Abstract
Introduction: Internal fixation with hook plate has been used to treat acromioclavicular joint dislocation. This study aims to evaluate the effect of its use on shoulder function, to further analyze the contributing factors, and provide a basis for selection and design of improved internal fixation treatment of the acromioclavicular joint dislocation in the future. Methods: A retrospective analysis was performed on patients treated with a hook plate for acromioclavicular joint dislocation in our hospital from January 2010 to February 2013. There were 33 cases in total, including 25 males and 8 females, with mean age of 48.27 ± 8.7 years. There were 29 cases of Rockwood type III acromioclavicular dislocation, 4 cases of type V. The Constant-Murley shoulder function scoring system was used to evaluate the shoulder function recovery status after surgery. Anteroposterior shoulder X-ray was used to assess the position of the hook plate, status of acromioclavicular joint reduction and the occurrence of postoperative complications. Results: According to the Constant-Murley shoulder function scoring system, the average scores were 78 ± 6 points 8 to 12 months after the surgery and before the removal of the hook plate, the average scores were 89 ± 5 minutes two months after the removal of hook plate. Postoperative X-ray imaging showed osteolysis in 10 cases (30.3%), osteoarthritis in six cases (18.1%), osteolysis associated with osteoarthritis in four cases(12.1%), and steel hook broken in one case (3%). Conclusion: The use of hook plate on open reduction and internal fixation of the acromioclavicular joint dislocation had little adverse effect on shoulder function and is an effective method for the treatment of acromioclavicular joint dislocation. Osteoarthritis and osteolysis are the two common complications after hook plate use, which are associated with the impairment of shoulder function. Shoulder function will be improved after removal of the hook plate.
Keywords: Acromioclavicular joint, dislocation, hook plate, function, osteolysis, osteoarthritis
Introduction
Acromioclavicular joint dislocation is very common following upper extremity trauma. For acromioclavicular joint dislocations that are Rookwood type III and above, surgical treatment is currently recommended. The most commonly used surgical approach is open reduction and hook plate fixation. Because the hook plate matches the anatomy of the clavicle and shoulder and allows for the micro-adjustment of the acromioclavicular joint, it has been widely used clinically. But complications after the use of clavicular hook plate for acromioclavicular joint dislocation and distal clavicle fracture treatment, such as postoperative shoulder pain and limited shoulder motion, are also often reported. Thus, it is important to study the effects of the hook plate fixation on shoulder function, which will provide the basis for the selection and design of improved fixation of acromioclavicular joint dislocation treatments. Unfortunately, few such studies have been performed. We analyzed retrospectively 33 patients who have been treated with hook plate for acromioclavicular joint dislocation in our hospital from January 2010 to February 2013, to assess the impact of hook plate on shoulder function.
We found that the use of hook plate on open reduction and internal fixation of the acromioclavicular joint dislocation had little adverse effect on shoulder function and is an effective method for the treatment of acromioclavicular joint dislocation. Osteoarthritis and osteolysis are the two common complications after hook plate use, which are associated with the impairment of shoulder function. Shoulder function will be improved after removal of the hook plate.
Methods
General information
There were total 33 cases of pure acromioclavicular joint dislocation without associated injuries, including 25 males, and 8 females; mean age was 48.27 ± 8.7 years (age range 19-67 years old). There were 29 cases of Rockwood type III acromioclavicular dislocation, 4 cases of type V. 18 cases had the injuries on the left side, 15 cases on the right side. All patients had open reduction and hook plate fixation within 2 to 6 days after injury, and had the hook plate removed within 8 to 12 months after the surgery.
Surgery
All patients were treated with combined neck and brachial plexus anesthesia. After the commencement of anesthesia, patients were on supine position with the injured shoulder raised. A curved incision was cut along the distal clavicle to the acromion, the distal clavicle, the acromioclavicular joint and the acromion were exposed. If there was articular cartilage debris or loose cartilage disk in the acromioclavicular joint, it was removed first. Then the dislocated acromioclavicular joint was reduce and temporarily fixed, the hook end of a pre-bent steel plate was inserted into the rear bottom of the shoulder, and the proximal end of the plate was screwed into the clavicle. X-ray was used to confirm the reduce of the dislocation, then silk suture was used to repair torn ligaments and acromioclavicular joint capsule, the incision was closed after rinse. Postoperative neck wrist strap was used to protect the shoulder and rehabilitation exercises were planned individually in accordance with the situation of each patient.
Postoperative shoulder function assessment
The postoperative shoulder function was assessed using the Constant-Murley shoulder function score criteria [1]: pain (maximum score 15 points); activity level (maximum 20 points); range of motion (maximum 40 points); strength (maximum 25 points), total score of 100 points. The better the function, the higher the rating. Shoulder anteroposterior X-ray was taken six months after the surgery or before the removal of the hook plate to study the subacromial osteolysis, osteoarthritis of the acromioclavicular joint and the reduce condition of the dislocation.
Statistical analysis
All data are expressed as mean ± standard deviation. Statistical analysis was performed using SPSS software with group t test and Fisher’s exact test. P < 0.05 was considered statistically significant.
Results
All 33 cases were assessed for shoulder function using the Constant-Murley shoulder function score criteria before and two months after the removal of the hook plate. Shoulder anteroposterior X-ray was taken in all patients before and after the internal fixation surgery, before and after the removal of the hook plate. No postoperative wound infection occurred in any of the 33 patients. X-ray images showed that the dislocated acromioclavicular joints were completely reduce in all cases; no dislocation occurred after the surgery or after removal of the hook plate. Subacromial osteolysis was found in 10 patients (9 males, 1 female) (Figure 1); acromioclavicular joint osteoarthritis was found in 6 cases (5 males and 1 female); and co-occurrence of subacromial osteolysis and acromioclavicular joint osteoarthritis was found in 4 cases (all male) (Figure 2). The hook plate was broken in one case, but no acromioclavicular joint dislocation was found in this case (Figure 3). Co-occurrence of acromioclavicular osteoarthritis and coracoclavicular ligament ossification was found in 1 case (Figure 4). The occurrence rate of hook plate related complications was significantly higher in men than women (P = 0.035, Table 1).
Figure 1.
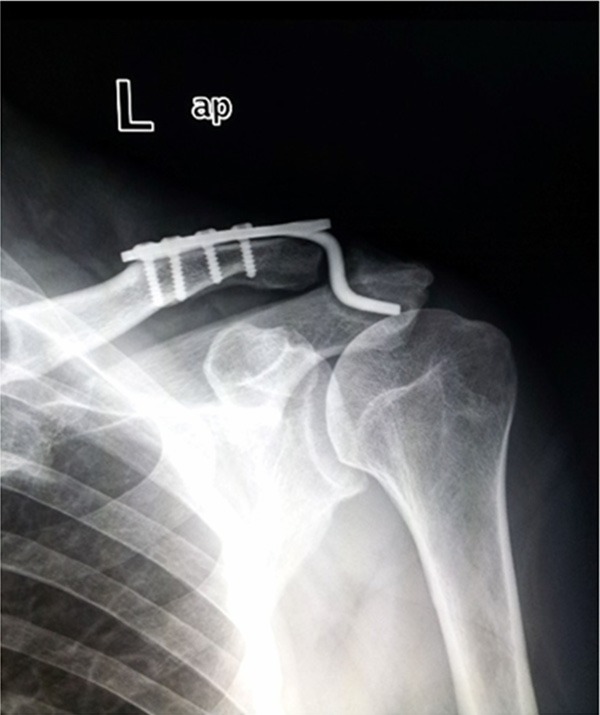
Subacromial osteolysis shown on shoulder X ray. It was found in 10 patients (9 males, 1 female).
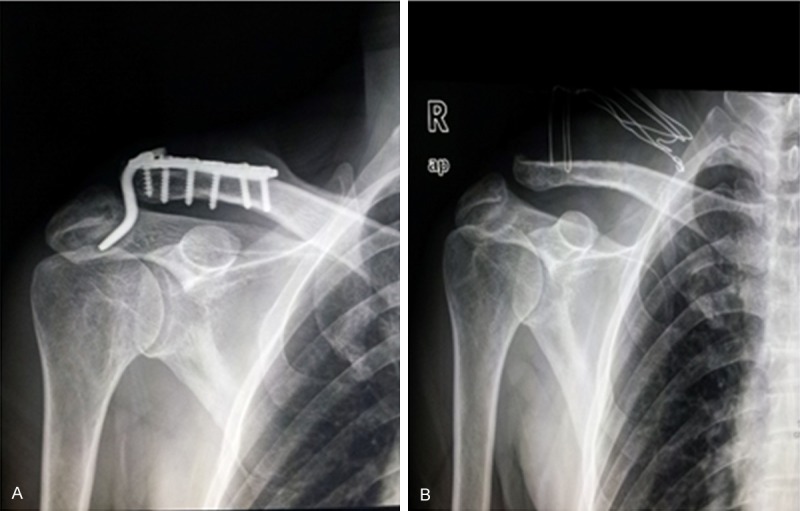
Figure 2.

Co-occurrence of subacromial osteolysis and acromioclavicular joint osteoarthritis shown on shoulder X ray. They were found in 4 cases (all male). A. Shoulder X ray before removal of hook plate; B. Shoulder X ray after removal of hook plate
Figure 3.
Broken hook plate shown on shoulder X ray. The hook plate was broken in one case, but no acromioclavicular joint dislocation was found.
Figure 4.
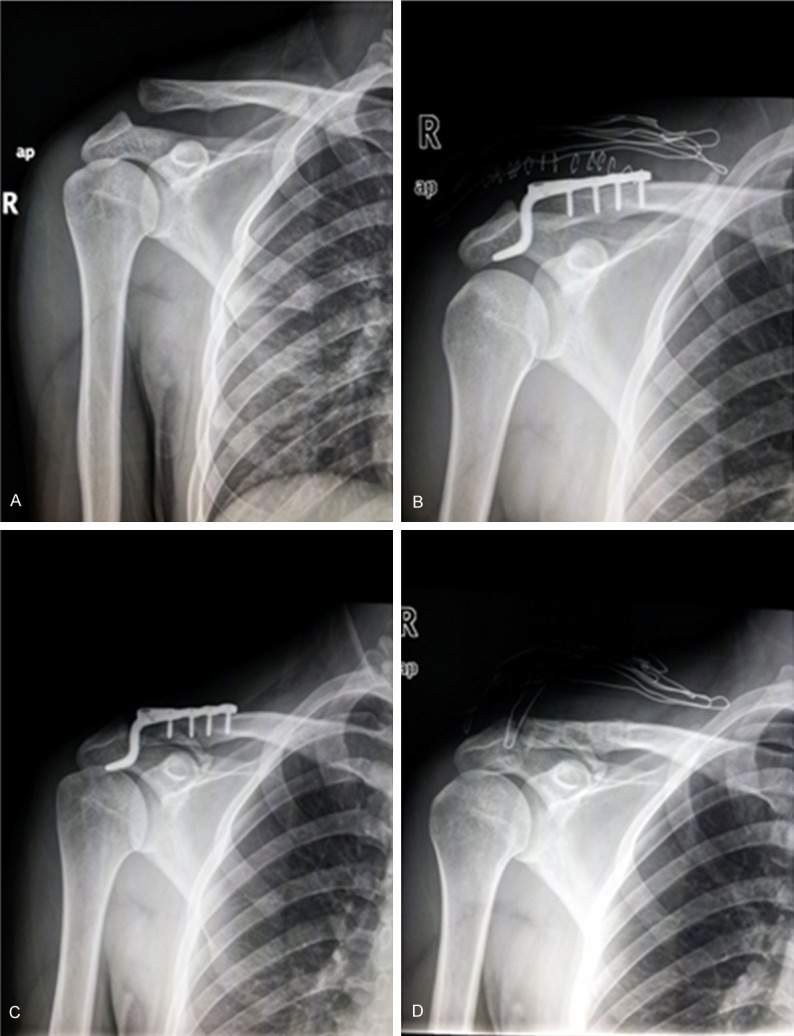
Co-occurrence of acromioclavicular osteoarthritis and coracoclavicular ligament ossification shown on shoulder X ray. They were found in 1 case. A. Shoulder X ray before surgery; B. Right after surgery; C. 11 months after surgery and right before the removal of the hook plate; D. After removal of the hook plate.
Table 1.
Postoperative complications of open reduction and internal fixation with hook plate to treat acromioclavicular joint dislocation
| Postoperative complications | Cases (%) | Total (%) | P value | |
|---|---|---|---|---|
|
| ||||
| Male (25) | Female (8) | 33 | Fisher’s exact test | |
| Osteolysis | 9 (36.0%) | 1 (12.5%) | 10 (30.3%) | 0.382 |
| Osteoarthritis | 5 *(20.0%) | 1 (12.5%) | 6 (18.1%) | 0.409 |
| Osteolysis + Osteoarthritis | 4 (16.0%) | 0 (0%) | 4 (12.1%) | 0.55 |
| Joint re-dislocation | 0 (0%) | 0 (0%) | 0 (0%) | |
| Incision infection | 0 (0%) | 0 (0%) | 0 (0%) | |
| Total | 18 (72.0%) | 2 (25.0%) | 20 (60.0%) | 0.035 |
Coracoclavicular ligament ossification occurred in one case.
.
The Constant-Murley shoulder function scores were 78 ± 6 points at 8 to 12 months after the surgery and right before the removal of the hook plate; the score was 89 ± 5 points at 2 months after removal of the hook plate. There is significant difference between the Constant-Murley shoulder function scores before and after the removal of the hook plate (P = 0.005). And the scores of patients without complications shown by X-ray were higher than those who have complications of osteolysis and osteoarthritis complications (Table 2).
Table 2.
Average Constant score of acromioclavicular joint after surgery
| X ray changes of the joint (Taken before removal of plate) | Constant score of the joint (point) | |||
|---|---|---|---|---|
|
| ||||
| Before removal | After removal | t | p value | |
| Abnormal X ray (20 cases) | 73 ± 6 | 85 ± 5 | ||
| Osteolysis (10 cases) | 79 ± 5 | 92 ± 4 | 3.39 | 0.008 |
| Osteoarthritis (6 cases) | 74 ± 6 | 83 ± 4 | 2.523 | 0.053 |
| Osteolysis + Osteoarthritis (4 cases)* | 58 ± 7 | 69 ± 7 | 3.236 | 0.048 |
| Normal X ray (13 cases) | 86 ± 4 | 95 ± 3 | 2.179 | 0.05 |
| Total (33 cases) | 78 ± 6 | 89 ± 5 | 3.015 | 0.005 |
The hook plate was broken in one case, but no acromioclavicular joint dislocation.
Discussion
Acromioclavicular joint dislocation is a common clinical traumatic disease. The mechanism and treatment options of this disease have been widely understood. For acromioclavicular joint dislocation rated Rockwood type III and above, more aggressive surgical approach was usually used to fix the dislocated acromioclavicular joint [2,3]. According to a recent survey among shoulder/sport surgeons in major hospitals in Germany, More than 90% treat Rockwood I or II injuries conservatively and Rockwood III to VI injuries surgically [4]. Choices of surgical fixation approaches include Kirschner wire or hook plate fixation of the acromioclavicular joint, inter-coracoclavicular screw fixation, Endobutton loop plate fixation of clavicle and coracoid process [5]. Although Kirschner wire fixation of the acromioclavicular joint, or screw fixation of the clavicle and coracoid process could achieve the goal of reduction of the dislocation initially, since the acromioclavicular joint is amphiarthrotic, fixation failure often occurred due to loosing and fracture of the internal fixation caused by stress concentration, therefore, they were rarely used clinically. Endobutton loop fixation of clavicle and coracoid process avoids the stiffened fixation of the acromioclavicular joint, allowing movement of the shoulder, but the surgery is more complex, and there is a lack of large sample study and long-term follow-up study to assess the efficacy. Since the clavicular hook plate works by forming a leverage through the proximal end of the plate fixed to the distal clavicle and the hook penetrating the acromion, so it not only reduces the dislocation of the acromioclavicular joint by adding pressure joint, but also maintains the characteristics of amphiarthrosis of the acromioclavicular joint, the measurement results of this technique is the closest to the normal biomechanics of the acromioclavicular joint [6], and thus is the most commonly used treatment plan for acromioclavicular joint dislocation. According to the German survey mentioned above, favored techniques have completely changed since 2001 when the majority of physicians preferred AC joint transfixation or coracoclavicular cerclages, both techniques that are rarely used today. The hook plate appears to have become “standard therapy which is the favored surgical technique in 44% of the surveyed surgeons [4].
For hook plate treatment of acromioclavicular joint dislocation, time is also critical. von Heideken et al showed that the median Constant Score was 91 for the acute surgery group and 85 for the delayed surgery group. The acutely treated patients had better outcomes according to the median shoulder pain and disability index, shortened version of the disabilities of the arm, shoulder, and hand. The acutely treated patients had less pain in their injured shoulder during rest and during movement [7].
But there have been reports showing that complications could occur postoperatively [8,9]. Lin et al demonstrated by musculoskeletal sonography that clavicular hook plate could cause subacromial shoulder impingement and rotator cuff lesion. Their data also suggest an association between hardware-induced impingement and poorer functional scores. They advocated the removal of the implant as soon as bony union and/or ligamentous healing is achieved [10].
In this study, our retrospective analysis found that all dislocations of the acromioclavicular joint were successfully reduced when treated with hook plate for Rockwood III and V dislocations, which was confirmed by postoperative X-ray films. There was no recurrence of joint dislocation during the follow-up study, but hook plate-related complications were not uncommon. Subacromial osteolysis and acromioclavicular joint osteoarthritis are the most common complications, where the average incidence rate of osteolysis was 30.3%, and the average incidence rate of acromioclavicular osteoarthritis was 18.1%. There were varying degrees of shoulder dysfunction before removal of the hook plate, and the shoulder function was significantly improved after removal of the plate, indicating a close correlation of hook plate implant with shoulder dysfunction. The idea of acromioclavicular hook plate design is to reduce and fix the acromioclavicular joint by inserting the end of the steel hook into the subacromial space, in theory, this will not damage the nearby structures such as the rotator cuff and shoulder; and since the hook plate does not directly go through the acromioclavicular joint, thus it will not damage the surface of the acromioclavicular joint either. However, biopsy studies performed by ElMaraghy et al [11] showed that when using the hook plate to fix acromioclavicular joint, the hook could easily pierce the subacromial bursa and contact with rotator cuff structures such as supraspinatus muscle, and in some specimens, the tip end of the hook had reached the subacromial surface. They also found that there were significant gender differences in acromion morphology: the width and thickness of men’s shoulders were larger than those of women. Therefore, if we can further optimize the morphology of the end of the acromioclavicular hook plate and choose a hook plate of different size according to individual needs, it will likely reduce the incidence of shoulder pain and other complications. We also found that in some patients the shoulder pain was not severe, but shoulder motion was poor, especially it was hard for the upper limbs to be raised more than 90 degrees. Studies suggest that if arm elevation is less than 90 degrees, the relative rotation of the clavicle against the shoulder is small; but if arm elevation is more than 90 degrees, the rotation of the clavicle becomes significant [12]. Especially when the hook of the plate is positioned under subacromial surface and in close contact it, the rotation of the clavicle is limited, which may cause difficulties in the elevation of the shoulder after surgery. Removal of the hook plate as early as possible maybe the only way to solve complications such as subacromial osteolysis. But the optimal time to remove the hook plate remains controversial, and in some literatures it was taken about a year after internal fixation. In our study, we removed the plate within 8-12 months after the surgery, no further dislocation was found. Alexander DF et al [13] removed the plate one year after the surgery and studied the acromioclavicular joint 18 months after the injury occurred (6 months after removal of the plate) using shoulder MRI, they found the rate of acromioclavicular ligament healing was 88%. There has been no follow-up report on early and midterm acromioclavicular ligament healing condition after the surgery.
In summary, open reduction and internal fixation with hook plate is an effect treatment for acromioclavicular joint dislocation, but hook plate had a significant impact on shoulder function, for example it could cause complications such as osteolysis, acromioclavicular osteoarthritis. But the shoulder function was significantly improved after the hook plate was removed. And how to further optimize the design of hook plate and what is the optimal time to remove the hook plate in order to decrease the incidence of complications are the focus for future studies.
Acknowledgements
The investigation reported in the manuscript was performed with informed consent and following all the guidelines for experimental investigation with human subjects required by Affiliated Hospital of Nanjing University of Traditional Chinese Medicine, Jiangyin Traditional Chinese Medical Hospital and The Second Affiliated Hospital of Suzhou University
Disclosure of conflict of interest
All authors stated that there is no conflict of interest.
References
- 1.Constant CR, Murley AH. A clinical method of functiona assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 2.Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J shoulder Elbow Surg. 2008;17:220–5. doi: 10.1016/j.jse.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Phillips AM, Smart C, Groom AF. Acromioclavicular dislocation. Conservative or surgical therapy. Clin Orthop Relat Res. 1998;353:10–7. [PubMed] [Google Scholar]
- 4.Balke M, Schneider MM, Akoto R, Bäthis H, Bouillon B, Banerjee M. Acute acromioclavicular joint injuries: Changes in diagnosis and therapy over the last 10 years. Unfallchirurg. 2014 doi: 10.1007/s00113-013-2547-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Zhu L, Yang HJ, Zhao WJ, Yang WM, Zhou H. Case-control study on Endobutton plate or clavicular hook plate for the repair of acromioclavicular joint dislocations. Zhongguo Gu Shang. 2012;25:120–123. [PubMed] [Google Scholar]
- 6.McConnell AJ, Yoo DJ, Zdero R, Schemitsch EH, McKee MD. Methods of operative fixation of the acromioclavicular joint: a biomechanical comparison. J Orthop Trauma. 2007;21:248–253. doi: 10.1097/BOT.0b013e31803eb14e. [DOI] [PubMed] [Google Scholar]
- 7.von Heideken J, Boström Windhamre H, Une-Larsson V, Ekelund A. Acute surgical treatment of acromioclavicular dislocation type V with a hook plate: superiority to late reconstruction. J Shoulder Elbow Surg. 2013;22:9–17. doi: 10.1016/j.jse.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Ejam S, Lind T, Falkenberg B. Surgical treatment of acute and chronic acromioclavicular dislocation Tossy type III and v using the Hook plate. Acta Orthop Belg. 2008;74:441–5. [PubMed] [Google Scholar]
- 9.Kienast B, Thietje R, Queitsch C, Gille J, Schulz AP, Meiners J. Mid-term results after operative treatment of Rockwood grade III-V acromioclavicular joint dislocations with an ac-hook-plate. Eur J Med Res. 2011;16:52–56. doi: 10.1186/2047-783X-16-2-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin HY, Wong PK, Ho WP, Chuang TY, Liao YS, Wong CC. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion--dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. doi: 10.1186/1749-799X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ElMaraghy AW, Devereaux MW, Ravichandiran K, Agur AM. Subacromial morphometric assessment of the clavicle hook plate. Injury. 2010;41:613–619. doi: 10.1016/j.injury.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 12.Fung M, Kato S, Barrance PJ, Elias JJ, McFarland EG, Nobuhara K, Chao EY. Scapular and clavicular kinematics during humeral elevation: a study with cadavers. J Shoulder Elbow Surg. 2001;10:278–85. doi: 10.1067/mse.2001.114496. [DOI] [PubMed] [Google Scholar]
- 13.Alexander DF, Carmine Z, Olivo C, Renzo P, Stefano F. The use of hook plate in type III and V acromio-clavicular Rockwood dislocations: Clinical and radiological midterm results and MRI evaluation in 42 patients. Injury. 2012;43:147–152. doi: 10.1016/j.injury.2011.04.002. [DOI] [PubMed] [Google Scholar]


