Abstract
Both obesity and strenuous outdoor work are known risk factors for heat-related illness (HRI). These risk factors may be compounded by more and longer periods of extreme heat in the southeastern U.S. To quantify occupational risk and investigate the possible predictive value of a GIS-based tool, a weighted occupation-based metabolic equivalent (MET) index was created. The correlation between current MET-weighted employment rates or obesity rates and 2012 HRI report rates in Alabama were then determined. With the current dataset, results indicate occupational and obesity rates may explain some of the geographical variation seen in HRI report rates, although results are not statistically significant with this limited dataset. Mapping occupational and physiological risk factors with HRI rates may be useful for environmental and occupational health professionals to identify “hotspots” that may require special attention.
Introduction
Heat stress is a serious health threat during the summertime for a large portion of the U.S. population, particularly during physical exertion. According to the Centers for Disease Control and Prevention (CDC), from 1979 to 2003 heat killed 8,015 Americans—more than hurricanes, lightning, tornadoes, floods, and earthquakes combined (CDC, 2009). Recent government statistics on heat-related fatalities indicate, “Between 1999 and 2003, a total of 3,442 deaths resulting from exposure to extreme heat were reported (annual mean: 688) and males accounted for 66% of those deaths (CDC, 2006a).” In 2011, 206 people died as a result of extreme heat, up from 138 fatalities in 2010 (National Oceanic and Atmospheric Administration [NOAA], 2012). The 10-year average for heat-related fatalities is 119 (NOAA, 2012).
In 2012 the Intergovernmental Panel on Climate Change (IPCC) released a special report on extreme events, concluding that increases in the frequency and magnitude of warm daily temperature extremes and decreases in cold extremes will occur in the 21st century at the global scale with 99%–100% probability (IPCC, 2012). The report also states that daily temperature extremes will increase this century, with 90%–100% probability that heat waves will increase in length, frequency, or intensity over most land areas. Observations since 1950 document changes in daily temperature extremes and heat waves (IPCC, 2012) and a recent analysis of extreme heat events in the U.S. between 1979 and 2011 suggests the number of heat wave days has been increasing in the southeast (Smith, Zaitchik, & Gohlke, 2012).
Anderson (2011) estimated that limiting the global mean temperature to 2°C of warming will still result in current historical temperature extremes becoming the norm for 70%–80% of the Earth's surface. Hyatt and co-authors (2010) utilized published formulas for the Wet Bulb Globe Temperature (WBGT) in combination with global gridded climate data and concluded that estimated future increases of WBGT may create extreme heat exposure situations in large areas of the world.
Although global and national estimates of health effects due to climate change have been summarized, further studies are required to develop a better understanding of health risks across divergent geographical locations (Zhang, Bi, & Hiller, 2007). Public health researchers and practitioners are playing a lead role in this endeavor to develop estimates of interaction between exposure and susceptibility to health effects in identifying the most appropriate adaptation measures (Luber & Hess, 2007). For example, the elderly are thought to be particularly susceptible to heat stress, and mapping of the proportion of elderly has been used in adaptation planning (Minnesota Department of Health, 2013). In contrast, occupational risk factors have received limited attention in public health adaptation planning.
Alabama's high humidity and temperature extremes can lead to heat-related illnesses (HRI) and deaths (Alabama Department of Public Health [ADPH], 2012a). A study of temperature-related deaths in Alabama by Taylor and McGwin (2000) found that mortality rates for hyperthermia were higher in Alabama than nationally. The authors stated that rates among males were higher than those of females, with the highest rates found among African-American males. The cause of the higher rates among African-American males is not known, but the finding was consistent with nationwide studies (CDC, 2000). Risk factors include low socioeconomic status, alcohol consumption, certain drugs, underlying chronic disease, previous heat stroke, and physical exertion (Taylor & McGwin, 2000).
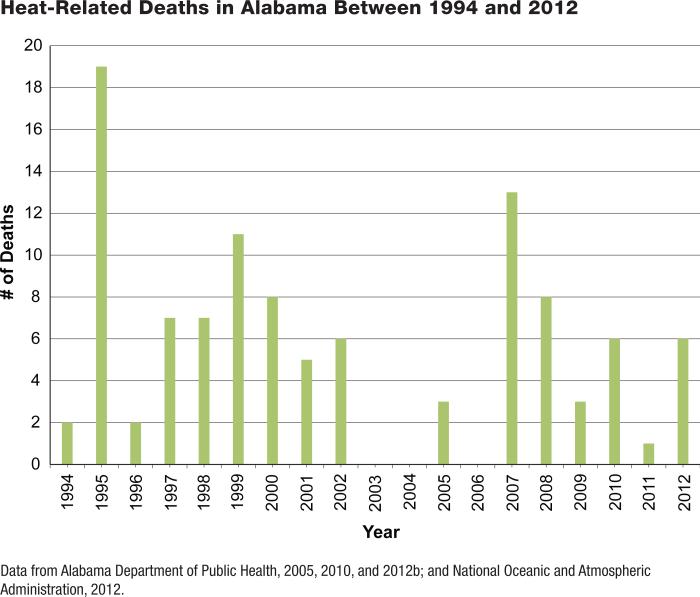
Mortality in the state of Alabama due to excessive heat include a high of 125 in 1980 and yearly deaths since 1994 are charted in Figure 1 (ADPH, 2005, 2010, 2012b; NOAA, 2012). Most of the victims during the 1980 heat wave were elderly shut-ins who lacked air conditioning. A less intense heat wave in August 2007 resulted in 13 fatalities, while the majority of those treated at hospitals were of working age (26–50) and were working outside when they experienced heat stress (Pence & Stefkovich, 2008), suggesting the demographics of heat-related deaths may be changing.
FIGURE 1.
Heat-Related Deaths in Alabama Between 1994 and 2012
HRI and fatalities in Alabama were recently added to the list of notifiable diseases required to be reported to the health department (ADPH, 2012a). Of the 809 HRI in 2012, 347 were reported as work related (ADPH, 2012a). Other state surveillance programs have also suggested work-related HRI contributes significantly to the overall numbers of HRI (e.g., Florida Department of Health, 2012; North Carolina Public Health, 2012). Bonauto and co-authors (2007) used both International Statistical Classification of Diseases and Related Health Problems (ICD)-9 and American National Standards Institute (ANSI) Z16.2 codes with sub sequent medical record review to identify 480 Washington State Fund workers’ compensation claims for HRI over the 11-year time period of 1995–2005. North American Industry Classification System industries with the highest workers’ compensation HRI average annual claims incidence rate were fire protection; roofing construction; and highway, bridge, and street construction. HRI claims were associated with high outdoor ambient temperatures, and medical risk factors for HRI were present in some cases. Risk factors for classical heat stroke include cardiovascular and respiratory disease, diabetes, obesity, and the use of medications that reduce sweating, impair thermoregulation, and weaken cardiovascular responses (Bonauto et al., 2007). The risk for developing exertional heat illness increases with body mass index (Donoghue & Bates, 2000; Gardner et al., 1996) and may be an important factor in determining occupational HRI.
This article maps occupational risks (as indicated by number of workers in high-risk occupations, based on physical exertion data) by county for the state of Alabama and identifies those counties with the highest proportion of at-risk workers per capita. This data should allow health agencies to target specific counties and industries for the dissemination of preventive care information, as well as identify likely future heat strain response priority locations.
Methods
To address occupation-specific vulnerabilities, metabolic equivalent (MET) values for Activities in American Time Use Survey (ATUS) data were obtained from the National Cancer Institute's Web site (National Cancer Institute, 2012a). These data are from a study by Tudor-Locke and coauthors (2009), who used the 2003 Bureau of Labor Statistics (BLS) ATUS, which contains “438 distinct primary activity variables that can be analyzed with regard to how time is spent by Americans.” The Compendium of Physical Activities facilitates comparison of coded intensity levels across studies. Tudor-Locke and co-authors (2009) link compendium estimates of physical activity intensity (METs) with all activities reported in the 2003 ATUS. One MET is defined as “the energy to lie/sit quietly. It is equivalent to a metabolic rate of consuming 3.5 mL O2/kg/minute.” The MET values in the resulting dataset range from 0.00 to 10.00. The higher the number, the more strenuous the task. MET values in the dataset range from a low value of 0.92 (sleeping) to a high value of 10.00 (playing rugby).
Occupation-specific MET-ATUS data were downloaded from the National Cancer Institute (2012b). MET values for occupations range from a low of 1.5, e.g., chief executives, to 8.0, e.g., logging workers. Census Occupation Classification codes for 2002 in the MET-ATUS data were matched to their corresponding 2002 Standard Occupational Classification Codes (SOC) by using 2002 Current Population Survey (CPS) Occupational Codes as a data crosswalk (U.S. Census Bureau, 2012).
Alabama employment data containing estimated employment for SOC codes were downloaded from the Alabama Department of Labor, summarized for 16 metropolitan statistical areas (MSAs) (Alabama Department of Labor, 2012a). Microsoft Access was used to join MET data for each MSA and SOC code.
Alabama HRI data were obtained from the Alabama Department of Public Health for reporting period June 29, 2012, through September 15, 2012, which included the following fields: type (HRI or heat-related death), facility county, age group (1–14, 15–24, 25–44, 45–59, or 60+), sex, contributing factor (athletic related, work related, or other), and entry timestamp. It should be noted that sex and contributing factor were not reported for five of the six heat-related death records.
The Alabama Department of Public Health has mapped this data by state public health area and also has charted cases by date and age range. In terms of time trends, reported cases in 2012 reached an early high of more than 70 cases in early July and then trended downward with additional spikes above 30 cases in mid- and late July. The largest category for age was 25–44 (37%), followed by 45–59 (23%), 15–24 (20%), 60+ (17%), and 1–14 (3%) (ADPH, 2012b).
Weighted MET rates were calculated for each MSA as follows: first, occupational MET values were multiplied by estimated employment to obtain a weighted MET value for each occupation. These weighted MET occupation values were then summed for each MSA. To obtain the population in each MSA, average employment values were summed for each county in the MSA. Employment data, “Annual 2010 Selected Data Relative to Employment, Wages, & Benefit Payments,” was downloaded from the Alabama Department of Labor (2012b). Finally, the weighted MET sum for each MSA was divided by its employment population to obtain a weighted MET rate. These operations were performed for (1) all MET values, (2) the average (per MSA) for all MET values, (3) MET values <3.00, (4) MET values 3.00–5.99, (5) MET values 6.00–10.00, and (6) MET values for out- door occupations. These breaks correspond to the MET categories of sedentary and light (<3.00), moderate (3.00–5.99), and vigorous (≥6.00) by the National Cancer Institute (2012b).
Also, county obesity prevalence and leisure-time physical inactivity prevalence data were obtained from the CDC Diabetes Inter active Atlases (CDC, 2004, 2010). These values were summed for each MSA.
Finally, the ADPH-reported HRI incidents for each MSA were summed and divided by each MSA's population to obtain HRI rates per MSA. These rates were calculated for all reported HRIs as well as just those HRIs for which the contributing factor was work related. Once all data were formatted as rates per MSA, Pearson product-moment correlation coefficients and p-values were calculated between HRI (work-related HRI) and occupational MET categories and obesity in MATLAB R2013b using the corr function.
Results
Table 1 summarizes the 2012 HRI data analyzed. First, a possible connection between occupation, exertion, and HRI was investigated. Table 2 is a small subset of activity codes and their associated MET values, which were obtained after mapping METATUS data CPS codes to their corresponding 2002 SOC codes.
TABLE 1.
Summary of 2012 Alabama Heat-Related Deaths and Illnesses
| Category | # |
| Heat-related deaths | 6 |
| Other | 1 |
| (Blank) | 5 |
| Heat-related illnesses | 809 |
| Athletic related | 104 |
| Other | 358 |
| Work related | 347 |
| Total | 815 |
TABLE 2.
Activity Codes and Metabolic Equivalent (MET) Values Assigned to a Subset of Occupations
| Management Occupation Title From 2002 Census Occupational Classification System | 2002 Census Code | 2002 SOCa Code | Assigned Activity Codes | Assigned MET Values |
|---|---|---|---|---|
| Fire fighters | 3740 | 33-2011 | 12 | 5.0 |
| Couriers and messengers | 5510 | 43-5021 | 10 | 4.5 |
| Agricultural inspectors | 6010 | 45-2011 | 10 | 4.5 |
| Logging workers | 6130 | 45-4020 | 16 | 8.0 |
| Brick masons, block masons, and stone masons | 6220 | 47-2020 | 13 | 5.0 |
SOC = Standard Occupational Classification Codes.
Pearson correlation coefficients and p-values for work-related HRI with the estimated employment rates in various MET categories and obesity are reported in Table 3. Proportion of employees in the MET 3–5.99 category were marginally positively correlated to work-related HRI (p = .08). This MET category includes occupations with significant outdoor time such as fire fighters, groundskeepers, trash collectors, brick masons, sheet metal workers, plumb-ers, and electricians.
TABLE 3.
Pearson Correlation Coefficients and p-Values for Work-Related Heat-Related Illnesses and Employment Rate in Various Metabolic Equivalent (MET) Categories and Obesity
| Category | Correlation Coefficient | p-Value |
|---|---|---|
| All METs | −.15 | .59 |
| MET <3.00 | −.36 | .18 |
| MET 3.00-5.99 | .45 | .08 |
| MET 6.00-10.00 | −.17 | .55 |
| Outdoor METs | −.05 | .87 |
| Obesity | .29 | .30 |
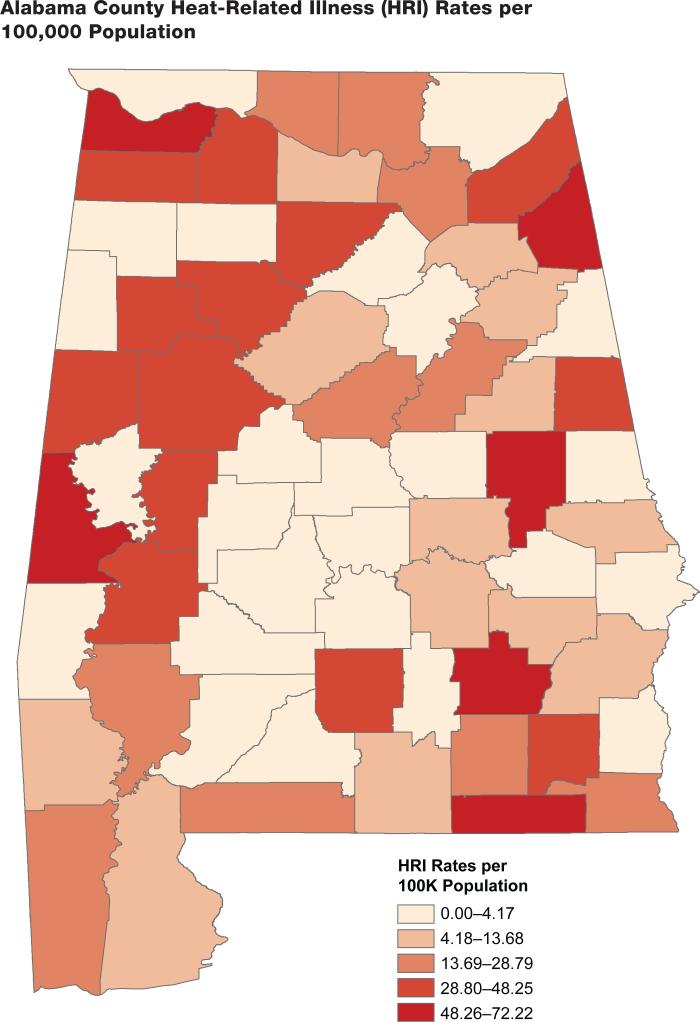
Utilizing ESRI ArcGIS 10.1, the reported cases of HRI by county were mapped. For each county, the report count was divided by the county population (Census 2010 estimates) and multiplied by 100,000 in order to obtain a report rate per 100,000 population. This is mapped in Figure 2 and helps visualize which counties are reporting higher HRI rates than one might expect based purely on population.
FIGURE 2.
Alabama County Heat-Related Illness (HRI) Rates per 100,000 Population
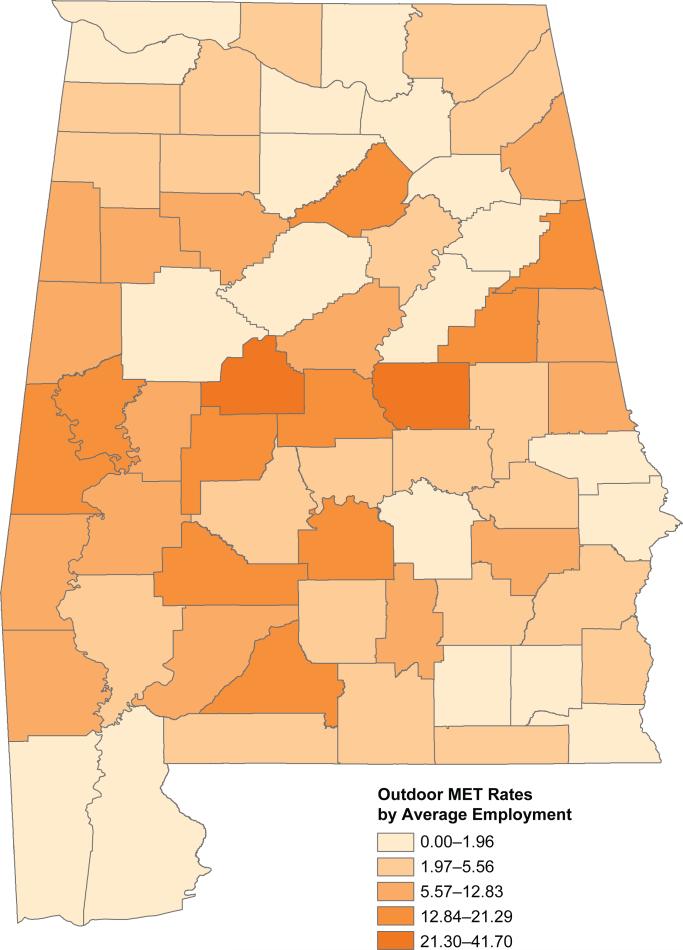
Finally, the weighted county MET employment for identified outdoor MET (OutMET) values were mapped. For each county, the sum of OutMET was divided by the county's average employment (Census 2010 estimates). These values are mapped in Figure 3.
FIGURE 3.
Alabama Weighted Outdoor Metabolic Equivalent (MET) Rates by Average County Employment
Discussion
Limitations exist in the current application that may explain the lack of statistical significance in correlations between HRI and occupational MET categories and obesity. For example, although obesity is a known risk factor for HRI (Gardner et al., 1996), Alabama's most obese counties correspond to some of the state's most rural counties, falling within the Black Belt region (CDC, 2006b). Someone experiencing an HRI in one of these counties may receive medical treatment in another county; thus, the reporting county does not necessarily correspond to the county of residence.
Other factors likely contributing to poor correlations between the various MET data categorizations and HRI include both low HRI sample size, only one year of data, and employment data aggregation. Employment data had to be estimated for most counties by extrapolating values from multicounty (MSA-level) data, which leads to poor spatial resolution. Mapping vulnerability to extreme heat events by mapping occupation-related risk may aid in developing geographically specific prevention strategies for extreme heat events. Mapping allows us to identify areas of greater risk from factors like occupation and obesity, singly or in combination and to plan accordingly. Datasets that have been further disaggre-gated to the ZIP code or census tract level will increase the statistical power of future analysis of occupational risk factors and increase the utility of mapping for local level adaptation planning. Comparing predicted MET risks with actual reported HRI cases is important, as no clear correlation may exist between HRI risk and the number of employees working in vigorous or outdoor occupations (Table 4). A higher MET value for these occupations may be offset by appropriate clothing/gear, work-rest cycles, and acclimation. Additional research into specific occupation risk factors is warranted, along the lines of the state of Washington study by Bonauto and co-authors (2007), who found, for example, that roofing construction had one of the highest workers’ compensation HRI average annual claims rates.
TABLE 4.
Master List of Outdoor Occupations
| METa Value | SOCa Code | SOC Title |
|---|---|---|
| 8.0 | 45-4021 | Fallers |
| 8.0 | 45-4022 | Logging equipment operators |
| 8.0 | 45-4023 | Log graders and scalers |
| 8.0 | 45-4029 | Logging workers, all other |
| 7.5 | 47-2221 | Structural iron and steel workers |
| 7.5 | 53-7062 | Laborers and freight, stock, and material movers, hand |
| 7.5 | 53-7121 | Tank car, truck, and ship loaders |
| 6.0 | 47-2031 | Carpenters |
| 6.0 | 47-2061 | Construction laborers |
| 5.0 | 33-2011 | Fire fighters |
| 5.0 | 47-2021 | Brickmasons and blockmasons |
| 5.0 | 47-2051 | Cement masons and concrete finishers |
| 5.0 | 47-2071 | Paving, surfacing, and tamping equipment operators |
| 5.0 | 47-2081 | Drywall and ceiling tile installers |
| 5.0 | 47-2211 | Sheet metal workers |
| 5.0 | 47-3011 | Helpers—brickmasons, blockmasons, stonemasons, and tile |
| 5.0 | 47-3012 | Helpers—carpenters |
| 5.0 | 47-3013 | Helpers—electricians |
| 5.0 | 47-3014 | Helpers—painters, paperhangers, plasterers, and stucco masons |
| 5.0 | 47-3015 | Helpers—pipelayers, plumbers, pipefitters, and steamfitters |
| 5.0 | 47-3016 | Helpers—roofers |
| 5.0 | 47-3019 | Helpers, construction trades, all other |
| 5.0 | 47-5021 | Earth drillers, except oil and gas |
| 4.5 | 37-3011 | Landscaping and groundskeeping workers |
| 4.5 | 37-3012 | Pesticide handlers, sprayers, and applicators, vegetation |
| 4.5 | 37-3013 | Tree trimmers and pruners |
| 4.0 | 47-2132 | Insulation workers, mechanical |
| 4.0 | 47-2141 | Painters, construction and maintenance |
| 4.0 | 47-2151 | Pipelayers |
| 4.0 | 47-2152 | Plumbers, pipefitters, and steamfitters |
| 4.0 | 47-2171 | Reinforcing iron and rebar workers |
| 4.0 | 47-4031 | Fence erectors |
| 4.0 | 47-5011 | Derrick operators, oil and gas |
| 4.0 | 47-5012 | Rotary drill operators, oil and gas |
| 4.0 | 49-9021 | Heating, air conditioning, and refrigeration mechanics and installers |
| 4.0 | 51-2041 | Structural metal fabricators and fitters |
| 4.0 | 53-7081 | Refuse and recyclable material collectors |
| 3.5 | 47-2042 | Floor layers, except carpet, wood, and hard tiles |
| 3.5 | 47-2044 | Tile and marble setters |
| 3.5 | 47-2181 | Roofers |
| 3.5 | 47-4051 | Highway maintenance workers |
| 3.5 | 47-4071 | Septic tank servicers and sewer pipe cleaners |
| 3.5 | 47-5081 | Helpers—extraction workers |
| 3.0 | 43-5041 | Meter readers, utilities |
| 3.0 | 45-2092 | Farmworkers and laborers, crop, nursery, and greenhouse |
| 3.0 | 45-2093 | Farmworkers, farm and ranch, and aquacultural animals |
| 3.0 | 45-2099 | Agricultural workers, all other |
| 3.0 | 47-2111 | Electricians |
| 3.0 | 47-5041 | Continuous mining machine operators |
| 3.0 | 47-5042 | Mine cutting and channeling machine operators |
| 3.0 | 47-5049 | Mining machine operators, all other |
| 3.0 | 49-9051 | Electrical power line installers and repairers |
| 3.0 | 49-9052 | Telecommunications line installers and repairers |
| 3.0 | 53-5011 | Sailors and marine oilers |
| 2.5 | 17-1022 | Surveyors |
| 2.5 | 19-1032 | Foresters |
| 2.5 | 27-2022 | Coaches and scouts |
| 2.5 | 27-2023 | Umpires, referees, and other sports officials |
| 2.5 | 33-3041 | Parking enforcement workers |
| 2.5 | 47-2073 | Operating engineers and other construction equipment operators |
| 2.0 | 33-9091 | Crossing guards |
| 2.0 | 33-9092 | Lifeguards, ski patrol, and other recreational protective service workers |
| 1.5 | 53-7021 | Crane and tower operators |
| 1.5 | 53-7032 | Excavating and loading machine and dragline operators |
MET = metabolic equivalent. SOC = Standard Occupational Classification Codes.
Conclusion
County maps depicting HRI rates per capita and weighted MET rates depict areas of greater HRI incidence and potential occupational risk factors for HRI, respectively. Such maps may lead to improved public health strategies for health care professionals and emergency responders.
Additional promising future research avenues include the use of GIS tools to analyze both relatively static (demographic risk factors such as obesity and social vulnerability) and dynamic (environmental risk factors such as temperature and humidity) variables to the end that GIS may prove useful as a predictive tool by environmental and public health practitioners in order to prepare for heat-related emergencies.
Contributor Information
Kyle G. Crider, School of Engineering University of Alabama at Birmingham.
Elizabeth H. Maples, School of Public Health University of Alabama at Birmingham.
Julia M. Gohlke, School of Public Health University of Alabama at Birmingham.
References
- Alabama Department of Labor Occupational wage estimates. 2012a Retrieved from http://www2.labor.alabama.gov/cew/default.aspx.
- Alabama Department of Labor Annual 2010 selected data relative to employment, wages & benefit payments. 2012b Retrieved from http://www2.labor.alabama.gov/cew/2010/Annual/Statewide summarybycounty.aspx.
- Alabama Department of Public Health Health precautions urged during periods of prolonged heat [Press release] 2005 Retrieved from http://www.adph.org/news/assets/050621.pdf.
- Alabama Department of Public Health Heat leads to at least six deaths in Alabama this summer, precautions urged [Press release] 2010 Retrieved from http://www.adph.org/news/assets/100820.pdf.
- Alabama Department of Public Health Heat-related illnesses. 2012a Retrieved from http://www.adph.org/injuryprevention/index.asp?id=4458.
- Alabama Department of Public Health Heat-related illness and death, as of 9/14/12. 2012b Retrieved from http://www.adph.org/injuryprevention/assets/HeatRelatedCasesGraphic.pdf.
- Anderson BT. Near-term increase in frequency of seasonal temperature extremes prior to the 2°C global warming target. Climatic Change. 2011;108(3):581–589. [Google Scholar]
- Bonauto D, Anderson R, Rauser E, Burke B. Occupational heat illness in Washington State, 1995–2005. American Journal of Industrial Medicine. 2007;50(12):940–950. doi: 10.1002/ajim.20517. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Hypothermia-related deaths—Alaska, October 1998–April 1999, and trends in the United States, 1979–1996. Morbidity and Mortality Weekly Report. 2000;49(1):11–14. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention County level estimates of obesity—state maps. 2004 Retrieved from http://www.cdc.gov/diabetes/atlas/obesityrisk/atlas.html.
- Centers for Disease Control and Prevention Heat-related deaths—United States, 1999–2003. Morbidity and Mortality Weekly Report. 2006a;55(29):796–798. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Community health advisors light up Alabama's black belt. 2006b Retrieved from http://www.cdc.gov/prc/stories-prevention-research/stories/community-health-advisors-light-up-alabama-black-belt.htm.
- Centers for Disease Control and Prevention Extreme heat: A prevention guide to promote your personal health and safety. 2009 Retrieved from http://www.bt.cdc.gov/disasters/extremeheat/heat_guide.asp.
- Centers for Disease Control and Prevention Diabetes interactive atlases. 2010 Retrieved from http://www.cdc.gov/diabetes/atlas/countydata/atlas.html.
- Donoghue AM, Bates GP. The risk of heat exhaustion at a deep underground metalliferous mine in relation to body-mass index and predicted VO2max. Occupational Medicine (London) 2000;50(4):259–263. doi: 10.1093/occmed/50.4.259. [DOI] [PubMed] [Google Scholar]
- Florida Department of Health Florida injury surveillance data system. 2012 Retrieved from http://www.doh.state.fl.us/DEMO/InjuryPrevention/InjuryData.html.
- Gardner JW, Kark JA, Karnei K, Sanborn JS, Gastaldo E, Burr P, Wenger CB. Risk factors predicting exertional heat illness in male Marine Corps recruits. Medicine and Science in Sports and Exercise. 1996;28(8):939–944. doi: 10.1097/00005768-199608000-00001. [DOI] [PubMed] [Google Scholar]
- Hyatt OM, Lemke B, Kjellstrom T. Regional maps of occupational heat exposure: Past, present, and potential future. Global Health Action. 2010;3 doi: 10.3402/gha.v3i0.5715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intergovernmental Panel on Climate Change . Managing the risks of extreme events and disasters to advance climate change adaptation: Special report of the intergovernmental panel on climate change. Cambridge University Press; New York: 2012. [Google Scholar]
- Luber G, Hess J. Climate change and human health in the United States. Journal of Environmental Health. 2007;70(5):44–46. [PubMed] [Google Scholar]
- Minnesota Department of Health Extreme heat events. 2013 Retrieved from http://www.health.state.mn.us/divs/climatechange/extremeheat.html#populations.
- National Cancer Institute Metabolic equivalent (MET) values for activities in American time use survey (ATUS) 2012a Retrieved from http://riskfactor.cancer.gov/tools/atus-met/
- National Cancer Institute Metabolic equivalent (MET) values for activities in the 2002 census occupational classification system (OCS) 2012b Retrieved from http://riskfactor.cancer.gov/tools/ocs-met/
- National Oceanic and Atmospheric Administration 2011 Heat-related fatalities by state and location. 2012 Retrieved from http://www.nws.noaa.gov/om/hazstats/heat11.pdf.
- North Carolina Public Health Current data on heat-related illness in North Carolina. 2012 Retrieved from http://publichealth. nc.gov/chronicdiseaseandinjury/heat.htm.
- Pence K, Stefkovich J. A comparison of the Alabama heat wave of August 2007 with that of June/July 1980. 2008 Retrieved from http://www.srh.noaa.gov/bmx/?n=research_heatwave20071980.
- Smith TT, Zaitchik BF, Gohlke JM. Heat waves in the United States: Definitions, patterns, and trends. Climatic Change. 2012;118(3–4):811–825. doi: 10.1007/s10584-012-0659-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor A, McGwin G. Temperature-related deaths in Alabama. Southern Medical Journal. 2000;93(8):787–792. [PubMed] [Google Scholar]
- Tudor-Locke C, Washington TL, Ainsworth BE, Troiano RP. Linking the American time use survey (ATUS) and the compendium of physical activities: Methods and rationale. Journal of Physical Activity and Health. 2009;6(3):347–353. doi: 10.1123/jpah.6.3.347. [DOI] [PubMed] [Google Scholar]
- Census Bureau US. 2002–2010 Occupation census crosswalk. 2012 Retrieved from http://www.census.gov/people/io/
- Zhang Y, Bi P, Hiller JE. Climate change and disability-adjusted life years. Journal of Environmental Health. 2007;70(3):32–36. [PubMed] [Google Scholar]