Abstract
Context:
Focal fibrous hyperplasia, also known as irritation or traumatic fibroma, is a reactive, inflammatory hyperplastic lesion of the connective tissue.
Aim:
The aim of this study is to perform a retrospective study of a focal fibrous hyperplasia of 18 years.
Materials and Methods:
We retrospectively reviewed 193 cases of focal fibrous hyperplasia of the oral cavity from the medical and histological reports of the Department of Oral Pathology, Pernambuco University, Brazil, during the period between January 1992 and December 2009.
Settings and Design:
Data with regard to age, gender, location, size of the lesion (equal to or less than 1 cm, between 1 and 2 cm and greater than 2 cm), pain, history of trauma, treatment, length of follow-up (from diagnosis to release or last review) and recurrence, were collected.
Results:
The most commonly affected site was the buccal mucosa (n = 119, 61.7%). Almost two-thirds of the cases were concentrated from the second to the fifth decade of life. Females were more affected than men and a history of trauma was related by 90.7% of the patients. Two recurrences were notified (1.0%).
Conclusion:
Further studies are needed on the distribution of the lesion in different ethnic and geographical populations. The influence of sex hormones on the development of focal fibrous hyperplasia must be clarified.
Keywords: Reactive hyperplasia, traumatic fibroma, tumors
INTRODUCTION
Focal fibrous hyperplasia (FFH), also known as irritation or traumatic fibroma, is a reactive, inflammatory hyperplastic lesion of the connective tissue. It presents usually as a yellowish–white or mucosal colored, sessile, smooth-surfaced, asymptomatic, soft nodule. The surface may be hyperkeratotic or ulcerated, owing to repeated trauma. The most common intraoral site is along the occlusal line of the buccal mucosa – an area subject to masticatory trauma – but it also affects the lower lip, tongue, hard palate and edentulous alveolar ridge.[1] The aim of this study is to describe the clinical features of 193 cases of FFH, diagnosed in a service of oral and maxillofacial surgery in Brazil.
MATERIALS AND METHODS
Study design
We retrospectively studied 193 cases of FFH from the medical and histological reports of patients with soft-tissue reactive lesions that involved the oral cavity from the Department of Oral Pathology, Pernambuco University, Brazil, during the period between January 1992 and December 2009. This study was approved by the Ethics Committee (0075.0.107.000-08).
Inclusion and exclusion criteria
All patients with a histopathological diagnosis of FFH were included. Patients with an incomplete history were excluded.
Analyzed variables
Data were collected regarding the age, gender, location, size of the lesion (equal to or less than 1 cm, between 1 and 2 cm and greater than 2 cm), pain, history of trauma, treatment, length of follow-up (from diagnosis to release or last review) and recurrence.
Data analyses
In this retrospective cross-sectional study, we have limited the analysis to the description of variables such as proportions and means. The interpretations are summarized in Figures and Tables.
RESULTS
Of the 1290 soft-tissue reactive lesions of the oral cavity, 193 were confirmed histologically as FFH, a prevalence of 15%. The most common affected sites were the buccal mucosa [Figure 1], lower lip and dorsal tongue [Table 1]. Almost two-thirds of the cases were concentrated from the second to the fifth decade of life, with a mean of 41.4 years and a peak prevalence in the fifth decade [Figure 2]. There were 136 female and 57 male patients, with a female:male ratio of 2.4:1. A history of local trauma was related by 175 patients (90.7%). Most patients reported no pain (92.2%) and the lesions rarely exceeded 2 cm in diameter (49.2%) [Figures 3 and 4]. All cases were treated by surgical excision under local anesthesia. Seventeen patients failed to attend for follow-up examinations. The follow-up period for the remaining patients ranged from one week to about four years after the operation and two recurrences were notified (1.0%).
Figure 1.

Focal fibrous hyperplasia in the buccal mucosa
Table 1.
Distribution of 193 FFHs according to the site of involvement
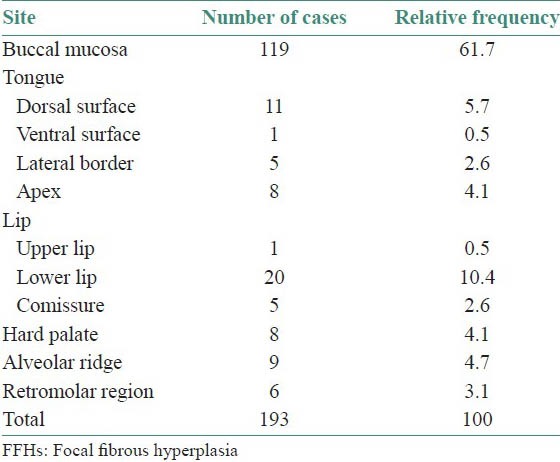
Figure 2.
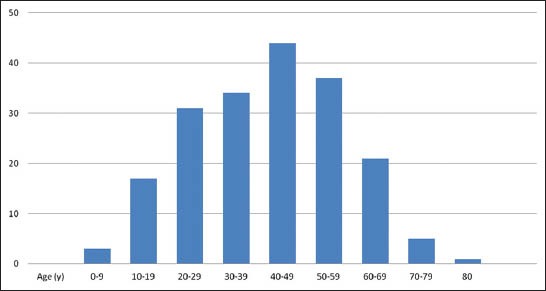
Distribution of 193 focal fibrous hyperplasia according to the age of patients
Figure 3.
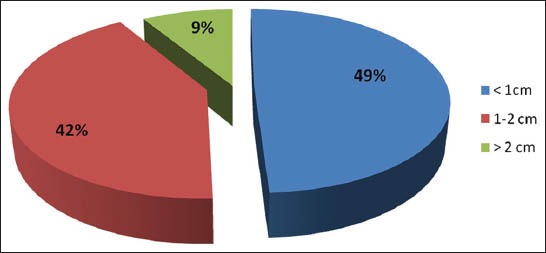
Distribution of 193 focal fibrous hyperplasia according to the diameter of lesions
Figure 4.

Focal fibrous hyperplasia with a larger diameter in the alveolar region of the maxilla
DISCUSSION
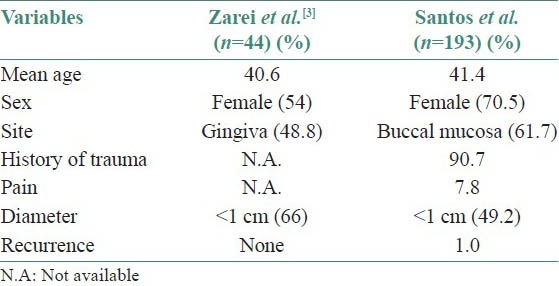
Although relatively common in the oral cavity,[2] we have found a paucity of studies on FFH in the Pubmed English language literature. To date, the largest case series on FFH have been published by Zarei et al.,[3] along with other reactive lesions of the oral cavity. Therefore, additional epidemiological studies are needed in order to more fully describe their characteristics.
The results of this study show that FFH affects people of all ages and both genders, but has a high frequency in female adults, similar to that found by Zarei et al.[3] This predilection for adults is probably related to the specific features in this range of life, which include wear dentures, lower-lip-biting habit, chronic cheek-biting and biting objects. As observed in the present study, mechanical trauma is closely related to the development of the FFH, contrary to the idea that this lesion is a true neoplasm. In addition, it is possible that female hormones contribute to an increased production and accumulation of collagen by fibroblasts in the presence of a chronic injury. Interestingly, other reactive lesions also show a great predilection for females and are detected in the first five decades of life, when hormonal changes are most predominant.[4,5,6,7]
Our findings as regards the site confirm the previous reports[1,8] that found a higher prevalence of FFH in the buccal mucosa along the bite line, but contrasted with the study by Zarei et al.,[3] where it was mostly found in the gingiva [Table 2]. Regardless of the site, FFH characteristically exhibits a limited growth potential, which is a determining factor for the absence of superficial ulcerations due to secondary trauma. Definitive diagnosis is based on histological analysis to rule out the possibility of lesions that may have a similar appearance, such as, pyogenic granuloma (PG), peripheral giant-cell granuloma (PGCG) and peripheral ossifying fibroma (POF).
Table 2.
Comparison of data from Zarei et al.[3] and Santos et al.
Histologically, FFH is characterized by an unencapsulated, solid, nodular mass of dense and sometimes hyalinized fibrous connective tissue. The surface epithelium is usually atrophic, but may show signs of continued trauma, such as, excess keratin, intracellular edema of the superficial layers or traumatic ulceration.[9] [Figure 5]. About 1% of the FFH present stellate and giant cells.[10] [Figure 6]. Although PG, POF and PGCG are also strongly associated with the chronic local irritation and trauma, their histological aspects are different from the FFH, especially when the lesions have a short duration. PG consists of prominent vascular spaces lined with endothelium in a loosely arranged fibrillary matrix, with moderate-to-severe chronic inflammation,[5,11] while in the POF, the presence of mineralization areas – bone, cementum-like material or dystrophic calcifications – with multinucleated giant cells near them is a common finding.[6] On account of their clinical and histopathological similarity, it is considered that at least some cases of POF may arise as a result of the maturation of a longstanding PG.[12] PGCG is a rather common lesion of the oral cavity, arising mainly from the connective tissue of the gingiva or the periosteum of the alveolar ridge due to the irritation trauma. The lesion is characterized by a non-encapsulated highly cellular mass with abundant giants cells dispersed throughout.[7]
Figure 5.
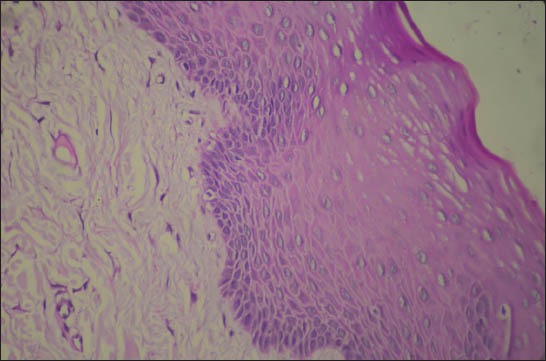
Histological section showing a fibrous connective tissue with mild chronic inflammatory infiltrate covered by a hyperplastic epithelium, with hyperkeratosis and hyperchromatism of the basal/parabasal layers (H and E, ×100)
Figure 6.
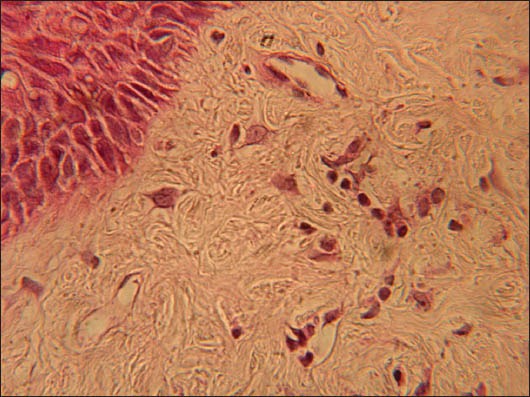
Histological section showing the presence of some large stellate cells with two and three nuclei (H and E, ×400 original magnification)
In addition, it is important to explain that FFH should be differentiated from an unusual non-neoplastic lesion of the oral cavity known as giant-cell fibroma (GCF). This lesion occurs most commonly on the tongue and gingiva, in the young patients, without sex predilection. Microscopically, CFG is composed of a non-inflammated fibrous connective tissue, with the presence of large stellate cells, usually with one or two nuclei, just beneath the epithelium. Multinucleated giant cells are seen occasionally.[13] However, the giant cells are not exclusive of the CFG and can also be seen in other lesions, including FFH, looking to be part of the normal spectrum of tissue responses to injuries.[14] Immunohistochemical stains show that these cells are only vimentin-positive, suggesting a fibroblast phenotype.[15,16]
Simple excision is the treatment of choice of FFH and recurrence is unlikely unless the inciting trauma continues or is repeated, as is observed in the present study. Of late, Trajtenberg and Adibi[17] have suggested that laser excision is an alternative for treating oral soft tissue lesions, including FFH, since it avoids the use of postoperative medications and accelerates the healing process.
In summary, except for variations in the sites of involvement, the features of FFH among Brazilians are similar to those reported by Zarei et al.[3] in Iranians. Further studies are needed on the distribution of the lesions in different ethnic and geographical populations. The influence of sex hormones on the development of FFH must be clarified.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gonsalves WC, Chi AC, Neville BW. Common oral lesions: Part II. Masses and neoplasia. Am Fam Physician. 2007;75:509–12. [PubMed] [Google Scholar]
- 2.Bouquot JE, Gundlach KK. Oral exophytic lesions in 23,616 white Americans over 35 years of age. Oral Surg Oral Med Oral Pathol. 1986;62:284–91. doi: 10.1016/0030-4220(86)90010-1. [DOI] [PubMed] [Google Scholar]
- 3.Zarei MR, Chamani G, Amanpoor S. Reactive hyperplasia of the oral cavity in Kerman province, Iran: A review of 172 cases. Br J Oral Maxillofac Surg. 2007;45:288–92. doi: 10.1016/j.bjoms.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Whitaker SB, Bouquot JE. Identification and semiquantification of estrogen and progesterone receptors in peripheral giant cell lesions of the jaws. J Periodontol. 1994;65:280–3. doi: 10.1902/jop.1994.65.3.280. [DOI] [PubMed] [Google Scholar]
- 5.Saravana GHL. Oral pyogenic granuloma: A review of 137 cases. Br J Oral Maxillofac Surg. 2009;47:318–9. doi: 10.1016/j.bjoms.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Mishra MB, Bhishen KA, Mishra S. Peripheral ossifying fibroma. J Oral Maxillofac Pathol. 2011;15:65–8. doi: 10.4103/0973-029X.80023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katsikeris N, Kakarantza-Angelopoulou E, Angelopoulos AP. Peripheral giant cell granuloma. Clinicopathologic study of 224 new cases and review of 956 reported cases. Int J Oral Maxillofac Surg. 1988;17:94–9. doi: 10.1016/s0901-5027(88)80158-9. [DOI] [PubMed] [Google Scholar]
- 8.Dayan D, Wolman M, Hammel I. Histochemical study of the blue autofluorescence of collagen in oral irritation fibroma: Effects of age of patients and of the duration of lesions. Histol Histopathol. 1994;9:11–3. [PubMed] [Google Scholar]
- 9.Robinson RA. 1st ed. Philadelphia (PA): Lippincot Williams and Wilkins; 2009. Head and neck pathology: Atlas for histologic and cytologic diagnosis. [Google Scholar]
- 10.Regezi JA, Courtney RM, Kerr DA. Fibrous lesions of the skin and mucous membranes which contain stellate and multinucleated cells. Oral Surg Oral Med Oral Pathol. 1975;39:605–14. doi: 10.1016/0030-4220(75)90202-9. [DOI] [PubMed] [Google Scholar]
- 11.Martins-Filho PR, Piva MR, da Silva LC, Reinheimer DM, Santos TS. Aggressive pregnancy tumor (pyogenic granuloma) with extensive alveolar bone loss mimicking a malignant tumor: Case report and review of literature. Int J Morphol. 2011;29:164–7. [Google Scholar]
- 12.Fausto KA. 7th ed. Philadelphia (PA): WB Saunders; 2008. Robbins and Cotran pathologic basis of disease. [Google Scholar]
- 13.Kuo RC, Wang YP, Chen HM, Sun A, Liu BY, Kuo YS. Clinicopathological study of oral giant cell fibromas. J Formos Med Assoc. 2009;108:725–9. doi: 10.1016/S0929-6646(09)60396-X. [DOI] [PubMed] [Google Scholar]
- 14.Odell E, Lock C, Lombardi T. Phenotypic characterisation of stellate and giant cells in giant cell fibroma by immunocytochemistry. J Oral Pathol Med. 1994;23:284–7. doi: 10.1111/j.1600-0714.1994.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 15.Magnusson BC, Rasmusson LG. The giant cell fibroma. A review of 103 cases with immunohistochemical findings. Acta Odontol Scand. 1995;53:293–6. doi: 10.3109/00016359509005990. [DOI] [PubMed] [Google Scholar]
- 16.Campos E, Gomez RS. Immunocytochemical study of giant cell fibroma. Braz Dent J. 1999;10:89–92. [PubMed] [Google Scholar]
- 17.Trajtenberg C, Adibi S. Removal of an irritation fibroma using an Er, Cr: YSGG laser: A case report. Gen Dent. 2008;56:648–51. [PubMed] [Google Scholar]


