Abstract
Objective
We assessed the change in attitudes, knowledge, and perspectives of medical students towards chiropractic after a 1-hour educational intervention.
Methods
A mixed-methods approach was used with a 52-item cross-sectional paper survey and 1 focus group of third-year medical students. The views of these medical students towards chiropractic were assessed previously in their second-year of medical school. ANOVA and the Wilcoxon rank-sum test were used to assess between-group differences between the medical students' views before and after the educational intervention. The constant comparative method for analyzing qualitative data was used to identify emergent themes from the focus group transcript.
Results
Of 112 third-year medical students, 58 completed the survey (51.7% response rate). The focus group consisted of 6 medical students. Self-reported understanding of chiropractic and number of attitude-positive responses were significantly higher in the group after the educational session. The average number of correct responses assessing knowledge on chiropractic also was significantly higher. Focus group themes were that medical students wanted exposure to chiropractic in clinical settings, had negative attitudes towards chiropractic formed from hidden curriculum, had concerns regarding evidence and safety of chiropractic, and thought that timing of the session on chiropractic was too late in the curriculum.
Conclusions
The attitudes and knowledge of medical students towards chiropractic improved immediately after a 1-hour educational intervention. Formally educating medical students on chiropractic may help minimize hidden curriculum issues regarding chiropractic, as identified by the medical students, and facilitate collaboration between medical and chiropractic providers.
Key Indexing Terms: Attitude; Chiropractic; Education; Knowledge; Students, Medical
INTRODUCTION
Chiropractic is one of the most commonly used complementary therapies in North America.1–4 There likely are reasons for its popular use. The most common conditions treated by chiropractors are musculoskeletal conditions of the back and neck (low back pain and neck pain), which represent a substantial burden of disease globally.1,2,5 Spinal manipulation and mobilization, large components of chiropractic care, have been found to provide benefit to individuals with musculoskeletal conditions, particularly low back and neck pain.6–11 Recent methodologically rigorous studies have clarified the potential for adverse events with cervical manipulation.12,13 Specifically, current evidence suggests that individuals receiving chiropractic care do not have an excess risk of vertebrobasilar artery stroke compared to those receiving primary care.12,13 Chiropractic care also has been associated with high patient satisfaction rates with the quality of care provided.14 These factors likely have contributed to the use of chiropractic among the general population in North America.
Despite its popular use, the chiropractic profession has remained at the margins of attaining cultural authority and becoming fully integrated into mainstream health care. Previous studies often have considered chiropractic as a therapy under complementary and alternative medicine (CAM).15–20 The chiropractic profession reportedly has been viewed as having poor ethics and dishonesty when compared to other health care professions.21 Organizations and authors have identified the lack of integration with mainstream health care as a major challenge for the chiropractic profession and have suggested strategies to overcome this barrier.21–23 Proposed strategies included chiropractors focusing on public health initiatives, chiropractic educational reform, interdisciplinary training, and interprofessional collaboration.21–23
One potential barrier to the integration of chiropractic into mainstream health care has been the negative perceptions of physicians towards chiropractic.24–26 This barrier may be more evident among physicians who attend to the same patient population as chiropractors, including family physicians and orthopedic surgeons. Busse et al.24 surveyed orthopedic surgeons (via fax, 49% response rate) in North America and found 44.5% of respondents had a negative impression of chiropractic. Approximately half of the respondents referred patients for chiropractic care each year, mainly due to patient request. An analysis of their written comments suggested that one of the barriers to interprofessional collaboration between orthopedic surgeons and chiropractors was variability in practice styles within the chiropractic profession.25 Our previous study (herein referred to as Phase I) surveying medical students (via paper, 50% response rate) found that respondents wanted formal education on chiropractic within their medical curriculum.26 It was suggested that greater understanding of chiropractic care was needed to facilitate future collaboration with chiropractors.26
One strategy for overcoming the barrier of negative perceptions of chiropractic among current and future physicians is providing them with education on chiropractic. This may help to facilitate interdisciplinary training and interprofessional collaboration between chiropractors and other health care providers. However, few studies have taken the important steps of evaluating the effectiveness of educational sessions on improving attitudes, knowledge, and perspectives towards chiropractic. Hopper et al.27 found that a 1-hour lecture on CAM was effective in changing attitudes of medical students towards complementary therapies. The inclusion of education on complementary therapies within formal medical curricula appears to improve attitudes towards CAM, particularly in the early years of study.28,29 Conversely, medical students with no previous experience or exposure to chiropractic tend to have more negative attitudes towards the chiropractic profession.26 However, to the best of our knowledge, it is unknown whether education on chiropractic for medical students would be effective in improving their attitudes and knowledge specifically towards chiropractic. This is important to help determine whether interprofessional education is effective in promoting future collaboration between chiropractic and other health care providers, including medical physicians.
The purpose of this study was to assess whether the attitudes, knowledge, and perspectives of medical students to chiropractic change immediately after a 1-hour educational intervention on chiropractic.
METHODS
This study (herein referred to as Phase II) used a mixed methods approach to assess the views of medical students towards chiropractic after an educational intervention. Our mixed methods approach combined quantitative data to measure the magnitude and frequency of constructs, and qualitative data to help explain why certain phenomena occur. Specifically, our Phase II approach consisted of a 52-item cross-sectional paper survey (ie, survey given in paper-and-pencil format at one time point) and one focus group of medical students. The target population was third-year medical students enrolled in a 4-year medical program at a local university. This population was selected because they had 2 years of formalized education in medical school, but no formal curriculum on chiropractic. This same cohort of students was studied previously in Phase I using a mixed-methods approach consisting of a paper survey, key informant interviews, and a focus group in their second year of medical school.26
Inclusion criteria consisted of willingness to participate and fluency in English. Exclusion criteria included failure to provide written consent. Ethics approval for this study was obtained from the research ethics boards at the Canadian Memorial Chiropractic College and the University of Toronto.
Educational Intervention
The 1-hour introductory session on chiropractic was provided during the medical students' preclinical training early in their third year of medical school. This educational session was a part of the formal medical curriculum. The lecture was delivered by a chiropractor who had obtained postgraduate training and a fellowship in chiropractic sciences. The chiropractor also was a professor at an educational institution and worked in an academic family health team within a hospital setting. The educational session covered chiropractic training in Canada, scope of practice, common treatment modalities, and current evidence on the effectiveness and safety of spinal manipulation. The session was presented using lecture format (presentation slides), followed by a discussion between the lecturer and the class during a question-and-answer period.
Survey Instrument
The 52-item survey is available from the authors upon request and sample items from the survey are included in Figure 1. The survey was developed by the research team using previously described methodology.26 These methods involved a number of steps in creating, piloting, and administering questionnaires that had been recommended for survey development.30,31 Briefly, the survey was developed by the research team through a literature review to discern thematic areas around the views of medical students toward complementary therapies. The survey was reviewed by an experienced researcher in qualitative methods who consulted with the research team. The survey then was pretested on 4 medical students who were not a part of the sample population. The pretest resulted in modifications to the order and wording of questions. This survey was administered previously to the same medical class in their second year of study (Phase I).26 In Phase I, the survey was introduced to medical students following a second-year community health lecture with the course director's permission. In their third year of the program, the paper survey was introduced after a 1-hour introductory lecture on chiropractic that was a part of the formal curriculum. Permission also was obtained before introducing the survey to the medical class after the educational session on chiropractic. To maintain participants' anonymity, surveys were returned voluntarily via a drop box at the classroom exit.
Figure 1.
Sample questions from the survey that assessed attitudes, knowledge, and perspectives of medical students towards chiropractic.
Determined by research team consensus, the questionnaire included: one question-item assessing sex of respondents, one question-item assessing self-reported “current level of understanding of chiropractic,” one question-item assessing whether respondents had previous experience or exposure to chiropractic (eg, consulted a chiropractor, received chiropractic treatment, visited a chiropractic institution), 14 question-items assessing “knowledge of chiropractic,” four question-items assessing “perspective towards chiropractic,” 30 question-items assessing “attitude towards chiropractic,” and one open-ended question-item for any additional comments related to their opinion of chiropractic. These questions used either a 5-point Likert scale (strongly disagree [1], disagree [2], undecided/don't know [3], agree [4], and strongly agree [5]) or a nominal scale (yes, no, unsure). For the knowledge questions, participants were asked to agree, disagree, or be undecided/don't know about various types of care (eg, acute, holistic, wellness, musculoskeletal, chronic, and preventative) and types of treatment modalities (eg, joint/spinal manipulation, soft tissue, acupuncture, therapeutic modalities, medical referral, nutritional referral, exercise prescription/education, and massage) provided by chiropractors.
Focus Group
Following the survey, the third-year medical students had the opportunity to volunteer for a 1-hour focus group targeting six to 10 individuals. The size of the focus group was based on previous research suggesting that focus groups should be composed of six to 10 individuals.32 This format can elicit ideas that participants might not have considered on their own and inspire additional thoughts.32 This format also was intended to explore additional views of the medical students through discussions that may not have been captured by the survey, explore some of the themes identified in the Phase II survey results, and explore themes identified in the Phase I study.26 Our Phase I study found that medical students viewed chiropractic as an increasingly evidence-based complementary therapy for low back pain and chronic pain; based their views on indirect sources, including a hidden curriculum (ie, unintended lessons in education through informal dialogue, messages, and interactions at school); wanted to learn about chiropractic in their formal curriculum; and felt that greater understanding of chiropractic was needed for future patient referrals.26
The focus group was conducted in a private setting on the university downtown campus. The moderator of the focus group was a medical student who was not a part of the study population. The moderator used semistructured questions to explore their views towards the chiropractic profession and possible collaboration with chiropractic. Semistructured questions were developed through a literature review and expert advice from an experienced researcher in qualitative methods. The experienced researcher consulted with the research team, then revised the questions based on trends from survey results. Written informed consent was obtained from each participant to participate and audiotape the focus group. Gift cards of $20.00 in Canadian dollars (with courtesy lunch during the focus group session) were provided to each participant in appreciation of their time. Data were transcribed verbatim into written text from the audiotape. The semistructured questions for the focus group are available by contacting the principal investigator.
Analysis
Descriptive statistics (proportions) were obtained for sex and current level of chiropractic understanding. From the 30 question-items assessing “attitude towards chiropractic,” response-totals for attitude-positive (agree/strongly agree), attitude-negative (disagree/strongly disagree), and undecided/don't know were obtained for each individual to formulate summary measures of their attitudes towards chiropractic. The ANOVA was used to assess between-group differences on the attitude-response totals over various grouping variables for Phase II, and between Phases I and II. The Wilcoxon rank-sum test was used to compare the differences between the 2 phases' self-rated understanding of chiropractic (ordinal data). Since the surveys were not uniquely coded, the data were unlinked, which did not allow us to pair individuals in the analysis. The response totals were stratified and compared over 10 different group variables. A difference in proportions test (2 × 2 χ2) was used to compare proportions of participants with varying self-rated “awareness of current scientific evidence for chiropractic” between Phases I and II. Since the standard for statistical significance (p value of .05) remained unadjusted, these results are to be interpreted with caution. R Project statistical software version 2.10.0 (The R Foundation for Statistical Computing, Institut für Statistik und Wahrscheinlichkeitstheorie, Vienna, Austria) was used to perform the analysis.
The verbatim transcript of the focus group was analyzed independently by 2 investigators using the constant comparative method (a method for analyzing qualitative data). Constant comparative method is a methodological framework used to develop a grounded theory to explain some aspect of a lived experience.33 This involved comparing and contrasting the data for significant phrases and sentences to conceptualize and categorize data.33 The 2 researchers met to harmonize individual interpretations until consensus was reached on themes, categories, and subcategories. A second pair of independent reviewers was used to analyze the transcript as a data audit for the identified themes, categories, and subcategories.
RESULTS
Survey
Of the 112 medical students attending this class in their medical curriculum, 58 (51.7% response rate) completed the survey. The sex of the respondents was 50% male and 50% female. Most medical students (67.2%) did not have a previous experience with chiropractic (eg, consulted a chiropractor, had chiropractic treatment, visited a chiropractic institution, Table 1). Of the 4 respondents (6.9%) who reported an excellent “understanding of chiropractic,” 3 respondents had previous chiropractic experience (ie, consulted a chiropractor and had received chiropractic treatment).
Table 1.
Demographics and Current Level of Understanding of Chiropractic From Phase II (n = 58 respondents)
|
No. |
% |
|
| Sex | ||
| Male | 29 | 50.0 |
| Female | 29 | 50.0 |
| Previous chiropractic experience | ||
| Yes | 21 | 35.5 |
| No | 37 | 67.2 |
| Self-reported current level of understanding of chiropractic | ||
| Excellent | 4 | 7.0 |
| Good | 16 | 28.1 |
| Satisfactory | 28 | 49.1 |
| Poor | 9 | 15.8 |
| Very poor | 0 | 0 |
Results From Phase II
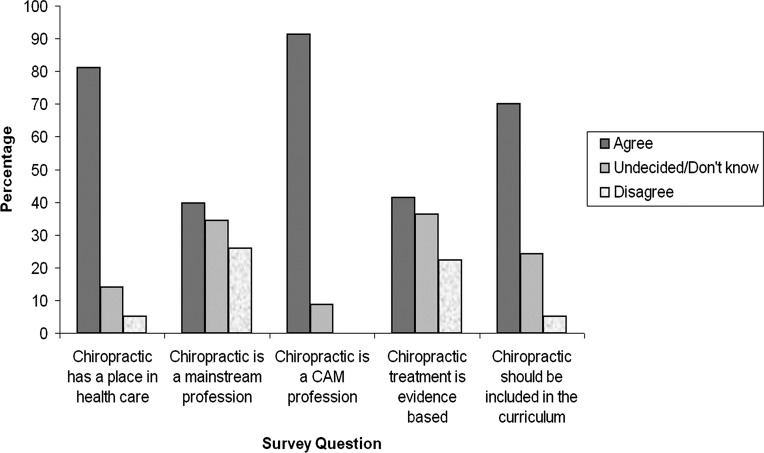
The predominant views of medical students towards chiropractic in Phase II were that chiropractic has a place in health care (68.9% agree), chiropractic is a CAM profession (60.3% agree, 31.0% strongly agree), and information about chiropractic should be included within my early years of medical curriculum (51.7% agree; Table 2, Fig. 2). Furthermore, medical students thought that chiropractors should work in interprofessional teams within a variety of settings (ie, family health teams [55.2% agree], hospitals [51.7% agree], private practice [58.6% agree], and community health centers [56.9% agree]; Table 2). More than half of medical students (55.2%) did not make an effort outside of medical school to learn about chiropractic. No clear trends were identified regarding whether medical students considered chiropractic to be evidence-based (36.2% undecided/don't know, 37.9% agree), or as a part of mainstream health care (24.1% disagree, 34.5% undecided/don't know, 37.9% agree). Most medical students (81.0%) considered interprofessional education to be important and would like to learn more about chiropractic (60.3%; Table 3).
Table 2.
Attitude and Perspective Towards Chiropractic From Phase II: Number of Responses (Strongly Disagree to Strongly Agree)
|
Question Item |
Strongly Disagree No. (%) |
Disagree No. (%) |
Undecided/Do Not Know No. (%) |
Agree No. (%) |
Strongly Agree No. (%) |
No. of Missing Responses |
| The chiropractic profession has a place in health care | 1 (1.7) | 2 (3.4) | 8 (13.8) | 40 (68.9) | 7 (12.1) | 0 |
| Chiropractic is a mainstream profession in health care | 1 (1.7) | 14 (24.1) | 20 (34.5) | 22 (37.9) | 1 (1.7) | 0 |
| Chiropractic is a complementary and alternative medicine profession | 0 (0.0) | 0 (0.0) | 5 (8.6) | 35 (60.3) | 18 (31.0) | 0 |
| Information about chiropractic should be included within the early years of my medical curriculum | 1 (1.7) | 2 (3.4) | 14 (24.1) | 30 (51.7) | 11 (18.9) | 0 |
| I make my own effort, outside of medical school, to learn about chiropractic | 9 (15.5) | 32 (55.2) | 9 (15.5) | 8 (13.8) | 0 (0.0) | 0 |
| From your experience, medical school educators are knowledgeable about chiropractic | 1 (1.7) | 11 (18.9) | 33 (56.9) | 11 (18.9) | 2 (3.4) | 0 |
| Chiropractic treatment is “evidence based,” that is use of evidence in research to guide practice | 3 (5.2) | 10 (17.2) | 21 (36.2) | 22 (37.9) | 2 (3.4) | 0 |
| Chiropractic should work in interprofessional teams within: | ||||||
| (a) Family health teams | 2 (3.4) | 0 (0.0) | 14 (24.1) | 32 (55.2) | 9 (15.5) | 1 |
| (b) Hospitals | 2 (3.4) | 5 (8.6) | 17 (29.3) | 30 (51.7) | 4 (6.9) | 0 |
| (c) Private practice | 1 (1.7) | 0 (0.0) | 14 (24.1) | 34 (58.6) | 7 (12.1) | 2 |
| (d) Community health centers | 2 (3.4) | 2 (3.4) | 12 (20.7) | 33 (56.9) | 7 (12.1) | 0 |
Figure 2.
Views of medical students towards chiropractic in Phase II. *Agree includes “strongly agree” and “agree.” Disagree includes “strongly disagree” and “disagree.” CAM = complementary and alternative medicine
Table 3.
Attitude Towards Chiropractic From Phase II: Positive, Negative and Undecided/Don't Know Responses by Grouping Variables
|
Grouping Variable |
No. (%) |
No. Positive Responses | No. Undecided/Do Not Know Responses | No. Negative Responses |
|
Mean (SD) |
Mean (SD) |
Mean (SD) |
||
| Sex | ||||
| Male | 29 (50.0) | 18.24 (7.03) | 6.66 (5.18) | 4.10 (6.24) |
| Female | 29 (50.0) | 17.76 (7.52) | 7.41 (5.70) | 3.83 (4.24) |
| Current level of understanding of chiropractic | ||||
| Good | 20 (33.9) | 19.05 (7.63) | 5.40 (4.62) | 4.55 (6.48) |
| Satisfactory | 28 (47.5) | 18.04 (7.13) | 7.25 (5.86) | 3.71 (4.68) |
| Poor | 10 (15.9) | 15.80 (6.83) | 9.70 (4.88) | 3.50 (4.65) |
| Previous chiropractic experience? | ||||
| Yes | 21 (35.5) | 19.29 (7.42) | 7.10 (6.77) | 2.62 (2.96) |
| No | 37 (62.7) | 17.27 (7.10) | 7.00 (4.58) | 4.73 (6.15) |
| Received chiropractic treatment? | ||||
| Yes | 14 (23.7) | 19.29 (8.81) | 6.79 (7.87) | 2.93 (3.36) |
| No | 44 (75.8) | 17.59 (6.70) | 7.11 (4.49) | 4.30 (5.77) |
| Is interprofessional education (IPE) important to you? | ||||
| Yes | 47 (81.0) | 19.68 (5.83) | 6.68 (5.42) | 2.64 (3.37) |
| No | 3 (5.1) | 7.00 (6.56) | 6.33 (5.03) | 15.67 (10.69) |
| Unsure | 8 (13.7) | 12.25 (8.94)a | 9.38 (5.58) | 7.38 (6.07)a |
| Are you aware of the current scientific evidence for chiropractic treatment? | ||||
| Yes | 24 (41.3) | 18.17 (7.22) | 5.58 (4.22) | 5.25 (6.94) |
| No | 21 (36.2) | 18.24 (6.62) | 8.05 (5.41) | 2.71 (3.45) |
| Unsure | 13 (22.4) | 17.31 (8.60) | 8.08 (7.02) | 3.62 (3.84) |
| Would you like to learn more about chiropractic care? | ||||
| Yes | 35 (60.3) | 20.60 (5.90) | 6.00 (5.42) | 2.40 (3.42) |
| No | 15 (25.8) | 13.20 (8.10) | 8.33 (5.26) | 7.47 (7.79) |
| Unsure | 8 (13.7) | 15.63 (5.85)b | 9.13 (5.19) | 4.25 (3.33)b |
From the 30 question-items assessing “attitude towards chiropractic,” response-totals for attitude-positive (agree/strongly agree), attitude-negative (disagree/strongly disagree), and undecided/don't know were obtained for each individual to formulate summary measures of their attitudes towards chiropractic. ANOVA was used to assess between-group differences on the attitude-response totals over various grouping variables (ie, comparing the number of attitude positive, undecided/don't know, and negative responses between groups stratified by responses to the given question).
Mean number of responses with p < .001 between groups in ANOVA.
Mean number of responses with p < .01 between groups in ANOVA.
Table 3 shows the effect of different grouping variables on totals for attitude-positive, attitude-negative, and undecided/don't know responses. Unlike the results from Phase I,26 there was no difference in attitude among individuals with varying levels of self-reported “level of understanding on chiropractic.” Moreover, individuals who had previous experience with chiropractic, regardless of the type of experience, showed no difference in the number of attitude-positive, -negative, or undecided responses. Individuals reporting that they were aware of the current evidence for chiropractic treatment did not differ from their counterparts in terms of attitude.
Comparing Phase I and Phase II Results
Overall, attitudes differed between the 2 phases. We saw a significant increase in number of attitude-positive responses (p < .0001), a decrease in attitude-negative (p = .03), and decrease in undecided responses in the Phase II participants (p = .001; Table 4). For self-perceived level of understanding of chiropractic, individuals in Phase II had ranked themselves significantly higher as a group (Wilcoxon rank-sum, p = .0002). Table 4 shows that a greater percentage of respondents rated themselves as having at least a “Good” understanding of chiropractic in Phase II compared to Phase I (ie, 35.1% vs 21.5%; Table 5).
Table 4.
Attitude Towards Chiropractic: Positive, Negative and Undecided/Don't Know Responses by Phase
|
Phase |
No. |
No. Positive Responses Mean (SD) |
No. Undecided/Do Not Know Responses Mean (SD) |
No. Negative Responses Mean (SD) |
| 1 | 112 | 12.39 (7.52) | 10.40 (6.75) | 6.21 (6.87) |
| 2 | 58 | 18.00 (7.22)a | 7.03 (5.42)b | 3.97 (5.29)c |
Phase I refers to study by Wong et al.26 and Phase II refers to this current study.
Mean number of responses with p < .001 between groups in ANOVA.
Mean number of responses with p < .01 between groups in ANOVA.
Mean number of responses with p < .05 between groups in ANOVA.
Table 5.
Responses to Self-reported Current Level of Understanding of Chiropractic by Phase
|
Phase |
Excellent % (No.) |
Good % (No.) |
Satisfactory % (No.) |
Poor % (No.) |
Very Poor % (No.) |
Total % (No.) |
| 1 | 2.7 (3) | 18.8 (21) | 31.3 (35) | 42.0 (47) | 5.4 (6) | 100.0 (112) |
| 2 | 7.0 (4) | 28.1 (16) | 49.1 (28) | 15.8 (0) | 0.0 (0) | 100.0 (57) |
Phase I refers to study by Wong et al.26 and Phase II refers to this current study.
The chiropractic modalities with the highest percentage of individuals lacking knowledge in Phase II were acupuncture (86.2%), nutritional information (77.6%), preventative care (65.5%), therapeutic modalities (62.1%), and acute care (48.3%). The average correct number of responses by individuals in Phase II (8.55 [3.21] or 61%) was significantly higher than the average number of correct responses in phase 1 (6.76 [3.52] or 48%; p = .001).
Regarding current scientific evidence for chiropractic, 41.4% of respondents reported that “they were aware of it,” which is a significant increase from the 9.9% who responded that “they were aware of it” in phase 1 (χ2, p < .0001). In addition, the number of individuals who responded that they were unaware decreased from 73.2% to 36.2% (χ2, p < .0001) and the percentage of unsure increased from 16.9% to 22.4% (χ2, p = .38).
Focus Group
The 1-hour focus group session was conducted 10 days after the survey was administered and involved six third-year medical students. The participants' use of specific dialogue in the focus group provided a context for assessing their attitudes, knowledge, and perspectives toward chiropractic. The following themes were identified:
Learning About Chiropractic in a Clinical Setting
The students would like to gain insight on the perspective of patients receiving chiropractic care from a chiropractor and their patients. Specifically, the students felt that it would be helpful to shadow practitioners and see the benefits of chiropractic to patients in a clinical setting. This would help them feel more comfortable referring to chiropractors.
“It would be really beneficial if we could actually interact with a provider … see what they do, like their scope of practice plus the patients they see. Maybe hearing from the patients themselves … can vocalize “oh, this has been really helpful … like my back feels great” … for us to see that this is a good practitioner, their patients are happy. This is someone I'd be comfortable referring to.”
Possible Negative Hidden Curriculum Around Chiropractic
The students reported a lack of exposure to chiropractic in the formal curriculum. However, the students did perceive more negative attitudes towards the profession among some faculty members through a hidden curriculum (eg, informal references to chiropractic during lectures or small group sessions).
“No [formal discussion about chiropractic in our medical education], not that I can remember at all over the last 3 years other than this 1 to 2 hour lecture … There is a lot of stigma associated with it and I know specifically in 1 session that we had a spinal surgeon … who had very negative opinions about chiropractic … obviously that has an influence on us as students.”
Some Concerns About the Chiropractic Profession
The students still had questions about the safety, evidence, and credibility of the chiropractic profession. These should be addressed in additional educational sessions on chiropractic.
“Just a lack of understanding of what a chiropractor does and the safety associated with it, are barriers to me, you know, when I'm practicing or referring someone to a chiropractor.”
“Showed us journal articles … this is the kind of evidence we were looking for, and she had presented this to us about safety and about patient satisfaction. I think those are 2 big topics for me that…maybe I can take this seriously, rather than just brushing it off, you know, as a service.”
Benefits and Timing of Educational Session on Chiropractic
The students found the educational session on chiropractic to be helpful. However, they perceived that the timing of the session (ie, an introductory chiropractic lecture in third year) was too late into their formal curriculum. Previous attitudes based on informal sources that were predominantly negative still lingered. However, their attitudes did move somewhat towards the positive direction after the educational session.
“The session, in and of itself, was great and I think it really addressed a lot of the things we probably had questions about … I think it's too little too late … and going into it with negative perceptions … and getting the message that it isn't accepted, and then having this 1 great session where they tell you how great the outcomes are, how much the patients like it … the session was great, in and of itself, but we should have had that session in first year.”
DISCUSSION
Our study examined the change in attitudes, knowledge, and perspectives of medical students towards chiropractic after a 1-hour educational intervention. Survey results from the Phase II group, compared to the Phase I group, revealed these significant findings: (1) increased number of attitude positive responses, (2) improved self-perceived understanding of chiropractic, (3) average number of correct responses assessing knowledge on chiropractic increased, and (4) greater percentage of respondents reporting awareness of the scientific evidence for chiropractic. The focus group identified several themes, highlighting that medical students wanted exposure to chiropractic in clinical settings, had negative attitudes towards chiropractic formed from the hidden curriculum, wanted more information regarding the evidence and safety of chiropractic. and thought the timing of the introductory session on chiropractic (ie, in third year) was too late in the curriculum. Overall, these results suggest that the 1-hour educational session helped improve attitudes and knowledge towards chiropractic immediately following the session. However, medical students' views may be improved further with earlier education on chiropractic (including within clinical settings) that addresses the evidence, safety, and negative hidden curriculum regarding chiropractic.
Our findings suggest that an educational session is able to improve the attitudes and knowledge of medical students towards chiropractic immediately after the session. However, a number of concerns are held by medical students that should be addressed in a broader scale to facilitate greater understanding of chiropractic. First, medical students should be exposed further to the scientific literature around the effectiveness and associated risks with interventions performed by chiropractors, particularly spinal manipulation. Spinal manipulation has been found to be effective for a number of musculoskeletal complaints within the current literature.6–11 Moreover, current evidence suggests that individuals receiving chiropractic care are not at an excess risk for vertebrobasilar artery stroke compared to primary care, which is a common concern among medical professionals.12,13 Second, current medical faculty and health care providers may benefit from resources that provide evidence-based education about chiropractic. This may improve their understanding of chiropractic and chiropractic literature, while minimizing negative hidden curriculum related to chiropractic. Phase I and Phase II studies revealed a common student experience of observing negative comments about chiropractic from faculty members, suggesting a negative hidden curriculum in their formal education.26
The timing and setting of the exposure on chiropractic also appears to be important factors. Exposure to chiropractic may need to start early in the formal medical curriculum. Specifically, the medical students wanted to learn from chiropractors in practice and interact with chiropractic patients to hear about their experiences. A previous study also found that students were more receptive to learning about other professions in their earlier rather than later years of education.34 In addition, the medical students desired formal exposure to chiropractic in a clinical setting. This is supported, in part, by previous work that found medical practitioners and chiropractors working together had formed better collaborative relationships.35–37
Strengths and Limitations
There are strengths to this study. First, we used a mixed-methods approach to explore the views of medical students towards chiropractic with quantitative and qualitative data. It has been suggested that this is a more comprehensive approach to exploring attitudes.38 Second, for the quantitative data, we used a prepiloted survey instrument developed based on survey methodology and that was reviewed by an experienced researcher in qualitative methods. The survey also was returned via a drop box at the classroom exit to maintain participants' anonymity. Third, the facilitator of the focus group was a medical student not in the target population. This aimed to minimize social acceptability bias that may have been present if the facilitator had a chiropractic background. Lastly, a pair of independent reviewers conducted a data audit of the identified themes from the focus group transcript.
There also are limitations to this study. First, the surveys were not individually coded, and, therefore, individual change from Phases I and II within subjects could not be determined. The change from Phases I and II are between groups and the respondents comprising the groups may have differed between phases. However, the respondents who are most vocal about chiropractic are more likely to have responded, and this would have applied to both phases. Second, these results from a 52% response rate may have limited generalizability to medical students as a whole. Nonresponders may have different responses that were not captured in our data, though their views were likely explored in the focus group discussions. Third, the survey included a response option to certain questions as “undecided/don't know.” However, “undecided” is not the same as “don't know,” and the use of this category, therefore, is a limitation to the study. The survey questions also were all in the same direction on the Likert scale and this may have introduced an inherent response bias. Lastly, since the study involved one focus group, additional groups may have yielded different information. However, most themes were similar to those found in Phase I, so saturation likely was reached through the combination of focus groups between the 2 phases.
Future Research Directions
We currently are examining the same group of medical students' attitudes and knowledge in their fourth year of the medical program (ie, Phase III). During their fourth year, the medical students receive clinical training through clerkship and some students are placed in clinical settings with additional formal exposure to chiropractic. Specifically, some students have formal exposure to chiropractic and interaction with chiropractic learners during an interprofessional education session on low back pain. Therefore, this study has 2 objectives: to assess the long-term effectiveness of the educational session after 1 year and to compare the attitudes, knowledge, and perspectives of medical students who receive formal exposure to chiropractic in a clinical setting versus those who do not. Eisenberg et al.39,40 suggested that when healthcare providers were trained together, it was beneficial to future collaboration in practice. Studies also are needed to examine the effectiveness of more extensive education on chiropractic among future health care providers, and to assess the effectiveness of education on collaboration in clinical practice. Furthermore, it may be helpful for studies to examine the implicit attitudes of medical students towards chiropractic. Previous research by Chung et al.41 found that physical therapy students in a Canadian University master's entry program had a negative implicit bias towards chiropractic. Our Phases I and II studies found that Canadian medical students were interested in learning more about chiropractic, based on their explicit attitudes. However, they may have deep-rooted beliefs, identified as implicit attitudes, which are more negative towards chiropractic and may hinder effective collaboration. Future research in this area is recommended.
CONCLUSIONS
Our results supported the use of a 1-hour educational session to improve attitudes, knowledge, and perspectives of medical students to chiropractic immediately after the session. We also identified a number of issues that should be considered in future educational reform. First, education on chiropractic may be provided earlier in the formal medical curriculum and include exposure in clinical settings. In addition, future educational sessions should consider addressing the evidence, safety, and negative hidden curriculum towards chiropractic. This may help promote future collaboration between medical providers and chiropractors. Educating future healthcare providers on chiropractic can be considered as one of many strategies to further integrate chiropractic into mainstream healthcare.
FUNDING AND CONFLICTS OF INTEREST
This work was funded internally. The authors declare that there are no conflicts of interest to declare relevant to this work.
Footnotes
This paper was selected as a 2014 Association of Chiropractic Colleges - Research Agenda Conference Prize Winning Paper - Award funded by the National Board of Chiropractic Examiners.
REFERENCES
- 1.Coulter ID, Hurwitz EL, Adams AH, et al. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine (Phila Pa 1976) 2002;27:291–296. doi: 10.1097/00007632-200202010-00018. discussion 297–298. [DOI] [PubMed] [Google Scholar]
- 2.Hurwitz EL, Coulter ID, Adams AH, et al. Use of chiropractic services from 1985 through 1991 in the United States and Canada. Am J Public Health. 1998;88:771–776. doi: 10.2105/ajph.88.5.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karpman RR. Musculoskeletal disease in the United States: who provides the care. Clin Orthop Relat Res. 2001;385:52–56. doi: 10.1097/00003086-200104000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Shekelle PG, Markovich M, Louie R. Factors associated with choosing a chiropractor for episodes of back pain care. Med Care. 1995;33:842–850. doi: 10.1097/00005650-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyles R, Toy P, Mellon J, Jr, et al. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. J Man Manip Ther. 2011;19:135–142. doi: 10.1179/2042618611Y.0000000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goertz CM, Pohlman KA, Vining RD, et al. Patient-centered outcomes of high-velocity, low-amplitude spinal manipulation for low back pain: a systematic review. J Electromyogr Kinesiol. 2012;22:670–691. doi: 10.1016/j.jelekin.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Huisman PA, Speksnijder CM, de Wijer A. The effect of thoracic spine manipulation on pain and disability in patients with non-specific neck pain: a systematic review. Disabil Rehabil. 2013;35:1677–1685. doi: 10.3109/09638288.2012.750689. [DOI] [PubMed] [Google Scholar]
- 9.Miller J, Gross A, D'Sylva J, et al. Manual therapy and exercise for neck pain: A systematic review. Man Ther. 2010 doi: 10.1016/j.math.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Rodine RJ, Vernon H. Cervical radiculopathy: a systematic review on treatment by spinal manipulation and measurement with the Neck Disability Index. J Can Chiropr Assoc. 2012;56:18–28. [PMC free article] [PubMed] [Google Scholar]
- 11.Vincent K, Maigne JY, Fischhoff C, et al. Systematic review of manual therapies for nonspecific neck pain. Joint Bone Spine. 2012;80:508–515. doi: 10.1016/j.jbspin.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Cassidy JD, Boyle E, Côté P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine (Phila Pa 1976) 2008;33:S176–S183. doi: 10.1097/BRS.0b013e3181644600. [DOI] [PubMed] [Google Scholar]
- 13.Boyle E, Cote P, Grier AR, et al. Examining vertebrobasilar artery stroke in two Canadian provinces. Spine (Phila Pa 1976) 2008;33:S170–S175. doi: 10.1097/BRS.0b013e31816454e0. [DOI] [PubMed] [Google Scholar]
- 14.Sherman KJ, Cherkin DC, Connelly MT, et al. Complementary and alternative medical therapies for chronic low back pain: what treatments are patients willing to try? BMC Complement Altern Med. 2004;4:9. doi: 10.1186/1472-6882-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 16.Kanodia AK, Legedza AT, Davis RB, et al. Perceived benefit of Complementary and Alternative Medicine (CAM) for back pain: a national survey. J Am Board Fam Med. 2010;23:354–362. doi: 10.3122/jabfm.2010.03.080252. [DOI] [PubMed] [Google Scholar]
- 17.Kelner M, Wellman B, Welsh S, et al. How far can complementary and alternative medicine go? The case of chiropractic and homeopathy. Soc Sci Med. 2006;63:2617–2627. doi: 10.1016/j.socscimed.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Leach MJ. Profile of the complementary and alternative medicine workforce across Australia, New Zealand, Canada, United States and United Kingdom. Complement Ther Med. 2013;21:364–378. doi: 10.1016/j.ctim.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Santaguida PL, Gross A, Busse J, et al. Complementary and alternative medicine in back pain usation report. Evid Rep Technol Assess (Full Rep) 2009;177:1–221. [PMC free article] [PubMed] [Google Scholar]
- 20.Toupin April K, Gaboury I. A survey of Canadian regulated complementary and alternative medicine schools about research, evidence-based health care and interprofessional training, as well as continuing education. BMC Complement Altern Med. 2013;13:374. doi: 10.1186/1472-6882-13-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy DR, Schneider MJ, Seaman DR, et al. How can chiropractic become a respected mainstream profession? The example of podiatry. Chiropr Osteopat. 2008;16:10. doi: 10.1186/1746-1340-16-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meeker WC, Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136:216–227. doi: 10.7326/0003-4819-136-3-200202050-00010. [DOI] [PubMed] [Google Scholar]
- 23.Lehman JJ, Suozzi PJ. Founding integrative medicine centers of excellence: one strategy for chiropractic medicine to build higher cultural authority. J Chiropr Educ. 2008;22:29–33. doi: 10.7899/1042-5055-22.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Busse JW, Jacobs C, Ngo T, et al. Attitudes toward chiropractic: a survey of North American orthopedic surgeons. Spine (Phila Pa 1976) 2009;34:2818–2825. doi: 10.1097/BRS.0b013e3181c1512f. [DOI] [PubMed] [Google Scholar]
- 25.Busse JW, Jim J, Jacobs C, et al. Attitudes towards chiropractic: an analysis of written comments from a survey of north American orthopaedic surgeons. Chiropr Man Therap. 2011;19:25. doi: 10.1186/2045-709X-19-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong JJ, Di Loreto L, Kara A, et al. Assessing the attitudes, knowledge and perspectives of medical students to chiropractic. J Can Chiropr Assoc. 2013;57:18–31. [PMC free article] [PubMed] [Google Scholar]
- 27.Hopper I, Cohen M. Complementary therapies and the medical profession: a study of medical students' attitudes. Altern Ther Health Med. 1998;4:68–73. [PubMed] [Google Scholar]
- 28.Nedrow AR, Istvan J, Haas M, et al. Implications for education in complementary and alternative medicine: a survey of entry attitudes in students at five health professional schools. J Altern Complement Med. 2007;13:381–386. doi: 10.1089/acm.2007.6273. [DOI] [PubMed] [Google Scholar]
- 29.Anderson ES, Thorpe LN. Early interprofessional interactions: does student age matter? J Interprof Care. 2008;22:263–282. doi: 10.1080/13561820802054689. [DOI] [PubMed] [Google Scholar]
- 30.Boynton PM. Administering, analysing, and reporting your questionnaire. BMJ. 2004;328:1372–1375. doi: 10.1136/bmj.328.7452.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. 2004;328:1312–1315. doi: 10.1136/bmj.328.7451.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Slaughter P, Pinfold P, Flintoff V, et al. Focus Groups in Health Services Research at the Institute for Clinical and Evaluative Sciences. Toronto: The Institute for Clinical and Evaluative Sciences; 1999. [Google Scholar]
- 33.Itoi EH, Itoigawa Y, Omi R, et al. Is protecting the healing ligament beneficial after immobilization in external rotation for an initial shoulder dislocation? Am J Sports Med. 2013;41:1126–1132. doi: 10.1177/0363546513480620. [DOI] [PubMed] [Google Scholar]
- 34.Riccard CP, Skelton M. Comparative analysis of 1st, 2nd, and 4th year MD students' attitudes toward complementary alternative medicine (CAM) BMC Res Notes. 2008;1:84. doi: 10.1186/1756-0500-1-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boon HS, Mior SA, Barnsley J, et al. The difference between integration and collaboration in patient care: results from key informant interviews working in multiprofessional health care teams. J Manipulative Physiol Ther. 2009;32:715–722. doi: 10.1016/j.jmpt.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Mior S, Barnsley J, Boon H, et al. Designing a framework for the delivery of collaborative musculoskeletal care involving chiropractors and physicians in community-based primary care. J Interprof Care. 2010;24:678–689. doi: 10.3109/13561821003608757. [DOI] [PubMed] [Google Scholar]
- 37.Mior S, Gamble B, Barnsley J, et al. Changes in primary care physician's management of low back pain in a model of interprofessional collaborative care: an uncontrolled before-after study. Chiropr Man Therap. 2013;21:6. doi: 10.1186/2045-709X-21-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hadi MA, Alldred DP, Closs SJ, et al. A mixed-methods evaluation of a nurse-pharmacist-managed pain clinic: design, rationale and limitations. Can Pharm J (Ott) 2013;146:197–201. doi: 10.1177/1715163513490400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eisenberg DM, Kessler RC, Foster C, et al. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 40.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 41.Chung C, Manga J, McGregor M, et al. Interprofessional collaboration and turf wars: how prevalent are hidden attitudes? J Chiropr Educ. 2012;26:32–39. [PMC free article] [PubMed] [Google Scholar]