Abstract
Objective:
Although recovery increasingly guides substance use disorder services and policy, definitions of recovery continue to lack specificity, thereby hindering measure development and research. The goal of this study was to move the substance use disorders field beyond broad definitions by empirically identifying the domains and specific elements of recovery as experienced by persons in recovery from diverse pathways.
Method:
An Internet-based survey was completed by 9,341 individuals (54% female) who self-identified as being in recovery, recovered, in medication-assisted recovery, or as having had a problem with alcohol or drugs (but no longer do). Respondents were recruited via extensive outreach with treatment and recovery organizations, electronic media, and self-help groups. The survey included 47 recovery elements developed through qualitative work followed by an iterative reduction process. Exploratory and confirmatory factor analyses were conducted using split-half samples, followed by sensitivity analyses for key sample groupings.
Results:
Four recovery domains with 35 recovery elements emerged: abstinence in recovery, essentials of recovery, enriched recovery, and spirituality of recovery. The four-factor structure was robust regardless of length of recovery, 12-step or treatment exposure, and current substance use status. Four uncommon elements did not load on any factor but are presented to indicate the diversity of definitions.
Conclusions:
Our empirical findings offer specific items that can be used in evaluating recovery-oriented systems of care. Researchers studying recovery should include measures that extend beyond substance use and encompass elements such as those examined here—e.g., self-care, concern for others, personal growth, and developing ways of being that sustain change in substance use.
As substance use disorder services and policy increasingly embrace the broad construct of recovery as their target outcome (Clark, 2008, 2012; Office of National Drug Control Policy, 2011), details regarding the nature of recovery become essential. We present findings from the first nationwide study designed to identify specific elements of recovery obtained from a large sample representing diverse substance-related histories and recovery pathways.
The concept of recovery from substance use disorders (SUDs) is used by at least two major constituencies: the scientific community and people in recovery. Each has independently developed a set of meanings and practices related to recovery that operated in parallel until recently. The scientific community (e.g., physicians, medical societies, SUD researchers, clinical treatment organizations) has used the term to represent a medically directed course for clinical diagnosis, treatment, and rehabilitation. In contrast, the recovery community initially developed its concept of recovery from the fellowship of Alcoholics Anonymous (AA), whose basic text (the “Big Book”) describes a “program of recovery” (p. 71) that involves abstinence from alcohol and developing a new “way of living” (p. 97) in a spiritual framework outlined in the program’s 12 steps (Alcoholics Anonymous, 1939). More than half of professional treatment programs use the 12-step concept of recovery to some extent (Roman and Johnson, 2004a, 2004b).
The Affordable Care Act (Congressional Budget Office, 2010), which emphasizes the need for continuing care for chronic conditions including SUDs, coincides with two major SUD paradigmatic shifts: from a symptom/pathology focus to a wellness orientation (i.e., recovery) and from acute to chronic care models (Laudet, 2011; White, 2006). With recovery becoming the goal of services, the need to define recovery is apparent. The American Society of Addiction Medicine has defined the “state of recovery” as reaching “a state of physical and psychological health such that abstinence from dependency-producing drugs is complete and comfortable” (American Society of Addiction Medicine, 1982). A 2005 recovery definition from the Center for Substance Abuse Treatment stated: “Recovery from alcohol and drug problems is a process of change through which an individual achieves abstinence and improved health, wellness and quality of life” (Center for Substance Abuse Treatment, 2007, p. 9). Subsequently, an expert panel convened by the Betty Ford Institute issued another preliminary definition of recovery: “Recovery is a voluntarily maintained lifestyle characterized by sobriety, personal health, and citizenship” (Betty Ford Institute Consensus Panel, 2007, p. 222). Note that all of these definitions include abstinence but do not equate abstinence (or remission) with recovery. To measure recovery, the Betty Ford panel suggested using the World Health Organization Quality of Life (WHOQOL) instruments but acknowledged that no single instrument existed to adequately measure all recovery elements (Betty Ford Institute Consensus Panel, 2007).
While signaling a sea change, these definitions from the scientific community do not specify the elements of the broader construct; especially missing is the voice of experience of the individuals undergoing the process themselves. Because recovery is self-directed and self-determined (Center for Substance Abuse Treatment, 2007), key stakeholders are those experiencing it. SUD professionals can best assess substance use and remission from a dependence diagnosis; however, those in recovery can best define the specifics of recovery. This heterogeneous group includes those in recovery from different pathways—not just formal treatment—because fewer than 40% of those with SUD ever receive treatment (Compton et al., 2007; Hasin et al., 2007). The majority attain and sustain recovery without treatment via other pathways such as 12-step groups alone, non-12-step groups, medication-assisted support and other non-abstinent (“harm reduction”) approaches, cultural avenues, faith-based communities, and no formal help—for example, “natural recovery” (Sobell et al., 2000; Toneatto et al., 1999).
A definition of recovery that reflects the heterogeneity of pathways to recovery and includes a menu of elements that characterize recovery may be useful to the SUD field in at least three ways.
First, it would guide development of recovery support services (Kaplan, 2008; Laudet and Humphreys, 2013) by addressing aspects of recovery that are relevant to recovering individuals but often neglected by traditional SUD services—in part because they have heretofore not been identified empirically.
Second, it would provide a tool for internal quality monitoring and accountability to external funders and guide researchers in the selection of outcome domains when evaluating recovery-oriented systems of care. Identifying the key domains and specific elements of recovery would advance our understanding of the “way of being” in recovery, similar to how the Addiction Severity Index and the parallel Treatment Services Review provide treatment programs with tools for determining client needs and services received (Alterman and McLellan, 1993; McLellan et al., 1993, 1994, 1998). Similar instruments are ultimately needed to evaluate recovery-oriented services.
Third, a greater understanding of the positive experience of recovery may reduce the stigma currently attached to individuals working toward achieving and sustaining recovery. Recovery remains highly stigmatized (Peter D. Hart Research Associates, 2004; Pescosolido et al., 2010), but a comprehensive recovery definition will illustrate the personal and social qualities associated with recovery that can be expected, and in which one can take pride (Betty Ford Institute Consensus Panel, 2007).
Current study
The “What Is Recovery?” study was conducted to develop a detailed recovery definition that reflects the heterogeneity of individuals in recovery. We specifically sought to identify detailed elements of recovery that would be highly endorsed regardless of recovery pathway (e.g., treated vs. not treated) while also capturing unique definitional elements that may be primarily relevant to specific pathways.
Method
Respondents provided informed consent using procedures approved by the Institutional Review Board of the Public Health Institute.
Initial item development
We first developed and pre-tested an extensive pool of items reflecting how individuals from diverse pathways defined recovery. We started with the multidimensional, psychometrically strong WHO scales that capture aspects of physical, mental, and social health; independence; environment (WHOQOL Group, 1998; WHOQOL Group, 2005); and spiritual beliefs (WHOQOL-SRPB, 2002, pp. 20–23; WHOQOL SRPB Group, 2006). We reviewed papers, reports, and websites related to recovery, remission, and SUD definitions. We crafted items reflecting the suggestions of people in recovery who had reviewed the WHOQOL scales, beginning with the circle of individuals we knew who were in recovery and followed by a snowball sample of more than 30 men and women of different ethnicities, recovery durations, and pathways.
The resulting 167 items were pre-tested with a mixed-methods approach—an online survey (N = 238) and targeted qualitative telephone interviews with a subsample of the online respondents (n = 54). Survey respondents were randomly selected from alumni lists of six treatment and recovery centers (N = 72), supplemented with 166 persons recruited via ads on Craigslist. Based on answers to the items and to ensure representation of diverse recovery approaches and demographics, customized telephone interviews were conducted to explore outlier responses, problematic items, and different response options (e.g., Likert 1–7 scale vs. including a specific option to acknowledge items that did not belong in their definition but may belong in other individuals’ definitions). Items were eliminated if they were considered irrelevant to recovery (i.e., aspects of daily living or just being human), if they suggested perfection, if they were similar to more highly endorsed item(s), or if they had low endorsement (<70% said an item definitely belonged or >10% said it didn’t belong), with this exception: We retained items that were central to key subgroups (e.g., non-abstainers, those in natural recovery). This multistage analysis resulted in a reduced and refined set of 47 items on which we report here.
Recruitment
To obtain a sample that reflected the heterogeneity of recovery, we implemented a purposeful, targeted recruitment strategy designed specifically to reach individuals from the varied recovery approaches identified from the literature and our work in the field. To reach treated individuals, we partnered with treatment alumni organizations nationwide. To reach those in faith-based recovery, we recruited from faith-based organizations. To reach those using non-12-step mutual aid, we worked with four popular non-12-step organizations. To reach individuals who only use 12-step mutual aid, recruitment included distribution of flyers to Alano Clubs and at AA venues. To reach people involved in non-abstinent recovery approaches, we partnered with the National Alliance for Medication Assisted Recovery and HAMS (Harm Reduction for Alcohol) radio. To get the word out to individuals in natural recovery, we posted advertisements with links to the survey on Craigslist in 33 cities; some ads avoided the term recovery and instead solicited individuals who “used to have an alcohol or drug problem.”
We also made an explicit effort to reach African Americans and Hispanics in recovery, including through a Christian radio program in the south and Hispanic Univision in northern California. Our broad-based recruitment effort was supported by state and regional departments of behavioral health across the country, the National Council on Alcoholism and Drug Dependence, national health providers, and SUD-oriented physician organizations, publications, and advocacy groups such as Faces and Voices of Recovery. Our study website, www.WhatIsRecovery.org, lists our 58 formal study partners; we had more than 150 additional informal research partners.
Research partners helped by posting announcements about the study on their websites and by disseminating emails to their constituents voicing their support for the study. Recruitment materials encouraged passing along information about the study to others. All recruitment materials directed respondents to the study website, which included an explanation of the study and the link to the anonymous, confidential online survey.
The survey took less than 20 minutes to complete. A random sample of respondents was asked if they would fill out the survey a second time approximately 1 week later to test item reliability (for which they received a $35 Amazon gift card); those participants (n = 200) completed a second consent form explaining that contact information would be required and their surveys would no longer be anonymous.
Survey instrument
The online survey, created using SurveyGizmo (Boulder, CO), was available from July 15 to October 31, 2012, and is now posted on the Alcohol Research Group website (www.arg.org). Key measures included substance misuse history and recovery definition.
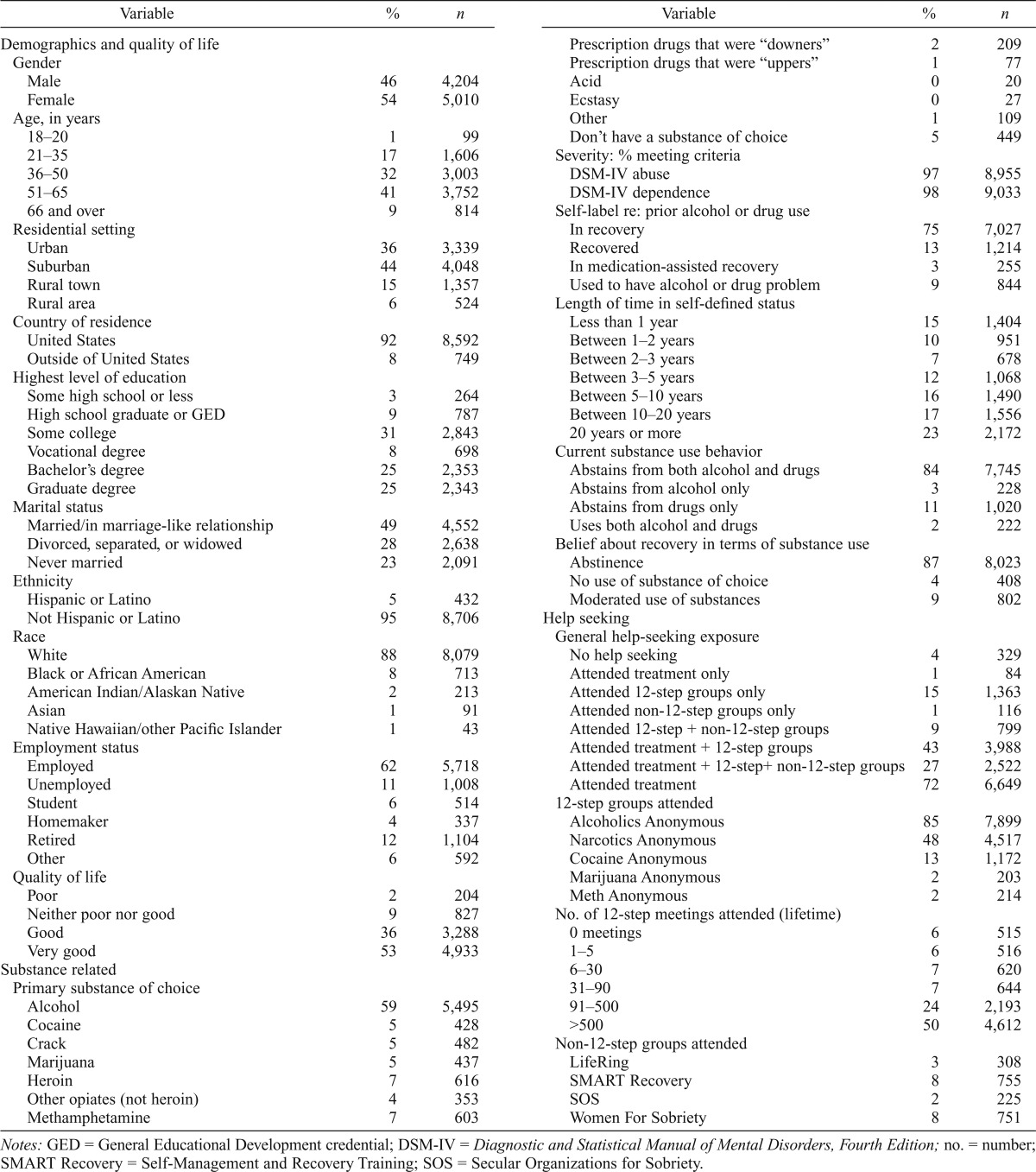
Substance misuse history (Table 1).
Table 1.
Sample characteristics and substance use history (N = 9,341)
| Variable | % | n | Variable | % | n |
| Demographics and quality of life | Prescription drugs that were “downers” | 2 | 209 | ||
| Gender | Prescription drugs that were “uppers” | 1 | 77 | ||
| Male | 46 | 4,204 | Acid | 0 | 20 |
| Female | 54 | 5,010 | Ecstasy | 0 | 27 |
| Age, in years | Other | 1 | 109 | ||
| 18-20 | 1 | 99 | Don’t have a substance of choice | 5 | 449 |
| 21-35 | 17 | 1,606 | Severity: % meeting criteria | ||
| 36-50 | 32 | 3,003 | DSM-IV abuse | 97 | 8,955 |
| 51-65 | 41 | 3,752 | DSM-IV dependence | 98 | 9,033 |
| 66 and over | 9 | 814 | Self-label re: prior alcohol or drug use | ||
| Residential setting | In recovery | 75 | 7,027 | ||
| Urban | 36 | 3,339 | Recovered | 13 | 1,214 |
| Suburban | 44 | 4,048 | In medication-assisted recovery | 3 | 255 |
| Rural town | 15 | 1,357 | Used to have alcohol or drug problem | 9 | 844 |
| Rural area | 6 | 524 | Length of time in self-defined status | ||
| Country of residence | Less than 1 year | 15 | 1,404 | ||
| United States | 92 | 8,592 | Between 1–2 years | 10 | 951 |
| Outside of United States | 8 | 749 | Between 2–3 years | 7 | 678 |
| Highest level of education | Between 3–5 years | 12 | 1,068 | ||
| Some high school or less | 3 | 264 | Between 5–10 years | 16 | 1,490 |
| High school graduate or GED | 9 | 787 | Between 10–20 years | 17 | 1,556 |
| Some college | 31 | 2,843 | 20 years or more | 23 | 2,172 |
| Vocational degree | 8 | 698 | Current substance use behavior | ||
| Bachelor’s degree | 25 | 2,353 | Abstains from both alcohol and drugs | 84 | 7,745 |
| Graduate degree | 25 | 2,343 | Abstains from alcohol only | 3 | 228 |
| Marital status | Abstains from drugs only | 11 | 1,020 | ||
| Married/in marriage-like relationship | 49 | 4,552 | Uses both alcohol and drugs | 2 | 222 |
| Divorced, separated, or widowed | 28 | 2,638 | Belief about recovery in terms of substance use | ||
| Never married | 23 | 2,091 | Abstinence | 87 | 8,023 |
| Ethnicity | No use of substance of choice | 4 | 408 | ||
| Hispanic or Latino | 5 | 432 | Moderated use of substances | 9 | 802 |
| Not Hispanic or Latino | 95 | 8,706 | Help seeking | ||
| Race | General help-seeking exposure | ||||
| White | 88 | 8,079 | No help seeking | 4 | 329 |
| Black or African American | 8 | 713 | Attended treatment only | 1 | 84 |
| American Indian/Alaskan Native | 2 | 213 | Attended 12-step groups only | 15 | 1,363 |
| Asian | 1 | 91 | Attended non- 12-step groups only | 1 | 116 |
| Native Hawaiian/other Pacific Islander | 1 | 43 | Attended 12-step + non-12-step groups | 9 | 799 |
| Employment status | Attended treatment + 12-step groups | 43 | 3,988 | ||
| Employed | 62 | 5,718 | Attended treatment + 12-step+ non-12-step groups | 27 | 2,522 |
| Unemployed | 11 | 1,008 | Attended treatment | 72 | 6,649 |
| Student | 6 | 514 | 12-step groups attended | ||
| Homemaker | 4 | 337 | Alcoholics Anonymous | 85 | 7,899 |
| Retired | 12 | 1,104 | Narcotics Anonymous | 48 | 4,517 |
| Other | 6 | 592 | Cocaine Anonymous | 13 | 1,172 |
| Quality of life | Marijuana Anonymous | 2 | 203 | ||
| Poor | 2 | 204 | Meth Anonymous | 2 | 214 |
| Neither poor nor good | 9 | 827 | No. of 12-step meetings attended (lifetime) | ||
| Good | 36 | 3,288 | 0 meetings | 6 | 515 |
| Very good | 53 | 4,933 | 1-5 | 6 | 516 |
| Substance related | 6-30 | 7 | 620 | ||
| Primary substance of choice | 31-90 | 7 | 644 | ||
| Alcohol | 59 | 5,495 | 91-500 | 24 | 2,193 |
| Cocaine | 5 | 428 | >500 | 50 | 4,612 |
| Crack | 5 | 482 | Non-12-step groups attended | ||
| Marijuana | 5 | 437 | LifeRing | 3 | 308 |
| Heroin | 7 | 616 | SMART Recovery | 8 | 755 |
| Other opiates (not heroin) | 4 | 353 | SOS | 2 | 225 |
| Methamphetamine | 7 | 603 | Women For Sobriety | 8 | 751 |
Notes: GED = General Educational Development credential; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; no. = number; SMART Recovery = Self-Management and Recovery Training; SOS = Secular Organizations for Sobriety.
Severity was determined using the Lifetime version of the Mini International Neuropsychiatric Interview (M.I.N.I.), a short structured diagnostic interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), and the International Statistical Classification of Diseases and Related Health Problems, Tenth Edition (ICD-10; World Health Organization, 1992), psychiatric disorders (Sheehan et al., 1998). Length of time in “recovery” was based on how long respondents considered themselves to be in their self-defined status (i.e., “in recovery,” “recovered,” “used to have an alcohol or drug problem but don’t anymore,” or “in medication-assisted recovery”). We computed a dichotomized measure of current substance use: abstinent from alcohol and drugs versus moderated use.
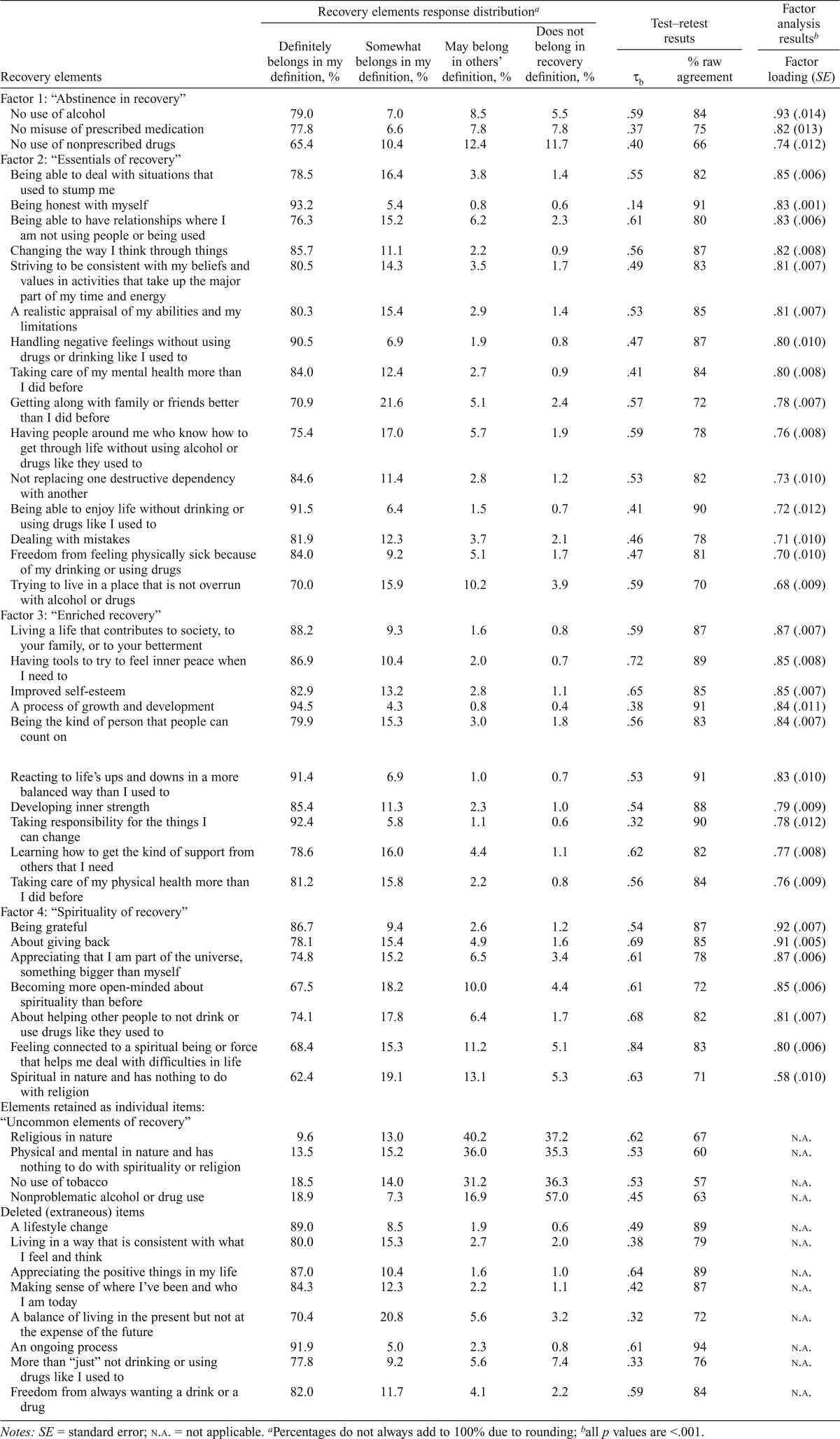
Recovery definition (Table 2).
Table 2.
Recovery definition elements: Response distribution, test–retest results, and latent factor analysis results
| Recovery elements | Recovery elements response distributiona |
Test–retest resuts |
Factor analysis resultsb |
||||
| Definitely belongs in my definition, % | Somewhat belongs in my definition, % | May belong in others’ definition, % | Does not belong in recovery definition, % | ||||
| τb | % raw agreement | Factor loading (SE) | |||||
| Factor 1: “Abstinence in recovery” | 4 | ||||||
| No use of alcohol | 79.0 | 7.0 | 8.5 | 5.5 | .59 | 84 | .93 (.014) |
| No misuse of prescribed medication | 77.8 | 6.6 | 7.8 | 7.8 | .37 | 75 | .82 (013) |
| No use of nonprescribed drugs | 65.4 | 10.4 | 12.4 | 11.7 | .40 | 66 | .74 (.012) |
| Factor 2: “Essentials of recovery” | |||||||
| Being able to deal with situations that used to stump me | 78.5 | 16.4 | 3.8 | 1.4 | .55 | 82 | .85 (.006) |
| Being honest with myself | 93.2 | 5.4 | 0.8 | 0.6 | .14 | 91 | .83 (.001) |
| Being able to have relationships where I am not using people or being used | 76.3 | 15.2 | 6.2 | 2.3 | .61 | 80 | .83 (.006) |
| Changing the way I think through things | 85.7 | 11.1 | 2.2 | 0.9 | .56 | 87 | .82 (.008) |
| Striving to be consistent with my beliefs and values in activities that take up the major part of my time and energy | 80.5 | 14.3 | 3.5 | 1.7 | .49 | 83 | .81 (.007) |
| A realistic appraisal of my abilities and my limitations | 80.3 | 15.4 | 2.9 | 1.4 | .53 | 85 | .81 (.007) |
| Handling negative feelings without using drugs or drinking like I used to | 90.5 | 6.9 | 1.9 | 0.8 | .47 | 87 | .80 (.010) |
| Taking care of my mental health more than I did before | 84.0 | 12.4 | 2.7 | 0.9 | .41 | 84 | .80 (.008) |
| Getting along with family or friends better than I did before | 70.9 | 21.6 | 5.1 | 2.4 | .57 | 72 | .78 (.007) |
| Having people around me who know how to get through life without using alcohol or drugs like they used to | 75.4 | 17.0 | 5.7 | 1.9 | .59 | 78 | .76 (.008) |
| Not replacing one destructive dependency with another | 84.6 | 11.4 | 2.8 | 1.2 | .53 | 82 | .73 (.010) |
| Being able to enjoy life without drinking or using drugs like I used to | 91.5 | 6.4 | 1.5 | 0.7 | .41 | 90 | .72 (.012) |
| Dealing with mistakes | 81.9 | 12.3 | 3.7 | 2.1 | .46 | 78 | .71 (.010) |
| Freedom from feeling physically sick because of my drinking or using drugs | 84.0 | 9.2 | 5.1 | 1.7 | .47 | 81 | .70 (.010) |
| Trying to live in a place that is not overrun with alcohol or drugs | 70.0 | 15.9 | 10.2 | 3.9 | .59 | 70 | .68 (.009) |
| Factor 3: “Enriched recovery” | |||||||
| Living a life that contributes to society, to your family, or to your betterment | 88.2 | 9.3 | 1.6 | 0.8 | .59 | 87 | .87 (.007) |
| Having tools to try to feel inner peace when I need to | 86.9 | 10.4 | 2.0 | 0.7 | .72 | 89 | .85 (.008) |
| Improved self-esteem | 82.9 | 13.2 | 2.8 | 1.1 | .65 | 85 | .85 (.007) |
| A process of growth and development | 94.5 | 4.3 | 0.8 | 0.4 | .38 | 91 | .84 (.011) |
| Being the kind of person that people can count on | 79.9 | 15.3 | 3.0 | 1.8 | .56 | 83 | .84 (.007) |
| Reacting to life’s ups and downs in a more balanced way than I used to | 91.4 | 6.9 | 1.0 | 0.7 | .53 | 91 | .83 (.010) |
| Developing inner strength | 85.4 | 11.3 | 2.3 | 1.0 | .54 | 88 | .79 (.009) |
| Taking responsibility for the things I can change | 92.4 | 5.8 | 1.1 | 0.6 | .32 | 90 | .78 (.012) |
| Learning how to get the kind of support from others that I need | 78.6 | 16.0 | 4.4 | 1.1 | .62 | 82 | .77 (.008) |
| Taking care of my physical health more than I did before | 81.2 | 15.8 | 2.2 | 0.8 | .56 | 84 | .76 (.009) |
| Factor 4: “Spirituality of recovery” | |||||||
| Being grateful | 86.7 | 9.4 | 2.6 | 1.2 | .54 | 87 | .92 (.007) |
| About giving back | 78.1 | 15.4 | 4.9 | 1.6 | .69 | 85 | .91 (.005) |
| Appreciating that I am part of the universe, something bigger than myself | 74.8 | 15.2 | 6.5 | 3.4 | .61 | 78 | .87 (.006) |
| Becoming more open-minded about spirituality than before | 67.5 | 18.2 | 10.0 | 4.4 | .61 | 72 | .85 (.006) |
| About helping other people to not drink or use drugs like they used to | 74.1 | 17.8 | 6.4 | 1.7 | .68 | 82 | .81 (.007) |
| Feeling connected to a spiritual being or force that helps me deal with difficulties in life | 68.4 | 15.3 | 11.2 | 5.1 | .84 | 83 | .80 (.006) |
| Spiritual in nature and has nothing to do with religion | 62.4 | 19.1 | 13.1 | 5.3 | .63 | 71 | .58 (.010) |
| Elements retained as individual items: “Uncommon elements of recovery” | |||||||
| Religious in nature | 9.6 | 13.0 | 40.2 | 37.2 | .62 | 67 | n.a. |
| Physical and mental in nature and has nothing to do with spirituality or religion | 13.5 | 15.2 | 36.0 | 35.3 | .53 | 60 | n.a. |
| No use of tobacco | 18.5 | 14.0 | 31.2 | 36.3 | .53 | 57 | n.a. |
| Nonproblematic alcohol or drug use | 18.9 | 7.3 | 16.9 | 57.0 | .45 | 63 | n.a. |
| Deleted (extraneous) items | |||||||
| A lifestyle change | 89.0 | 8.5 | 1.9 | 0.6 | .49 | 89 | n.a. |
| Living in a way that is consistent with what | 80.0 | 15.3 | 2.7 | 2.0 | .38 | 79 | n.a. |
| I feel and think | |||||||
| Appreciating the positive things in my life | 87.0 | 10.4 | 1.6 | 1.0 | .64 | 89 | n.a. |
| Making sense of where I’ve been and who | 84.3 | 12.3 | 2.2 | 1.1 | .42 | 87 | n.a. |
| I am today | |||||||
| A balance of living in the present but not at the expense of the future | 70.4 | 20.8 | 5.6 | 3.2 | .32 | 72 | n.a. |
| An ongoing process | 91.9 | 5.0 | 2.3 | 0.8 | .61 | 94 | n.a. |
| More than “just” not drinking or using drugs like I used to | 77.8 | 9.2 | 5.6 | 7.4 | .33 | 76 | n.a. |
| Freedom from always wanting a drink or a drug | 82.0 | 11.7 | 4.1 | 2.2 | .59 | 84 | n.a. |
Notes: SE = standard error; n.a. = not applicable.
Percentages do not always add to 100% due to rounding;
allp values are <.001.
Four response categories were available to indicate endorsement of the 47 recovery items: (a) “definitely belongs in your definition of recovery,” (b) “somewhat belongs in your definition of recovery,” (c) “does not belong in your definition of recovery, but may belong in other people’s definition of recovery,” and (d) “does not really belong in a definition of recovery.”
Analysis
Our ultimate goal was to conduct item response analysis to further reduce the item pool, uncover conceptual item groupings through factor analysis, and identify groups of individuals who defined recovery in similar ways. We hypothesized that a heterogeneous sample might endorse a core set of items but vary in other key elements such as whether recovery requires total abstinence and issues around spirituality. We conducted extensive bivariate (chi-square) analyses of items by sample groupings (e.g., demographics, substance use history, help seeking) to inform item-reduction efforts while ensuring that omission of certain items would not diminish generalizability to a diverse population.
Kendall’s Tau-b (τb) (Kruskal, 1958) was used to assess test–retest reliability of the recovery items. We also calculated raw agreement based on the sum of matched pairs across the diagonal for each item.
Exploratory factor analysis (EFA) was used to examine the underlying dimensionality of the full set of 47 items using Mplus Version 7.1 (Muthén and Muthén, 2013). Factor extraction was carried out on a split-half sample using a robust weighted least squares estimator (WLSMV) with a diagonal weight matrix (Muthén, 1984; Muthén et al., 1997) and GEOMIN oblique rotation to extract factors (Browne, 2001; Yates, 1987). Before subsequent confirmatory factor analysis (CFA) models were conducted, resulting models were compared on model fit statistics, patterns of EFA factor loadings, and correlations between items that informed a priori our decisions about the CFA to be estimated.
A four-factor CFA model of 35 retained items with factor variances fixed at 1 was then estimated with the second split-half sample. The specific model estimated was a normal ogive model (Muthén and Asparouhov, 2002) with GEOMIN oblique rotation method. Goodness of fit considerations included the Tucker–Lewis Index (TLI) and the root mean square error of approximation (RMSEA).
The EFA and CFA described above were repeated with the full sample and with key grouping variables. Factor structures were compared to those from the first split-half sample, and model fit was assessed and factor loadings compared to those from the second split-half sample.
Next, factor scores were estimated using our CFA model. To enable comparisons with future studies, we also created raw factor scores by summing items within each factor using original item categories (defined as 0, 1, 2, 3; where 0 = does not belong, 1 = may belong, 2 = somewhat belongs, 3 = definitely belongs). Analysis of variance models were estimated using factor scores generated from Mplus to statistically compare factor scores for six key subgroups, with the average raw factor scores estimates reported for interpretative purposes. Last, we analyzed subgroup differences on four items that did not load on any factor, using chi-square statistics.
Results
Description of sample
The four largest-yielding sources for hearing about the study produced more than half of the entire sample (not shown): family and friends (15%), recovery organizations (13%), Craigslist (12%), and treatment and alumni groups (12%). Respondents also heard about the study through social media (7%), non-12-step self-help groups (7%), 12-step groups (5%), advertisements (4%), and conferences and Alano Clubs (about 1% each). Almost one quarter selected “other” (24%).
Because of our multifaceted recruitment approach, it was impossible to estimate a denominator to use in calculating a study response rate. Demographic comparisons of our “What Is Recovery?” sample to national samples of individuals in recovery—that is, the National Alcohol Survey (Alcohol Research Group, 1964–2005) and the Office of Alcoholism and Substance Abuse Services survey (New York State Office of Alcoholism and Substance Abuse Services, 2012)—showed no major differences across samples. Importantly, the demographic breakdown of our sample was almost exactly the same as that of the “Life in Recovery” sample (Laudet, 2013; Laudet et al., 2014), the only other published online survey of individuals in recovery. As a final check for consistency with other recovery samples, we compared those within our sample who had received treatment with other large, nationally representative treatment samples, that is, the Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity; Project MATCH Research Group, 1997) and COMBINE (Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence; Anton et al., 2006) studies; no major differences were found. Taken together, these comparisons (Subbaraman et al., in press) suggest that our sample is similar to other samples of individuals in recovery.
Slightly more respondents were female (Table 1). More than three fourths of the sample was older than age 35, half had a bachelor’s degree or greater, and 11% were unemployed. The majority was non-Hispanic and White. Only 2% reported a poor quality of life.
The primary problem substance was alcohol in more than half of the sample. Only 2% did not meet DSM-IV criteria for alcohol or drug dependence. Three quarters of the respondents self-labeled as “in recovery,” and the majority had been in their self-defined status for more than 5 years. Most were currently abstaining from both alcohol and drugs, and endorsed that recovery is abstinence.
Only 4% were in natural recovery (no history of treatment or self-help group use, shown in Table 1 as “no help seeking”). High proportions had been in treatment and to AA, about half had been to Narcotics Anonymous, and 18% had been to at least one of the non-12-step support groups included on the survey (aggregate not shown; Table 1 shows rates of exposure for each group). Twelve-step exposure and treatment overlapped considerably. Twelve-step meeting attendance was quite high, with half reporting more than 500 meetings in their lifetime.
Recovery item response distribution
The distribution of respondent answers across the four response categories is shown in Table 2. Items are organized by the four conceptual groupings that emerged from the factor analysis (labeled abstinence in recovery, essentials of recovery, enriched recovery, and spirituality of recovery); a fifth grouping of uncommon elements that did not load on any factor; and deleted, extraneous items (see Latent factor analysis, below). Overall, there was fairly strong endorsement (i.e., “definitely belongs”) for the elements (items) in the four factors, and low endorsement (i.e., low proportions of “definitely belongs” and high proportions choosing “does not belong”) for those in the uncommon recovery elements. We speak here of “tolerance” for recovery elements when relatively high proportions choose “does not belong in your definition of recovery but may belong in other people’s definition of recovery.” We see high tolerance for the uncommon elements (range: 17%–40%) and considerable tolerance (i.e., by more than 10% of the sample) for five other elements (three of which are in the spirituality factor). The tolerance exhibited for the uncommon elements supports the decision to retain these items as representative of equally valid but not widely held recovery elements.
Based on patterns emerging from cross-tabulation of recovery items by different re-categorizations of sample groupings, the six key grouping variables that most clearly represented heterogeneous recovery definitions were based on (a) recovery duration (1 year or less; 2–5 years; more than 5 years), (b) current substance use status (abstinent vs. moderated use); (c) substance of choice (alcohol; drugs; none); (d) 12-step meeting exposure (0–90 meetings vs. >90 meetings); (e) treated vs. untreated; and (f) being in natural recovery (vs. not).
Test–retest results (Table 2)
Analysis of the 200 test–retest surveys found good-to-very-good agreement (τb’s of 0.6 or greater) for 13 items and fair agreement (τb’s between 0.4 and 0.5) for 26 items. Tau-b is very sensitive to items with extremely skewed distributions (e.g., small cell sizes; see being honest with myself in factor 2, and a process of growth and development and taking responsibility in factor 3). In the presence of such skewed distributions, “raw agreement” (sum of the diagonals) is an especially relevant measure of item stability: raw agreement was 70% or greater for 42 items, and the overall proportion who endorsed an item at both administrations is 95% (not shown).
Latent factor analysis (Table 2)
Based on the EFA with the first split-half of the full sample using the 47 recovery elements, eight redundant, nondiscriminatory items that were conceptually similar (and demonstrated similar patterns of support with other items) were deleted as were four other items that did not load on any factor. A four-factor model, explaining 66% of the total variance, was chosen for conducting CFA with 35 items on the second split-half of the full sample. Good model fit was found (RMSEA = .058 and TLI = .982).
Both the EFA and CFA replicated with the full sample as well as with the grouping variables for which there were sufficient samples (we were unable to run the EFA and CFA for the natural recovery group, n = 329). Factor loadings for the full sample are shown in Table 2.
As introduced above, the four factors are “abstinence in recovery” (3 items), “essentials of recovery” (15 items), “enriched recovery” (10 items), and “spirituality of recovery” (7 items). Factor loadings range from .585 (last item in factor 4) to .928 (first item in factor 1). Only two items have loadings lower than .7 (last items in factors 2 and 4). Correlations between factors (not shown) were low between the abstinence factor and the other factors (less than .31) and were high for the others (r = .90 between essentials and enriched factors; and between the spirituality factor and, respectively, the essentials and enriched factors, r = .83 and r = .76).
All three elements in factor 1, “abstinence in recovery,” refer specifically to substance use: no use of alcohol, no misuse of prescribed medications, and no use of nonprescribed drugs. Recall that support is modest for the latter element (i.e., nearly a quarter of the sample does not view abstinence from non-prescribed drugs as belonging in their own recovery definition).
Factor 2 is labeled the “essentials of recovery,” as the component elements appear to capture basic ways of being that may be necessary to sustain substantial changes in substance use: being able to deal with challenging situations, relationships, negative feelings, family/friends, and mistakes; mental changes in terms of honesty, ways of thinking, realistic appraisal of self, and enjoying life; behavioral changes like consistency, caring for mental health, not replacing one destructive dependency with another one, and having supportive social networks and living conditions; and physical changes from no longer feeling sick because of overuse of substances. Very few said that these elements do not belong in any recovery definition.
In the third factor, “enriched recovery,” the elements are subtly different from those in factor 2, but the factor loadings clearly indicate a distinct conceptual grouping. They pertain to looking outward (living a life that contributes, being someone people can count on, reacting in a balanced way, taking responsibility), turning inward (having tools for inner peace, better self-esteem, inner strength), and taking care of one’s self (getting support from others and caring for physical health). Of note, the two health elements pertaining respectively to taking care of physical and mental health loaded more strongly on different factors, with mental health placed within the “essential recovery” factor.
Factor 4, the “spirituality of recovery,” is not limited to concepts obviously spiritual in nature but also encompasses such notions as gratitude, giving back, and helping others. Other elements of the spirituality factor, such as feeling connected to a spiritual being or force, are more explicitly spiritual. The last item, recovery is spiritual in nature and has nothing to do with religion, is an explicit distancing from religion while an acknowledgment of the spiritual nature of recovery. As noted above, elements with the word spiritual were rejected by 4%–5% of the sample; at the same time, 10%–13% of the sample said those elements may belong in others’ definitions, again signaling high awareness that these concepts are important to many people in recovery regardless of one’s own views.
Differences in factor scores based on key grouping variables
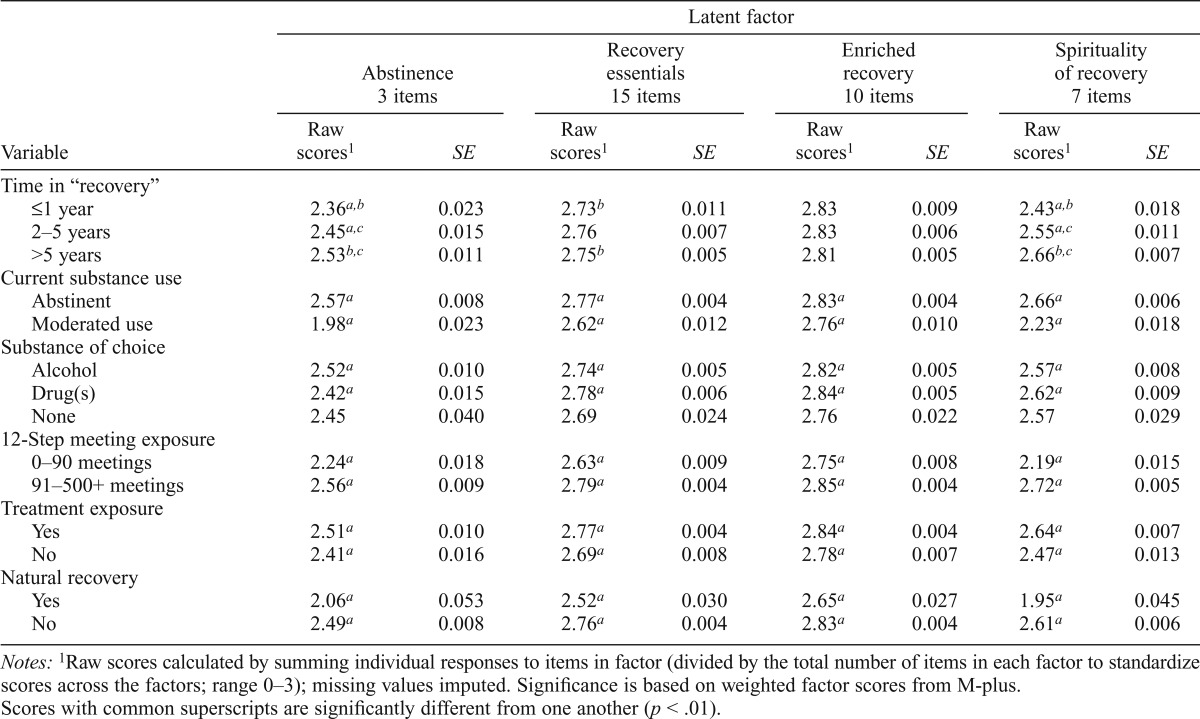
To gauge differences in participants’ overall recovery definitions, we compared factor scores based on recovery duration, substance use status (abstaining or not), primary substance, amount of 12-step meeting exposure, exposure to treatment, and being in natural recovery. For interpretability across studies, mean raw scores are shown (Table 3); comparisons between the CFA factor scores and the raw scores yielded highly significant correlations that ranged from .890 to .944 (not shown).
Table 3.
Total factor scores based on time in recovery, current substance use, substance of choice, 12-step meeting exposure, and treatment seeking: raw scores and standard errors (SE)
| Variable | Latent factor |
|||||||
| Abstinence 3 items |
Recovery essentials 15 items |
Enriched recovery 10 items |
Spirituality of recovery 7 items |
|||||
| Raw scores1 | SE | Raw scores1 | SE | Raw scores1 | SE | Raw scores1 | SE | |
| Time in “recovery” | ||||||||
| ≤1 year | 2.36a,b | 0.023 | 2.73b | 0.011 | 2.83 | 0.009 | 2.43a,b | 0.018 |
| 2–5 years | 2.45a,c | 0.015 | 2.76 | 0.007 | 2.83 | 0.006 | 2.55a,c | 0.011 |
| >5 years | 2.53b,c | 0.011 | 2.66 | 0.005 | 2.81 | 0.005 | 2.66b,c | 0.007 |
| Current substance use | ||||||||
| Abstinent | 2.57a | 0.008 | 2.77a | 0.004 | 2.83a | 0.004 | 2.66a | 0.006 |
| Moderated use | 1.98a | 0.023 | 2.62a | 0.012 | 2.76a | 0.010 | 2.23a | 0.018 |
| Substance of choice | ||||||||
| Alcohol | 2.52a | 0.010 | 2.74a | 0.005 | 2.82a | 0.005 | 2.57a | 0.008 |
| Drug(s) | 2.42a | 0.015 | 2.78a | 0.006 | 2.84a | 0.005 | 2.62a | 0.009 |
| None | 2.45 | 0.040 | 2.69 | 0.024 | 2.76 | 0.022 | 2.57 | 0.029 |
| 12-Step meeting exposure | ||||||||
| 0–90 meetings | 2.24a | 0.018 | 2.63a | 0.009 | 2.75a | 0.008 | 2.19a | 0.015 |
| 91–500+meetings | 2.56a | 0.009 | 2.79a | 0.004 | 2.85a | 0.004 | 2.72a | 0.005 |
| Treatment exposure | ||||||||
| Yes | 2.51a | 0.010 | 2.77a | 0.004 | 2.84a | 0.004 | 2.64a | 0.007 |
| No | 2.41a | 0.016 | 2.69a | 0.008 | 2.78a | 0.007 | 2.47a | 0.013 |
| Natural recovery | ||||||||
| Yes | 2.06a | 0.053 | 2.52a | 0.030 | 2.65a | 0.027 | 1.95a | 0.045 |
| No | 2.49a | 0.008 | 2.76a | 0.004 | 2.83a | 0.004 | 2.61a | 0.006 |
Notes: 1Raw scores calculated by summing individual responses to items in factor (divided by the total number of items in each factor to standardize scores across the factors; range 0–3); missing values imputed. Significance is based on weighted factor scores from M-plus. Scores with common superscripts are significantly different from one another (p < .01).
Significant differences (p < .001) in factor scores were found for all factors for the six respondent groupings, with the exception of recovery duration for the enriched recovery factor. For example, for the abstinence and the spirituality of recovery factors, those with more than 5 years in recovery had significantly higher scores than those with 2–5 years and with 1 year or less, and those with 2–5 years had higher scores than those with 1 year or less. Note that differences emerged as statistically significant but were of modest magnitude.
Scores were significantly higher for the abstainers than the moderated users for all four factors, with the magnitude of differences slightly larger than was found for time in recovery. Although modest in magnitude, significantly higher factor scores were also seen for respondents who had attended more than 90 12-step meetings, and among treated individuals. Conversely, all factor scores were significantly lower for those in natural recovery, who also had the lowest factor score of any group for the spirituality factor. Results were mixed when considering substance of choice: Among the alcohol group, the scores were significantly higher on the abstinence factor but were lower on the other three factors.
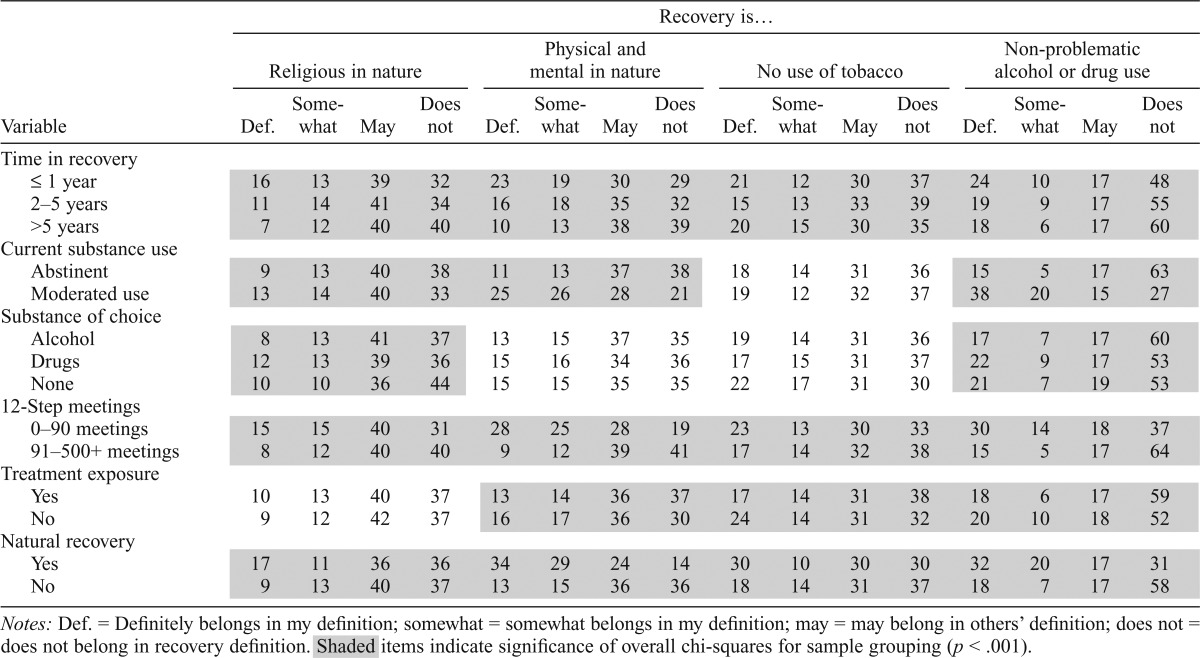
Differences in responses to unusual definitions of recovery (Table 4)
Table 4.
Unusual elements of recovery: response distribution by time in recovery, current substance use status, substance of choice, and 12-step meeting exposure
| Variable | Recovery is… |
|||||||||||||||
| Religious in nature |
Physical and mental in nature |
No use of tobacco |
Non-problematic alcohol or drug use |
|||||||||||||
| Def. | Somewhat | May | Does not | Def. | Somewhat | May | Does not | Def. | Somewhat | May | Does not | Def. | Somewhat | May | Does not | |
| Time in recovery | ||||||||||||||||
| < 1 year | 16 | 13 | 39 | 32 | 23 | 19 | 30 | 29 | 21 | 12 | 30 | 37 | 24 | 10 | 17 | 48 |
| 2–5 years | 11 | 14 | 41 | 34 | 16 | 18 | 35 | 32 | 15 | 13 | 33 | 39 | 19 | 9 | 17 | 55 |
| >5 years | 7 | 12 | 40 | 40 | 10 | 13 | 38 | 39 | 20 | 15 | 30 | 35 | 18 | 6 | 17 | 60 |
| Current substance use | ||||||||||||||||
| Abstinent | 9 | 13 | 40 | 38 | 11 | 13 | 37 | 38 | 18 | 14 | 31 | 36 | 15 | 5 | 17 | 63 |
| Moderated use | 13 | 14 | 40 | 33 | 25 | 26 | 28 | 21 | 19 | 12 | 32 | 37 | 38 | 20 | 15 | 27 |
| Substance of choice | ||||||||||||||||
| Alcohol | 8 | 13 | 41 | 37 | 13 | 15 | 37 | 35 | 19 | 14 | 31 | 36 | 17 | 7 | 17 | 60 |
| Drugs | 12 | 13 | 39 | 36 | 15 | 16 | 34 | 36 | 17 | 15 | 31 | 37 | 22 | 9 | 17 | 53 |
| None | 10 | 10 | 36 | 44 | 15 | 15 | 35 | 35 | 22 | 17 | 31 | 30 | 21 | 7 | 19 | 53 |
| 12-Step meetings | ||||||||||||||||
| 0-90 meetings | 15 | 15 | 40 | 31 | 28 | 25 | 28 | 19 | 33 | 13 | 30 | 33 | 30 | 14 | 18 | 37 |
| 91-500+meetings | 8 | 12 | 40 | 40 | 9 | 12 | 39 | 41 | 17 | 14 | 32 | 38 | 15 | 5 | 17 | 64 |
| Treatment exposure | ||||||||||||||||
| Yes | 10 | 13 | 40 | 37 | 13 | 14 | 36 | 37 | 17 | 14 | 31 | 38 | 18 | 6 | 17 | 59 |
| No | 9 | 12 | 42 | 37 | 16 | 17 | 36 | 30 | 24 | 14 | 31 | 32 | 20 | 10 | 18 | 52 |
| Natural recovery | ||||||||||||||||
| Yes | 17 | 11 | 36 | 36 | 34 | 29 | 24 | 14 | 30 | 10 | 30 | 30 | 32 | 20 | 17 | 31 |
| No | 9 | 13 | 40 | 37 | 13 | 15 | 36 | 36 | 18 | 14 | 31 | 37 | 18 | 7 | 17 | 58 |
Notes: Def. = Definitely belongs in my definition; somewhat = somewhat belongs in my definition; may = may belong in others’ definition; does not = does not belong in recovery definition. Shaded items indicate significance of overall chi-squares for sample grouping (p < .001).
Next, we consider differences in support for the four unusual recovery element items, which did not load on any factors but are retained to represent the breadth of recovery elements represented by diverse approaches to recovery. Significant differences were found for most elements for all groupings of respondents. The items recovery is religious in nature and recovery is physical and mental in nature and has nothing to do with spirituality or religion were mainly supported by those with less time in recovery, those who were not abstaining, those with 0–90 12-step meetings, and those in natural recovery.
The view that recovery is no use of tobacco was endorsed by 35% of those with more than 5 years in recovery, for whom a similar proportion said it “does not belong in any definition of recovery.” Thirty-one percent of those with more than 90 meetings support this element, compared to 36% of those with fewer meetings. Thus, support for its inclusion in a recovery definition does not appear to hinge on having a longer length of recovery or on having attended more 12-step meetings; rather, the opposite appears to be the case. The highest support for its inclusion is among those who had not been to treatment and those in natural recovery.
Last, the fourth recovery element emerging as uncommon is that recovery is nonproblematic alcohol or drug use. The majority of those who were not abstaining and those who are in natural recovery support this in their definition of recovery.
Discussion
This is the first extensive effort to empirically explore the domains of recovery and to identify the specific elements that comprise these domains. Test–retest results were concordant, implying stability for these elements. The sensitivity analyses based on our key grouping variables highlight one advantage of our large study and diversity of recruitment sources: the four-factor structure for the 35 recovery elements is robust regardless of length in recovery, 12-step or treatment exposure, and current substance use status. Although not based on a probability sample, our study provides a starting point for understanding recovery through the voices of those who experienced it themselves, through diverse pathways.
Overall, the six elements endorsed most (>90%) as definitely belonging in their definition included three elements of “essential recovery” (being honest with myself, handling negative feelings without using drugs or alcohol, being able to enjoy life without drinking or using drugs like I used to) and three elements of “enriched recovery” (a process of growth and development, reacting to life’s ups and downs in a more balanced way than I used to, taking responsibility for the things I can change). Although factor scores for these domains were significantly higher among individuals with greater levels of 12-step exposure, the magnitude of differences is small, suggesting that the elements in those factors—many of which indeed reflect 12-step principles—appear to be somewhat universal among survey participants. This conclusion is consistent with findings from a qualitative study conducted among a smaller sample of formerly drug-dependent individuals in abstinent recovery, where one in five respondents spontaneously described recovery as “working on yourself/self-improvement” and almost all (97%) agreed that “recovery is a continuous process that never ends” (Laudet, 2007).
In contrast, the recovery element endorsed by the fewest respondents as definitely belonging in their definition was in the spirituality factor—recovery is spiritual in nature and has nothing to do with religion (63%). Other elements containing the notion of spirituality consistently had low endorsement and a relatively high proportion of “may belong in others’ definition” ratings (around 10%). Of note, two elements in this factor centered on helping behaviors (recovery is about giving back, recovery is about helping other people to not drink or use drugs like they used to), which were endorsed by more than 90% of the sample. This bolsters evidence that helping behaviors indeed are an expression of spirituality in the recovery context (Zemore and Kaskutas, 2004).
Limitations
The study was conducted exclusively online, with data collection limited to 3.5 months in mid-2012. Racial minorities and individuals with lower education are underrepresented in our sample. Although the Internet use gap between Whites and non-Whites is rapidly closing, and 78% of U.S. adults were using the Internet in 2011, educational attainment continues to be strongly correlated with Internet adoption (Zickuhr and Smith, 2012). We cannot determine from the existing data whether an individual obtained his or her higher education after entering recovery and will incorporate that question in future recovery studies. We conducted post hoc analyses to determine whether the recovery elements might apply only to well-educated, racial/ethnic majority populations in recovery; they do not. Minorities and those without a college degree scored slightly lower on the abstinence factor but slightly higher on the other three factors.
We have no definitive way to assess our sample’s generalizability with regard to the (as yet unknown) “universe” of individuals in recovery, although our comparisons to other samples of individuals in recovery showed that treatment samples appear to include fewer females and older individuals, and Internet samples reach fewer Hispanics and individuals with lower education levels. Importantly, our sample demographics are almost identical to Faces and Voices of Recovery’s “Life in Recovery survey,” also conducted exclusively online the same year as our study (Laudet, 2013). Furthermore, the demographic profile of treated individuals in our sample is similar to the profiles of other large, national treatment samples (Subbaraman et al., in press).
However, our sample has a low proportion (4%) of those in natural recovery, despite extensive Craigslist recruitment that purposefully avoided the word “recovery.” Given these challenges, we plan to use the next National Alcohol Survey to reach a representative, racially and educationally diverse sample of persons in recovery.
Implications
These findings highlight specific areas that chronic care models such as recovery-oriented systems of care could address to promote recovery and that researchers studying recovery should consider—e.g., self-care, concern for others, personal growth, and developing ways of being that sustain changes in substance use. For example, providers might add or suggest sober fun activities and opportunities for volunteering and emphasize contributing to society.
Footnotes
This study was supported by National Institute on Alcohol Abuse and Alcoholism Grant AA017954-01A1.
References
- Alcohol Research Group. National Alcohol Survey (NAS1–NAS11) Berkeley, CA: Alcohol Research Group, Public Health Institute; 1964–2005. [Google Scholar]
- Anonymous Alcoholics. Alcoholics Anonymous: The story of how many thousands of men and women have recovered. New York, NY: Works Publishing; 1939. [Google Scholar]
- Alterman AI, McLellan AT. Inpatient and day hospital treatment services for cocaine and alcohol dependence. Journal of Substance Abuse Treatment. 1993;10:269–275. doi: 10.1016/0740-5472(93)90074-c. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Society of Addiction Medicine. Public Policy Statement on the State of Recovery. 1982. Archived by WebCite at http://www.webcitation.org/6IKsAZDzs. [Google Scholar]
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Williams LD, the COMBINE Study Research Group Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE study: A randomized controlled trial. Journal of the American Medical Association. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. Journal of Substance Abuse Treatment. 2007;33:221–228. doi: 10.1016/j.jsat.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Browne MW. An overview of analytic rotation in exploratory factor analysis. Multivariate Behavioral Research. 2001;36:111–150. [Google Scholar]
- Center for Substance Abuse Treatment. National Summit on Recovery: Conference Report. 2007. DHHS Publication No. (SMA) 07-4276. Rock-ville, MD: Substance Abuse and Mental Health Services Administration. Archived by WebCite at http://www.webcitation.org/6IML7OyMP. [Google Scholar]
- Clark HW. Recovery-oriented systems of care: SAMHSA/CSAT’s public health approach to substance use problems and disorders Aligning Concepts, Practice, and Contexts to Promote Long Term Recovery: An action plan. Philadelphia, PA: Substance Abuse Mental Health Services Administration, Center for Substance Abuse Treatment; 2008. [Google Scholar]
- Clark HW. A model for recovery-oriented systems of care from a national perspective. Las Vegas, NV: Presented at the 13th annual NCRG Conference on Gambling and Addiction; 2012, September. [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. Selected CBO Publications Related to Health Care Legislation, 2009–2010. 2010. Archived by WebCite at http://www.webcitation.org/6Npes0ITg. [Google Scholar]
- Peter D, Hart Research Associates . Faces and Voices of Recovery Public Survey. 2004. Washington, D.C: Peter D. Hart Research Associates. Retrieved from: http://ww.facesandvoicesofrecovery.org/resources/hart_survey.php. [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Kaplan L. The role of recovery support services in recovery-oriented systems of care (DHHS Publication No. (SMA) 08–4315) 2008. Rockville, MD: Center for Substance Abuse Services, Substance Abuse and Mental Health Services Administration. Archived by WebCite at http://www.webcitation.org/6Npj7lnTg] [Google Scholar]
- Kruskal WH. Ordinal measures of association. Journal of the American Statistical Association. 1958;53:814–861. [Google Scholar]
- Laudet A. Life in Recovery Survey. 2013. Washington, DC: Faces and Voices of Recovery. Archived by WebCite at http://www.webcitation.org/6Hy1e1JAO. [Google Scholar]
- Laudet A, Timko C, Hill T. Comparing life experiences in active addiction and recovery between veterans and non-veterans: A national study. Journal of Addictive Diseases. 2014;33:148–162. doi: 10.1080/10550887.2014.909702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB. What does recovery mean to you? Lessons from the recovery experience for research and practice. Journal of Substance Abuse Treatment. 2007;33:243–256. doi: 10.1016/j.jsat.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB. The case for considering quality of life in addiction research and clinical practice. Addiction Science and Clinical Practice. 2011;6:44–55. [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Humphreys K. Promoting recovery in an evolving policy context: What do we know and what do we need to know about recovery support services? Journal of Substance Abuse Treatment. 2013;45:126–133. doi: 10.1016/j.jsat.2013.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Metzger DS, Grissom GR, Woody GE, Luborsky L, O’Brien CP. Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: Role of treatment services. Journal of Consulting and Clinical Psychology. 1994;62:1141–1158. doi: 10.1037//0022-006x.62.6.1141. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Grissom GR, Brill P, Durell J, Metzger DS, O’Brien CP. Private substance abuse treatments: Are some programs more effective than others? Journal of Substance Abuse Treatment. 1993;10:243–254. doi: 10.1016/0740-5472(93)90071-9. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Hagan TA, Levine M, Gould F, Meyers K, Ben-civengo M, Durell J. Supplemental social services improve outcomes in public addiction treatment. Addiction. 1998;93:1489–1499. doi: 10.1046/j.1360-0443.1998.931014895.x. [DOI] [PubMed] [Google Scholar]
- Muthén B. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika. 1984;49:115–132. [Google Scholar]
- Muthén B, Asparouhov T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. 2002. Archived by WebCite at http://www.webcitation.org/65wvNEgl6. [Google Scholar]
- Muthén BO, du Toit SHC, Spisic D. Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes. 1997. Los Angeles, CA: University of California. Retrieved from http://pages.gseis.ucla.edu/faculty/muthen/articles/Article_075.pdf. [Google Scholar]
- Muthén LK, Muthén BO. Mplus version 7.1. Los Angeles, CA: Authors; 2013. [Google Scholar]
- New York State Office of Alcoholism and Substance Abuse Services. Survey: Ten percent of American adults report being in recovery from substance abuse or addiction. 2012, March 6. Archived by WebCite at http://www.webcitation.org/6FwzbsS1A. [Google Scholar]
- Office of National Drug Control Policy. National Drug Control Strategy. 2011. Washington, DC: Author. Archived by WebCite at http://www.webcitation.org/6OXocZGQn. [Google Scholar]
- Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry. 2010;167:1321–1330. doi: 10.1176/appi.ajp.2010.09121743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Roman PM, Johnson JA. National Treatment Center Study Summary Report: Private treatment centers. 2004a. Athens, GA: Institute for Behavioral Research, University of Georgia. Archived by WebCite at http://www.webcitation.org/6NqwxWdUx. [Google Scholar]
- Roman PM, Johnson JA. National Treatment Center Study Summary Report: Public treatment centers. 2004b. Athens, GA: Institute for Behavioral Research, University of Georgia. Archived by WebCite at http://www.webcitation.org/6E4OnSSJJ. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuro-psychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, Supplement. 1998;20:22–33. quiz 34–57. [PubMed] [Google Scholar]
- Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: Methodological review of the research with suggestions for future directions. Addiction. 2000;95:749–764. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- Subbaraman MS, Laudet AB, Ritter LA, Stunz A, Kaskutas LA. Multi-source recruitment strategies for advancing addiction recovery research beyond treated samples. Journal of Community Psychology. in press doi: 10.1002/jcop.21702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toneatto T, Sobell LC, Sobell MB, Rubel E. Natural recovery from cocaine dependence. Psychology of Addictive Behaviors. 1999;13:259–268. [Google Scholar]
- White WL. Recovery: The next frontier. In: White WL, Kurtz E, Sanders M, editors. Recovery management. Chicago, IL: Great Lakes Addiction Technology Transfer Center (ATTC) Network; 2006. pp. 1–6. [Google Scholar]
- WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): Development and general psychometric properties. Social Science & Medicine. 1998;46:1569–1585. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- WHOQOL Group. US Version WHOQOL-100 and Importance Items User’s Manual and Interpretation Guide. Seattle, WA: The World Health Organization and the University of Washington, Seattle; 2005. [Google Scholar]
- WHOQOL-SRPB. WHOQOL Spirituality, Religiousness and Personal Beliefs (SRPB) field-test instrument (pp. 1–25) Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- WHOQOL SRPB Group. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Social Science & Medicine. 2006;62:1486–1497. doi: 10.1016/j.socscimed.2005.08.001. [DOI] [PubMed] [Google Scholar]
- World Health Organization. ICD-10: International statistical classification of diseases and related health problems (10th revised ed. Vol. 1) Geneva, Switzerland: Author; 1992. [Google Scholar]
- Yates A. Multivariate exploratory data analysis: A perspective on exploratory factor analysis. Albany, NY: State University of New York Press; 1987. [Google Scholar]
- Zemore SE, Kaskutas LA. Helping, spirituality and Alcoholics Anonymous in recovery. Journal of Studies on Alcohol. 2004;65:383–391. doi: 10.15288/jsa.2004.65.383. [DOI] [PubMed] [Google Scholar]
- Zickuhr K, Smith A. Digital differences: Internet adoption over time. 2012. Washington, DC: Pew Internet & American Life Project. Archived by WebCite at http://www.webcitation.org/6HzK7wlzK. [Google Scholar]


