Abstract
Programmed cell death, a physiologic process for removing cells, is critically important in normal development and for elimination of damaged cells. Conversely, unattended cell death contributes to a variety of human disease pathogenesis. Thus, precise understanding of molecular mechanisms underlying control of cell death is important and relevant to public health. Recent studies emphasize that transforming growth factor-β-activated kinase 1 (TAK1) is a central regulator of cell death and is activated through a diverse set of intra- and extracellular stimuli. The physiologic importance of TAK1 and TAK1-binding proteins in cell survival and death has been demonstrated using a number of genetically engineered mice. These studies uncover an indispensable role of TAK1 and its binding proteins for maintenance of cell viability and tissue homeostasis in a variety of organs. TAK1 is known to control cell viability and inflammation through activating downstream effectors such as NF-κB and mitogen-activated protein kinases (MAPKs). It is also emerging that TAK1 regulates cell survival not solely through NF-κB but also through NF-κB-independent pathways such as oxidative stress and receptor-interacting protein kinase 1 (RIPK1) kinase activity-dependent pathway. Moreover, recent studies have identified TAK1's seemingly paradoxical role to induce programmed necrosis, also referred to as necroptosis. This review summarizes the consequences of TAK1 deficiency in different cell and tissue types from the perspective of cell death and also focuses on the mechanism by which TAK1 complex inhibits or promotes programmed cell death. This review serves to synthesize our current understanding of TAK1 in cell survival and death to identify promising directions for future research and TAK1's potential relevance to human disease pathogenesis.
Facts
TAK1 is activated by numerous exogenous and endogenous ligands, such as microbial lipopolysaccharide, IL-1, TNFα and TNF-related apoptosis-inducing ligand (TRAIL), and initiates cell signaling leading to the activation of NF-κB and MAPKs.
Loss of TAK1 activity results in apoptosis in most tissue types.
Prosurvival signaling, through downstream NF-κB, accounts for some but not all of the cell death observed when TAK1 is inhibited or deleted.
Conversely, hyperactivation of TAK1 leads to receptor-interacting protein kinase 3 (RIPK3)-dependent necroptosis.
Dysregulation of TAK1 signaling pathway in mice leads to tissue abnormalities resembling human disease pathogenesis.
Open Questions
What are the mechanisms by which TAK1 activity is regulated in response to the rich diversity of environmental and endogenous stimuli in vivo?
What is the precise mechanism by which TAK1 regulates apoptosis independently of NF-κB?
How does TAK1 promote RIPK1/RIPK3-dependent necroptosis?
Given TAK1's role as an inhibitor of apoptosis and inducer of necroptosis, how can inhibition of TAK1 be used therapeutically?
Programmed cell death is triggered under diverse biologic events including inflammation, tissue injury and during development. TAK1 is activated by a number of stressors such as cytokines and bacterial ligands, and then transmits the signal-transduction pathway leading to cellular responses. TAK1 has a powerful prosurvival role in activating the Iκb kinase (IKK)-NF-κB pathway, which has a number of target genes, many of which block apoptosis, promote cell proliferation and stimulate inflammatory responses.1, 2, 3 Loss of TAK1 sensitizes cells to death through many of the myriad pathways known to activate TAK1, including TNFα. However, accumulating results suggest that TAK1 is essential for cell survival, above and beyond its role in NF-κB activation through pathways that are discussed in this review. Furthermore, despite TAK1's prosurvival function, TAK1 has also been found to participate actively in the RIPK1- and RIPK3-mediated necroptosis pathway under some circumstances. The story of TAK1 in maintaining and disrupting life leads to the conceptual synthesis of TAK1 as a regulator of cell fate. This review discusses the role of TAK1 signaling in cell death by incorporating TAK1's multiple paths to cell survival and cell death. Control of survival and cell death may allow us to target specific cells, such as tumor cells, for particular types of cell death.
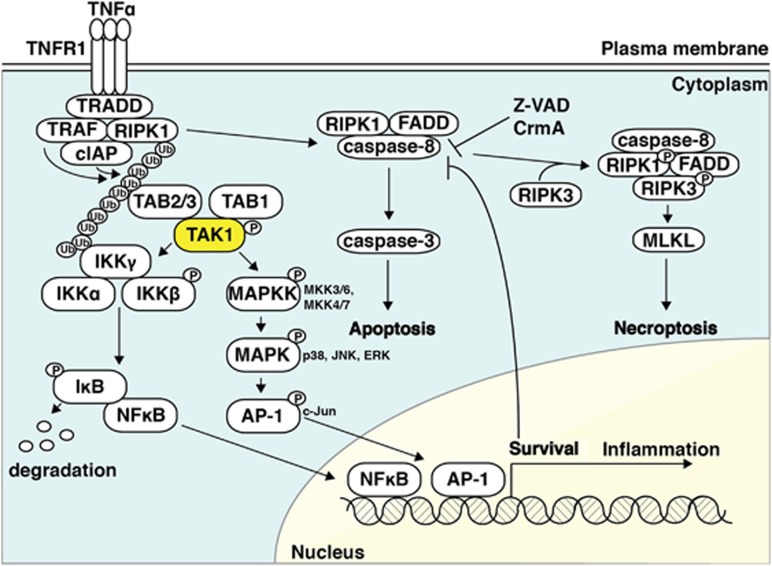
TAK1 Activation and Downstream Pathways
The kinase TAK1 was first identified as a mitogen-activated protein kinase kinase kinase (MAP3K) and found to be activated by TGFβ and bone morphologic protein.4 Since this original finding, TAK1 also has been shown to be activated by a number of signaling molecules including cytokines such as TNFα and IL-1; ligands that interact with Toll-like receptors, B-cell receptor and T-cell receptor; and the lipotoxic molecule, ceramide.5, 6, 7, 8, 9, 10, 11, 12, 13 Other endogenous death ligands of the TNF family, including TRAIL, also induce TAK1 activation.14, 15 Exogenous stressors and environmental changes such as osmotic stress, UV irradiation, ischemia and nutrient withdrawal activate TAK1.13, 14, 16, 17 Among these stimuli, the mechanism of TAK1 activation and its role in the TNFα signaling pathway has been extensively studied. Upon TNFα stimulation, adaptor molecules including TNFα receptor type-1-associated death domain protein (TRADD), TNFα receptor-associated factor 2 and 5 (TRAF2 and TRAF5), cellular inhibitor of apoptosis 1 and 2 (cIAP1/2) and RIPK1 are recruited to the receptor complex (TNF receptor 1 (TNFR1) Complex I) (Figure 1), in which RIPK1 acquires a K63-linked or linear polyubiquitin chain by E3 ligases, TRAF2/5 cIAP1/2 or linear ubiquitin chain assembly complex containing two E3 ligases HOIL-1 and HOIP.18, 19, 20, 21, 22 TAK1 is recruited and activated through TAK1-binding protein 2 (TAB2) binding to the RIPK1 polyubiquitin chain.23, 24 Upon binding the polyubiquitin chain, TAK1 phosphorylates and activates the IKK complex composed of IKKα, IKKβ and NEMO (also called IKKγ), which leads to phosphorylation and degradation of IκB resulting in activation of NF-κB (Figure 1). Activated TAK1 also phosphorylates and activates MAPKKs leading to activation of MAPKs such as ERK, p38 and JNK (Figure 1).6, 25 NF-κB and MAPKs induce downstream expression of inflammatory cytokines and antiapoptotic proteins such as cellular FLICE-like inhibitory protein (c-FLIP) and cIAPs.26, 27 Drawing a link between TAK1 signaling and metabolism, studies have found that starvation and TRAIL induce autophagy in which TAK1 is actively involved by activating AMP-activated protein kinase and IKKs.14, 17, 28, 29 In summary, TAK1 responds to exogenous stress conditions through a variety of mechanisms including TNFα family receptors, and activates cellular processes to mitigate stress conditions through intracellular signaling pathways including, but not limited to, IKK-NF-κB and MAPK pathways (Figure 1).
Figure 1.
TNFα induces cell survival, apoptosis and necroptosis. Upon TNFα stimulation, TNFR1 forms Complex I, in which RIPK1 acquires a polyubiquitin chain.18, 19, 20, 21 TAK1 binds to the polyubiquitin chain though TAB2, and activates the IKK complex, leading to the activation of NF-κB. TAK1 also activates MAPK cascades.6, 25 NF-κB and MAPKs induce expression of inflammatory cytokines and antiapoptotic proteins.26, 27 After Complex I formation, under some circumstances, the complex dissociates from TNFR1, leading to the formation of cytosolic protein complex known as Complex IIa composed of TRADD, FADD, RIPK1 and caspase-8.43 Caspase-8 activation initiates a caspase cascade, which leads to apoptotic cell death.44 If caspase-8 is inhibited, Complex IIb which include FADD, RIPK1 and RIPK3 is formed.45 RIPK1-RIPK3 executes necroptosis through downstream molecule such as MLKL46, 47, 48
The Roles of TAK1-Binding Proteins in TAK1 Activation
TAK1 forms complexes with its binding proteins TAB1, TAB2 and TAB3.30, 31, 32 TAB2 and TAB3 are close homologs, whereas TAB1 is structurally unrelated to TAB2 or TAB3. TAB1 and TAB2/TAB3 bind to the N-terminal kinase domain and the C-terminal region of TAK1, respectively. TAB1 mediates oligomerization, autophosphorylation and activation of TAK1.16, 33, 34 TAB1 is essential for TAK1 activation in response to osmotic stress but dispensable for cytokine-mediated TAK1 activation.16 O-linked glycosylation of TAB1 on S395 is implicated in activation of TAK1 activation in response to osmotic stress.35 In contrast, TAB2 and its analogous protein TAB3 have been shown to have an important role in activation of TAK1 in cytokine signaling. TAB2 and TAB3 each have Np14 zinc-finger domain, which is necessary for recruitment of TAK1 to the RIPK1 polyubiquitin chain in the TNFα signaling pathway (Figure 1).18, 24 Consistently, inhibition of TAB2 reduces TAK1 activity in several tissues and cell types.32, 36, 37 However, Broglie et al.38 described that loss of Tab2 in dermal fibroblasts rather prolonged and increased the activation of TAK1 following TNFα stimulation. TAK1 is normally transiently activated by TNFα and deactivated by protein phosphatase 6 (PP6)39 and protein phosphatase 2A.40 TAB2 tethers the interaction between TAK1 and PP6 on the RIPK1 polyubiquitin chain in the TNFα signaling pathway, which may explain how TAB2 deficiency could lead to sustained activation of TAK1. In this context, activation of TAK1 may be compensated for by TAB3. While structurally very different, TAB1 and TAB2, at least in the epidermis, intestinal epithelium and differentiated macrophages have been shown to function redundantly to activate TAK1.41, 42 As double deletion of Tab1 and Tab2 almost completely ablates TAK1 activity and phenocopies Tak1 deletion in the epidermis and intestinal epithelium, TAB3 does not appear to have a dominant role in TAK1 activation in these tissues. Further elucidation of the roles of these individual binding proteins requires more study, but it must be stressed that activation of TAK1 is regulated by TAB1, TAB2 and TAB3 in vivo, and their respective contributions are complex and depend upon tissue type and cellular context.
TAK1 Inhibits Apoptosis
When TAK1 is absent, cells are sensitive to cell death in response to several stressors. Among them, TAK1-regulated TNFα-induced cell death is well characterized. After TNFα receptor complex (Complex I) formation, under some circumstances, the TNFα-bound receptor complex dissociates from TNFR1, leading to molecular reorganization and the formation of a cytosolic death-inducing signaling complex including TRADD, FAS-associated protein with a death domain (FADD), RIPK1 and caspase-8, known as Complex IIa (Figure 1).43 In this complex, caspase-8 is dimerized, self-cleaved and activated to further activate downstream executioner caspases such as caspase-3, which leads to apoptotic cell death.44 Moreover, if caspase-8 is perturbed by gene deletion or inhibited by a viral protein CrmA or by pharmacologic inhibitors, TNFα induces another shift of protein complexes toward Complex IIb that include FADD, RIPK1 and RIPK3 (Figure 1).45 RIPK1-RIPK3 executes programmed necrosis, which is often called necroptosis, to induce an alternative cell death pathway when apoptosis fails.46, 47, 48 Inhibition of TAK1 is usually followed by caspase-8 and -3 activation in response to TNFα, which suggests that TAK1 inhibits caspase activation cascade to block apoptotic cell death.49 Thus, TAK1 is likely to blunt the formation or activation of Complex IIa. Recent studies revealed two major mechanisms through which TAK1 inhibits caspase activation (Figure 2).
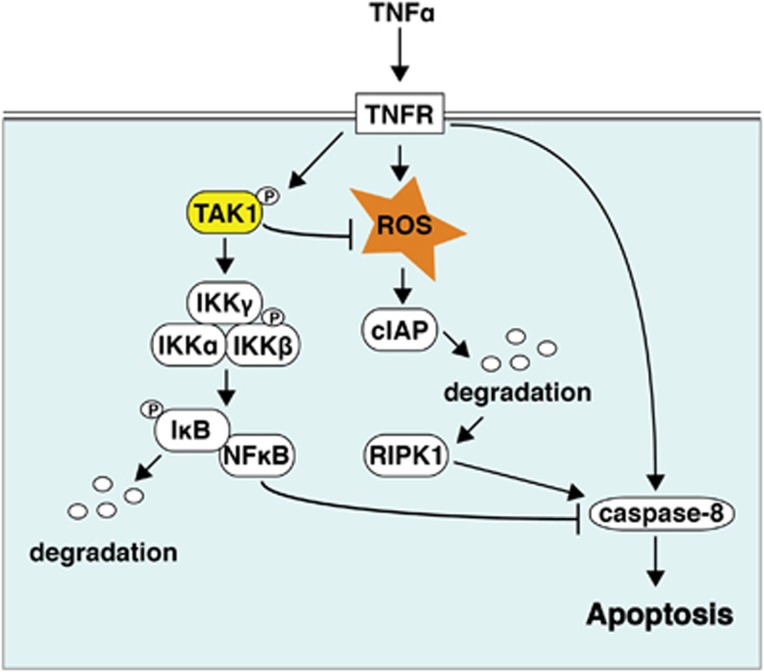
Figure 2.
TAK1 protects cells from TNFα-induced apoptosis through two distinct pathways. TAK1 is an upstream kinase of NF-κB.6 NF-κB transcriptionally upregulates antiapoptotic protein such as c-FLIP and IAP family proteins that inhibit caspase activation.26, 27 In addition, TAK1 prevents TNFα-induced accumulation of ROS. ROS potentially cause depletion of cIAP proteins,15 resulting in deubiquitination of RIPK1. This form of RIPK1 can activate caspase-8 in a kinase-dependent manner.61 Thus, TAK1-NF-κB pathway and TAK1-dependent antioxidant pathway coordinately inhibit caspase activation and apoptotic cell death
TAK1-NF-κB pathway: TAK1 is a well-documented upstream kinase of NF-κB.3, 6, 7 NF-κB transcriptionally upregulates antiapoptotic protein such as c-FLIP and IAP family proteins (Figure 1). The IAP family includes cIAP1, cIAP2 and XIAP, which can inhibit caspase activation.50 c-FLIP is structurally similar to caspases-8 but does not possess protease activity and forms a heterodimer with caspase-8, which competitively inhibits formation of highly active caspase-8 homodimer.51, 52 We note here that c-FLIP-caspase-8 heterodimer still possesses limited proteolytic activity,53, 54 which is important for cross-talk between apoptosis and necroptosis, as discussed later. Thus, it is feasible that TAK1 inhibits caspase activation through activation of NF-κB. However, it also suggests that an NF-κB-independent pathway is responsible for inhibition of apoptosis. In mouse models, Tak1 deletion causes more extensive cell death and tissue damage than ablation of NF-κB by deletion of IKKβ or NEMO/IKKγ (see Table 1). Intestinal epithelial-specific Tak1 gene deletion causes TNFα-dependent tissue disruption from embryonic day 18.5, whereas ablation of IKKβ or NEMO/IKKγ does not cause significant cell death at early postnatal days.55, 56 Hepatocyte-specific deletion of TAK1 triggers TNFα-dependent liver injury and hepatocellular carcinoma within 6 weeks of age, whereas loss of NF-κB activation by NEMO deletion causes much milder liver injury around 20 weeks of age.57 Furthermore, it appears that NF-κB activity is not always regulated by TAK1 in some tissues in vivo. For example, Tak1 deletion in blood vessels leads to TNFα-induced endothelial cell death without altering NF-κB activity.37 Thus, impairment of NF-κB may not be the sole mechanism for cell death in Tak1-deficient cells (Figure 2).
Table 1. Phenotypes of cell death gene deletion in mouse models.
| Gene | Phenotype of germline deletion | Summary of phenotypes in tissue-specific gene deletion |
|---|---|---|
| Ikkβ | Lethal E12–13106, 107, 108 | (Epidermis) Increased cell death—>Lethal P8–9109 (Intestinal epithelium) Normal110 (Liver) Normal111 (Hematopoietic system) T-cell death112 (Myeloid) Normal113 |
| NEMO (Ikkγ) | Lethal E12–13114, 115 | (Epidermis) Increased cell death—>Lethal P7–10116 (Intestinal epithelium) Inflammation—>Ccolitis after 3 weeks of age56 (Endothelium/blood vessel) Normal117 (Liver) Hepatocellular carcinoma around 9–12 months of age118 |
| Tak1 | Lethal E10–118, 25, 119 | (Epidermis) Increased cell death—>Lethal P5–782 (Intestinal epithelium) Increased cell death—>Lethal P055 (Inducible intestinal epithelium) Ileitis and loss of paneth cells55, 65 (Endothelium/blood vessel) Increased cell death, defective vascularization—>Lethal E10–1137 (Liver) Increased cell death—>Hepatocellular carcinoma within 6 weeks of age57, 83 (Hematopoietic system) Increased cell death—>Depletion of stem cells84, 85, 86 (Myeloid) Macrophage death, splenomegaly and hyperproliferation of neutrophils87, 89 |
| Tab1 | Lethal E15–16120, 121 | (Epidermis, intestinal epithelium) Normal but double deletion of Tab1 and Tab2 phenocopies Tak1 deletion41 (Endothelium/blood vessel) Normal37 (Liver) Normal36 (Macrophage) Cell death upon treatment with lipopolysaccharide42 |
| Tab2 | Lethal E12–13122 | (Epidermis, intestinal epithelium) Normal but double deletion of Tab1 and Tab2 phenocopies Tak1 deletion41 (Endothelium/blood vessel) Vessel dilation—>Lethal E12–1337 (Liver) Normal but mild fibrosis in aged mice36 (Macrophage) Cell death upon treatment with lipopolysaccharide42 |
| Tab3 | Normal123 | |
| Caspase 8 | Lethal E10–11124 | (Epidermis) Increased cell death—>Lethal by P792 (Inducible intestinal epithelium) Ileitis and loss of paneth cells, which can be restored by Ripk3 deletion93 (Liver) Normal125 (Endothelium/blood vessel) Defective vascularization125—>Lethal E10–12125 |
| Fadd | Lethal E10–12126, 127 | (Intestinal epithelium) Ileitis that can be restored by Ripk3 deletion95 |
|
c-Flip |
Lethal E10–11128
Defective vascularization |
(Epidermis) Increased cell death—>Lethal E10–14129
(Intestinal epithelium) Increased cell death —> Lethal by P10130
(Liver) Increased cell death131
(Myeloid) Splenomegaly and hyperproliferation of neutrophils132 |
| Ripk1 | Lethal E18–P080, 81, 133 Systemic inflammation, TNFα-induced apoptosis and RIPK3-induced necroptosis are the causes of mouse mortality80, 81 | |
| Ripk3 | Normal105 | |
|
Knock-in gene |
Phenotype of germline knock-in |
|
| Ripk1 kinase-dead | Normal97 | |
| Ripk3 kinase-dead | Lethal E10–11 Defective vascularization97 | |
TAK1-ROS-cIAP pathway: TNFα-induced caspase activation and subsequent cell death in Tak1-deficient cells is effectively blocked by gene deletion of Ripk1 or necrostatin-1, a pharmacologic inhibitor of RIPK1 kinase activity.49, 58, 59 Thus, Tak1 deficiency engages RIPK1-dependent apoptosis. However, previous studies demonstrate that extrinsic apoptosis induced by TNF family ligands is usually RIPK1-independent,60 and kinase activity of RIPK1 is not required for caspase activation.61 Only when cIAP is depleted by synthetic IAP antagonists (smac mimetics) or by genotoxic stress does TNFα or genotoxic stress induces RIPK1 kinase activity-dependent caspase-8 activation.62, 63 cIAPs are responsible for K63-linked polyubiquitination of RIPK1,64 which inhibits formation of Complex IIa (Figure 1).62 Interestingly, inhibition of TAK1 decreases the protein amount of cIAPs following stimulation of TNFα.15 Thus, TAK1 is important for maintenance of cIAP protein amount, which blocks Complex IIa activation. By what mechanism is cIAP reduced in Tak1-deficient cells? It has been demonstrated that Tak1 deficiency accumulates reactive oxygen species (ROS) in response to TNFα stimulation, and ROS scavengers rescue cell death in vitro and in vivo.15, 65, 66 One possible mechanism is that stress-induced ROS lead to degradation of cIAPs. Indeed, TNFα-induced loss of cIAPs in Tak1-deficient cells is restored by treatment with ROS scavenger, butylated hydroxyanisole.15 Because depletion of NF-κB only marginally increases ROS under the same experimental condition as Tak1 deletion,66 TAK1-ROS-cIAP pathway seems to act independently of TAK1-NF-κB pathway. Future studies need to identify the molecular pathways though which TAK1 modulates cellular redox status. In summary, not only activation of TAK1-IKK-NF-κB pathway but also TAK1 regulation of cellular redox system are the keys to inhibit apoptosis (Figure 2). Future efforts should focus on the unidentified mechanism of TAK1-dependent alteration of cellular redox status.
TAK1 as a Necroptosis Inducer
Is TAK1 only involved in caspase-dependent cell death? Another interesting topic is the relationship between TAK1 and a different form of programmed cell death, necroptosis. When apoptosis is blocked by inhibition of caspase-8, RIPK1 and RIPK3 form Complex IIb, and they execute necroptosis, a regulated form of necrosis (Figure 1). RIPK3 phosphorylates mixed lineage kinase domain-like (MLKL), which induces oligomerization of MLKL resulting in plasma membrane rupture.67, 68, 69 In human cells, it has been proposed that MLKL modulates phosphoglycerate mutase family member 5 (PGAM5) and dynamin-related protein 1 (Drp1), in which Drp1 mediates mitochondrial fragmentation, which is necessary for metabolic inactivation and induction of necroptosis.69, 70 However, recent evidence suggests that PGAM5 and Drp1 may not be required for execution of necroptosis in murine cells.71, 72 Nonetheless, catalytically active RIPK1 and RIPK3 are important for stable RIPK1-RIPK3 complex formation and subsequent execution of necroptotic cell death.73, 74, 75 In this context, necrostatin-1 is widely used for improving tissue damage mediated by necroptosis induction.61 A surprising finding regarding the regulation of RIPK1 and RIPK3 phosphorylation came from the analysis of Tab2-deficient fibroblasts, which exhibit sustained activation of TAK1 following TNFα stimulation.38 Despite the presence of TAK1 activation, Tab2-deficient fibroblasts are killed by TNFα challenge.49 Interestingly, while Tak1 deficiency induces caspase activation leading to apoptosis upon TNFα stimulation, Tab2 deficiency shows almost no caspase activation and results in cell death having typical necrotic features such as plasma membrane rupture.49 Furthermore, TNFα-induced cell death in Tab2-deficient fibroblasts is almost completely rescued by Ripk3 deletion, whereas Ripk3 deletion has no effect on Tak1-deficient fibroblasts. Thus, Tab2 deletion causes necroptosis following TNFα stimulation. Two lines of evidence show that sustained TAK1 activation causes RIPK3-dependent necroptosis. One is that enforced activation of TAK1 through overexpression induces RIPK3 phosphorylation and necroptosis. The other is that additional deletion of Tak1 in Tab2-deficient fibroblasts solely induces caspase-dependent apoptosis following TNFα stimulation.49 These results collectively reveal an unexpected role of TAK1 in cell death pathways, as an inducer of necroptosis (Figure 3). Furthermore, it has been shown that TAK1 activates RIPK3, reciprocally RIPK3 activates TAK1, and these activations are facilitated by RIPK1, which mediates TAK1-RIPK1-RIPK3 binding.49 Thus, TAK1-RIPK1-RIPK3 is activated by a positive feedforward mechanism (Figure 3).49 How is TAK-RIPK1-RIPK3 assembled? Deubiquitination of RIPK1 is known to be the critical process for assembly of the necroptotic complex.62, 76 Conversely, stabilization of RIPK1 polyubiquitin chain prevents necroptosis.76 As discussed earlier, TAB2 is a polyubiquitin chain-binding protein and directly binds to TAK1. Hence, TAB2 tethers the binding between TAK1 and polyubiquitin chain of RIPK1 (Figure 1). Thus, the absence of TAB2 prevents TAK1 binding to the RIPK1 polyubiquitin chain, which could lead to an alternative type of binding between TAK1 and RIPK1, resulting in activation of TAK1-RIPK1-RIPK3 assembly (Figure 3). Alternatively, under pathologic conditions, viral inhibition of caspase promotes deubiquitination of RIPK1 and releases TAK1 from the polyubiquitin chain, which may result in the assembly of TAK1-RIPK1-RIPK3 (Figure 3). These possibilities should be investigated in the future studies. Although it is clear that TAK1 promotes RIPK3 activity, the importance of TAK1 in necroptosis needs to be carefully considered. Our results suggest that Tak1 deletion induces caspase-8 activation but, even if caspase-8 is inhibited, Tak1-deficient cells still undergo cell death following TNFα stimulation.49 In line with this, combined inhibition of caspase and RIPK3 rescues TNFα-induced cell death in Tak1-deficient cells.58, 77, 78, 79 These results suggest that, although the default pathway of cell death in Tak1-deficient cells is apoptosis, Tak1 deficiency engages an alternative RIPK1-RIPK3 necroptosis pathway if the default pathway is blocked. Interestingly, even though RIPK1 was believed to be an essential mediator of RIPK3 activation, necroptosis can still be engaged with Ripk1 deletion.80, 81 Thus, necroptosis may be mediated through not only TAK1-RIPK1-RIPK3 complex but also through alternative complexes lacking either TAK1 or RIPK1. In summary, despite the fact that Tak1 deletion leads to hypersensitivity to TNFα-induced cell death (apoptosis), activation of TAK1 is also associated with TNFα-induced cell death (necroptosis). We will discuss later why TAK1 has such seemingly paradoxical roles in cell death.
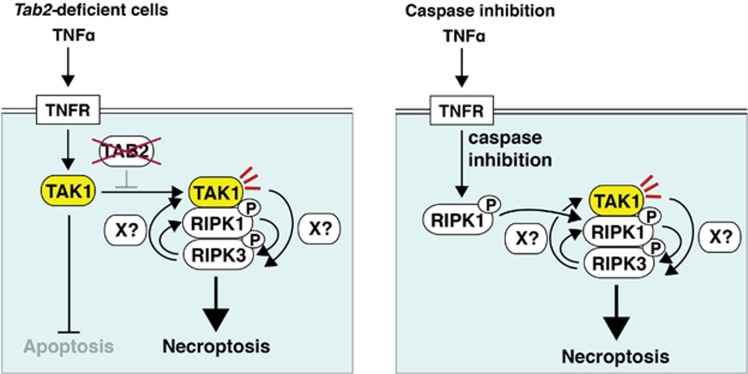
Figure 3.
TAK1 enhances necroptosis. RIPK3 is activated through two pathways: (1) deletion of Tab2 leads to TAK1 activation in a sustained manner following TNFα stimulation.38 Sustained activation of TAK1 binds to and activates RIPK1 and RIPK3. TAK1 can increase phosphorylation and activation of RIPK3, and conversely, RIPK3 can increase phosphorylation and activation of TAK1.49 However, it is still not clear whether TAK1 and RIPK3 directly phosphorylate each other; (2) when caspase-8 is blocked, RIPK1 and RIPK3 form Complex IIb to induce necroptosis. Phosphorylation of RIPK1 and RIPK3 are important for stable RIPK1-RIPK3 complex formation,73, 74, 75 where TAK1 is also activated and facilitates RIPK3 activation, resulting in the activation of a feedforward loop between TAK1-RIPK1-RIPK3
Pathology of Tak1 Deficiency in a Variety of Tissue in Mouse Models
Deficient TAK1 signaling in mice disrupts tissue homeostasis and provokes damage to tissues that often resembles human disease pathologies, as listed in Table 1. Epithelial cell-specific deletion of Tak1 in the epidermis or intestinal epithelium causes caspase activation and cell death leading to severe inflammation, which resembles psoriasis in the case of epidermal Tak1 deletion, and inflammatory bowel disease (IBD) in intestinal epithelium Tak1 deletion.55, 65, 66, 82 Endothelium-specific deletion of Tak1 causes endothelial cell death and blood vessel regression around E10–11, which results in embryonic lethality.37 Hepatocyte-specific deletion of Tak1 also causes cell death and liver injury.57, 83 However, unlike epithelial and endothelial tissues, Tak1 deficiency in hepatocytes does not cause profound tissue damage and is not associated with immediate animal mortality. Instead, Tak1-deficient hepatocyte death induces inflammation and promotes compensatory proliferation, which eventually leads to hepatocellular carcinoma within 6 weeks.57, 83 Hematopoietic-specific Tak1 deletion depletes hematopoietic progenitor cells, T cells and macrophages.10, 11, 12, 58, 84, 85, 86, 87 Deletion of TNF receptor 1 (Tnfr1) largely rescues these injuries and animal mortalities,37, 55, 57, 82, 83, 84, 85 demonstrating that TNFα is the major killer of Tak1-deficient cells in these tissues. However, some Tak1-deficient tissue injuries are still observed in Tnfr1-null background.37, 65, 84, 85 Thus, Tak1 deficiency appears to also induce TNFα-independent cell death in vivo through mechanisms likely to be mediated by other TAK1 stimuli, including bacterial moieties and nutrient and genotoxic stress. Nonetheless, these tissue injuries are associated with caspase activation and are not rescued by Ripk3 deletion, indicating that they are primarily apoptosis.37, 49, 55, 57, 82, 83, 84, 85, 88 We note here that the role of TAK1 in vivo may not be limited to prevention of cell death. For example, Tak1-deficient neutrophils hyperproliferate rather than dying spontaneously, leading to splenomegaly and myelomonocytic leukemia.87, 89 Although TAK1 is known as an activator of NF-κB and p38 MAPK, Tak1 deletion in neutrophils increases activity of these downstream factors, which warrants further mechanistic analysis. Finally, we recently show that Tab2 deletion exaggerates wound-induced cell death and delays wound healing in vivo.49 As Tab2 deletion potentially results in hyperactivation of TAK1 in dermal fibroblasts as discussed earlier and the delay in wound healing is restored by blocking necroptosis (Ripk3 deletion), TAK1 is likely to be actively involved in induction of necroptosis at least in the wound response. TAK1 may also be potentially hyperactivated when caspase is exogenously inhibited by viral infection or under yet unidentified conditions, which could be associated with pathologic necroptotic conditions such as ischemic tissue injuries and systemic inflammation.90, 91
Functional Interaction of TAK1 and Other Cell Death Molecules In Vivo
The physiologic importance of other cell death molecules has also been extensively studied for the past several years, and research has revealed that programmed cell death deficiencies lead to disparate pathologies (Table 1). Interestingly, there are many phenotypic similarities among mouse models harboring deletion of Tak1 and other cell death genes (Table 1), suggesting in vivo functional interactions among them. The most surprising similarity is shared by mice having gene deletion of Tak1 or caspase-8. For example, either Tak1 or caspase-8 deletion in the epidermis results in psoriasis-like skin inflammation resulting in animal mortality around postnatal days 5–8 (P5–8).82, 92 Inducible deletion of Tak1 or caspase-8 in the intestinal epithelium causes IBD-like intestinal inflammation, which is associated with loss of a specific cell type known as paneth cells.55, 93 Similarly, epidermal- and intestinal epithelium-specific deletion of Fadd, which abrogates caspase-8 activation, causes inflammatory skin disease and IBD-like ileitis.94, 95 Although either Tak1 or Fadd/caspase-8 deletion causes cell death, the types of cell death are different. Tak1 deletion is associated with the activation of downstream caspase-3,55, 82 whereas deletion of caspase-8 induces necroptosis in vivo, which is rescued by deletion of Ripk3.54, 95, 96 Why are the timing and features of tissue injury so similar in mice having deletion of Tak1 or caspase-8? There is a well-studied inhibitory regulation from apoptosis to necroptosis (Figure 4, blue inhibition arrow). Thus, inhibition of caspase-8 activates necroptosis. The recent finding of TAK1 as a mediator of necroptosis raises the interesting possibility that there is an additional inhibitory regulation from necroptosis to apoptosis (Figure 4, red inhibition arrow). Two lines of evidence support the idea that necroptosis inhibits apoptosis: (1) inhibition of RIPK3 by expressing a kinase-dead version of RIPK3 is reported to cause apoptotic cell death in vivo, which results in blood vessel abnormalities similar to endothelial-specific deletion of Tak1;37, 97 (2) deletion of Ripk1 primarily induces apoptotic cell death and tissue injury in vivo, although necroptosis is also induced.80, 81 Thus, inhibition and/or deletion of any part of the necroptotic protein kinase cascade (TAK1, RIPK1 or RIPK3) activates apoptotic cell death in vivo. Based on these, we propose that apoptosis and necroptosis are reciprocally regulated (Figure 4). Because of this reciprocal regulation, if one cell death pathway is inhibited, the other cell death is spontaneously activated, resulting in similar tissue injuries with the same timing in Tak1 or caspase-8-deficient tissues. What are the molecular mechanisms for these inhibitory reciprocal regulations? Caspase-8-c-FLIP heterodimer is known to be the key modulator for inhibition of necroptosis.51, 54, 98, 99 Deletion of c-Flip causes embryonic lethality with blood vessel abnormality similar to deletion of caspase-8 or of Tak1 (Table 1).98 Thus far, two mechanisms for caspase-c-FLIP inhibition of necroptosis are proposed: one is that caspase-8-c-FLIP cleaves and degrades RIPK1 and RIPK3;100, 101 and the other is that caspase-8 cleaves and degrades a deubiquitinase CYLD, resulting in stabilization of the polyubiquitin chain of RIPK1, which prevents RIPK3 activation.76 In contrast to caspase-8-c-FLIP regulation of necroptosis, the regulation of apoptosis by necroptosis signaling proteins is just beginning to be investigated. It has thus far been clear that the necroptosis-mediated inhibition of apoptosis possesses unique and complex features. Only manipulation of TAK1 induces predictable outcomes, in which both deletion of Tak1 gene and inhibition of TAK1 by a selective inhibitor, 5Z-7-oxozeaenol,102 activates apoptotic cell death.103, 104 In contrast, it is very puzzling that inhibition and gene deletion of RIPK1 and RIPK3 result in different phenotypes. Inhibition of RIPK3 kinase activity activates caspases and tissue injury,97 whereas deletion of Ripk3 does not cause any abnormality.105 Conversely, inhibition of RIPK1 by knocking-in a kinase-dead version of RIPK1 or necrostatin-1 treatment does not cause any tissue injury,47, 97 whereas deletion of Ripk1 causes cell death and systemic inflammation in vivo.80, 81 It should be of immediate interest to elucidate the molecular mechanism of how TAK1, RIPK1 and RIPK3 interplay to inhibit apoptosis pathways.
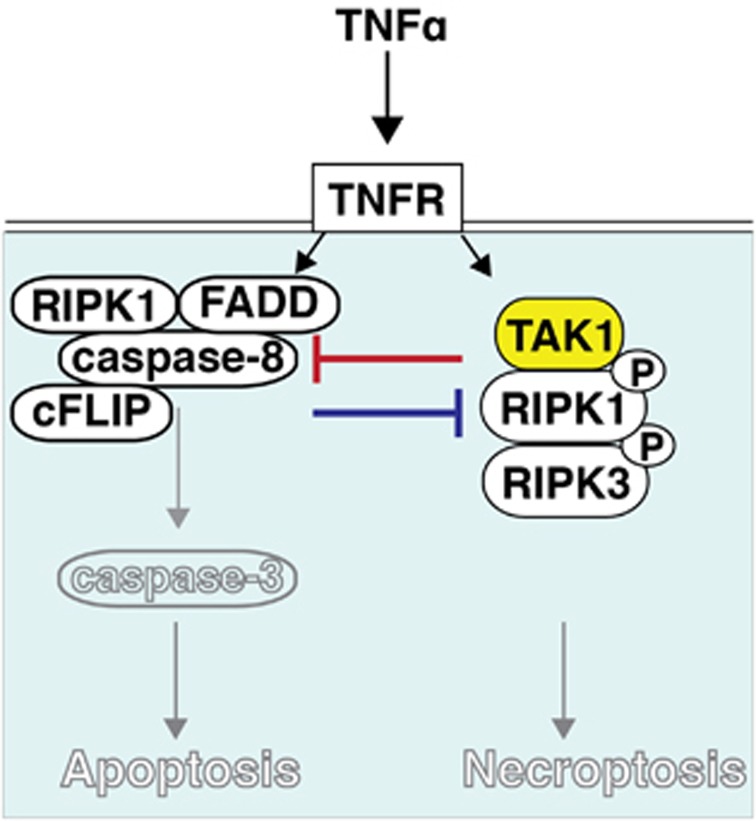
Figure 4.
TAK1 and caspase are reciprocally regulated. Recent evidence indicates that apoptosis and necroptosis are reciprocally regulated. Inhibition of caspase or deletion of c-FLIP induces necroptosis, whereas inhibition of TAK1 or RIPK3 induces apoptosis. We propose that the balance between apoptotic and necroptotic signals prevents cell death under normal conditions, and any event that causes imbalance between these reciprocal inhibitions, such as treatment with a caspase inhibitor, leads to cell death
Conclusions
It is clear that TAK1 is a key molecular component in the determination of cell fate. Historically, the role of TAK1 has been considered prosurvival, first characterized by antiapoptotic proteins downstream of NF-κB and cell growth and proliferation downstream of MAPK pathways. We now know that TAK1 engages multiple downstream cell death pathways in response to a rich diversity of environmental and endogenous stimuli. As an inhibitor of caspase activation, TAK1 prevents TNFα-mediated apoptotic cell death through modulation of the RIPK1-FADD-caspase-8 pathway. An NF-κB-independent cell survival pathway downstream of TAK1 has just begun to be explored, with interesting possibilities involving ROS and cIAPs. However, when caspase-8 is blocked or TAK1 activation is sustained, TAK1 acts as a cell death inducer through necroptosis activation. Similarly, the mechanism by which TAK1 promotes RIPK1/RIPK3-dependent necroptosis warrants further study. Enforcing cell death pathways can be used therapeutically to kill undesired cells such as tumor cells. Inhibition of TAK1 induces stress-dependent apoptosis. Furthermore, although some tumor cells are known to gain antiapoptotic functions, inhibition of TAK1 alone is effective as inhibition of both TAK1 and caspase still induces cell death. Thus, inhibition of TAK1 is one of the most promising approaches to therapeutic cell killing, as proposed also in recent cancer studies.102, 105 This further emphasizes the importance of studies elucidating the regulatory mechanisms of TAK1 in the cell death network.
Glossary
- c-FLIP
cellular FLICE-like inhibitory protein
- cIAP
cellular inhibitor of apoptosis
- Drp1
dynamin-related protein 1
- FADD
FAS-associated via death domain
- IBD
inflammatory bowel disease
- IKK
Iκb kinase
- MAPK
mitogen-activated protein kinase
- MLKL
mixed lineage kinase domain-like
- PGAM5
phosphoglycerate mutase family member 5
- PP6
protein phosphatase 6
- RIPK1
receptor-interacting protein kinase 1
- RIPK3
receptor-interacting protein kinase 3
- ROS
reactive oxygen species
- TAB1
TAK1-binding protein 1
- TAB2
TAK1-binding protein 2
- TAK1
TGF-β-activated kinase 1
- TGFβ
transforming growth factor-β
- TNFR
TNF receptor
- TRADD
TNFα receptor type-1-associated death domain protein
- TRAF
TNFα receptor-associated factor
- TRAIL
TNF-related apoptosis-inducing ligand
The authors declare no conflict of interest.
Footnotes
Edited by G Melino
References
- Gilmore TD.NF-κB transcription factors, 2014. Available at: http://www.NF-?B.org .
- Pahl HL. Activators and target genes of Rel/NF-κB transcription factors. Oncogene. 1999;18:6853–6866. doi: 10.1038/sj.onc.1203239. [DOI] [PubMed] [Google Scholar]
- Hayden MS, Ghosh S. Shared principles in NF-κB signaling. Cell. 2008;132:344–362. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K, Shirakabe K, Shibuya H, Irie K, Oishi I, Ueno N, et al. Identification of a member of the MAPKKK family as a potential mediator of TGF-β signal transduction. Science. 1995;270:2008–2011. doi: 10.1126/science.270.5244.2008. [DOI] [PubMed] [Google Scholar]
- Ajibade AA, Wang HY, Wang RF. Cell type-specific function of TAK1 in innate immune signaling. Trends Immunol. 2013;34:307–316. doi: 10.1016/j.it.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Ninomiya-Tsuji J, Kishimoto K, Hiyama A, Inoue J, Cao Z, Matsumoto K. The kinase TAK1 can activate the NIK-IκB as well as the MAP kinase cascade in the IL-1 signalling pathway. Nature. 1999;398:252–256. doi: 10.1038/18465. [DOI] [PubMed] [Google Scholar]
- Sakurai H. Targeting of TAK1 in inflammatory disorders and cancer. Trends Pharmacol Sci. 2012;33:522–530. doi: 10.1016/j.tips.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Sato S, Sanjo H, Takeda K, Ninomiya-Tsuji J, Yamamoto M, Kawai T, et al. Essential function for the kinase TAK1 in innate and adaptive immune responses. Nat Immunol. 2005;6:1087–1095. doi: 10.1038/ni1255. [DOI] [PubMed] [Google Scholar]
- Tseng PH, Matsuzawa A, Zhang W, Mino T, Vignali DA, Karin M. Different modes of ubiquitination of the adaptor TRAF3 selectively activate the expression of type I interferons and proinflammatory cytokines. Nat Immunol. 2010;11:70–75. doi: 10.1038/ni.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato S, Sanjo H, Tsujimura T, Ninomiya-Tsuji J, Yamamoto M, Kawai T, et al. TAK1 is indispensable for development of T cells and prevention of colitis by the generation of regulatory T cells. Int Immunol. 2006;18:1405–1411. doi: 10.1093/intimm/dxl082. [DOI] [PubMed] [Google Scholar]
- Wan YY, Chi H, Xie M, Schneider MD, Flavell RA. The kinase TAK1 integrates antigen and cytokine receptor signaling for T cell development, survival and function. Nat Immunol. 2006;7:851–858. doi: 10.1038/ni1355. [DOI] [PubMed] [Google Scholar]
- Liu HH, Xie M, Schneider MD, Chen ZJ. Essential role of TAK1 in thymocyte development and activation. Proc Natl Acad Sci USA. 2006;103:11677–11682. doi: 10.1073/pnas.0603089103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirakabe K, Yamaguchi K, Shibuya H, Irie K, Matsuda S, Moriguchi T, et al. TAK1 mediates the ceramide signaling to stress-activated protein kinase/c-Jun N-terminal kinase. J Biol Chem. 1997;272:8141–8144. doi: 10.1074/jbc.272.13.8141. [DOI] [PubMed] [Google Scholar]
- Herrero-Martin G, Hoyer-Hansen M, Garcia-Garcia C, Fumarola C, Farkas T, Lopez-Rivas A, et al. TAK1 activates AMPK-dependent cytoprotective autophagy in TRAIL-treated epithelial cells. EMBO J. 2009;28:677–685. doi: 10.1038/emboj.2009.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morioka S, Omori E, Kajino T, Kajino-Sakamoto R, Matsumoto K, Ninomiya-Tsuji J. TAK1 kinase determines TRAIL sensitivity by modulating reactive oxygen species and cIAP. Oncogene. 2009;28:2257–2265. doi: 10.1038/onc.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagaki M, Omori E, Kim JY, Komatsu Y, Scott G, Ray MK, et al. TAK1-binding protein 1, TAB1, mediates osmotic stress-induced TAK1 activation but is dispensable for TAK1-mediated cytokine signaling. J Biol Chem. 2008;283:33080–33086. doi: 10.1074/jbc.M807574200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie M, Zhang D, Dyck JR, Li Y, Zhang H, Morishima M, et al. A pivotal role for endogenous TGF-β-activated kinase-1 in the LKB1/AMP-activated protein kinase energy-sensor pathway. Proc Natl Acad Sci USA. 2006;103:17378–17383. doi: 10.1073/pnas.0604708103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ea CK, Deng L, Xia ZP, Pineda G, Chen ZJ. Activation of IKK by TNFα requires site-specific ubiquitination of RIP1 and polyubiquitin binding by NEMO. Mol Cell. 2006;22:245–257. doi: 10.1016/j.molcel.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Mahoney DJ, Cheung HH, Mrad RL, Plenchette S, Simard C, Enwere E, et al. Both cIAP1 and cIAP2 regulate TNFα-mediated NF-κB activation. Proc Natl Acad Sci USA. 2008;105:11778–11783. doi: 10.1073/pnas.0711122105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokunaga F, Sakata S, Saeki Y, Satomi Y, Kirisako T, Kamei K, et al. Involvement of linear polyubiquitylation of NEMO in NF-κB activation. Nat Cell Biol. 2009;11:123–132. doi: 10.1038/ncb1821. [DOI] [PubMed] [Google Scholar]
- Haas TL, Emmerich CH, Gerlach B, Schmukle AC, Cordier SM, Rieser E, et al. Recruitment of the linear ubiquitin chain assembly complex stabilizes the TNF-R1 signaling complex and is required for TNF-mediated gene induction. Mol Cell. 2009;36:831–844. doi: 10.1016/j.molcel.2009.10.013. [DOI] [PubMed] [Google Scholar]
- Gerlach B, Cordier SM, Schmukle AC, Emmerich CH, Rieser E, Haas TL, et al. Linear ubiquitination prevents inflammation and regulates immune signalling. Nature. 2011;471:591–596. doi: 10.1038/nature09816. [DOI] [PubMed] [Google Scholar]
- Kishida S, Sanjo H, Akira S, Matsumoto K, Ninomiya-Tsuji J. TAK1-binding protein 2 facilitates ubiquitination of TRAF6 and assembly of TRAF6 with IKK in the IL-1 signaling pathway. Genes Cells. 2005;10:447–454. doi: 10.1111/j.1365-2443.2005.00852.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanayama A, Seth RB, Sun L, Ea CK, Hong M, Shaito A, et al. TAB2 and TAB3 activate the NF-κB pathway through binding to polyubiquitin chains. Mol Cell. 2004;15:535–548. doi: 10.1016/j.molcel.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Shim JH, Xiao C, Paschal AE, Bailey ST, Rao P, Hayden MS, et al. TAK1, but not TAB1 or TAB2, plays an essential role in multiple signaling pathways in vivo. Genes Dev. 2005;19:2668–2681. doi: 10.1101/gad.1360605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L, Kamata H, Solinas G, Luo JL, Maeda S, Venuprasad K, et al. The E3 ubiquitin ligase itch couples JNK activation to TNFα-induced cell death by inducing c-FLIP(L) turnover. Cell. 2006;124:601–613. doi: 10.1016/j.cell.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Wang CY, Mayo MW, Korneluk RG, Goeddel DV, Baldwin AS., Jr NF-κB antiapoptosis: induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science. 1998;281:1680–1683. doi: 10.1126/science.281.5383.1680. [DOI] [PubMed] [Google Scholar]
- Momcilovic M, Hong SP, Carlson M. Mammalian TAK1 activates Snf1 protein kinase in yeast and phosphorylates AMP-activated protein kinase in vitro. J Biol Chem. 2006;281:25336–25343. doi: 10.1074/jbc.M604399200. [DOI] [PubMed] [Google Scholar]
- Criollo A, Niso-Santano M, Malik SA, Michaud M, Morselli E, Marino G, et al. Inhibition of autophagy by TAB2 and TAB3. EMBO J. 2011;30:4908–4920. doi: 10.1038/emboj.2011.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibuya H, Yamaguchi K, Shirakabe K, Tonegawa A, Gotoh Y, Ueno N, et al. TAB1: an activator of the TAK1 MAPKKK in TGF-β signal transduction. Science. 1996;272:1179–1182. doi: 10.1126/science.272.5265.1179. [DOI] [PubMed] [Google Scholar]
- Takaesu G, Kishida S, Hiyama A, Yamaguchi K, Shibuya H, Irie K, et al. TAB2, a novel adaptor protein, mediates activation of TAK1 MAPKKK by linking TAK1 to TRAF6 in the IL-1 signal transduction pathway. Mol Cell. 2000;5:649–658. doi: 10.1016/s1097-2765(00)80244-0. [DOI] [PubMed] [Google Scholar]
- Ishitani T, Takaesu G, Ninomiya-Tsuji J, Shibuya H, Gaynor RB, Matsumoto K. Role of the TAB2-related protein TAB3 in IL-1 and TNF signaling. EMBO J. 2003;22:6277–6288. doi: 10.1093/emboj/cdg605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholz R, Sidler CL, Thali RF, Winssinger N, Cheung PC, Neumann D. Autoactivation of transforming growth factor β-activated kinase 1 is a sequential bimolecular process. J Biol Chem. 2010;285:25753–25766. doi: 10.1074/jbc.M109.093468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishimoto K, Matsumoto K, Ninomiya-Tsuji J. TAK1 mitogen-activated protein kinase kinase kinase is activated by autophosphorylation within its activation loop. J Biol Chem. 2000;275:7359–7364. doi: 10.1074/jbc.275.10.7359. [DOI] [PubMed] [Google Scholar]
- Pathak S, Borodkin VS, Albarbarawi O, Campbell DG, Ibrahim A, van Aalten DM. O-GlcNAcylation of TAB1 modulates TAK1-mediated cytokine release. EMBO J. 2012;31:1394–1404. doi: 10.1038/emboj.2012.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda Y, Morioka S, Matsumoto K, Ninomiya-Tsuji J. TAK1 binding protein 2 is essential for liver protection from stressors. PLoS One. 2014;9:e88037. doi: 10.1371/journal.pone.0088037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morioka S, Inagaki M, Komatsu Y, Mishina Y, Matsumoto K, Ninomiya-Tsuji J. TAK1 kinase signaling regulates embryonic angiogenesis by modulating endothelial cell survival and migration. Blood. 2012;120:3846–3857. doi: 10.1182/blood-2012-03-416198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broglie P, Matsumoto K, Akira S, Brautigan DL, Ninomiya-Tsuji J. Transforming growth factor β-activated kinase 1 (TAK1) kinase adaptor, TAK1-binding protein 2, plays dual roles in TAK1 signaling by recruiting both an activator and an inhibitor of TAK1 kinase in tumor necrosis factor signaling pathway. J Biol Chem. 2010;285:2333–2339. doi: 10.1074/jbc.M109.090522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajino T, Ren H, Iemura S, Natsume T, Stefansson B, Brautigan DL, et al. Protein phosphatase 6 down-regulates TAK1 kinase activation in the IL-1 signaling pathway. J Biol Chem. 2006;281:39891–39896. doi: 10.1074/jbc.M608155200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SI, Kwak JH, Wang L, Choi ME. Protein phosphatase 2A is a negative regulator of transforming growth factor-β1-induced TAK1 activation in mesangial cells. J Biol Chem. 2008;283:10753–10763. doi: 10.1074/jbc.M801263200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omori E, Inagaki M, Mishina Y, Matsumoto K, Ninomiya-Tsuji J. Epithelial transforming growth factor β-activated kinase 1 (TAK1) is activated through two independent mechanisms and regulates reactive oxygen species. Proc Natl Acad Sci USA. 2012;109:3365–3370. doi: 10.1073/pnas.1116188109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihaly SR, Morioka S, Ninomiya-Tsuji J, Takaesu G. Activated macrophage survival is coordinated by TAK1 binding proteins. PLoS One. 2014;9:e94982. doi: 10.1371/journal.pone.0094982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micheau O, Tschopp J. Induction of TNF receptor I-mediated apoptosis via two sequential signaling complexes. Cell. 2003;114:181–190. doi: 10.1016/s0092-8674(03)00521-x. [DOI] [PubMed] [Google Scholar]
- Vandenabeele P, Declercq W, Van Herreweghe F, Vanden Berghe T. The role of the kinases RIP1 and RIP3 in TNF-induced necrosis. Sci Signal. 2010;3:re4. doi: 10.1126/scisignal.3115re4. [DOI] [PubMed] [Google Scholar]
- Vandenabeele P, Galluzzi L, Vanden Berghe T, Kroemer G. Molecular mechanisms of necroptosis: an ordered cellular explosion. Nat Rev Mol Cell Biol. 2010;11:700–714. doi: 10.1038/nrm2970. [DOI] [PubMed] [Google Scholar]
- Kaczmarek A, Vandenabeele P, Krysko DV. Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity. 2013;38:209–223. doi: 10.1016/j.immuni.2013.02.003. [DOI] [PubMed] [Google Scholar]
- Degterev A, Hitomi J, Germscheid M, Ch'en IL, Korkina O, Teng X, et al. Identification of RIP1 kinase as a specific cellular target of necrostatins. Nat Chem Biol. 2008;4:313–321. doi: 10.1038/nchembio.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S, Wang L, Miao L, Wang T, Du F, Zhao L, et al. Receptor interacting protein kinase-3 determines cellular necrotic response to TNF-α. Cell. 2009;137:1100–1111. doi: 10.1016/j.cell.2009.05.021. [DOI] [PubMed] [Google Scholar]
- Morioka S, Broglie P, Omori E, Ikeda Y, Takaesu G, Matsumoto K, et al. TAK1 kinase switches cell fate from apoptosis to necrosis following TNF stimulation. J Cell Biol. 2014;204:607–623. doi: 10.1083/jcb.201305070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deveraux QL, Roy N, Stennicke HR, Van Arsdale T, Zhou Q, Srinivasula SM, et al. IAPs block apoptotic events induced by caspase-8 and cytochrome c by direct inhibition of distinct caspases. EMBO J. 1998;17:2215–2223. doi: 10.1093/emboj/17.8.2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberst A, Green DR. It cuts both ways: reconciling the dual roles of caspase 8 in cell death and survival. Nat Rev Mol Cell Biol. 2011;12:757–763. doi: 10.1038/nrm3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irmler M, Thome M, Hahne M, Schneider P, Hofmann K, Steiner V, et al. Inhibition of death receptor signals by cellular FLIP. Nature. 1997;388:190–195. doi: 10.1038/40657. [DOI] [PubMed] [Google Scholar]
- Chang DW, Xing Z, Pan Y, Algeciras-Schimnich A, Barnhart BC, Yaish-Ohad S, et al. c-FLIP(L) is a dual function regulator for caspase-8 activation and CD95-mediated apoptosis. EMBO J. 2002;21:3704–3714. doi: 10.1093/emboj/cdf356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberst A, Dillon CP, Weinlich R, McCormick LL, Fitzgerald P, Pop C, et al. Catalytic activity of the caspase-8-FLIP(L) complex inhibits RIPK3-dependent necrosis. Nature. 2011;471:363–367. doi: 10.1038/nature09852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajino-Sakamoto R, Inagaki M, Lippert E, Akira S, Robine S, Matsumoto K, et al. Enterocyte-derived TAK1 signaling prevents epithelium apoptosis and the development of ileitis and colitis. J Immunol. 2008;181:1143–1152. doi: 10.4049/jimmunol.181.2.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nenci A, Becker C, Wullaert A, Gareus R, van Loo G, Danese S, et al. Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature. 2007;446:557–561. doi: 10.1038/nature05698. [DOI] [PubMed] [Google Scholar]
- Bettermann K, Vucur M, Haybaeck J, Koppe C, Janssen J, Heymann F, et al. TAK1 suppresses a NEMO-dependent but NF-κB-independent pathway to liver cancer. Cancer Cell. 2010;17:481–496. doi: 10.1016/j.ccr.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Lamothe B, Lai Y, Xie M, Schneider MD, Darnay BG. TAK1 is essential for osteoclast differentiation and is an important modulator of cell death by apoptosis and necroptosis. Mol Cell Biol. 2013;33:582–595. doi: 10.1128/MCB.01225-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arslan SC, Scheidereit C. The prevalence of TNFα-induced necrosis over apoptosis is determined by TAK1-RIP1 interplay. PLoS One. 2011;6:e26069. doi: 10.1371/journal.pone.0026069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ting AT, Pimentel-Muinos FX, Seed B. RIP mediates tumor necrosis factor receptor 1 activation of NF-κB but not Fas/APO-1-initiated apoptosis. EMBO J. 1996;15:6189–6196. [PMC free article] [PubMed] [Google Scholar]
- Ofengeim D, Yuan J. Regulation of RIP1 kinase signalling at the crossroads of inflammation and cell death. Nat Rev Mol Cell Biol. 2013;14:727–736. doi: 10.1038/nrm3683. [DOI] [PubMed] [Google Scholar]
- Wang L, Du F, Wang X. TNF-α induces two distinct caspase-8 activation pathways. Cell. 2008;133:693–703. doi: 10.1016/j.cell.2008.03.036. [DOI] [PubMed] [Google Scholar]
- Tenev T, Bianchi K, Darding M, Broemer M, Langlais C, Wallberg F, et al. The Ripoptosome, a signaling platform that assembles in response to genotoxic stress and loss of IAPs. Mol Cell. 2011;43:432–448. doi: 10.1016/j.molcel.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Bertrand MJ, Milutinovic S, Dickson KM, Ho WC, Boudreault A, Durkin J, et al. cIAP1 and cIAP2 facilitate cancer cell survival by functioning as E3 ligases that promote RIP1 ubiquitination. Mol Cell. 2008;30:689–700. doi: 10.1016/j.molcel.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Kajino-Sakamoto R, Omori E, Nighot PK, Blikslager AT, Matsumoto K, Ninomiya-Tsuji J. TGF-β-activated kinase 1 signaling maintains intestinal integrity by preventing accumulation of reactive oxygen species in the intestinal epithelium. J Immunol. 2010;185:4729–4737. doi: 10.4049/jimmunol.0903587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omori E, Morioka S, Matsumoto K, Ninomiya-Tsuji J. TAK1 regulates reactive oxygen species and cell death in keratinocytes, which is essential for skin integrity. J Biol Chem. 2008;283:26161–26168. doi: 10.1074/jbc.M804513200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Sun L, Su L, Rizo J, Liu L, Wang LF, et al. Mixed lineage kinase domain-like protein MLKL causes necrotic membrane disruption upon phosphorylation by RIP3. Mol Cell. 2014;54:133–146. doi: 10.1016/j.molcel.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Cai Z, Jitkaew S, Zhao J, Chiang HC, Choksi S, Liu J, et al. Plasma membrane translocation of trimerized MLKL protein is required for TNF-induced necroptosis. Nat Cell Biol. 2014;16:55–65. doi: 10.1038/ncb2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun L, Wang H, Wang Z, He S, Chen S, Liao D, et al. Mixed lineage kinase domain-like protein mediates necrosis signaling downstream of RIP3 kinase. Cell. 2012;148:213–227. doi: 10.1016/j.cell.2011.11.031. [DOI] [PubMed] [Google Scholar]
- Wang Z, Jiang H, Chen S, Du F, Wang X. The mitochondrial phosphatase PGAM5 functions at the convergence point of multiple necrotic death pathways. Cell. 2012;148:228–243. doi: 10.1016/j.cell.2011.11.030. [DOI] [PubMed] [Google Scholar]
- Remijsen Q, Goossens V, Grootjans S, Van den Haute C, Vanlangenakker N, Dondelinger Y, et al. Depletion of RIPK3 or MLKL blocks TNF-driven necroptosis and switches towards a delayed RIPK1 kinase-dependent apoptosis. Cell Death Dis. 2014;5:e1004. doi: 10.1038/cddis.2013.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JM, Czabotar PE, Hildebrand JM, Lucet IS, Zhang JG, Alvarez-Diaz S, et al. The pseudokinase MLKL mediates necroptosis via a molecular switch mechanism. Immunity. 2013;39:443–453. doi: 10.1016/j.immuni.2013.06.018. [DOI] [PubMed] [Google Scholar]
- Cho YS, Challa S, Moquin D, Genga R, Ray TD, Guildford M, et al. Phosphorylation-driven assembly of the RIP1–RIP3 complex regulates programmed necrosis and virus-induced inflammation. Cell. 2009;137:1112–1123. doi: 10.1016/j.cell.2009.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S, Wang L, Miao L, Wang T, Du F, Zhao L, et al. Receptor interacting protein kinase-3 determines cellular necrotic response to TNF-α. Cell. 2009;137:1100–1111. doi: 10.1016/j.cell.2009.05.021. [DOI] [PubMed] [Google Scholar]
- Zhang DW, Shao J, Lin J, Zhang N, Lu BJ, Lin SC, et al. RIP3, an energy metabolism regulator that switches TNF-induced cell death from apoptosis to necrosis. Science. 2009;325:332–336. doi: 10.1126/science.1172308. [DOI] [PubMed] [Google Scholar]
- O'Donnell MA, Perez-Jimenez E, Oberst A, Ng A, Massoumi R, Xavier R, et al. Caspase 8 inhibits programmed necrosis by processing CYLD. Nat Cell Biol. 2011;13:1437–1442. doi: 10.1038/ncb2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arslan SC, Scheidereit C. The prevalence of TNFα-induced necrosis over apoptosis is determined by TAK1-RIP1 interplay. PLoS One. 2011;6:e26069. doi: 10.1371/journal.pone.0026069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanlangenakker N, Vanden Berghe T, Bogaert P, Laukens B, Zobel K, Deshayes K, et al. cIAP1 and TAK1 protect cells from TNF-induced necrosis by preventing RIP1/RIP3-dependent reactive oxygen species production. Cell Death Differ. 2011;18:656–665. doi: 10.1038/cdd.2010.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dondelinger Y, Aguileta MA, Goossens V, Dubuisson C, Grootjans S, Dejardin E, et al. RIPK3 contributes to TNFR1-mediated RIPK1 kinase-dependent apoptosis in conditions of cIAP1/2 depletion or TAK1 kinase inhibition. Cell Death Differ. 2013;20:1381–1392. doi: 10.1038/cdd.2013.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon CP, Weinlich R, Rodriguez DA, Cripps JG, Quarato G, Gurung P, et al. RIPK1 blocks early postnatal lethality mediated by caspase-8 and RIPK3. Cell. 2014;157:1189–1202. doi: 10.1016/j.cell.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickard JA, O'Donnell JA, Evans JM, Lalaoui N, Poh AR, Rogers T, et al. RIPK1 regulates RIPK3-MLKL-driven systemic inflammation and emergency hematopoiesis. Cell. 2014;157:1175–1188. doi: 10.1016/j.cell.2014.04.019. [DOI] [PubMed] [Google Scholar]
- Omori E, Matsumoto K, Sanjo H, Sato S, Akira S, Smart RC, et al. TAK1 is a master regulator of epidermal homeostasis involving skin inflammation and apoptosis. J Biol Chem. 2006;281:19610–19617. doi: 10.1074/jbc.M603384200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inokuchi S, Aoyama T, Miura K, Osterreicher CH, Kodama Y, Miyai K, et al. Disruption of TAK1 in hepatocytes causes hepatic injury, inflammation, fibrosis, and carcinogenesis. Proc Natl Acad Sci USA. 2010;107:844–849. doi: 10.1073/pnas.0909781107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takaesu G, Inagaki M, Takubo K, Mishina Y, Hess PR, Dean GA, et al. TAK1 (MAP3K7) signaling regulates hematopoietic stem cells through TNF-dependent and -independent mechanisms. PLoS One. 2012;7:e51073. doi: 10.1371/journal.pone.0051073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y, Li H, Zhang J, Volk A, Zhang S, Wei W, et al. TNF-α/Fas-RIP-1-induced cell death signaling separates murine hematopoietic stem cells/progenitors into 2 distinct populations. Blood. 2011;118:6057–6067. doi: 10.1182/blood-2011-06-359448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang M, Wei X, Guo Y, Breslin P, Zhang S, Zhang S, et al. TAK1 is required for the survival of hematopoietic cells and hepatocytes in mice. J Exp Med. 2008;205:1611–1619. doi: 10.1084/jem.20080297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajibade AA, Wang Q, Cui J, Zou J, Xia X, Wang M, et al. TAK1 negatively regulates NF-κB and p38 MAP kinase activation in Gr-1+CD11b+ neutrophils. Immunity. 2012;36:43–54. doi: 10.1016/j.immuni.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vucur M, Reisinger F, Gautheron J, Janssen J, Roderburg C, Cardenas DV, et al. RIP3 inhibits inflammatory hepatocarcinogenesis but promotes cholestasis by controlling caspase-8- and JNK-dependent compensatory cell proliferation. Cell Rep. 2013;4:776–790. doi: 10.1016/j.celrep.2013.07.035. [DOI] [PubMed] [Google Scholar]
- Lamothe B, Lai Y, Hur L, Orozco NM, Wang J, Campos AD, et al. Deletion of TAK1 in the myeloid lineage results in the spontaneous development of myelomonocytic leukemia in mice. PLoS One. 2012;7:e51228. doi: 10.1371/journal.pone.0051228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duprez L, Takahashi N, Van Hauwermeiren F, Vandendriessche B, Goossens V, Vanden Berghe T, et al. RIP kinase-dependent necrosis drives lethal systemic inflammatory response syndrome. Immunity. 2011;35:908–918. doi: 10.1016/j.immuni.2011.09.020. [DOI] [PubMed] [Google Scholar]
- Degterev A, Huang Z, Boyce M, Li Y, Jagtap P, Mizushima N, et al. Chemical inhibitor of nonapoptotic cell death with therapeutic potential for ischemic brain injury. Nat Chem Biol. 2005;1:112–119. doi: 10.1038/nchembio711. [DOI] [PubMed] [Google Scholar]
- Kovalenko A, Kim JC, Kang TB, Rajput A, Bogdanov K, Dittrich-Breiholz O, et al. Caspase-8 deficiency in epidermal keratinocytes triggers an inflammatory skin disease. J Exp Med. 2009;206:2161–2177. doi: 10.1084/jem.20090616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunther C, Martini E, Wittkopf N, Amann K, Weigmann B, Neumann H, et al. Caspase-8 regulates TNF-α-induced epithelial necroptosis and terminal ileitis. Nature. 2011;477:335–339. doi: 10.1038/nature10400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnet MC, Preukschat D, Welz PS, van Loo G, Ermolaeva MA, Bloch W, et al. The adaptor protein FADD protects epidermal keratinocytes from necroptosis in vivo and prevents skin inflammation. Immunity. 2011;35:572–582. doi: 10.1016/j.immuni.2011.08.014. [DOI] [PubMed] [Google Scholar]
- Welz PS, Wullaert A, Vlantis K, Kondylis V, Fernandez-Majada V, Ermolaeva M, et al. FADD prevents RIP3-mediated epithelial cell necrosis and chronic intestinal inflammation. Nature. 2011;477:330–334. doi: 10.1038/nature10273. [DOI] [PubMed] [Google Scholar]
- Kaiser WJ, Upton JW, Long AB, Livingston-Rosanoff D, Daley-Bauer LP, Hakem R, et al. RIP3 mediates the embryonic lethality of caspase-8-deficient mice. Nature. 2011;471:368–372. doi: 10.1038/nature09857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton K, Dugger DL, Wickliffe KE, Kapoor N, de Almagro MC, Vucic D, et al. Activity of protein kinase RIPK3 determines whether cells die by necroptosis or apoptosis. Science. 2014;343:1357–1360. doi: 10.1126/science.1249361. [DOI] [PubMed] [Google Scholar]
- Dillon CP, Oberst A, Weinlich R, Janke LJ, Kang TB, Ben-Moshe T, et al. Survival function of the FADD-CASPASE-8-cFLIP(L) complex. Cell Rep. 2012;1:401–407. doi: 10.1016/j.celrep.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green DR, Oberst A, Dillon CP, Weinlich R, Salvesen GS. RIPK-dependent necrosis and its regulation by caspases: a mystery in five acts. Mol Cell. 2011;44:9–16. doi: 10.1016/j.molcel.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y, Devin A, Rodriguez Y, Liu ZG. Cleavage of the death domain kinase RIP by caspase-8 prompts TNF-induced apoptosis. Genes Dev. 1999;13:2514–2526. doi: 10.1101/gad.13.19.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S, Yang Y, Mei Y, Ma L, Zhu DE, Hoti N, et al. Cleavage of RIP3 inactivates its caspase-independent apoptosis pathway by removal of kinase domain. Cell Signal. 2007;19:2056–2067. doi: 10.1016/j.cellsig.2007.05.016. [DOI] [PubMed] [Google Scholar]
- Ninomiya-Tsuji J, Kajino T, Ono K, Ohtomo T, Matsumoto M, Shiina M, et al. A resorcylic acid lactone, 5Z-7-oxozeaenol, prevents inflammation by inhibiting the catalytic activity of TAK1 MAPK kinase kinase. J Biol Chem. 2003;278:18485–18490. doi: 10.1074/jbc.M207453200. [DOI] [PubMed] [Google Scholar]
- Singh A, Sweeney MF, Yu M, Burger A, Greninger P, Benes C, et al. TAK1 inhibition promotes apoptosis in KRAS-dependent colon cancers. Cell. 2012;148:639–650. doi: 10.1016/j.cell.2011.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omori E, Matsumoto K, Zhu S, Smart RC, Ninomiya-Tsuji J. Ablation of TAK1 upregulates reactive oxygen species and selectively kills tumor cells. Cancer Res. 2010;70:8417–8425. doi: 10.1158/0008-5472.CAN-10-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton K, Sun X, Dixit VM. Kinase RIP3 is dispensable for normal NF-κBs, signaling by the B-cell and T-cell receptors, tumor necrosis factor receptor 1, and Toll-like receptors 2 and 4. Mol Cell Biol. 2004;24:1464–1469. doi: 10.1128/MCB.24.4.1464-1469.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M, Fuentes ME, Yamaguchi K, Durnin MH, Dalrymple SA, Hardy KL, et al. Embryonic lethality, liver degeneration, and impaired NF-κB activation in IKK-β-deficient mice. Immunity. 1999;10:421–429. doi: 10.1016/s1074-7613(00)80042-4. [DOI] [PubMed] [Google Scholar]
- Li ZW, Chu W, Hu Y, Delhase M, Deerinck T, Ellisman M, et al. The IKKβ subunit of IκB kinase (IKK) is essential for nuclear factor κB activation and prevention of apoptosis. J Exp Med. 1999;189:1839–1845. doi: 10.1084/jem.189.11.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Van Antwerp D, Mercurio F, Lee KF, Verma IM. Severe liver degeneration in mice lacking the IκB kinase 2 gene. Science. 1999;284:321–325. doi: 10.1126/science.284.5412.321. [DOI] [PubMed] [Google Scholar]
- Pasparakis M, Courtois G, Hafner M, Schmidt-Supprian M, Nenci A, Toksoy A, et al. TNF-mediated inflammatory skin disease in mice with epidermis-specific deletion of IKK2. Nature. 2002;417:861–866. doi: 10.1038/nature00820. [DOI] [PubMed] [Google Scholar]
- Egan LJ, Eckmann L, Greten FR, Chae S, Li ZW, Myhre GM, et al. IκB-kinaseβ-dependent NF-κB activation provides radioprotection to the intestinal epithelium. Proc Natl Acad Sci USA. 2004;101:2452–2457. doi: 10.1073/pnas.0306734101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda S, Chang L, Li ZW, Luo JL, Leffert H, Karin M. IKKβ is required for prevention of apoptosis mediated by cell-bound but not by circulating TNFα. Immunity. 2003;19:725–737. doi: 10.1016/s1074-7613(03)00301-7. [DOI] [PubMed] [Google Scholar]
- Senftleben U, Li ZW, Baud V, Karin M. IKKβ is essential for protecting T cells from TNFα-induced apoptosis. Immunity. 2001;14:217–230. doi: 10.1016/s1074-7613(01)00104-2. [DOI] [PubMed] [Google Scholar]
- Park JM, Greten FR, Wong A, Westrick RJ, Arthur JS, Otsu K, et al. Signaling pathways and genes that inhibit pathogen-induced macrophage apoptosis – CREB and NF-κB as key regulators. Immunity. 2005;23:319–329. doi: 10.1016/j.immuni.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Schmidt-Supprian M, Bloch W, Courtois G, Addicks K, Israel A, Rajewsky K, et al. NEMO/IKK γ-deficient mice model incontinentia pigmenti. Mol Cell. 2000;5:981–992. doi: 10.1016/s1097-2765(00)80263-4. [DOI] [PubMed] [Google Scholar]
- Makris C, Godfrey VL, Krahn-Senftleben G, Takahashi T, Roberts JL, Schwarz T, et al. Female mice heterozygous for IKK γ/NEMO deficiencies develop a dermatopathy similar to the human X-linked disorder incontinentia pigmenti. Mol Cell. 2000;5:969–979. doi: 10.1016/s1097-2765(00)80262-2. [DOI] [PubMed] [Google Scholar]
- Nenci A, Huth M, Funteh A, Schmidt-Supprian M, Bloch W, Metzger D, et al. Skin lesion development in a mouse model of incontinentia pigmenti is triggered by NEMO deficiency in epidermal keratinocytes and requires TNF signaling. Hum Mol Genet. 2006;15:531–542. doi: 10.1093/hmg/ddi470. [DOI] [PubMed] [Google Scholar]
- Gareus R, Kotsaki E, Xanthoulea S, van der Made I, Gijbels MJ, Kardakaris R, et al. Endothelial cell-specific NF-κB inhibition protects mice from atherosclerosis. Cell Metab. 2008;8:372–383. doi: 10.1016/j.cmet.2008.08.016. [DOI] [PubMed] [Google Scholar]
- Luedde T, Beraza N, Kotsikoris V, van Loo G, Nenci A, De Vos R, et al. Deletion of NEMO/IKKγ in liver parenchymal cells causes steatohepatitis and hepatocellular carcinoma. Cancer Cell. 2007;11:119–132. doi: 10.1016/j.ccr.2006.12.016. [DOI] [PubMed] [Google Scholar]
- Jadrich JL, O'Connor MB, Coucouvanis E. The TGFβ activated kinase TAK1 regulates vascular development in vivo. Development. 2006;133:1529–1541. doi: 10.1242/dev.02333. [DOI] [PubMed] [Google Scholar]
- Inagaki M, Komatsu Y, Scott G, Yamada G, Ray M, Ninomiya-Tsuji J, et al. Generation of a conditional mutant allele for Tab1 in mouse. Genesis. 2008;46:431–439. doi: 10.1002/dvg.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komatsu Y, Shibuya H, Takeda N, Ninomiya-Tsuji J, Yasui T, Miyado K, et al. Targeted disruption of the Tab1 gene causes embryonic lethality and defects in cardiovascular and lung morphogenesis. Mech Dev. 2002;119:239–249. doi: 10.1016/s0925-4773(02)00391-x. [DOI] [PubMed] [Google Scholar]
- Sanjo H, Takeda K, Tsujimura T, Ninomiya-Tsuji J, Matsumoto K, Akira S. TAB2 is essential for prevention of apoptosis in fetal liver but not for interleukin-1 signaling. Mol Cell Biol. 2003;23:1231–1238. doi: 10.1128/MCB.23.4.1231-1238.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ori D, Kato H, Sanjo H, Tartey S, Mino T, Akira S, et al. Essential roles of K63-linked polyubiquitin-binding proteins TAB2 and TAB3 in B cell activation via MAPKs. J Immunol. 2013;190:4037–4045. doi: 10.4049/jimmunol.1300173. [DOI] [PubMed] [Google Scholar]
- Varfolomeev EE, Schuchmann M, Luria V, Chiannilkulchai N, Beckmann JS, Mett IL, et al. Targeted disruption of the mouse caspase 8 gene ablates cell death induction by the TNF receptors, Fas/Apo1, and DR3 and is lethal prenatally. Immunity. 1998;9:267–276. doi: 10.1016/s1074-7613(00)80609-3. [DOI] [PubMed] [Google Scholar]
- Kang TB, Ben-Moshe T, Varfolomeev EE, Pewzner-Jung Y, Yogev N, Jurewicz A, et al. Caspase-8 serves both apoptotic and nonapoptotic roles. J Immunol. 2004;173:2976–2984. doi: 10.4049/jimmunol.173.5.2976. [DOI] [PubMed] [Google Scholar]
- Zhang J, Cado D, Chen A, Kabra NH, Winoto A. Fas-mediated apoptosis and activation-induced T-cell proliferation are defective in mice lacking FADD/Mort1. Nature. 1998;392:296–300. doi: 10.1038/32681. [DOI] [PubMed] [Google Scholar]
- Yeh WC, de la Pompa JL, McCurrach ME, Shu HB, Elia AJ, Shahinian A, et al. FADD: essential for embryo development and signaling from some, but not all, inducers of apoptosis. Science. 1998;279:1954–1958. doi: 10.1126/science.279.5358.1954. [DOI] [PubMed] [Google Scholar]
- Yeh WC, Itie A, Elia AJ, Ng M, Shu HB, Wakeham A, et al. Requirement for Casper (c-FLIP) in regulation of death receptor-induced apoptosis and embryonic development. Immunity. 2000;12:633–642. doi: 10.1016/s1074-7613(00)80214-9. [DOI] [PubMed] [Google Scholar]
- Panayotova-Dimitrova D, Feoktistova M, Ploesser M, Kellert B, Hupe M, Horn S, et al. cFLIP regulates skin homeostasis and protects against TNF-induced keratinocyte apoptosis. Cell Rep. 2013;5:397–408. doi: 10.1016/j.celrep.2013.09.035. [DOI] [PubMed] [Google Scholar]
- Wittkopf N, Gunther C, Martini E, He G, Amann K, He YW, et al. Cellular FLICE-like inhibitory protein secures intestinal epithelial cell survival and immune homeostasis by regulating caspase-8. Gastroenterology. 2013;145:1369–1379. doi: 10.1053/j.gastro.2013.08.059. [DOI] [PubMed] [Google Scholar]
- Schattenberg JM, Zimmermann T, Worns M, Sprinzl MF, Kreft A, Kohl T, et al. Ablation of c-FLIP in hepatocytes enhances death-receptor mediated apoptosis and toxic liver injury in vivo. J Hepatol. 2011;55:1272–1280. doi: 10.1016/j.jhep.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Huang QQ, Perlman H, Huang Z, Birkett R, Kan L, Agrawal H, et al. FLIP: a novel regulator of macrophage differentiation and granulocyte homeostasis. Blood. 2010;116:4968–4977. doi: 10.1182/blood-2009-11-252841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelliher MA, Grimm S, Ishida Y, Kuo F, Stanger BZ, Leder P. The death domain kinase RIP mediates the TNF-induced NF-κB signal. Immunity. 1998;8:297–303. doi: 10.1016/s1074-7613(00)80535-x. [DOI] [PubMed] [Google Scholar]