Abstract
Background:
Oral mucocele is the most common benign minor (accessory) salivary gland lesion, caused due to mechanical trauma to the excretory duct of the gland. Clinically they are characterized by single or multiple, soft, fluctuant nodule, ranging from the normal color of the oral mucosa to deep blue. It affects at any age and is equally present in both sexes with highest incidence in second decade of life. They are classified as extravasation or retention type.
Objectives:
To analyze the data between 2010 and 2011 of, clinically and histopathologically diagnosed 58 oral mucoceles for age, gender, type, site, color, cause, symptoms and dimension.
Results:
Oral mucoceles were highly prevalent in the age group of 15-24 years, were seen in 51.72% of males and 48.28% of females, with a ratio of 1.07:1. The extravasation type (84.48%) was more common than the retention type (15.52%). The most common affected site was lower lip (36.20%) followed by ventral surface of the tongue (25.86%). The lowest frequency was observed in floor of mouth, upper lip and palate. The maximum numbers of mucoceles were asymptomatic (58.62%), and the color of the overlying mucosa had color of adjacent normal mucosa (48.28%). It was also observed that most of the mucoceles had diameter ranging from 5 to 14 mm. The causative factors of the lesion were lip biting (22.41%), trauma (5.18%) and numerous lesions (72.41%).
Conclusion:
Oral Mucoceles are frequently seen in an oral medicine service, mainly affecting young people and lower lip, measuring around 5 to 14 mm and the extravasation type being the most common.
Keywords: Blandin and Nuhn gland, extravasation, gland of weber, oral mucocele, pseudocyst, ranula, retention, von Ebner gland
INTRODUCTION
Oral mucoceles (OMs) are benign soft tissue masses and are clinically characterized by single or multiple, painless, soft, smooth, spherical, translucent, fluctuant nodule, which is usually asymptomatic.[1] Mucoceles (muco - mucus and coele - cavity), by definition, are cavities filled with mucus.[2,3] It is the most common minor (accessory) salivary gland lesion affecting the general population. Minor salivary glands are found in most parts of the oral cavity except the gingiva. The prevalence of mucocele is 2.5 lesions per 1000 population in America, 0.11% in Sweden and 0.08% in Brazil.[4] They represent the 17th most common lesion of oral cavity.[4] Oral mucoceles are usually dome-shaped enlargement with intact epithelium.[5] They are classified as extravasation or retention type.[6,7]
The extravasation type is a pseudocyst without defined walls and are caused due to mechanical trauma to the excretory duct of the gland leading to transection or rupture, with consequent extravasation of mucin into the connective tissue stroma and are seen frequently on lower labial mucosa, buccal mucosa and retromolar area; they are not lined by epithelial lining.[7] The mucus extravasation triggers a secondary inflammatory reaction. Many patients report the periodic discharge of viscous fluid from the lesion. The retention type is less common than extravasation, usually affects older individuals and is seen frequently on upper lip, hard palate, floor of mouth and maxillary sinus.[6,7,8] In mucous retention phenomena, mucus may be retained in the duct and/or acini as a result of duct obstruction by sialolith or strictures [Figure 1].[9] The ductal narrowing can occur due to frequent mouth washing with hydrogen peroxide, deodorant mouthwashes, tartar-control toothpastes or anti-plaque solutions, which are possible causes of irritation.[8]
Figure 1.
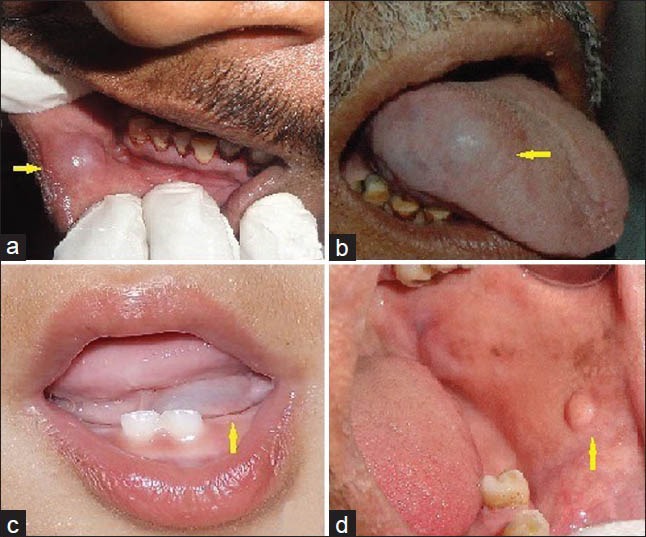
Clinical photographs of oral mucocele involving lower lip (a) tongue (b) floor of mouth (c) and buccal mucosa (d)
The OMs located on the floor of mouth are termed as ‘ranula’, which usually arises in the body of the sublingual gland and occasionally in the ducts of Rivini or in the Wharton's duct.[10] Ranulas are considered a variant of mucoceles and the name is derived from the typical swelling that resembles the air sacs of the frog - ‘rana tigrina’.[11] A ranula manifests as a cup-shaped fluctuant bluish swelling on the floor of mouth and tends to be larger than mucoceles located in other regions of the mouth, reaching some centimeters in diameter.[1,2] The purpose of this study was to analyze the data of OM with an emphasis on clinical and histopathological features and to review the current literature briefly.
MATERIALS AND METHODS
The hospital-based retrospective study was conducted by assessing the clinical records from the year 2010 to 2011, available in the archives of the department of histopathologically diagnosed 58 cases of OMs. The permission to undertake this study was obtained from the Institutional Ethics Committee. The descriptive data of these patients were evaluated and compared with previously documented data in the literature. The study variables included age, gender, type, site, color, etiology, symptoms and dimension of the lesion. The results were analyzed by using Statistical Package for the Social Sciences (SPSS) version 13.0 and Chi-square test.
RESULTS
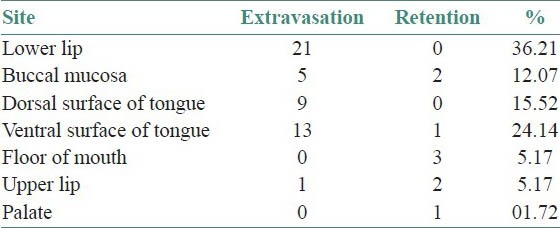
In this study, we observed that the number of patients affected with OMs were between 15 and 49 years with the mean age of 21.20 years [Figure 2]. The OMs were highly prevalent in the age group of 15-19 years (34.48%) followed by 20-24 years (31.04%). The males (51.72%) and females(48.28%) were more or less equally affected, with a ratio of 1.07:1. Out of total 58 patients, 49 (84.48%) patients had extravasation type and were highly prevalent in the age group of 15-24 years, whereas 9 (15.52%) patients had retention type of mucocele and were prevalent in the age group of 30-39 years. In total 49 cases of extravasation type, 25 were males and 24 were females [Figure 3]. The sites affected with OMs were lower lip (36.20%), buccal mucosa (10.34%), dorsal surface of tongue (15.52%), ventral surface of tongue (25.86%), floor of mouth (5.18%), upper lip (5.18%) and palate (1.72%). The lower lip was the most ommonly affected site by extravasation type, and floor of mouth was the most commonly affected site by retention type of OM [Table 1].
Figure 2.
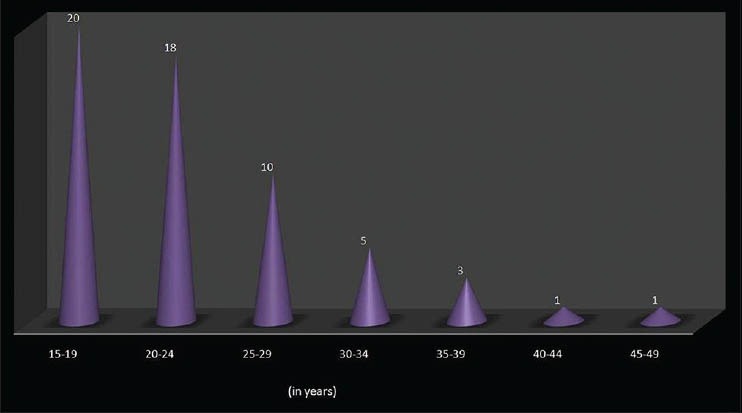
Age-wise distribution of oral mucocele
Figure 3.
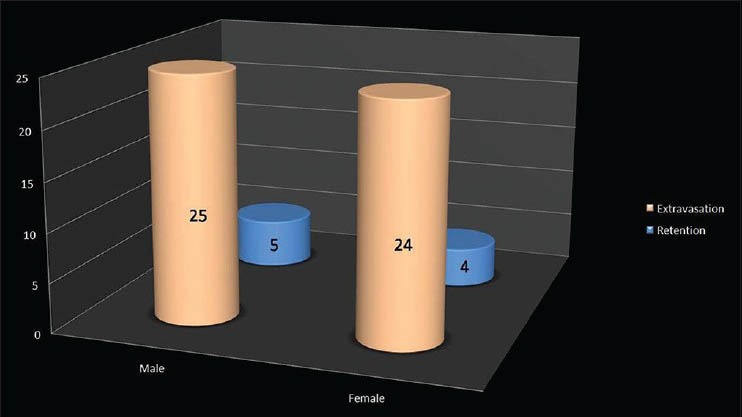
Correlation of gender and type of oral mucocele
Table 1.
Correlation of affected site and type of mucocele
In this study, 34 (58.62%) patients were asymptomatic, 21 (36.20%) patients had discomfort and 03 (05.18%) patients experienced pain [Figure 4]. It was also observed that the color of overlying mucosa of mucocele in 28 (48.28%) patients had normal color i.e. pinkish red, 21 (36.21%) patients had reddish brown color and 09 (15.51%) patients had bluish color [Figure 5]. In our study, it was also observed that the diameter of OMs measured between 5 mm and 34 mm. The OMs in 18 (31.04%) patients measured from 5 to 9 mm, 17 (29.32%) patients had 10-14 mm, 12 (20.69%) patients had 15-19 mm, 07 (12.07%) patients had 20-24 mm, 02 (3.44%) patients had 25-29 mm and 02 (3.44%) patients had 30-34 mm [Figure 6]. We viewed that the causative factors for the OMs were lip biting (22.41%), trauma (5.18%) and numerous lesions (72.41%) had no cause [Figure 7].
Figure 4.
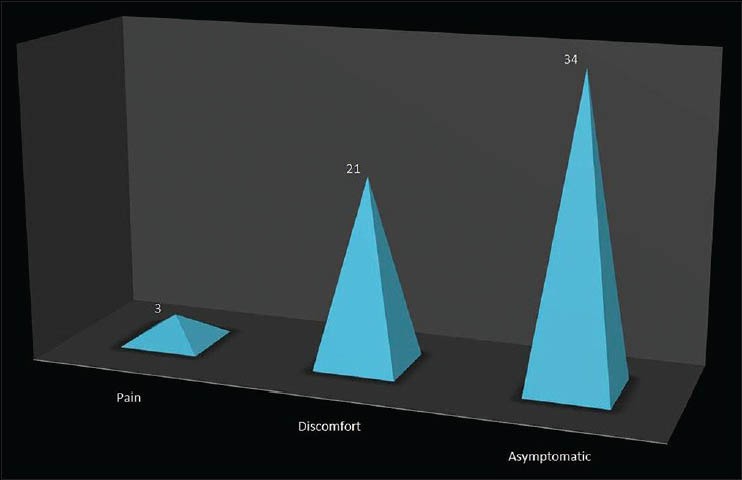
Symptoms associated with oral mucocele
Figure 5.
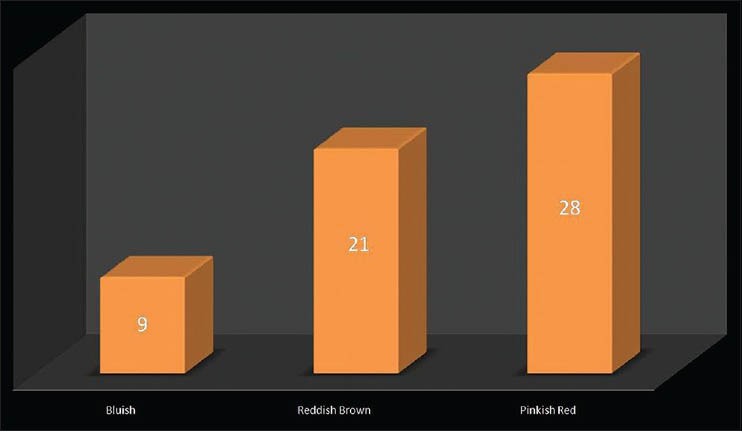
Distribution according to the color of lesion
Figure 6.
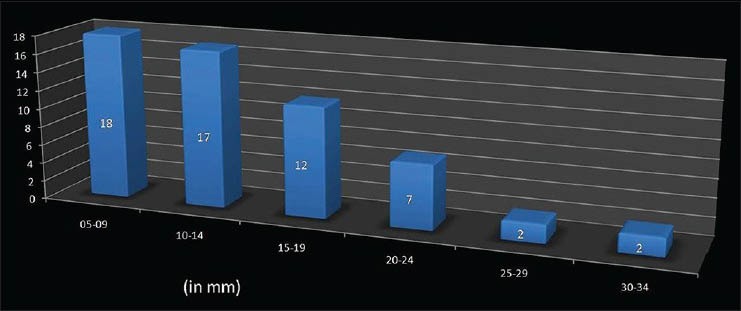
Distribution according to the dimension of lesion
Figure 7.
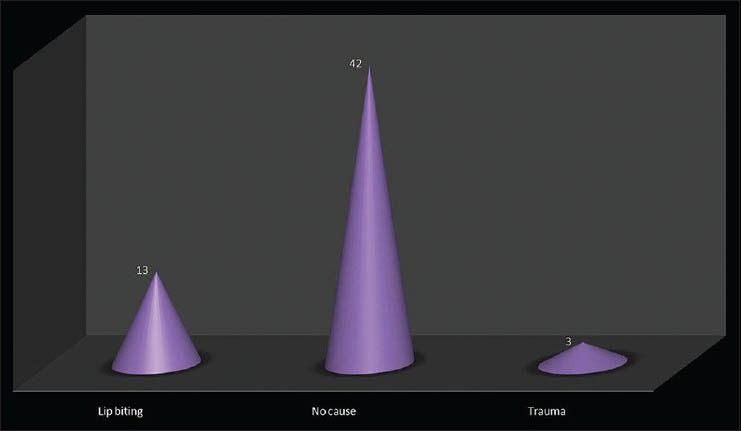
Distribution according to the etiological factors
DISCUSSION
Mucocele is a clinical term used to describe a swelling caused by pooling of saliva from a severed or obstructed minor salivary gland duct.[6] It is a self-limiting mucous containing cyst of salivary glands commonly occurring in the oral cavity, with relatively rapid onset and with fluctuating size.[4] The decrease in size may be due to rupture of the lesion and subsequent mucin accumulation or re-absorption of saliva deposits may cause the lesion to reform.[8]
Most of the OMs are devoid of the epithelial lining or are covered by granulation tissue.[7,8] Oral mucoceles can be single or multiple often rupturing and leaving slightly painful erosions that usually heal within few days.[12] The duration of lesion is not constant, from a few days to 3 years. The clinical presentation may vary depending on the depth of the lesion.[4] The lesions are located directly under the mucous membrane (superficial mucocele) or in the upper submucosa (classical mucocele).[4] Oral mucoceles may be located either as a fluid-filled vesicle or blister in the superficial mucosa or as a fluctuant nodule deep within the connective tissue. Spontaneous drainage of the inspisatted mucin, especially in superficial lesions followed by subsequent recurrence, may occur. The surface of long-standing lesions may show fibrosis.[12] The superficial lesions appear as thin-walled, bluish swellings that rupture easily while the deeper lesions are well circumscribed swellings usually covered by normal appearing oral mucosa.[5]
Oral mucoceles are believed to affect patients of all ages, with the highest incidence in the second decade of life. Teenagers and children are most commonly affected by mucoceles.[6] Menta et al.[10] Yamasoba et al.[13] and Oliveira et al.[14] reported that more than 65% of their patients with OMs were less than 20 years of age. Our findings simulated these findings. However, this always may not be true as the asymptomatic nature of the lesion may delay the patients in seeking treatment. Oral mucoceles are said to arise equally in both the sexes. The studies of Menta et al.[10] Yamasoba et al.[13] and Oliveira et al.[14] also reported similar results as of our study with male: Female ratio of 1.07:1.
Oral mucoceles occur in varying locations on the oral mucosal surfaces overlying accessory minor salivary glands. However, they occur more frequently in certain locations. Lower lip is most commonly affected by mucoceles. However, rare cases of mucoceles involving the upper lip, palate, retromolar region, buccal mucosa, lingual frenum and dorsal tongue have been reported. Ranula designates mucoceles located on the floor of the mouth.[8] Our results matched the findings about occurrence of lesion at lower lip and other oral sites. Surprisingly our findings contradicted the findings of Menta et al.[10] and Alethea et al.[12]
The color of mucoceles ranged from deep blue to the normal color of oral mucosa (pink).[8] The deep blue color results from tissue cyanosis, vascular congestion associated with the stretched overlying tissue and the translucency of the accumulated fluid beneath. The variation in color depends on the size of the lesion, its proximity to the mucosal surface and the elasticity of the overlying tissue.[3,7] The OMs of this study simulated these findings and matched with the studies of Jani et al.[3] and Paulo et al.[15]
Oral mucoceles rarely cause significant problems. Discomfort, interference with speech, mastication, swallowing and external swelling may occur depending on the size and location of mucoceles.[8] All these symptoms were present in our study with varying intensity. These findings simulated with the studies of Bagán et al.[16]
The etiology of OMs is obscure. Trauma and obstruction of salivary gland ducts are considered crucial factors. Surprisingly, in majority of our cases, we could not elicit the cause of mucocele, although lip biting and trauma history was established in few cases, which simulated the findings of Flaitz et al.,[17] López et al.[18] and Selim et al.[19]
Oral mucoceles of minor salivary glands are rarely larger than 1.5 cm in diameter and are always superficial. Mucoceles found in deeper areas are usually larger.[4] It was significantly noted in this study that most of the mucoceles had diameter ranging from 5 to 14 mm, which simulated with the findings of Sebastian et al.[16] and Flaitz et al.[17]
The histopathologic types of mucocele include the most common extravasation and the more rarely, retention variant. The histopathologic aspect of this lesion ranged from acute inflammation intermingling with the mucus collection to patterns of mature lesions with scarce amounts of mucus and connective tissue fibrosis. The lesion may show hyperplastic parakeratinized stratified squamous epithelium, small cystic spaces containing mucin and mucus-filled cells, areas of spilled mucin surrounded by a granulation tissue and sebaceous cells in the connective tissue [Figure 8]. Presence of salivary gland tissue and sialomucin is diagnostic. The age, gender and oral site differ according to the type of OM's.[14] Our study noted that 84.48% of the cases had extravasation type and was more prevalent in the age group of 15-24 years and lower lip.
Figure 8.
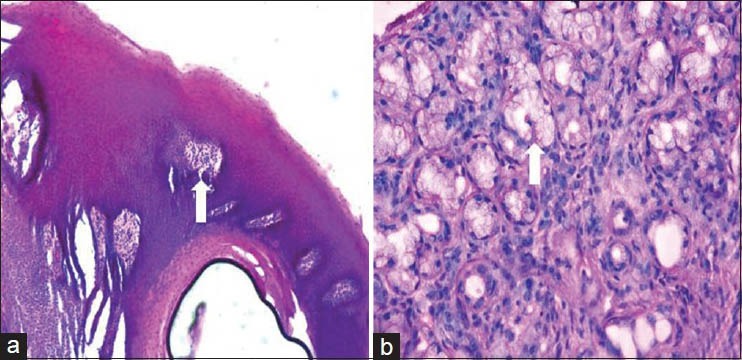
Photomicrograph shows hyperplastic parakeratinized stratified squamous epithelium with underlying connective tissue (a - H&E stain, ×100), photomicrograph showing small cystic spaces containing mucin and mucus-filled cells, few sebaceous cells arranged in groups and areas of spilled mucin surrounded by a granulation tissue are evident in the deeper connective tissue (white arrow) (b - H&E stain, ×200)
Thorough history taking and examination of the lesion is crucial for diagnosing OMs correctly. Although diagnosis is mainly clinical, anamnesis should be carried out correctly, searching for trauma.[7] The appearance of mucocele is pathognomonic, and the following points are crucial: Location, history of trauma, rapid appearance, variations in size, bluish color and the consistency.[20] Mucoceles are mobile lesions with soft and elastic consistency depending on how much tissue is present over the lesion. Despite this fluctuation, a drained mucocele would not fluctuate and a chronic mucocele with a developed fibrosis would have less fluctuation.[7] For specific cases, the diagnosis may require routine radiographs, ultrasonography or advanced diagnostic methods - computed tomography and magnetic resonance imaging for better visualizing the form, diameter, position and determination of the lesion origin. Fine-needle aspiration is a useful diagnostic technique for evaluating patients with salivary gland nodules and enlargement, especially when differential diagnosis of angiomatous lesion is involved.[21] High amylase and protein content can be revealed by the chemical analysis.[12]
Oral mucocele shall be differentiated from lipoma, oral hemangioma, oral lymphangioma, benign or malignant salivary gland neoplasms, venous varix, irritational fibroma, oral lymphoepithelial cyst, gingival cyst of adults, soft tissue abscess, cysticercosis, pyogenic granuloma, etc. The superficial mucoceles may be confused with cicatricial pemphigoid, bullous lichen planus, etc.[5,12]
The treatment for OM shall be either complete excision, marsupialization, dissection, cryosurgery, carbon dioxide lasers, electrocautery, intra-lesional injection of sclerosing agent OK-432 or steroid injection.[8] However, recurrence can occur and a new surgical intervention is necessary.
CONCLUSION
The non-neoplastic diseases of salivary gland pose a diagnostic and therapeutic challenge to the clinician because of close resemblance of clinical presentation despite different etiologies such as reactional inflammatory processes, metabolic and immune disorders, infections and iatrogenic responses. Thus, clinical knowledge of oral lesions, as well as the determination of aspects related to the etiopathogenesis of these lesions, is necessary for the correct diagnosis and for the indication of appropriate treatment.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Hayashida AM, Zerbinatti DC, Balducci I, Cabral LA, Almeida JD. Mucus extravasation and retention phenomena: A 24-year study. BMC Oral Health. 2010;10:15. doi: 10.1186/1472-6831-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kheur S, Desai R, Kelkar C. Mucocele of the anterior lingual salivary glands (Glands of Blandin and Nuhn) Indian J Dent Adv. 2010;2:153–5. [Google Scholar]
- 3.Jani DR, Chawda J, Sundaragiri SK, Parmar G. Mucocele--A study of 36 cases. Indian J Dent Res. 2010;21:337–40. doi: 10.4103/0970-9290.70793. [DOI] [PubMed] [Google Scholar]
- 4.Rashid A, Anwar N, Azizah A, Narayan K. Cases of mucocele treated in the Dental Department of Penang Hospital. Arch Orofac Sci. 2008;3:7–10. [Google Scholar]
- 5.Shamim T. Oral mucocele (mucous extravasation cyst) J Ayub Med Coll Abbottabad. 2009;21:169. [PubMed] [Google Scholar]
- 6.Daniels J, Mohammed I. Mucocele of lingual glands of Blandin and Nuhn: A report of 5 cases. Saudi Dent J. 2005;17:154–61. [Google Scholar]
- 7.Ata-Ali J, Carrillo C, Bonet C, Balaguer J. Oral mucocele: Review of literature. J Clin Exp Dent. 2010;2:e18–21. [Google Scholar]
- 8.Re Cecconi D, Achilli A, Tarozzi M, Lodi G. Mucoceles of the oral cavity: A large case series (1994-2008) and a literature review. Med Oral Pathol Oral Cir Bucal. 2010;15:e551–6. doi: 10.4317/medoral.15.e551. [DOI] [PubMed] [Google Scholar]
- 9.De Camargo Moraes P, Bönecker M, Furuse C, Thomaz LA, Teixeira RG, De Araújo VC. Mucocele of the gland of Blandin-Nuhn: Histological and clinical findings. Clin Oral Investig. 2009;13:351–3. doi: 10.1007/s00784-009-0252-x. [DOI] [PubMed] [Google Scholar]
- 10.Marcello MM, Park JH, Lourenc SV. Mucocele in pediatric patients: Analysis of 36 children. Pediatr Dermatol. 2008;25:308–11. doi: 10.1111/j.1525-1470.2008.00672.x. [DOI] [PubMed] [Google Scholar]
- 11.Ghom A. 1st ed. New Delhi: Jaypee; 2006. Textbook of Oral Medicine; p. 576. [Google Scholar]
- 12.Gupta B, Anegundi R, Sudha P, Gupta M. Mucocele: Two case reports. J Oral Health Community Dent. 2007;1:56–8. [Google Scholar]
- 13.Yamasoba T, Tayama N, Syoji M, Fukuta M. Clinicostatistical study of lower lip mucoceles. Head Neck. 1990;12:316–20. doi: 10.1002/hed.2880120407. [DOI] [PubMed] [Google Scholar]
- 14.Oliveira DT, Consolaro A, Freitas FJ. Histopathological spectrum of 112 cases of mucocele. Braz Dent J. 1993;4:29–36. [PubMed] [Google Scholar]
- 15.Martins-Filho PR, Santos Tde S, da Silva HF, Piva MR, Andrade ES, Da Silva LC. A clinico-pathologic review of 138 cases of mucoceles in a pediatric population. Quintessence Int. 2011;42:679–85. [PubMed] [Google Scholar]
- 16.Bagán Sebastián JV, Silvestre Donat FJ, Peñarrocha Diago M, Milián Masanet MA. Clinico-pathological study of oral mucoceles. Av Odontoestomatol. 1990;6:389. [PubMed] [Google Scholar]
- 17.Flaitz C, Hicks J. Mucocele and ranula. eMedicine. [Last accessed on 2009 Oct 19]. Available from: http://www.emedicine.com/derm/topic648.htm .
- 18.López-Jornet P, Bermejo-Fenoll A. Point of care: What is the most appropriate treatment for salivary mucoceles? Which is the best technique for this treatment? J Can Dent Assoc. 2004;70:484–5. [Google Scholar]
- 19.Selim M, Shea C. Mucous cyst. eMedicine. [Last accessed on 2007 Feb 07]. Available from: http://www.emedicine.com/derm/topic274.htm .
- 20.Yadav A, Grover H, Yadav P, Nanda P. A novel technique for the treatment of mucocele: A Case Report. Arch Dent Sci. 2011;2:33–5. [Google Scholar]
- 21.Syebele K. Regression of both oral mucocele and parotid swellings, following antiretroviral therapy. Int J Pediatr Otorhinolaryngol. 2010;74:89–92. doi: 10.1016/j.ijporl.2009.09.043. [DOI] [PubMed] [Google Scholar]


