Abstract
’Crohn's disease’ is an inflammatory granulomatous disease of the gastrointestinal tract with extra-intestinal manifestations. Oral lesions may precede the intestinal disease and serve as a source for histological diagnosis. We present a case of orofacial Crohn's disease where orofacial symptoms were present for about 13 years and occasional constipation was present, since 6 months. Oral examination plays an important role in early diagnosis of Crohn's disease.
Keywords: Crohn's disease, cobblestone, colitis, chronic, granulomatous enteritis, granuloma, granulomatous disease, pediatric crohn, oral
INTRODUCTION
Crohn's disease (CD) is an inflammatory bowel disease characterised by granulomatous inflammation, which may affect any site along the gastrointestinal tract from the mouth to anus.[1] An Italian physician, Giovanni Battista Morgagni, made the first description of Crohn's disease in 1769 when he diagnosed a man with chronic diarrhoea. In 1930, Dr. Burrill B Crohn saw a connection between this unknown debilitating condition with two of his patients. Consequently, Dr. Crohn and his colleagues presented a paper in 1932, “Regional ileitis: A pathologic and chronic entity”, describing the features of this disease to the American Medical Association. The CD was named after Burrill Crohn and it became an official medical entity in 1932.[2]
The incidence of Crohn's disease is estimated at 1 to 4 persons per 1,00,000. Crohn's disease is one of the second most common inflammatory bowel diseases, with the first being the ulcerative colitis. Together, these 2 diseases affect about 1 million individuals at one time. Crohn's disease can affect any part of the gastrointestinal system from the mouth to the anus with the dentist being the first to diagnose its oral manifestations.[1,2] The disease primarily affects the whites, often in early adulthood and has a slight predilection for females.[3] Oral lesions presenting as a clinical sign were first described in 1969 by Dudeney and their overall incidence ranges from 0.5% to 30%. Diagnosis of Crohn's disease via oral lesions was first reported in 1972 and is attributed to Varley.[3] However, detailed understanding of the specific lesions manifesting in the mouth and their clinical importance has evolved relatively recently.[4]
CASE REPORT
A 34-year-old male patient reported with swelling of face. The facial swelling was first noticed 13 years ago, which gradually increased in size followed by swelling of upper and lower lip. A physician had prescribed drugs, not known to the patient, which aggravated the swelling. Patient had discontinued the medication and did not report to the physician. The swelling gradually reduced without treatment but did not disappear completely. The patient avoided tamarind and raw mangoes as it seemed to aggravate the swelling. However, the swelling had started to increase in size over last six months. Medical history was non-contributory except for a six month-history of occasional constipation.
Clinical examination revealed diffuse swelling of lower third of face and gross enlargement of upper and lower lips [Figure 1]. The swelling was diffuse, non-tender and without bruit or pulsation. Angular cheilitis and spreading erythema were present near the right corner of mouth. Lymph node examination was unremarkable. On intraoral examination, multiple hyperplastic, swollen mucosal folds forming Cobble stone appearance in relation to right and left buccal mucosa was present [Figure 2], with generalized bead like gingival hyperplasia on the labial and buccal aspects [Figure 3] and palatal hyperplasia involving the rugae area were prominent [Figure 4]. Considering patients history and clinical examination, the clinical differential diagnoses included Crohn's disease, sarcoidosis and orofacial granulomatosis (OFG).
Figure 1.

The clinical photograph showing diffuse enlargement of face and lips
Figure 2.

The intraoral photograph showing bead like gingival enlargement
Figure 3.

The intraoral photograph showing cobble stone appearance with hyperplastic mucosal folds on left side of buccal mucosa
Figure 4.

The intraoral photograph showing hyperplasia of palatal mucosa
Hematological investigations revealed raised erythrocyte sedimentation rate ((ESR) 25 mm in 1st hour). Chest radiograph did not reveal anything significant. Incisional biopsy in relation to right and left buccal mucosa revealed oedematous superficial lamina propria with dilated lymphatic vessels. Lymphocytes were scattered diffusely and in clusters along with fibrous scattered aggregates of non-caseating granuloma [Figure 5]. The hematoxylin and eosin stained photomicrograph showing a parakeratinized stratified squamous epithelium along with the underlying granuloma formation under scanner view (5a) and low power view (5b and c). High power view shows scattered aggregates of non-caseating granuloma (5d and e), which are typically small consisting of macrophages, epitheloid cells surrounded by scattered lymphocytes and plasma cells (5f) suggestive of the granulomatous lesion.
Figure 5.
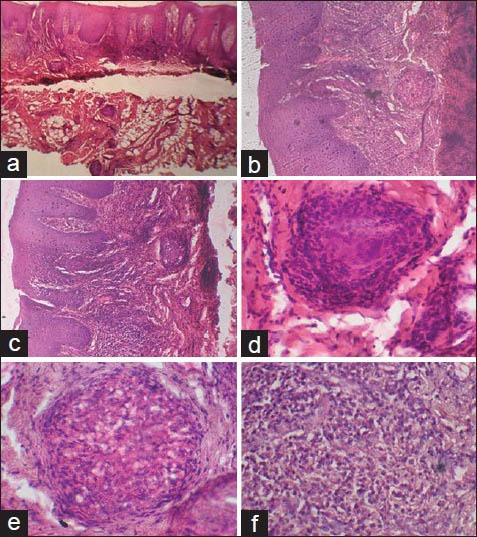
Photomicrograph showing a parakeratinized stratified squamous epithelium along with the underlying granuloma formation. (a – H&E stain, ×40. b and c – H&E stain, ×100). Photomicrograph shows scattered aggregates of non-caseating granuloma (d and e – H&E stain, ×200) which are typically small consisting of macrophages, epitheloid cells surrounded by scattered lymphocytes and plasma cells (f – H&E stain, ×400)
Colonoscopy advised in consult with a gastroenterologist revealed scattered areas of inflammation and erythema involving cecum and ascending colon [Figure 6] Further, multiple areas were biopsied which revealed numerous chronic inflammatory cells like lymphocytes and plasma cells indicating colitis.
Figure 6.

The Colonoscopy showing clinical inflammation of colon
DISCUSSION
Oral Crohn's disease (OCD) may present as cobble stoning, which refers to nodular granulomatous swellings of the mucosa,[5,6,7,8] mucosal tags,[4,5,8] deep linear ulceration,[4,8] hyperplasia of the gingivae,[6] midline lip fissuring, persistent lymphadenopathy,[3] aphthous ulcers,[6,8] angular cheilitis,[4,9] diffuse swelling of lips, buccal mucosa and facial soft tissues which is persistent, firm and painless,[10] perioral erythema,[4] and an uncommon presentation pyostomatitis vegetans, characterized by serpentine pustules that coalesce in a “snail track” pattern.[10]
Orofacial granulomatosis comprises a group of diseases characterized by noncaseating granulomatous inflammation affecting the soft tissues of oral and maxillofacial regions. This term was first introduced by Wiesenfeld in 1985, encompasses Melkerson-Rosenthal syndrome and cheilitis granulomatosa of Miescher.[11,12] In addition, oral granulomas can occur in such systemic conditions such as tuberculosis, Crohn's disease and sarcoidosis.[13]
Patients with intestinal CD who have involvement of the mouth typically are described as having oral CD (OCD).[4] Oral lesions of CD may precede abdominal symptoms and do not necessarily correlate with intestinal disease activity.[10] An oral biopsy will often confirm the nature of the lesions in the presence of a granulomatous inflammation. The histopathological analysis in Crohn's disease bears conspicuous resemblance in intestinal and oral lesions. It is characterized by the triad of deep focal fissuring of the mucosa, formation of noncaseating granuloma deep into the superficial mucosa and the presence of Langhan-type giant cells. Lymphedema of the upper corium and a diffuse or peri-lymphatic lymphocytic infiltrate are also often observed.[3]
The pathogenesis of CD is unknown and the role of genetic, infectious, immune and environmental factors continues to be debated. Oral localization of CD raises more acutely the question of the role of environmental factors. Toothpaste has been proposed as a causal factor of CD, but this hypothesis was not confirmed. Smoking clearly increases the risk for CD and worsens its course, but it is not associated with particular localization.[14] Although the etiology of CD is not known, experimental data, suggests that CD4+ T cells play a role.[6] The inflammatory process is characterized by increased production of proinflammatory cytokines. Tumour necrosis factor (TNF-α) plays a central role in the pathogenesis of the disease. The crucial pathogenic role of TNF in CD has been verified experimentally in mice that bear the genetic deletion of the TNF AU-rich regulatory elements (ARE) that leads to defective post-transcriptional regulation of tnf expression and chronic TNF overproduction. Further, chronically overproduce TNF and spontaneously develop CD8+ T lymphocyte-dependent Crohn-like inflammatory bowel disease pathology in the ileum. Restricting TNF overexpression in myeloid cells or T lymphocytes suffices for the induction of intestinal pathology, indicating the pathogenic potential of TNF derived from innate or adaptive effectors.[15,16]
Beclamethasone mouthwashes (0.5 mg dissolved in water, up to 6 times a day) bring symptomatic relief. However, there is considerable risk of systemic steroid absorption with attendant side effects, thereby mitigating against prolonged use of this form of treatment. Lip swelling is sometimes helped by topical tocrolimus. Intralesional injection of steroid into swollen lips has been reported. However, this form of treatment appears to bring only short-term benefit and can be painful. In patients with persistent pain, swelling and cosmetic disfigurement, the use of immunosuppression can be considered at an early point. Recently, other forms of treatment such as methotrexate and biologic treatment using anti-TNF antibodies have been reported to be useful. However, the potential risks of immunosuppression, which includes malignancy, must be weighed up carefully in such patients.[4]
Diagnosis of the disease by dentists and other clinicians through the evaluation of oral clinical findings is a rare incident.[3] Mucocutaneous and granulomatous lesions of the oral cavity should alert the clinician to investigate the gastrointestinal tract. Early diagnosis of Crohn's disease would lead to better patient management and prognosis.
ACKNOWLEDGEMENT
We would like to thank all the staff members of Department of Oral Medicine and Oral Pathology for their support and cooperation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Pittock S, Drumm B, Fleming P, McDermott M, Imrie C, Flint S, et al. The oral cavity in Crohn's disease. J Pediatr. 2001;138:767–71. doi: 10.1067/mpd.2001.113008. [DOI] [PubMed] [Google Scholar]
- 2.Naser SA, Arce M, Khaja A, Fernandez M, Naser N, Elwasila S, et al. Role of ATG16L, NOD2 and IL23R in Crohn's disease pathogenesis. World J Gastroenterol. 2012;18:412–24. doi: 10.3748/wjg.v18.i5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michailidou E, Arvanitidou S, Lombardi T, Kolokotronis A, Antoniades D, Samson J, et al. Oral lesions leading to the diagnosis of Crohn disease: Report on 5 patients. Quintessence Int. 2009;40:581–8. [PubMed] [Google Scholar]
- 4.Rowland M, Fleming P, Bourke B. Looking in the mouth for Crohn's disease. Inflamm Bowel Dis. 2010;16:332–7. doi: 10.1002/ibd.20983. [DOI] [PubMed] [Google Scholar]
- 5.Galbraith SS, Drolet BA, Kugathasan S, Paller AS, Esterly NB. Asymptomatic inflammatory bowel disease presenting with mucocutaneous findings. Pediatrics. 2005;116:e439–44. doi: 10.1542/peds.2004-2281. [DOI] [PubMed] [Google Scholar]
- 6.Freysdottir J, Zhang S, Tilakaratne WM, Fortune F. Oral biopsies from patients with orofacial granulomatosis with histology resembling crohn's disease have a prominent th1 environment. Inflamm Bowel Dis. 2007;13:439–45. doi: 10.1002/ibd.20023. [DOI] [PubMed] [Google Scholar]
- 7.Basu MK, Asquith P, Thompson RA, Cooke WT. Oral manifestations of Crohn's disease. Gut. 1975;16:249–54. doi: 10.1136/gut.16.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harty S, Fleming P, Rowland M, Crushell E, McDermott M, Drumm B, et al. A prospective study of the oral manifestations of Crohn's disease. Clin Gastroenterol Hepatol. 2005;3:886–91. doi: 10.1016/s1542-3565(05)00424-6. [DOI] [PubMed] [Google Scholar]
- 9.Bangsgaard N, Weile B, Skov L. Organised angular cheilitis as the initial sign of Crohn's disease in two children. Acta Derm Venereol. 2011;91:207–8. doi: 10.2340/00015555-1007. [DOI] [PubMed] [Google Scholar]
- 10.Chi AC, Neville BW, Krayer JW, Gonsalves WC. Oral manifestations of systemic disease. Am Fam Physician. 2010;82:1381–8. [PubMed] [Google Scholar]
- 11.Kauzman A, Quesnel-Mercier A, Lalonde B. Orofacial Granulomatosis: 2 case reports and literature review. J Can Dent Assoc. 2006;72:325–9. [PubMed] [Google Scholar]
- 12.Jinbu Y, Tsukinoki K, Kusama M, Watanbe Y. Orofacial granulomatosis: Report of a case. Oral Med Pathol. 2002;7:33–7. [Google Scholar]
- 13.Grave B, McCullough M, Wiesenfeld D. Orofacial granulomatosis-A 20-year review. Oral Dis. 2009;15:46–51. doi: 10.1111/j.1601-0825.2008.01500.x. [DOI] [PubMed] [Google Scholar]
- 14.Dupuy A, Cosnes J, Revuz J, Delchier JC, Gendre JP, Cosnes A. Oral crohn disease: Clinical characteristics and long-term follow-up of 9 cases. Arch Dermatol. 1999;135:439–42. doi: 10.1001/archderm.135.4.439. [DOI] [PubMed] [Google Scholar]
- 15.Leite MR, Santos SS, Lycra AC, Mota J, Santana GO. Thalidomide induces mucosal healing in Crohn's disease: Case report. World J Gastroenterol. 2011;17:5028–31. doi: 10.3748/wjg.v17.i45.5028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Apostolaki M, Armaka M, Victoratos P, Kollias G. Cellular mechanisms of TNF function in models of inflammation and autoimmunity. Curr Dir Autoimmun. 2010;11:1–26. doi: 10.1159/000289195. [DOI] [PubMed] [Google Scholar]


