and low prevalence of ultrasound indicate that current imaging practices deviate substantially from recently published guidelines that recommend ultrasound as the first imaging study for children with suspected nephrolithiasis.
The rationale for using ultrasound as the initial screening modality for children with suspected nephrolithiasis is that ultrasound accurately localizes most clinically important stones in children17,18 and CT can be reserved for children with a nondiagnostic ultrasound for whom the clinical suspicion for stones remains high. Passerotti et al18 observed that the sensitivity and specificity of ultrasound for 50 children with suspected nephrolithiasis were 70% and 100%, respectively, when compared with CT. Of the stones not visualized on ultrasound, 25% were in the ureter and the remainder were nonobstructive stones in the kidney. Prompted by the good sensitivity of ultrasound in detecting clinically significant stones, the radiation risk associated with CT, and the low diagnostic yield for alternative diagnoses,19 the American Urological Association in 2013 and the European Society for Pediatric Radiology in 2009 developed imaging protocols for children with suspected nephrolithiasis that recommend CT only if an initial ultrasound is nondiagnostic.5,6 The Image Gently Alliance7,8 also recommends limiting radiation when possible and promotes alternative imaging modalities such as ultrasound for children who need diagnostic imaging.
Ideally, this study should be conducted in children in whom nephrolithiasis is suspected before obtaining imaging rather than those found to have stones after imaging. Unfortunately, we cannot identify these patients with the use of claims data. Given that use of CT in the ED for abdominal pain, which is the most common presenting symptom for kidney stones,20 also varies substantially by region,11 it is unlikely that the imaging patterns we identified would differ significantly among children in whom nephrolithiasis is suspected but not confirmed. However, because CTs in this study may have been obtained to evaluate for kidney stones or other conditions on the differential diagnosis (eg, ovarian torsion, ureteropelvic junction obstruction), the diagnostic yield of CT to identify kidney stones and alternative diagnoses in children with abdominal and/or flank pain should be considered. Persaud et al20 reported that most children (72%; 244 of 339) who underwent helical CT for suspected nephrolithiasis did not have stones. Furthermore, few (9%) of 244 children without stones had clinically important alternative diagnoses identified by CT. Eshed and Witzling19 also evaluated the diagnoses of children with abdominal pain and suspicion for ureteral stones who underwent CT. In 20 children suspected to have nephrolithiasis, 3 were found to have stones as the source of the pain and CT confirmed an alternative diagnosis in only 4 more. Of note, the alternative diagnoses were lobar nephronia, ureteropelvic junction obstruction, ovarian torsion, and dermoid cyst, all of which can be identified by using ultrasound.
The public health implications of the high prevalence of initial CT use are heightened by the rising incidence of kidney stones among children. Over the past 25 years, the incidence of nephrolithiasis among adolescents has increased by 6% to 10% annually.21,22 The potential harms of radiation are further increased for patients with nephrolithiasis because multiple imaging studies are often performed for the same kidney stone episode. Alarmingly, Routh and co-workers demonstrated that 79% of children had ≥2 CTs for each stone episode treated at PHIS hospitals, with some children undergoing 8 CTs.9 Furthermore, some patients in whom nephrolithiasis begins in childhood will receive additional imaging for recurrent stones and will be exposed to radiation during surgical treatment, both of which increase lifetime radiation doses.9,23,24
We observed substantial geographic variability in initial CT utilization across the United States. Midwestern and southern states had the highest initial CT utilization, and the northeast states had the lowest initial CT utilization. However, even in states where initial CT use was relatively low, >40% of children underwent CT alone or CT before ultrasound. The observed regional variation was not due to differences in patient characteristics or temporal trends in CT utilization because adjustment for age, gender, year of presentation, and type of insurance resulted in very small and statistically insignificant changes in the association between geographic location and CT utilization. We also observed heterogeneity of initial CT utilization within census divisions. For example, within the Pacific division, California had relatively low CT utilization whereas 77% of children living in Washington underwent CT as the first imaging study. Generally, however, there was greater variation in CT utilization across versus within divisions. These results may help focus efforts to disseminate and implement imaging guidelines in areas of the country with high rates of initial CT use.
Variability in initial CT utilization is analogous to observed regional differences in per capita Medicare spending,25,26 which has been attributed to geographic differences in physician evaluation and management practices. Similar to variations in diabetes care among adults,27 we hypothesize that CT use to evaluate children with nephrolithiasis differs across the country due to engrained practice patterns or resources specific to local medical communities. Ultrasound may be less available in certain areas and some practitioners may be less comfortable with ultrasound evaluation given its operator and interpreter dependence. Additionally, it is possible that different specialists involved in the management of children with nephrolithiasis (eg, ED physicians versus pediatric urologists) may be more or less likely to order CT as the initial imaging study. Accordingly, geographic differences in the prevalence of specialists across the country may contribute to the variability in initial CT utilization we observed. An ancillary hypothesis is that the rapidly changing epidemiology of nephrolithiasis22,28,29 has contributed to wide variations in practices. Because CT is traditionally used to evaluate adults with suspected nephrolithiasis, many physicians may not be aware that ultrasound can be used to effectively diagnose kidney stones in children, who are now presenting with nephrolithiasis with increasing frequency.
Clinical guidelines have been shown to reduce variability and improve processes of care as well as outcomes.30 Future studies should assess awareness of these guidelines and determine the physician, institutional, and community characteristics that serve as barriers to implementation of recommended imaging practices. Additionally, interventions to decrease initial CT use should be developed. Miller et al31 established a collaborative network of urology practices to improve compliance with national guidelines on diagnostic imaging use for men with prostate cancer. They observed that providing data back to urologists on their imaging practices reduced inappropriate imaging utilization.32 Additionally, the Centers for Medicare and Medicaid Services Physician Quality Reporting System uses quality of care measures related to overuse of imaging in staging men with localized prostate cancer. Similar measures for overuse of CT imaging in children with nephrolithiasis could be developed and used by private payors, perhaps in the setting of hospitals participating in accountable care organizations established by these payors. Finally, systems that integrate clinical decision support into computerized order entry systems to provide evidence for or against imaging studies at the time of order entry may facilitate implementation of these measures.
We acknowledge the limitations to this study. First, we used claims dates to determine the order of imaging and claims. Misclassification of study order may exist because claims are not necessarily made on the day of service and 16% of imaging studies in this study had the same claims date. However, to mitigate bias, we classified all ultrasounds with the same claim date as a CT, IVP, or KUB as the first imaging study performed. It is also unlikely that any discrepancy between the claims date and date of service would alter our results given that ultrasound would rarely, if ever, be performed after CT for kidney stones. Second, as described previously, we were not able to determine imaging utilization for children for whom nephrolithiasis was suspected but who were ultimately found not to have stones. Third, we were not able to differentiate recurrent stones from incident stones. It is possible that ultrasound may be used more often as a screening study for children with a history of nephrolithiasis. However, this possibility should not affect our results unless recurrence rates differ by geographic region. Fourth, we were unable to measure race and socioeconomic level, which have been associated with the probability of nephrolithiasis and thus could influence the choice of initial imaging. However, it is unlikely that any association between race and socioeconomic level and CT utilization could explain the large geographic variability we observed. Finally, although MarketScan contains data from all 50 states, it is a sample of the population with commercial insurance and does not represent the overall population. Our results should not be extrapolated to uninsured or Medicaid/Medicare-insured subjects.
Conclusions
The use of CT as the initial imaging study for children with kidney stones is common and shows extensive regional variability in the United States. This finding indicates that current imaging practices deviate substantially from recently published guidelines that recommend ultrasound as the initial imaging study.
Glossary
- CI
confidence interval
- CT
computed tomography
- ED
emergency department
- IVP
intravenous pyelogram
- OR
odds ratio
- PHIS
Pediatric Hospital Information System
Footnotes
Dr Tasian conceptualized and designed the study, performed the data analysis, drafted the initial manuscript, revised the manuscript, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis; Dr Pulido conceptualized and designed the study, assisted in the data analysis, and revised the initial manuscript; Dr Keren assisted in the interpretation of data and reviewed and revised the manuscript; Drs Dick and Setodji assisted in the design of the study and data analysis and reviewed and revised the manuscript; Ms Hanley and Mr Madison assisted in the design of the study and performed and assisted in the data analysis; Dr. Saigal assisted in the design of the study and the interpretation of data and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
The National Institutes of Health provided financial support for data management and analysis but had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The views expressed in this article are those of the authors and do necessarily represent the official view of the National Institute of Diabetes and Digestive and Kidney Diseases.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Tasian was supported by National Institutes of Health grant T32HD060550. The analysis was funded by grant HHSN276201200016C from the National Institute of Diabetes and Digestive and Kidney Diseases. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Poletti PA, Platon A, Rutschmann OT, Schmidlin FR, Iselin CE, Becker CD. Low-dose versus standard-dose CT protocol in patients with clinically suspected renal colic. AJR Am J Roentgenol. 2007;188(4):927–933 [DOI] [PubMed] [Google Scholar]
- 2.Smith RC, Coll DM. Helical computed tomography in the diagnosis of ureteric colic. BJU Int. 2000;86(suppl 1):33–41 [DOI] [PubMed] [Google Scholar]
- 3.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078–2086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz SI, Saluja S, Brink JA, Forman HP. Radiation dose associated with unenhanced CT for suspected renal colic: impact of repetitive studies. AJR Am J Roentgenol. 2006;186(4):1120–1124 [DOI] [PubMed] [Google Scholar]
- 5.Fulgham PF, Assimos DG, Pearle MS, Preminger GM. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J Urol. 2013;189(4):1203–1213 [DOI] [PubMed] [Google Scholar]
- 6.Riccabona M, Avni FE, Blickman JG, et al. Imaging recommendations in paediatric uroradiology. Minutes of the ESPR uroradiology task force session on childhood obstructive uropathy, high-grade fetal hydronephrosis, childhood haematuria, and urolithiasis in childhood. ESPR Annual Congress, Edinburgh, UK, June 2008. Pediatr Radiol. 2009;39(8):891–898 [DOI] [PubMed] [Google Scholar]
- 7.Goske MJ, Applegate KE, Boylan J, et al. The Image Gently campaign: working together to change practice. AJR Am J Roentgenol. 2008;190(2):273–274 [DOI] [PubMed] [Google Scholar]
- 8.Goske MJ, Applegate KE, Boylan J, et al. The ‘Image Gently’ campaign: increasing CT radiation dose awareness through a national education and awareness program. Pediatr Radiol. 2008;38(3):265–269 [DOI] [PubMed] [Google Scholar]
- 9.Routh JC, Graham DA, Nelson CP. Trends in imaging and surgical management of pediatric urolithiasis at American pediatric hospitals. J Urol. 2010;184(4 suppl):1816–1822 [DOI] [PubMed] [Google Scholar]
- 10.Johnson EK, Graham DA, Chow JS, Nelson CP. Nationwide emergency department imaging practices for pediatric urolithiasis: room for improvement. J Urol. 2014. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fahimi J, Herring A, Harries A, Gonzales R, Alter H. Computed tomography use among children presenting to emergency departments with abdominal pain. Pediatrics. 2012;130(5). Available at: www.pediatrics.org/cgi/content/full/130/5/e1069 [DOI] [PubMed] [Google Scholar]
- 12.Wennberg DE. Variation in the delivery of health care: the stakes are high. Ann Intern Med. 1998;128(10):866–868 [DOI] [PubMed] [Google Scholar]
- 13.Litwin M, Saigal C. Urinary tract stones. In: National Institute of Diabetes and Digestive and Kidney Diseases , ed. US Department of Health and Human Services PHS, National Institutes of Health. Washington, DC: US Government Printing Office; 2012:314–315 [Google Scholar]
- 14.Wang HH, Huang L, Routh JC, Nelson CP. Shock wave lithotripsy vs ureteroscopy: variation in surgical management of kidney stones at freestanding children’s hospitals. J Urol. 2012;187(4):1402–1407 [DOI] [PubMed] [Google Scholar]
- 15.Census regions and divisions of the United States. Available from: https://www.census.gov/geo/maps-data/maps/pdfs/reference/us_regdiv.pdf. Accessed July 18, 2014
- 16.Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson EK, Faerber GJ, Roberts WW, et al. Are stone protocol computed tomography scans mandatory for children with suspected urinary calculi? Urology. 2011;78(3):662–666 [DOI] [PubMed] [Google Scholar]
- 18.Passerotti C, Chow JS, Silva A, et al. Ultrasound versus computerized tomography for evaluating urolithiasis. J Urol. 2009;182(4 suppl):1829–1834 [DOI] [PubMed] [Google Scholar]
- 19.Eshed I, Witzling M. The role of unenhanced helical CT in the evaluation of suspected renal colic and atypical abdominal pain in children. Pediatr Radiol. 2002;32(3):205–208 [DOI] [PubMed] [Google Scholar]
- 20.Persaud AC, Stevenson MD, McMahon DR, Christopher NC. Pediatric urolithiasis: clinical predictors in the emergency department. Pediatrics. 2009;124(3):888–894. [DOI] [PubMed] [Google Scholar]
- 21.Sas DJ, Hulsey TC, Shatat IF, Orak JK. Increasing incidence of kidney stones in children evaluated in the emergency department. J Pediatr. 2010;157(1):132–137 [DOI] [PubMed] [Google Scholar]
- 22.Routh JC, Graham DA, Nelson CP. Epidemiological trends in pediatric urolithiasis at United States freestanding pediatric hospitals. J Urol. 2010;184(3):1100–1104 [DOI] [PubMed] [Google Scholar]
- 23.National Research Council of the National Academies Health Risks from Exposure to Low Levels of Ionizing Radiation BEIR VII Phase 2. Washington, DC: The National Academies Press; 2006 [PubMed] [Google Scholar]
- 24.Kokorowski PJ, Chow JS, Strauss K, Pennison M, Routh JC, Nelson CP. Prospective measurement of patient exposure to radiation during pediatric ureteroscopy. J Urol. 2012;187(4):1408–1414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298 [DOI] [PubMed] [Google Scholar]
- 26.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287 [DOI] [PubMed] [Google Scholar]
- 27.Krein SL, Hofer TP, Kerr EA, Hayward RA. Whom should we profile? Examining diabetes care practice variation among primary care providers, provider groups, and health care facilities. Health Serv Res. 2002;37(5):1159–1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dwyer ME, Krambeck AE, Bergstralh EJ, Milliner DS, Lieske JC, Rule AD. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J Urol. 2012;188(1):247–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pearle MS, Calhoun EA, Curhan GC, Urologic Diseases of America Project . Urologic diseases in America project: urolithiasis. J Urol. 2005;173(3):848–857 [DOI] [PubMed] [Google Scholar]
- 30.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342(8883):1317–1322 [DOI] [PubMed] [Google Scholar]
- 31.Miller DC, Murtagh DS, Suh RS, Knapp PM, Dunn RL, Montie JE. Establishment of a urological surgery quality collaborative. J Urol. 2010;184(6):2485–2490 [DOI] [PubMed] [Google Scholar]
- 32.Miller DC, Murtagh DS, Suh RS, et al. Regional collaboration to improve radiographic staging practices among men with early stage prostate cancer. J Urol. 2011;186(3):844–849 [DOI] [PubMed] [Google Scholar]