Abstract
Objective:
A growing number of studies have examined the “immigrant paradox” with respect to the use of licit and illicit substances in the United States. However, there remains a need for a comprehensive examination of the multigenerational and global links between immigration and substance use disorders among adults in the United States.
Method:
The present study, using data from the National Epidemiologic Survey on Alcohol and Related Conditions, aimed to address these gaps by comparing the prevalence of substance use disorders of first-generation (n = 3,338) and second-generation (n = 2,515) immigrants with native-born American adults (n = 15,733) in the United States. We also examined the prevalence of substance use disorders among first-generation emigrants from Asia, Africa, Europe, and Latin America in contrast to second-generation and native-born Americans.
Results:
The prevalence of substance use disorders was highest among native-born Americans, slightly lower among second-generation immigrants, and markedly lower among first-generation immigrants. Adjusted risk ratios were largest among individuals who immigrated during adolescence (ages 12–17 years) and adulthood (age 18 years or older). Results were consistent among emigrants from major world regions.
Conclusions:
Consistent with a broad body of literature examining the links between the immigrant paradox and health outcomes, results suggest that nativity and age at arrival are significant factors related to substance use disorders among first- and second-generation immigrants in the United States.
Agrowing number of studies have examined the “immigrant paradox” with respect to the use of licit and illicit substances in the United States. Overall, this body of research suggests that immigrants to the United States, relative to the native born, are less likely to initiate and develop substance use disorders. Evidence for this phenomenon, also referred to as the “healthy immigrant effect,” has been observed among a variety of behavioral (e.g., antisocial behavior, intimate partner violence) and health (e.g., chronic disease, obesity) outcomes as well as among emigrants from various global regions and in multiple receiving nations (Kennedy et al., 2014; Salas-Wright et al, 2014a, 2014b; Salas-Wright and Vaughn, 2014; Vaughn et al., in press, 2014a, 2014b). Fundamentally, the paradox is that, despite having disproportionately lower income and education levels, immigrants are often healthier than their native-born counterparts.
A number of theoretical explanations have been articulated in an effort to conceptualize the protective relationship between immigrant status and substance use. One prominent conceptualization suggests that immigrants, by virtue of having successfully uprooted their lives from one nation to another, tend to be highly capable, self-disciplined, and healthy individuals. Drawing from this framework, immigrants are believed to self-select such that they are less likely to be involved in a variety of health-risk behaviors, including substance use (Rubalcava et al., 2008). A second, related explanation, previously referred to as the “cultural armamentarium hypothesis” (Vaughn et al., 2014b), posits that immigrants bring with them cultural norms and practices (e.g., anti–drug use norms, tendency to congregate around other immigrants) that may provide a form of “herd immunity” that can protect from involvement in substance use and other health-risk behaviors (Charles, 2006). A third possibility is that immigrants may abstain from high-risk or illegal activities such as substance use because of fears of deportation or involvement in a foreign criminal justice system (Hacker et al., 2011).
With respect to immigrant status and substance use, the bulk of empirical research has focused on youth, particularly youth of Latin American origin, noting that adolescent and young adult immigrants are less likely than their native-born counterparts to initiate substance use and develop substance use disorders (Coll et al., 2012; Schwartz et al., 2010). These studies have highlighted the differences with respect to immigrant generation, age at arrival, duration in the United States, and various acculturative mechanisms that might explain the immigration–substance use link (Almeida et al., 2012; Bacio et al., 2013; Blake et al., 2001; Bui, 2013; Gfroerer and Tan, 2003; Kopak, 2013; Peña et al., 2008; Salas-Wright et al., 2014a, 2014b; Schwartz et al., 2011, 2014). Studies focused on young adults, few in number, have compared the prevalence of substance use before and after immigration (De La Rosa et al., 2013) and disparities in substance-related risk behavior (Maldonado-Molina et al., 2011). The vast majority of these studies are limited in generalizability inasmuch as they use samples of youth from particular national/ethnic groups or specific regions of the United States (Turner and Gil, 2002). Investigations from adult samples focused on emigrants from Mexico (Borges et al., 2009, 2012), the former Soviet Union (Guarino et al., 2012), Asia (Moloney et al., 2008; Wong et al., 2007), and Latin America (Alegría et al., 2008; Ojeda et al., 2008) have found trends similar to those identified in younger samples. Studies of adults in the United States have been hampered by their inability to examine the stability of the relationship between substance use and immigration across multiple immigrant generations or among emigrants from various regions of the world (Johnson et al., 2002; Li and Wen, 2013; Salas-Wright and Vaughn, 2014).
Despite the growing number of studies on immigration and substance use, several important shortcomings persist. First, the bulk of research conducted on the immigrant paradox has been focused on substance use among adolescents and young adults. Although substance use among youth is undoubtedly an important issue, evidence suggests that substance use disorders persist well beyond these early developmental periods (Kessler et al., 2007). Second, studies that have focused on immigration and substance use among adult populations have tended to focus on emigrants from particular nations (e.g., Mexico) or regions (e.g., Asia) of origin, or geographically restricted areas of the United States (e.g., South Florida), rather than immigrants in general. Third, studies of the immigrant paradox for substance use have typically not examined any potential differences that might emerge between first- and second-generation emigrants or among emigrants from various regions of the world. In all, despite the advances made in recent years, there remains a need for a comprehensive examination of the multigenerational and global links between immigration and substance use among adults in the United States.
Present study
The present study uses data from a population-based study (i.e., the National Epidemiologic Survey on Alcohol and Related Conditions [NESARC]) to address these gaps in the literature. NESARC is an appropriate data source to address the shortcomings of the current literature because of its far-reaching scope and inclusion of immigrants across multiple generations and various global regions. Specifically, we examined the prevalence of substance use disorders among first- and second-generation immigrants and compared these with the prevalence among native-born Americans. Cognizant of the developmental implications linked with immigration, we also examined effects across age at immigrant arrival and duration in the United States. Last, we examined the stability of these associations by probing the links between immigration and substance use disorders among immigrants representing major regions of the world.
Method
Participants
Study findings are based on the NESARC, which is a nationally representative sample of non-institutionalized U.S. residents ages 18 years and older. We relied primarily on data from Wave II (2004–2005) of the NESARC; however, data from Wave I (2001–2002) were also analyzed as part of a sensitivity analysis conducted to assess the stability of study findings. The design and methods are presented in a summarized form; however, a more detailed description of the NESARC procedures is available elsewhere (Grant et al., 2003). The survey gathered background data and extensive information about substance use disorders from individuals living in households and group settings such as shelters, college dormitories, and group homes in all 50 states and the District of Columbia. The NESARC used a multistage cluster sampling design, oversampling young adults, Hispanics, and African Americans to ensure appropriate representation of racial and ethnic subgroups and to obtain reliable statistical estimation in these subpopulations. The response rate for Wave I data was 81% and for Wave II was 87%, with a cumulative response rate of 70% for both waves. The current study restricted analyses to adults between ages 18 and 49 years (n = 19,073).
Diagnostic assessment
Data were collected through face-to-face structured psychiatric interviews conducted by U.S. Census workers trained by the National Institute on Alcohol Abuse and Alcoholism and the U.S. Census Bureau. Interviewers administered the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV version (AUDADIS-IV), which provides diagnoses for clinical, personality, and substance use disorders. The AUDADIS-IV has been shown to have good to excellent reliability in assessing mental disorders in the general population (Grant et al., 1995; Hasin et al., 1997). Participants had the option of completing the NESARC interview in English, Spanish, or one of four Asian languages (Mandarin, Cantonese, Korean, and Vietnamese).
Measures
Immigrant status.
Respondents were asked whether they and their parents were born in the United States. Respondents who reported having been born outside the United States (n = 3,338) were classified as first-generation immigrants. Respondents who reported that they had been born in the United States but their parents had been born outside the United States (n = 2,515) were classified as second-generation immigrants. Respondents who reported that they and their parents were born in the United States were considered non-immigrants/native-born Americans (n = 15,733).
Substance use disorders.
Using the AUDADIS-IV, substance use disorders (abuse or dependence) with a prevalence of at least 2% in the general population were examined. These include alcohol use disorder, cannabis use disorder, and five additional illicit drug disorders (i.e., cocaine, stimulants, sedatives, tranquilizers, and opioids). For each of these disorders, respondents who were identified as having met diagnostic criteria during their lifetime were coded as 1, and all other individuals were coded as 0.
Sociodemographic and behavioral controls.
The following demographic variables were included as controls: age, gender, race/ethnicity, household income, education level, marital status, region of the United States, and urbanicity. In addition, in examining the associations between immigrant status and substance use disorders, we controlled for parental antisocial influence (i.e., mother or father had behavioral problems), parental substance use problems (i.e., mother or father ever had problems with alcohol or other drugs), and lifetime diagnoses of clinical and personality disorders.
Analysis
First, logistic regression analyses were conducted that examined the sociodemographic characteristics of first- and second-generation immigrants to the United States. Second, logistic regression analyses were conducted that compared non-immigrants with first- and second-generation immigrants in terms of substance use disorders. Third, multinomial regression analyses were conducted that compared non-immigrants with second-generation immigrants, childhood immigrants (e.g., immigrated before age 13 years), adolescent immigrants (i.e., immigrated between ages 13 and 17 years), and adult immigrants (i.e., immigrated after age 18 years). Last, predicted probabilities of substance use disorders were calculated in reference to age at the time of immigration and number of years lived in the United States. Adjusted odds ratios (AORs) and adjusted risk ratios were considered to be statistically significant if the associated confidence intervals did not cross the 1.0 threshold. For all statistical analyses, weighted prevalence estimates and standard errors were computed using Stata 13.1 SE software (StataCorp LP, College Station, TX). This system implements a Taylor series linearization to adjust standard errors of estimates for complex survey sampling design effects including clustered data.
Results
Sociodemographic characteristics of first- and second-generation immigrants
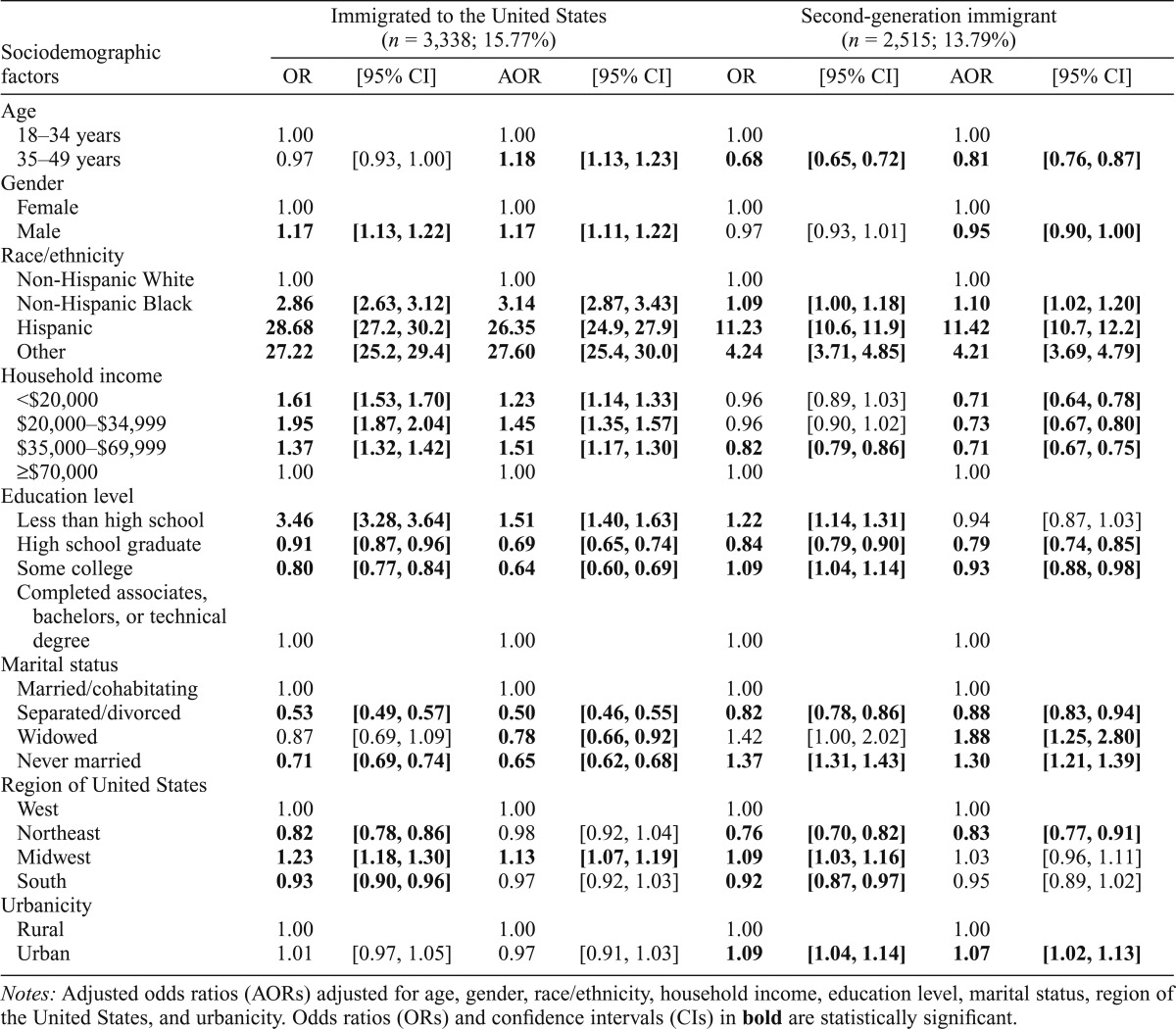
Table 1 displays the sociodemographic characteristics of first- and second-generation immigrant adults between ages 18 and 49 years in the United States. Compared with native-born Americans, first-generation immigrants were significantly more likely to be between ages 35 and 49 years (AOR = 1.18, 95% CI [1.13, 1.23]), to be male (AOR = 1.17, 95% CI [1.11, 1.22]), to be a racial/ethnic minority, to reside in a household with an income less than U.S. $70,000 per year, and to be less likely to have graduated from high school (AOR = 0.69, 95% CI [0.65, 0.74]). Compared with native-born Americans, second-generation immigrants were significantly less likely to be between ages 35 and 49 years (AOR = 0.81, 95% CI [0.76, 0.87]), to be male (AOR = 0.95, 95% CI [0.90, 1.00]), to reside in a household with an income less than $70,000 per year, to be more likely a racial/ethnic minority, and to reside in an urban area (AOR = 1.07, 95% CI [1.02, 1.13]).
Table 1.
Sociodemographic characteristics of first and second-generation immigrants to the United States compared with native-born Americans
| Sociodemographic factors | Immigrated to the United States (n = 3,338; 15.77%) |
Second-generation immigrant (n = 2,515; 13.79%) |
||||||
| OR | [95% CI] | AOR | [95% CI] | OR | [95% CI] | AOR | [95% CI] | |
| Age | ||||||||
| 18–34 years | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 35–49 years | 0.97 | [0.93, 1.00] | 1.18 | [1.13, 1.23] | 0.68 | [0.65, 0.72] | 0.81 | [0.76, 0.87] |
| Gender | ||||||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Male | 1.17 | [1.13, 1.22] | 1.17 | [1.11, 1.22] | 0.97 | [0.93, 1.01] | 0.95 | [0.90, 1.00] |
| Race/ethnicity | ||||||||
| Non-Hispanic White | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Non-Hispanic Black | 2.86 | [2.63, 3.12] | 3.14 | [2.87, 3.43] | 1.09 | [1.00, 1.18] | 1.10 | [1.02, 1.20] |
| Hispanic | 28.68 | [27.2, 30.2] | 26.35 | [24.9, 27.9] | 11.23 | [10.6, 11.9] | 11.42 | [10.7, 12.2] |
| Other | 27.22 | [25.2, 29.4] | 27.60 | [25.4, 30.0] | 4.24 | [3.71, 4.85] | 4.21 | [3.69, 4.79] |
| Household income | ||||||||
| <$20,000 | 1.61 | [1.53, 1.70] | 1.23 | [1.14, 1.33] | 0.96 | [0.89, 1.03] | 0.71 | [0.64, 0.78] |
| $20,000–$34,999 | 1.95 | [1.87, 2.04] | 1.45 | [1.35, 1.57] | 0.96 | [0.90, 1.02] | 0.73 | [0.67, 0.80] |
| $35,000–$69,999 | 1.37 | [1.32, 1.42] | 1.51 | [1.17, 1.30] | 0.82 | [0.79, 0.86] | 0.71 | [0.67, 0.75] |
| ≥$70,000 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Education level | ||||||||
| Less than high school | 3.46 | [3.28, 3.64] | 1.51 | [1.40, 1.63] | 1.22 | [1.14, 1.31] | 0.94 | [0.87, 1.03] |
| High school graduate | 0.91 | [0.87, 0.96] | 0.69 | [0.65, 0.74] | 0.84 | [0.79, 0.90] | 0.79 | [0.74, 0.85] |
| Some college | 0.80 | [0.77, 0.84] | 0.64 | [0.60, 0.69] | 1.09 | [1.04, 1.14] | 0.93 | [0.88, 0.98] |
| Completed associates, bachelors, or technical degree | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Marital status | ||||||||
| Married/cohabitating | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Separated/divorced | 0.53 | [0.49, 0.57] | 0.50 | [0.46, 0.55] | 0.82 | [0.78, 0.86] | 0.88 | [0.83, 0.94] |
| Widowed | 0.87 | [0.69, 1.09] | 0.78 | [0.66, 0.92] | 1.42 | [1.00, 2.02] | 1.88 | [1.25, 2.80] |
| Never married | 0.71 | [0.69, 0.74] | 0.65 | [0.62, 0.68] | 1.37 | [1.31, 1.43] | 1.30 | [1.21, 1.39] |
| Region of United States | ||||||||
| West | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Northeast | 0.82 | [0.78, 0.86] | 0.98 | [0.92, 1.04] | 0.76 | [0.70, 0.82] | 0.83 | [0.77, 0.91] |
| Midwest | 1.23 | [1.18, 1.30] | 1.13 | [1.07, 1.19] | 1.09 | [1.03, 1.16] | 1.03 | [0.96, 1.11] |
| South | 0.93 | [0.90, 0.96] | 0.97 | [0.92, 1.03] | 0.92 | [0.87, 0.97] | 0.95 | [0.89, 1.02] |
| Urbanicity | ||||||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Urban | 1.01 | [0.97, 1.05] | 0.97 | [0.91, 1.03] | 1.09 | [1.04, 1.14] | 1.07 | [1.02, 1.13] |
Notes: Adjusted odds ratios (AORs) adjusted for age, gender, race/ethnicity, household income, education level, marital status, region of the United States, and urbanicity. Odds ratios (ORs) and confidence intervals (CIs) in bold are statistically significant.
Are first- and second-generation immigrants less likely to have a substance use disorder?
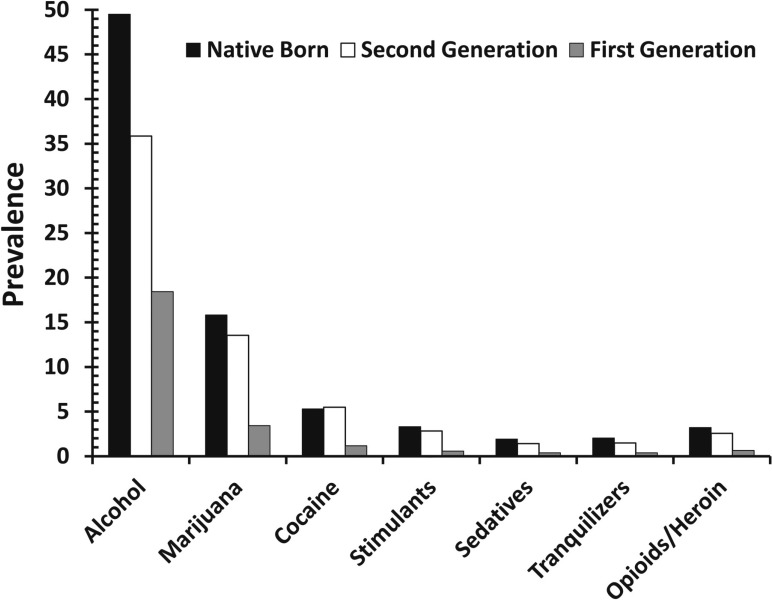
Figure 1 displays the prevalence of lifetime substance use disorders among native-born Americans and first- and second-generation immigrant adults. For all disorders examined in this study, the prevalence of morbidity was lowest among first-generation immigrants followed by second-generation immigrants and, last, native-born Americans. A steady increase in the prevalence of lifetime alcohol use disorder can be identified in comparing first-generation immigrants (18.43%), second-generation immigrants (35.86%), and native-born Americans (49.49%). Similarly, the prevalence of cannabis use disorder is markedly low among first-generation immigrants (3.43%) compared with both second-generation immigrants (13.54%) and native-born Americans (15.82%). A similar pattern was observed for the other illicit drug use disorders examined in this study, including cocaine, stimulant, sedative, tranquilizer, and opioid use disorders.
Figure 1.
Prevalence of lifetime substance use disorders among native-born Americans and first- and second-generation immigrant adults
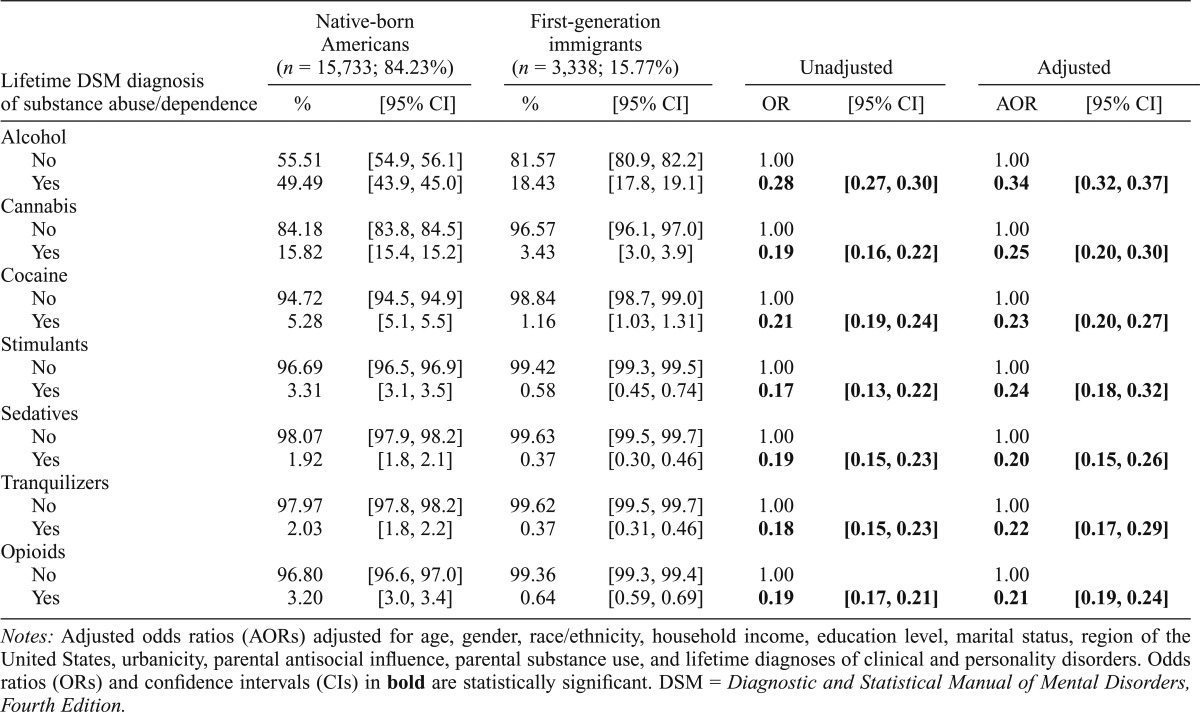
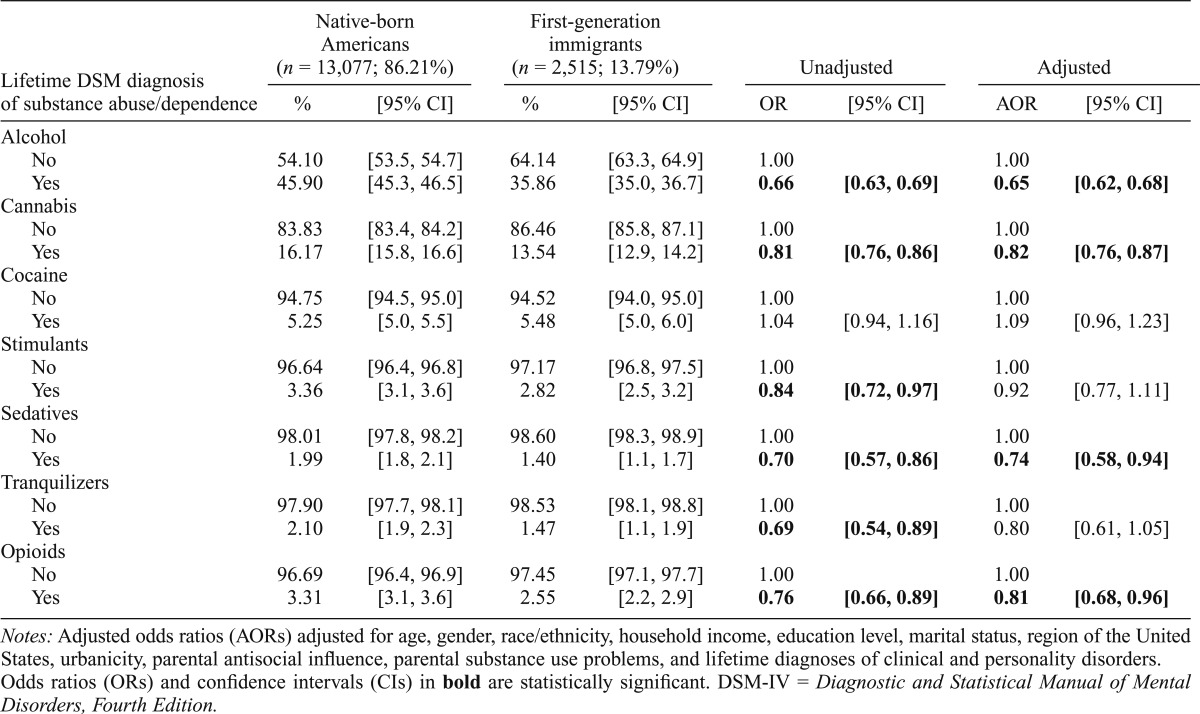
Tables 2 and 3 compare the prevalence of substance use disorders of native-born Americans with that of first- and second-generation immigrants to the United States, respectively. When we controlled for sociodemographic factors as well as parental antisocial influence, parental substance use, and lifetime diagnoses of clinical and personality disorders, first-generation immigrants were between roughly three and five times less likely than second-generation immigrants to have met criteria for all substance use disorders examined in this study. When we controlled for the same list of confounds, second-generation immigrants were significantly less likely than native-born Americans to have met criteria for alcohol (AOR = 0.65, 95% CI [0.62, 0.68]), cannabis (AOR = 0.82, 95% CI [0.76, 0.87]), sedative (AOR = 0.74, 95% CI [0.58, 0.94]), and opioid (AOR = 0.81, 95% CI [0.68, 0.96]) use disorders. However, in contrast to first-generation immigrants, no significant relationships were observed in terms of cocaine, stimulant, or tranquilizer use disorders. Moreover, the effect sizes for the significant associations identified between immigrant status and lifetime diagnoses of substance use disorders were far greater among first-generation immigrants (AORs between 0.21 and 0.34) than second-generation immigrants (AORs between 0.65 and 0.82).
Table 2.
Lifetime substance use disorders among native-born Americans and first-generation immigrants to the United States
| Lifetime DSM diagnosis of substance abuse/dependence | Native-born Americans (n = 15,733; 84.23%) |
First-generation immigrants (n = 3,338; 15.77%) |
Unadjusted |
Adjusted |
||||
| % | [95% CI] | % | [95% CI] | OR | [95% CI] | AOR | [95% CI] | |
| Alcohol | ||||||||
| No | 55.51 | [54.9, 56.1] | 81.57 | [80.9, 82.2] | 1.00 | 1.00 | ||
| Yes | 49.49 | [43.9, 45.0] | 18.43 | [17.8, 19.1] | 0.28 | [0.27, 0.30] | 0.34 | [0.32, 0.37] |
| Cannabis | ||||||||
| No | 84.18 | [83.8, 84.5] | 96.57 | [96.1, 97.0] | 1.00 | 1.00 | ||
| Yes | 15.82 | [15.4, 15.2] | 3.43 | [3.0, 3.9] | 0.19 | [0.16, 0.22] | 0.25 | [0.20, 0.30] |
| Cocaine | ||||||||
| No | 94.72 | [94.5, 94.9] | 98.84 | [98.7, 99.0] | 1.00 | 1.00 | ||
| Yes | 5.28 | [5.1, 5.5] | 1.16 | [1.03, 1.31] | 0.21 | [0.19, 0.24] | 0.23 | [0.20, 0.27] |
| Stimulants | ||||||||
| No | 96.69 | [96.5, 96.9] | 99.42 | [99.3, 99.5] | 1.00 | 1.00 | ||
| Yes | 3.31 | [3.1, 3.5] | 0.58 | [0.45, 0.74] | 0.17 | [0.13, 0.22] | 0.24 | [0.18, 0.32] |
| Sedatives | ||||||||
| No | 98.07 | [97.9, 98.2] | 99.63 | [99.5, 99.7] | 1.00 | 1.00 | ||
| Yes | 1.92 | [1.8, 2.1] | 0.37 | [0.30, 0.46] | 0.19 | [0.15, 0.23] | 0.20 | [0.15, 0.26] |
| Tranquilizers | ||||||||
| No | 97.97 | [97.8, 98.2] | 99.62 | [99.5, 99.7] | 1.00 | 1.00 | ||
| Yes | 2.03 | [1.8, 2.2] | 0.37 | [0.31, 0.46] | 0.18 | [0.15, 0.23] | 0.22 | [0.17, 0.29] |
| Opioids | ||||||||
| No | 96.80 | [96.6, 97.0] | 99.36 | [99.3, 99.4] | 1.00 | 1.00 | ||
| Yes | 3.20 | [3.0, 3.4] | 0.64 | [0.59, 0.69] | 0.19 | [0.17, 0.21] | 0.21 | [0.19, 0.24] |
Notes: Adjusted odds ratios (AORs) adjusted for age, gender, race/ethnicity, household income, education level, marital status, region of the United States, urbanicity, parental antisocial influence, parental substance use, and lifetime diagnoses of clinical and personality disorders. Odds ratios (ORs) and confidence intervals (CIs) in bold are statistically significant. DSM = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Table 3.
Lifetime substance use disorders among native-born Americans and second-generation immigrants to the United States
| Lifetime DSM diagnosis of substance abuse/dependence | Native-born Americans (n = 13,077; 86.21%) |
First-generation immigrants (n = 2,515; 13.79%) |
Unadjusted |
Adjusted |
||||
| % | [95% CI] | % | [95% CI] | OR | [95% CI] | AOR | [95% CI] | |
| Alcohol | ||||||||
| No | 54.10 | [53.5, 54.7] | 64.14 | [63.3, 64.9] | 1.00 | 1.00 | ||
| Yes | 45.90 | [45.3, 46.5] | 35.86 | [35.0, 36.7] | 0.66 | [0.63, 0.69] | 0.65 | [0.62, 0.68] |
| Cannabis | ||||||||
| No | 83.83 | [83.4, 84.2] | 86.46 | [85.8, 87.1] | 1.00 | 1.00 | ||
| Yes | 16.17 | [15.8, 16.6] | 13.54 | [12.9, 14.2] | 0.81 | [0.76, 0.86] | 0.82 | [0.76, 0.87] |
| Cocaine | ||||||||
| No | 94.75 | [94.5, 95.0] | 94.52 | [94.0, 95.0] | 1.00 | 1.00 | ||
| Yes | 5.25 | [5.0, 5.5] | 5.48 | [5.0, 6.0] | 1.04 | [0.94, 1.16] | 1.09 | [0.96, 1.23] |
| Stimulants | ||||||||
| No | 96.64 | [96.4, 96.8] | 97.17 | [96.8, 97.5] | 1.00 | 1.00 | ||
| Yes | 3.36 | [3.1, 3.6] | 2.82 | [2.5, 3.2] | 0.84 | [0.72, 0.97] | 0.92 | [0.77, 1.11] |
| Sedatives | ||||||||
| No | 98.01 | [97.8, 98.2] | 98.60 | [98.3, 98.9] | 1.00 | 1.00 | ||
| Yes | 1.99 | [1.8, 2.1] | 1.40 | [1.1, 1.7] | 0.70 | [0.57, 0.86] | 0.74 | [0.58, 0.94] |
| Tranquilizers | ||||||||
| No | 97.90 | [97.7, 98.1] | 98.53 | [98.1, 98.8] | 1.00 | 1.00 | ||
| Yes | 2.10 | [1.9, 2.3] | 1.47 | [1.1, 1.9] | 0.69 | [0.54, 0.89] | 0.80 | [0.61, 1.05] |
| Opioids | ||||||||
| No | 96.69 | [96.4, 96.9] | 97.45 | [97.1, 97.7] | 1.00 | 1.00 | ||
| Yes | 3.31 | [3.1, 3.6] | 2.55 | [2.2, 2.9] | 0.76 | [0.66, 0.89] | 0.81 | [0.68, 0.96] |
Notes: Adjusted odds ratios (AORs) adjusted for age, gender, race/ethnicity, household income, education level, marital status, region of the United States, urbanicity, parental antisocial influence, parental substance use problems, and lifetime diagnoses of clinical and personality disorders. Odds ratios (ORs) and confidence intervals (CIs) in bold are statistically significant. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
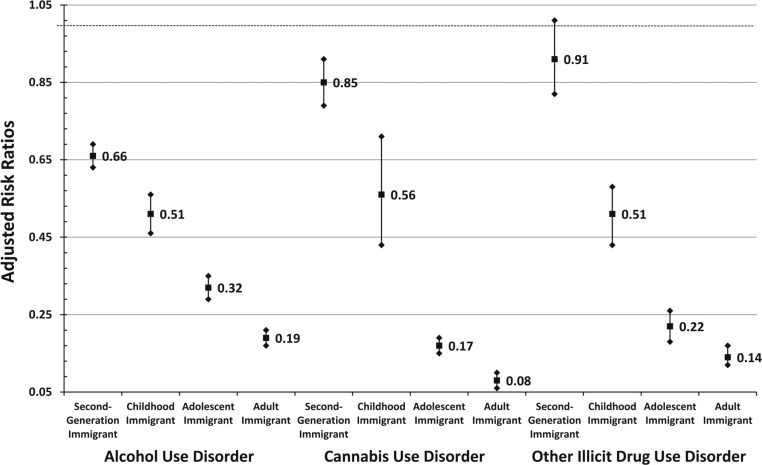
Immigrant generation and age at the time of immigration
Figure 2 adds additional nuance to the examination of the relationship between immigrant status and substance use disorders by comparing the prevalence of substance use disorders of native-born Americans with that of first- and second-generation immigrants who came as children (i.e., under age 13 years), adolescents (i.e., between ages 13 and 17 years), and adults (i.e., age 18 years or older). When we controlled for sociodemographic, parental, and mental health (i.e., lifetime diagnoses of clinical and personality disorders) factors, immigrants who came to the United States as adults were the least likely to have ever met criteria for a substance use disorder followed sequentially by immigrants who came as adolescents, immigrants who came as children, and, finally, second-generation immigrants. Of note, the effect sizes for these relationships were particularly robust for immigrants who came as adults (between roughly five and seven times less likely to have met criteria for a substance use disorder) or as adolescents (between roughly three and five times less likely to have met criteria for a substance use disorder). Supplementary analyses revealed that although the effects were stronger for females than for males, a similar pattern of associations was observed across gender.
Figure 2.
Adjusted risk ratios for substance use disorders among first- and second-generation immigrants by developmental age at the time of immigration with native-born Americans as the reference group. Squares represent the adjusted risk ratios, and the diamonds represent the upper and lower limits of the 95% confidence intervals.
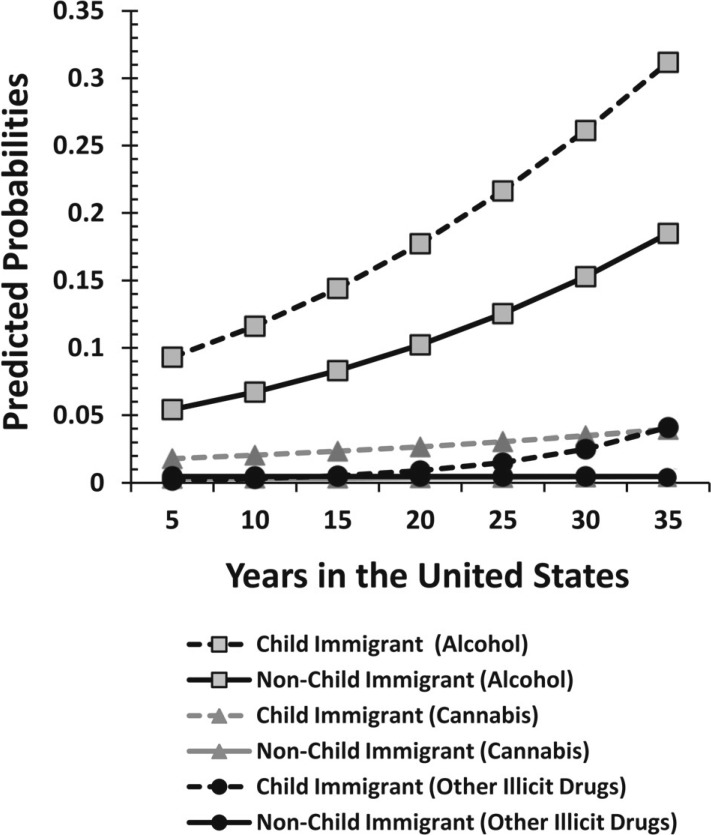
Age at the time of immigration and duration in the United States
Figure 3 presents the predicted probabilities for substance use disorders by age at the time of immigration and total duration in the United States. The probability of child immigrants (i.e., immigrated before age 13 years) and nonchild immigrants (i.e., immigrated at age 13 years or older) meeting the criteria for alcohol abuse or dependence steadily increased with the number of years spent in the United States. Compared with immigrants who came to the United States after childhood, child immigrants were found to have higher probabilities of alcohol use disorders at the outset and to have increasingly high probabilities over time. Supplementary analyses revealed that, although the predicted probabilities for males were higher than those for females, similar patterns were observed across gender. For cannabis use disorder, although the predicted probability of nonchild immigrants meeting criteria for abuse or dependence remained steadily low with increased duration, the predicted probability for child immigrants is higher at the outset and increases slightly over time. Finally, as for other illicit drug use disorders, the predicted probability for child and nonchild immigrants is very similar between 5 and 20 years of duration in the United States; however, after 25 years of duration, the predicted probabilities for child immigrants rapidly increase with time, whereas the predicted probability for nonchild immigrants remains flat. The rapid increases among child immigrants are observed for male but not female immigrants.
Figure 3.
Predicted probabilities of substance use disorders by age at immigration and years in the United States
Prevalence of substance use disorders among immigrants across major world regions
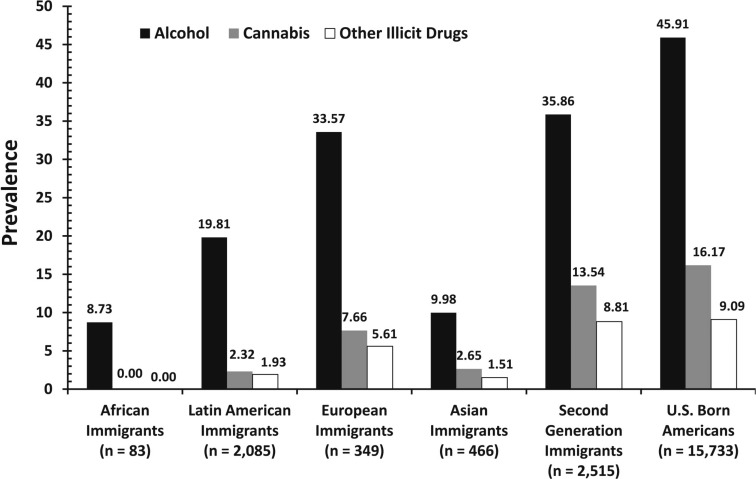
Figure 4 presents the prevalence of alcohol, cannabis, and other illicit drug (i.e., cocaine, stimulants, sedatives, tranquilizers, and opioids) use disorders among first-generation emigrants from four major global regions as well as that of second-generation emigrants and native-born Americans. Across the board, the prevalence of substance use disorders of native-born Americans and second-generation immigrants was greater than the prevalence identified among first-generation emigrants from Africa, Latin America, Europe, and Asia. European immigrants had the highest prevalence of alcohol use disorders (33.57%), followed by Latin American (19.81%), Asian (9.98%), and African (8.73%) immigrants. For cannabis and other illicit drug use disorders, the highest prevalence was also observed among European immigrants (cannabis: 7.66%; other illicit drug: 5.61%). The prevalence of cannabis and other illicit drug use disorders was quite low among Latin American (cannabis: 2.32%; other illicit drug: 1.93%) and Asian (cannabis: 2.65%; other illicit drug: 1.51%) immigrants. No African immigrants were identified as meeting the criteria for cannabis or other illicit drug abuse or dependence.
Figure 4.
Prevalence of alcohol, marijuana, and other illicit drug use disorders among native-born Americans and immigrant adults by global region
Sensitivity analysis
Results presented above are for Wave II data; however, we assessed the stability of the results using Wave I data collected 3 years prior. Results of logistic regression analyses for first-generation immigrants at Wave I largely mirrored the overall pattern found for Wave II. Namely, when we controlled for the same list of sociodemographic factors used above, immigrants were found to be roughly three to five times less likely than non-immigrants to meet the diagnostic criteria for all substance disorders examined in the study. Sensitivity analysis could not be conducted for second-generation immigrants because this information was not available in the Wave I data.
Discussion
The present study examined the links between immigration and substance use disorders by drawing from nationally representative samples of first- and second-generation immigrants and native-born American adults in the United States. Study findings suggest a severity-based gradient in which the prevalence of substance use disorders is highest among native-born Americans, slightly lower among second-generation immigrants, and markedly lower among first-generation immigrants. Second-generation immigrants were significantly less likely to meet the criteria for alcohol, marijuana, sedative, and opiates/heroin use disorders; however, effects were relatively modest and no difference was identified for several important substance use disorders (i.e., cocaine, stimulants, and tranquilizers). In contrast, first-generation immigrants were roughly three to five times less likely to meet the criteria for substance abuse/dependence for all the substances examined in this study. Moreover, further inspection revealed that age at immigrant arrival may also be of relevance because effects were largest among individuals who immigrated at later developmental stages. Immigrants who arrived at later developmental stages were also at lower risk for developing substance use disorders with greater total duration in the United States. In all, these results provide strong evidence in support of a multigenerational immigrant paradox, because second-generation immigrants were less likely than native-born Americans to meet the criteria for substance use disorders but to a lesser degree than first-generation immigrants who arrived during childhood, adolescence, and adulthood.
We also examined the relationship between immigration and substance use by comparing the prevalence of substance use disorders among first-generation emigrants from Asia, Africa, Europe, and Latin America with those of second-generation and native-born Americans. With respect to alcohol use disorder, particularly robust differences were observed for African and Asian immigrants in contrast with U.S.-born Americans. Indeed, native-born Americans (45.9%) were more than four times more likely than were emigrants from Africa (8.7%) and Asia (10.0%) to have met the criteria for alcohol abuse or dependence. Very large differences were also observed between African, Asian, and Latin American immigrants in contrast with native-born Americans in terms of cannabis and other illicit drug use disorders. Of note, the smallest differences in the prevalence of substance use disorders were observed between European immigrants and native-born Americans. This pattern of findings is consistent with recent studies contrasting the prevalence of other high-risk and antisocial behaviors between immigrants and native-born Americans across various regions of the world (Vaughn et al., 2014b). Overall, this consistent pattern of findings across major world regions serves to further substantiate the evidence of the immigrant paradox with respect to substance use disorders.
Study limitations
Despite the contributions of the present investigation, findings should be interpreted in light of several limitations. First, the temporal ordering of immigration and substance use disorders is not ideal given that the NESARC is not a true longitudinal study. Specifically, although we made use of data from both Wave I (2001–2002) and Wave II (2004–2005) of the NESARC, all analyses were cross-sectional in nature. Second, although the psychiatric interview format (AUDADIS-IV) is considered to have good to excellent reliability in assessing substance use disorders in the general population (Grant et al., 1995; Hasin et al., 1997), it may have introduced culture-related biases for emigrants from various culturally distinct regions of the world. Caution should be exercised in the interpretation of study findings, because it is possible that respondents from distinct cultural backgrounds may have interpreted and answered sensitive questions concerned with substance use and immigration status differently. Last, the NESARC does not include important precipitating, situational, contextual, or biological variables, which would facilitate a fuller examination of the relationship between immigration and substance use disorders. Future research on the links between immigration and substance use disorders would benefit from the incorporation of such factors into study designs.
Conclusions
Although previous research has examined the links between immigration and substance use, the present study is among the first to do so across multiple generations and multiple global regions with a nationally representative sample of adults in the United States. Results provide evidence in support of a multigenerational immigrant paradox in which first-generation immigrants and, to a lesser extent, second-generation immigrants are less likely than native-born Americans to meet the criteria for a host of substance use disorders. Moreover, the findings suggest that the older immigrants are at the time of immigration, the more robust the relationship between immigration and substance use disorders. These findings were consistent when examined among emigrants from major regions of the world including Africa, Asia, Europe, and Latin America. In all, consistent with a broad body of literature examining the links between the immigrant paradox and health outcomes, results suggest that nativity and age at arrival are significant factors related to substance use disorders among first- and second-generation immigrants in the United States.
Footnotes
This research was supported by National Institute on Drug Abuse Grant R25 DA026401.
References
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Meng X-L. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida J, Johnson RM, Matsumoto A, Godette DC. Substance use, generation and time in the United States: The modifying role of gender for immigrant urban adolescents. Social Science & Medicine. 2012;75:2069–2075. doi: 10.1016/j.socscimed.2012.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacio GA, Mays VM, Lau AS. Drinking initiation and problematic drinking among Latino adolescents: Explanations of the immigrant paradox. Psychology of Addictive Behaviors. 2013;27:14–22. doi: 10.1037/a0029996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake SM, Ledsky R, Goodenow C, O’Donnell L. Recency of immigration, substance use, and sexual behavior among Massachusetts adolescents. American Journal of Public Health. 2001;91:794–798. doi: 10.2105/ajph.91.5.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Medina-Mora ME, Orozco R, Fleiz C, Cherpitel C, Breslau J. The Mexican migration to the United States and substance use in northern Mexico. Addiction. 2009;104:603–611. doi: 10.1111/j.1360-0443.2008.02491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Rafful C, Benjet C, Tancredi DJ, Saito N, Aguilar-Gaxiola S, Breslau J. Mexican immigration to the US and alcohol and drug use opportunities: Does it make a difference in alcohol and/or drug use? Drug and Alcohol Dependence, 125, Supplement. 2012;1:S4–S11. doi: 10.1016/j.drugalcdep.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bui HN. Racial and ethnic differences in the immigrant paradox in substance use. Journal of Immigrant and Minority Health. 2013;15:866–881. doi: 10.1007/s10903-012-9670-y. [DOI] [PubMed] [Google Scholar]
- Charles CZ. New York, NY: Russell Sage Foundation; 2006. Won’t you be my neighbor? Race, class, and residence in Los Angeles. [Google Scholar]
- Coll C, Patton F, Marks A, Dimitrova R, Yang R, Suarez GA, Patrico A. Understanding the immigrant paradox in youth: Developmental and contextual considerations. In: Masten AS, Liebkind K, Hernandez DJ, editors. Realizing the potential of immigrant youth. New York, NY: Cambridge University Press; 2012. pp. 159–180. [Google Scholar]
- De La Rosa M, Dillon E R, Sastre F, Babino R. Alcohol use among recent Latino immigrants before and after immigration to the United States. American Journal on Addictions. 2013;22:162–168. doi: 10.1111/j.1521-0391.2013.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gfroerer JC, Tan LL. Substance use among foreign-born youths in the United States: Does the length of residence matter? American Journal of Public Health. 2003;93:1892–1895. doi: 10.2105/ajph.93.11.1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson E S, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Guarino H, Moore SK, Marsch LA, Florio S. The social production of substance abuse and HIV/HCV risk: An exploratory study of opioid-using immigrants from the former Soviet Union living in New York City. Substance Abuse Treatment, Prevention, and Policy. 2012;7:2–2. doi: 10.1186/1747-597X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker K, Chu J, Leung C, Marra R, Pirie A, Brahimi M, Marlin RP. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Social Science & Medicine. 2011;73:586–594. doi: 10.1016/j.socscimed.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): Reliability of alcohol and drug modules in a clinical sample. Drug and Alcohol Dependence. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Johnson TP, VanGeest JB, Cho YI. Migration and substance use: Evidence from the U.S. National Health Interview Survey. Substance Use & Misuse. 2002;37:941–972. doi: 10.1081/ja-120004160. [DOI] [PubMed] [Google Scholar]
- Kennedy S, Kidd MP, McDonald JT, Biddle N. The healthy immigrant effect: Patterns and evidence from four countries. Journal of International Migration and Integration. 2014 Advance online publication. [Google Scholar]
- Kessler RC, Angermeyer M, Anthony JC, de Graaf R, Demyttenaere K, Gasquet I, Üstün TB. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- Kopak AM. The relative importance of immigrant generation for Mexican Americans’ alcohol and tobacco use from adolescence to early adulthood. Journal of Immigrant and Minority Health. 2013;15:569–576. doi: 10.1007/s10903-012-9631-5. [DOI] [PubMed] [Google Scholar]
- Li K, Wen M. Substance use, age at migration, and length of residence among adult immigrants in the United States. Journal of Immigrant and Minority Health. 2013, August 8 doi: 10.1007/s10903-013-9887-4. Advance online publication. Retrieved from http://download.springer.com/static/pdf/185/art%253A10.1007%252Fs10903-013-9887-4.pdf?auth66=1408558331_abc59eedd340f7448f7204dcfbd67d0f&ext=.pdf. [DOI] [PubMed] [Google Scholar]
- Maldonado-Molina MM, Reingle JM, Jennings WG, Prado G. Drinking and driving among immigrant and US-born Hispanic young adults: Results from a longitudinal and nationally representative study. Addictive Behaviors. 2011;36:381–388. doi: 10.1016/j.addbeh.2010.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moloney M, Hunt G, Evans K. Asian American identity and drug consumption: From acculturation to normalization. Journal of Ethnicity in Substance Abuse. 2008;7:376–403. doi: 10.1080/15332640802508168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojeda VD, Patterson TL, Strathdee SA. The influence of perceived risk to health and immigration-related characteristics on substance use among Latino and other immigrants. American Journal of Public Health. 2008;98:862–868. doi: 10.2105/AJPH.2006.108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña JB, Wyman PA, Brown CH, Matthieu MM, Olivares TE, Hartel D, Zayas LH. Immigration generation status and its association with suicide attempts, substance use, and depressive symptoms among Latino adolescents in the USA. Prevention Science. 2008;9:299–310. doi: 10.1007/s11121-008-0105-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: New findings from the Mexican Family Life Survey. American Journal of Public Health. 2008;98:78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Clark TT, Vaughn MG, Córdova D. Profiles of acculturation among Hispanics in the United States: Links with discrimination and substance use. Social Psychiatry and Psychiatric Epidemiology. 2014a doi: 10.1007/s00127-014-0889-x. Advance online publication. Retrieved from http://download.springer.com/static/pdf/24/art%253A10.1007%252Fs00127-014-0889-x.pdf?auth66=1408558824_d2fc05d0ff74d96fc6904dda7e92e0fb&ext=.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Kagotho N, Vaughn MG. Mood, anxiety, and personality disorders among first and second-generation immigrants to the United States. Psychiatry Research. 2014b doi: 10.1016/j.psychres.2014.08.045. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG. A “refugee paradox” for substance use disorders? Drug and Alcohol Dependence. 2014;142:345–349. doi: 10.1016/j.drugalcdep.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Unger JB, Des Rosiers SE, Lorenzo-Blanco EI, Zamboanga BL, Huang S, Szapocznik J. Domains of acculturation and their effects on substance use and sexual behavior in recent Hispanic immigrant adolescents. Prevention Science. 2014;15:385–396. doi: 10.1007/s11121-013-0419-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: Implications for theory and research. American Psychologist. 2010;65:237–251. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Weisskirch RS, Zamboanga BL, Castillo LG, Ham LS, Huynh Q-L, Cano MA. Dimensions of acculturation: Associations with health risk behaviors among college students from immigrant families. Journal of Counseling Psychology. 2011;58:27–41. doi: 10.1037/a0021356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, Gil AG. Psychiatric and substance use disorders in South Florida: Racial/ethnic and gender contrasts in a young adult cohort. Archives of General Psychiatry. 2002;59:43–50. doi: 10.1001/archpsyc.59.1.43. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, Cooper-Sadlo S, Maynard BR, Larson MJ. Are immigrants more likely than native-born Americans to perpetrate intimate partner violence? Journal of Interpersonal Violence. 2014a doi: 10.1177/0886260514549053. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, DeLisi M, Maynard BR. The immigrant paradox: Immigrants are less antisocial than native-born Americans. Social Psychiatry and Psychiatric Epidemiology. 2014b;49:1129–1137. doi: 10.1007/s00127-013-0799-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, Maynard BR, Qian Z, Terzis L, Kusow K, DeLisi M. Criminal epidemiology and the immigrant paradox: Intergenerational discontinuity in violence and antisocial behavior among immigrants. Journal of Criminal Justice. in press [Google Scholar]
- Wong FY, Huang ZJ, Thompson EE, De Leon JM, Shah MS, Park RJ, Do TD. Substance use among a sample of foreign-and US-born Southeast Asians in an urban setting. Journal of Ethnicity in Substance Abuse. 2007;6:45–66. doi: 10.1300/J233v06n01_04. [DOI] [PubMed] [Google Scholar]