Abstract
Background and Objectives:
This study aims at the observation of the immunohistochemical expression of laminin in adenoid cystic carcinoma (ACC) of salivary gland origin and to analyze the distribution of laminin in various components of the tumor and correlate the expression of laminin with the growth and differentiation of the tumor.
Materials and Methods:
Thirty cases of ACC were subjected to immunohistochemical study using polyclonal antihuman laminin primary antibody, distribution of laminin in each case of ACC was observed in the following areas: Intracellularly, inner borders of the pseudocystic spaces, within the lumen of the pseudocysts, around the tumor islands and in the intervening stroma.
Results:
Laminin positivity was observed in the inner aspect of the pseudocystic spaces in 15 cases, within the lumen of pseudocystic spaces in 22 cases, in the intervening stroma in 20 cases, bordering the tumor islands in 16 cases and intracellularly in 4 cases.
Interpretation and Conclusion:
Based on these observations, it can be assumed that laminin plays a major role in proliferation of the tumor cells and in pseudocyst formation. Thus, laminin might play a significant role in the growth and differentiation of ACC and also help in assessing the prognosis of the tumor.
Keywords: Adenoid cystic carcinoma, immunohistochemistry, laminin, pseudocyst
INTRODUCTION
Adenoid cystic carcinoma (ACC) is an epithelial malignant neoplasm of salivary glands. In 1859, Billroth used the term “Cylindroma” to describe the standard for four salivary gland tumors. This term was widely used until 1953, when Foote and Frazell renamed the lesion with the expression “Adenoid Cystic Carcinoma.”[1]
ACC is a relatively rare tumor comprising less than 1% of all malignancies of head and neck area and accounting for about 7.5-10% of all salivary gland neoplasms.[2] Maj Chatterjee et al., (2000) analyzed 306 cases of salivary gland tumors in Medical college, Jabalpur among which ACC comprised 13.30% of cases.[3] Shafkat Ahmad et al., (2002) observed 100 salivary-gland tumors in Government Medical college, Srinagar. The percentage of malignant tumors was 28.5% among which ACC was the most common (35.7%).[4] Krishna Raj (2008) extensively reviewed 684 salivary gland tumors in Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, out of which 262 cases (38%) were malignant neoplasms among which 25% of cases were ACC.[5] Deepika Sirohi et al., (2009) observed 74 cases of salivary gland tumors in Armed Forces Medical College, Pune of which 17% were ACC.[6]
Laminin is a noncollagenous component of basement membrane. This multifunctional glycoprotein provides substrate for directing central nervous system maturation, enables the attachment of epithelial cells to the basement membrane and interacts with the cytoskeletal elements to aid in maintenance of cellular polarity. Overexpression of laminin receptor on tumor cells is implicated in their attachment at sites distant from the primary lesion and laminin's ability to induce production of Type IV collagenase likely aids in degradation and penetration of basement membrane by these metastatic tumor cells.[7,8] Hence, it is reasonable to assume that the distribution of laminin in ACC could be associated with its growth and differentiation and the variation in its distribution might be helpful in assessing the aggressiveness of the tumor.
The present study aims to demonstrate the immunohistochemical expression of laminin in ACC, to analyze its distribution in the tumor, assess its contribution in the growth and differentiation of ACC and the invasiveness of the tumor.
MATERIALS AND METHODS
The sample size was calculated using SS = Z2 pq/delta2 with a normal distribution table value at 95% confidence interval. Thirty cases of ACC were retrieved from the archives of our department and other Dental colleges. All the blocks were sectioned using a semiautomatic microtome (Microm HM340E). 3μm, thick sections were obtained and mounted on the poly-L-Lysine coated slides. These slides were incubated at 37°C overnight before the day of staining and at 60°C for 1 hour on the day of staining. The slides were deparaffinized using xylene and hydrated through graded iso-propyl alcohol. Heat induced antigen retrieval was carried out by heating tissues in Tris saline buffer using microwave oven - two cycles each at 96°C for 6 minutes. Tissues were then incubated with peroxide block for 12 minutes at room temperature and in protein block for 10 minutes. The sections so treated were then incubated with primary antibody (Polyclonal antihuman laminin primary antibody) for 2 hours. They were then incubated with post primary for 30 minutes, then incubated with secondary antibody: Novolink – Min polymer detection system for 30 minutes, with liquid DiAmino Benzidine chromogen for 1-2 minutes and counter stained with Mayer's Hematoxylin provided with the kit for 1 minute. The sections so stained were then viewed under the microscope and assessed for staining characteristics.
RESULTS
Observation
Observations were made on the basis of distribution of positive laminin staining. Basement membrane of the epithelium, blood vessels, nerves and muscles were used as internal positive control. The distribution of laminin in all the cases was observed in the following areas:
Intracellularly
Inner borders of the pseudocystic spaces
Within the pseudocystic spaces
Surrounding the islands
Intervening stroma.
The results of the immunohistochemical staining on the 30 cases of ACC were as follows:
13.3% of cases showed intracellular laminin positivity with P value of 0.0001 (statistically significant) [Figure 1 and Graph 1]
50% of the cases showed laminin positivity in the inner borders of the pseudocystic spaces with Pvalue of 1.00 (no statistical significance) [Figure 2 and Graph 1]
76.67% of cases showed positive expression of laminin within the lumen of the pseudocystic spaces with P value of 0.0035 (statistically significant) [Figure 3 and Graph 1]
53.3% of cases showed positive laminin staining around the tumor islands was with P value of 0.7150 (no statistical significance) [Figure 4 and Graph 1]
73.3% of the cases positive laminin staining in the intervening stroma was observed with P value of 0.0106 (statistically significant) [Figure 5 and Graph 1].
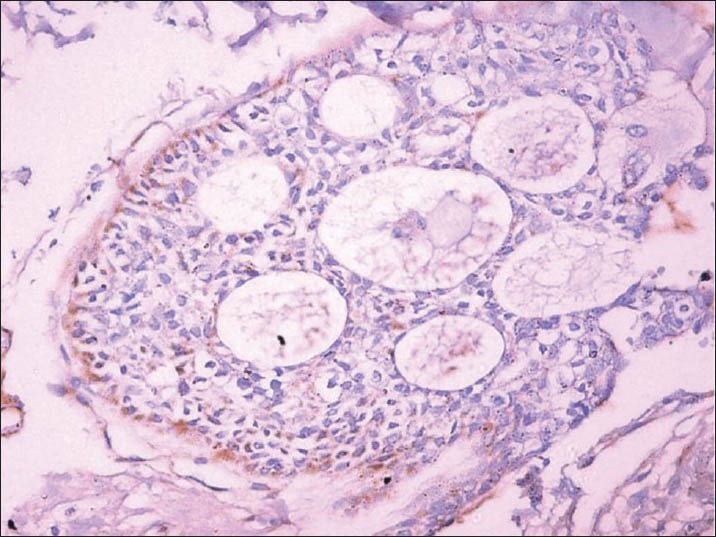
Figure 1.
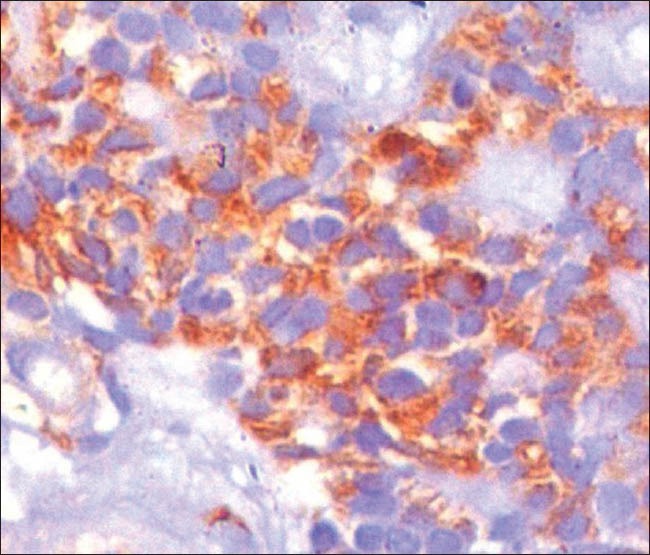
Photomicrograph showing positive cytoplasmic localization of laminin IHC, ×400)
Graph 1.
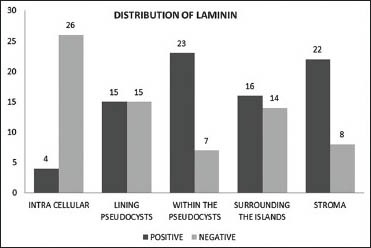
Overall distribution of laminin in adenoid cystic carcinoma
Figure 2.
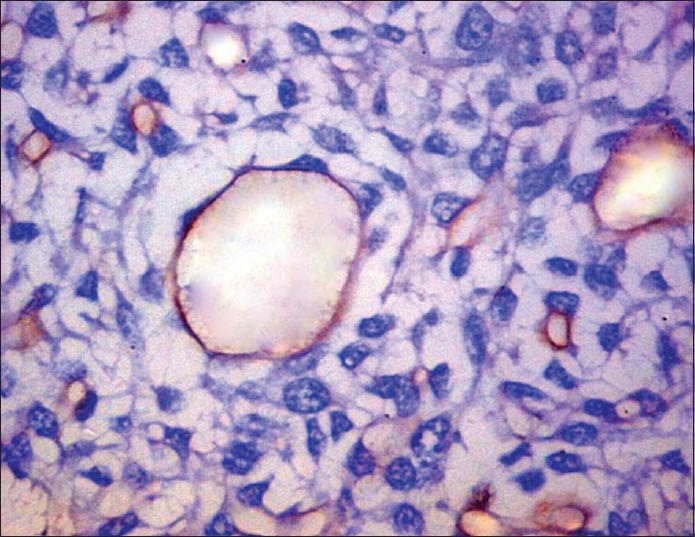
Photomicrograph of positive laminin expression in the inner aspect of pseudocystic spaces in a linear, uninterrupted and continuous pattern (IHC, ×200)
Figure 3.
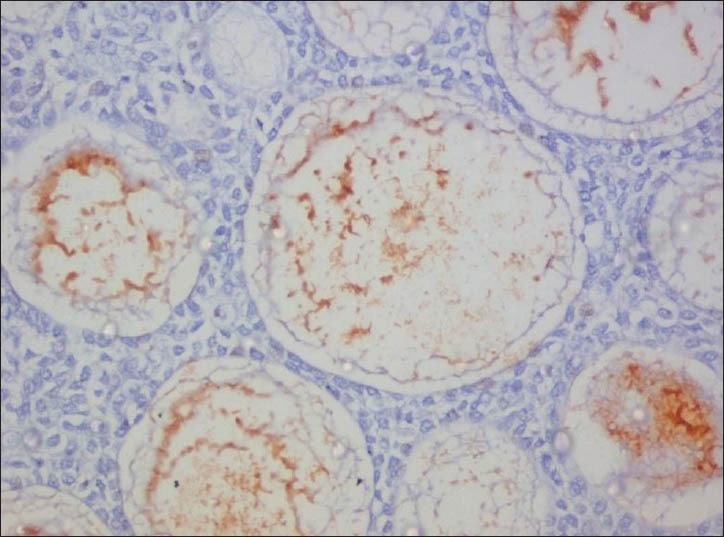
Photomicrograph of positive laminin expression within the pseudocysts (IHC, ×200)
Figure 4.
Photomicrograph showing basement membrane-like linear expression of laminin around the tumor islands (IHC, ×100)
Figure 5.
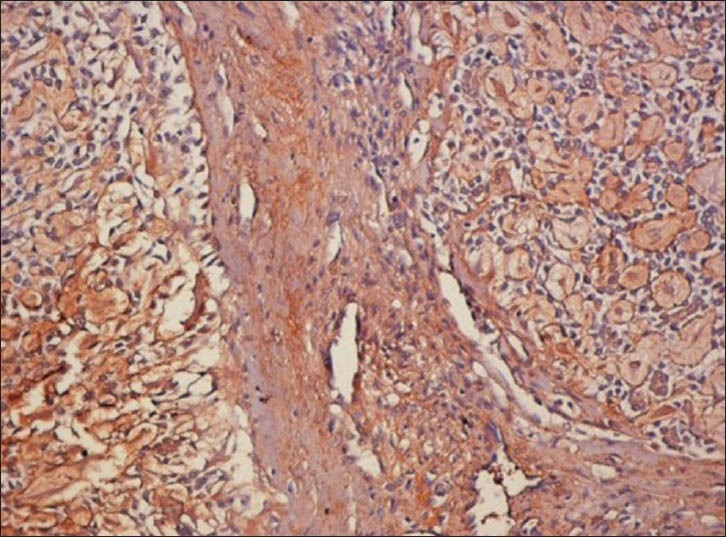
Photomicrograph showing diffuse pattern of laminin expression in the intervening stroma (IHC, ×100)
DISCUSSION
ACC is a malignant salivary gland neoplasm showing insidious and slow growth with high level of recurrence and distant metastasis long time after treatment.[9] Several cytogenetic studies have explored the molecular events in the development and progression of ACC. Persson et al., described a reciprocal t (6;9)(q22-23;p23-24) translocation which results in the formation of Myeloblastosis- Nuclear Factor 1 B-type (MYB-NFIB) fusion oncogene. MYB participates in regulation of cell proliferation, apoptosis and differentiation.[10] Histologically, it shows sheets or island-like proliferations of either round or cuboidal epithelial cells, with scanty cytoplasm and hyperchromatic large oval nuclei.[9] It is characterized by the formation of cribriform structures composed of two types of luminal structures, glandular structure consisting of ductal epithelium-like cells that retain salivary secretory material within the lumen [Figures 6 and 7] and the pseudocysts formed by myoepithelium-like cells which contain an extracellular matrix in their lumen.[11]
Figure 6.
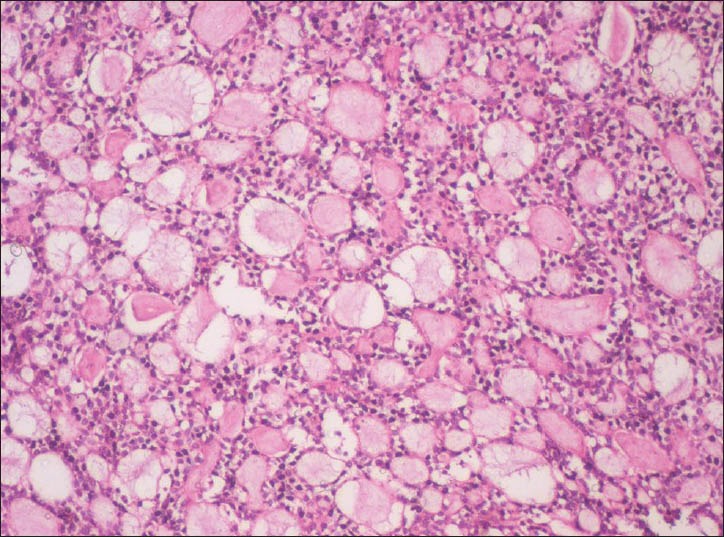
Photomicrograph of adenoid cystic carcinoma showing cribriform architecture with pseudocystic spaces filled with eosiniphilic coagulum. (H&E, ×100)
Figure 7.
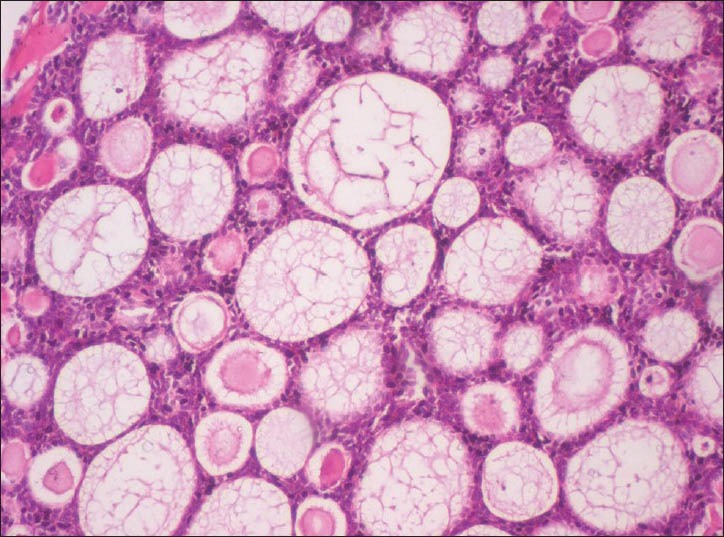
Higher magnification of adenoid cystic carcinoma showing cribriform architecture with pseudocystic spaces filled with eosiniphilic coagulum (H&E, ×200)
Numerous studies using electron microscopy have demonstrated single or multiple layers of basement membrane material in the inner aspect of pseudocystic structures. Based on these morphologic findings, it has been suggested that the pseudocystic structures result from an excessive secretion of extracellular matrix produced by the tumor cells.[7] Retention of the extracellular matrix within the pseudocysts suggests that the basement membrane rich matrix is essential for the proliferation of tumor cells.[12] Munakata et al., in 1996 suggested that the frequent invasion of the peripheral nerves, blood vessels and skeletal muscles by ACC is due to their affinity for basement membrane rich tissues. They also suggested that the tumor cells attach, spread and grow rapidly on the matrices containing basement membrane molecules.[12]
Laminins are cross-shaped, large molecular weight glycoproteins composed of one α-chain, one β-chain and one γ –chain.[13] They are multifunctional molecules with a central role in the organization and physiology of basement membrane. By interacting with cell surface receptors of the integrin family, laminins are responsible for the anchorage of cells and for the initiation of specific intracellular signals. Through other interactions with extracellular matrix proteins, laminins are involved in the architecture, organization and stability of basement membrane.[14] There is emerging evidence that these can regulate cell proliferation and have the capacity of specifying cell and tissue development, differentiation and function through their interaction with cell surface molecules.[15] Hence, it can be assumed that laminin may play a vital role in the growth and proliferation of ACC.
In the present study, the distribution of laminin was analysed in 30 cases of ACC. Formalin fixed paraffin embedded sections of ACC were selected and subjected to immunohistochemical staining using laminin marker (Polyclonal antihuman laminin primary antibody). The sections so stained were then viewed under the microscope and assessed for staining characteristics. The distribution of laminin in all the cases was observed in the following areas- intracellularly, lining the inner aspect of the pseudocystic spaces, within the pseudocystic spaces, surrounding the islands and in the intervening stroma.
In the present study, 13.3% of cases of ACC showed intracellular positivity for laminin with a P value of 0.0001 which is statistically significant. These results are in accordance with a study by A J D’Ardenne et al., (1986) who examined the distribution of laminin in 6 cases out of which only 1 case (16.66%) showed focal cytoplasmic staining for laminin.[16] Intracellular laminin could probably be related to the excessive production of basal lamina.[16]
In this study, 50% of cases showed laminin expression in the inner borders of the pseudocystic spaces, with no statistical significance (P value- 1.00). The results are in accordance with the studies by Makoto Toida (1984), D’Ardenne et al., (1986), Jun Cheng et al., (1992), Loducca (2000) and Raitz et al., (2003). Makoto Toida (1984) studied the distribution of laminin in 9 cases and found 100% positivity.[17] D’Ardenne et al., (1986) examined the distribution of laminin in 6 cases out of which 4 cases showed laminin positivity.[16] Jun Cheng et al., (1992),[11] Loducca (2000)[18] and Raitz et al., (2003)[19] conducted a similar study on 30, 5 and 10 cases, respectively and observed 100% positivity. No statistical analysis has been mentioned in their studies.
In our study, 76.67% of cases showed laminin positivity within the pseudocystic spaces and the results were statistically significant (P value- 0.0035). These results are in agreement with studies by Jun Cheng et al., (1992),[11] Loducca (2000),[18] and Raitz et al., (2003)[19] who observed 100% positivity on 30, 5 and 10 cases of ACC, respectively. The results were not subjected to statistical analysis.
The linear staining of laminin lining the pseudocystic spaces and within the lumen of the pseudocysts shows the presence of basement membrane-like material in the pseudocystic spaces produced by the tumor cells. The laminin positivity within the pseudolumen is due to the presence of molecules that are not integrated into basement membrane structures.[11] This excess production of basement membrane-like material could be a reflection of immunologic response and accounts for better prognosis.[11] The capacity to produce basal lamina appears to be an important property of ACC and is a morphologic manifestation of the tumor's contribution to the extracellular matrix. The amount of expression of laminin is variable and these quantitative differences probably reflect variations of growth or synthetic properties of individual tumors.[20]
In the present study, 53.3% of cases showed laminin staining around the individual islands with no statistical significance (P value- 0.7150). These results are consistent with studies by Makoto Toida (1984), D’Ardenne et al., (1986), Jun Cheng et al., (1992), Loducca (2000) and Raitz et al., (2003).
Makoto Toida (1984) studied the distribution of laminin in 9 cases and observed 100% positivity.[18] D’Ardenne et al., (1986) examined the distribution of laminin in six cases out of which four cases (66.66%) showed laminin positivity.[16] Jun Cheng et al., (1992),[11] Loducca (2000),[18] and Raitz et al., (2003)[19] conducted a similar study on 30, 5 and 10 cases, respectively and observed 100% positivity. Their results were not subjected to statistical analysis.
In our study, out of thirty cases, 73.3% cases showed laminin positivity in the intervening stroma and the results were statistically significant (P value 0.0106). These results are in agreement with the studies by Jun Cheng et al., (1992)[11] and Raitz et al., (2003)[19] who studied laminin distribution in 30 cases and 10 cases of ACC, respectively and observed 100% laminin positivity. No statistical analysis has been mentioned in their study.
The linear deposits of laminin around the tumor nests, in the stroma and interstitial spaces shows that, the extracellular matrix is rich in basement membrane molecules. This suggests that either basement membrane or some of the basement membrane molecules may be required for the proliferation of ACC cells.[11] In vitro studies conducted by Vanessa et al., (2002) to study the effect of laminin-1 on ACC cell line suggest that laminin-1 regulates the morphology of the cells derived from ACC. The growth of the cells within the substrate rich in laminin-1 creates duct-like and pseudocyst-like structures similar to those occurring in the neoplasm in vivo. Hence, it is assumed that the basement membrane observed in the neoplasm in vivo is secreted by the tumor cells themselves and laminin-1 may act as a autocrine factor determining the morphogenetic changes in the tumor cells.[15] Loss of laminin by ACC may occur during transformation to a more aggressive malignancy.[16]
Based on these results, it is assumed that the tumor cells synthesize and secrete the extracellular matrix rich in laminin. This molecule may act as a autocrine factor in determining the mophogenetic characteristics of the tumor cells. Initially these cells proliferate in the form of strands in which every cell is able to communicate with laminin molecules. These strands grow in various directions and contact each other. The stroma enclosed between the tumor cells is isolated from the outer stroma. The extracellular matrix component enclosed by the tumor cells constitutes the pseudocystic spaces. As the tumor further progresses, the tumor cells may proliferate into the pseudocyts giving rise to the solid growth pattern of tumor. The augmentation of basement membrane and an affinity for basement membrane molecules by ACC implies that the tumor cells take the advantage of this structure for proliferation, migration and invasion. Loss or reduced laminin expression may occur during transformation to a more aggressive malignancy. The measure of laminin may help in assessing the prognosis of the ACC. But, a larger series of cases including all the histological subtypes with longer follow up is required to confirm this hypothesis.
Our study concludes that ACC is a tumor with affinity for basement membrane. Laminin, a principal component of basement membrane is synthesized by the tumor cells. The synthesis and secretion of laminin by these tumor cells influences the proferation of the cells, growth and morpho differentiation of the tumor. The variable expression of laminin within the tumor also helps in assessing the prognosis of the tumor. Hence, immunostaining for laminin might be a vital tool in assessing the behavior of ACC.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Soares EC, Carreiro Filho FP, Costa FW, Vieira AC, Alves AP. Adenoid cystic carcinoma of the tongue: Case report and literature review. Med Oral Pathol Oral Cir Bucal. 2008;13:E475–8. [PubMed] [Google Scholar]
- 2.Barrett AW, Speight PM. Perineural invasion in adenoid cystic carcinoma of the salivary glands: A valid prognostic indicator.? Oral Oncol. 2009;45:936–40. doi: 10.1016/j.oraloncology.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Maj TC, Panda PK. A pathological study of benign and malignant tumors of salivary glands. MJAFI. 2000;56:282–6. doi: 10.1016/S0377-1237(17)30208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shafkat A, Mohainmad L, Rouf A. Clinicopathological study of primary salivary-gland tumors in Kashmir. JK Pract. 2002;9:231–3. [Google Scholar]
- 5.Subhashraj K. Salivary gland tumors: A single institution experience in India. Br J Oral Maxillofacial Surg. 2008;46:635–8. doi: 10.1016/j.bjoms.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 6.Sirohi D, Sharma R, Sinha R, Suresh Menon P. Salivary gland neoplasms: An analysis of 74 cases. J Maxillofac Oral Surg. 2009;8:164–6. doi: 10.1007/s12663-009-0040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martinez-Hernandez A, Amenta PS. The basement membranes in pathology. Lab Invest. 1983;48:656–77. [PubMed] [Google Scholar]
- 8.Campebel JH, Terranova VP. Laminin: Molecular organization and biological function. J Oral Pathol. 1988;17:309–23. doi: 10.1111/j.1600-0714.1988.tb01543.x. [DOI] [PubMed] [Google Scholar]
- 9.Franca CM, Jaeger MM, Jaeger RG, Arauâjo NS. The role of basement membrane proteins on the expression of neural cell adhesion molecule (N-CAM) in an adenoid cystic carcinoma cell line. Oral Oncol. 2000;36:248–52. doi: 10.1016/s1368-8375(99)00087-1. [DOI] [PubMed] [Google Scholar]
- 10.Bhaijee F, Pepper DJ, Pitman KT, Bell D. New developments in the molecular pathogenesis of head and neck tumors: A review of tumor-specific fusion oncogenes in mucoepidermoid carcinoma, adenoid cystic carcinoma and NUT midline carcinoma. Ann Diagn Pathol. 2011;15:69–77. doi: 10.1016/j.anndiagpath.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Cheng J, Saku T, Okabe H, Furthmayr H. Basement membranes in adenoid cystic carcinoma. An immunohistochemical study. Cancer. 1992;69:2631–40. doi: 10.1002/1097-0142(19920601)69:11<2631::aid-cncr2820691103>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 12.Munakata R, Irié T, Cheng J, Nakajima T, Saku T. Pseudocyst formation by adenoid cystic carcinoma cells in collagen gel culture and in SCID mice. J Oral Pathol Med. 1996;25:441–8. doi: 10.1111/j.1600-0714.1996.tb00294.x. [DOI] [PubMed] [Google Scholar]
- 13.Katayama M, Sekiguchi K. Laminin-5 in epithelial tumour invasion. J Mol Histol. 2004;35:277–86. doi: 10.1023/b:hijo.0000032359.35698.fe. [DOI] [PubMed] [Google Scholar]
- 14.Tunggal L, Ravaux J, Pesch M, Smola H, Krieg T, Gaill F, et al. Defective laminin 5 processing in cylindroma cells. Am J Pathol. 2002;160:459–68. doi: 10.1016/S0002-9440(10)64865-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freitas VM, Jaeger RG. The effect of laminin and its peptide SIKVAV on a human salivary gland adenoid cystic carcinoma cell line. Virchows Arch. 2002;441:569–76. doi: 10.1007/s00428-002-0678-x. [DOI] [PubMed] [Google Scholar]
- 16.d’Ardenne AJ, Kirkpatrick P, Wells CA, Davies JD. Laminin and fibronectin in adenoid cystic carcinoma. J Clin Pathol. 1986;39:138–44. doi: 10.1136/jcp.39.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toida M, Takeuchi J, Hara K, Sobue M, Tsukidate K, Goto K, et al. Histochemical studies of intercellular components of salivary gland tumors with special reference to glycosaminoglycan, laminin and vascular elements. Virchows Arch A Pathol Anat Histopathol. 1984;403:15–26. doi: 10.1007/BF00689335. [DOI] [PubMed] [Google Scholar]
- 18.Loducca SV, Raitz R, Araujo NS, Araujo VC. Polymorphous low-grade adenocarcinoma and adenoid cystic carcinoma: Distinct architectural composition revealed by type IV collagen, laminin and their integrin ligands (α2β1 and α3β1) Histopathology. 2000;37:118–23. doi: 10.1046/j.1365-2559.2000.00900.x. [DOI] [PubMed] [Google Scholar]
- 19.Raitz R, Martins MD, Araujo VC. A study of extracellular matrix in salivary gland tumors. J Oral Pathol Med. 2003;32:290–6. doi: 10.1034/j.1600-0714.2003.00019.x. [DOI] [PubMed] [Google Scholar]
- 20.García de Marcos JA, Calderón-Polanco J, Poblet E, del Castillo-Pardo de Vera JL, Arroyo-Rodríguez S, Galdeano-Arenas M, et al. Primary adenoid cystic carcinoma of the mandible: Case report and review of the literature. J Oral Maxillofac Surg. 2008;66:2609–15. doi: 10.1016/j.joms.2007.12.038. [DOI] [PubMed] [Google Scholar]


