Abstract
Objective
Eating behavior traits measured in early life predict eating behavior and weight trajectories later in development, and may be associated with certain parental feeding behaviors. Our goal was to investigate the relationship between a range of feeding behaviors, and preschoolers’ appetitive traits.
Method
Four hundred thirty-nine parents of UK 3–5 year olds completed scales measuring authoritarian vs. authoritative forms of limiting (Restriction vs. Monitoring) and promoting (Pressuring vs. Prompting) intake, as well as Emotional and Instrumental Feeding. Parents also completed scales measuring child Food responsiveness and Satiety responsiveness. Child BMI z-scores were calculated based on measured heights and weights.
Results
Parental Restriction was significantly associated with greater child Food responsiveness (p <.001), but parental Monitoring was not. Parental Pressuring was significantly associated with greater child Satiety responsiveness (p <.001), while parental Prompting was not. Parental Instrumental and Emotional feeding were both associated with greater child Food responsiveness (p <.001). All relationships were independent of child BMI z-score.
Discussion
Prospective data are needed to determine whether the parent–child feeding relationships identified here promote, or protect against, the development of eating pathology in children. However, our results suggest that cross-sectional associations depend on the style (e.g., authoritarian vs. authoritative), as well as the type of feeding behavior measured.
Keywords: restrictive feeding, pressure to eat, overfeeding, maternal feeding, nonnutritive feeding, parental control over feeding, intake regulation
Introduction
Eating behavior traits measured in early life are known to predict later eating behavior and weight trajectories.1 Investigating the predictors of such traits, or characteristics, may therefore help identify individuals at high risk of developing unhealthy eating patterns and/or body weight, and illuminate causes. Developmental models of obesity and eating disorders are generally concerned with different aspects of children’s eating behavior, i.e. appetite and intake in the case of obesity,2 weight control attempts and dysregulated eating in the case of eating disorders.3 However, both obesity and eating disorders demonstrate familial transmission, 4,5 highlighting a role for parents.
Evidence suggests that environmental as well as genetic pathways underlie familial transmission of eating pathology,6,7 but little is known about the nature of the environmental mechanisms at play. Studies have reported associations between disordered eating in offspring and maternal psychopathology, 8,9 as well as mothers’ weight-related concerns and weight control behaviors10 and critical evaluations of offspring weight and appearance. 11 Mothers with eating disorders have also been found to exert more control over their child’s eating.12 Less work in the eating disorders arena, though, has directly examined how parent feeding behaviors might impact children’s eating behaviors.
A relatively small body of research suggests that parental attempts to control the type and/or amount of food consumed, or to use food in nonnutritive contexts, could be important influences on eating disordered behavior in children.13–16 Parents’ attempts to limit the type and amount of food consumed are most frequently measured using the Restriction scale from the Child Feeding Questionnaire (CFQ17). Higher CFQ-Restriction scores have been associated with greater child adiposity and appetite,1,2 and also disinhibited eating in girls.18 Scores on the CFQ-Monitoring scale, though, which measures a milder, potentially more flexible type of intake limitation, have been associated with healthier BMIs, and more healthful eating behavior.1,2,19
Parents’ attempts to promote intake of healthy mealtime foods are typically measured with the CFQ-Pressure to eat scale. This assesses a demanding and inflexible form of intake promotion, and higher scores have been associated with lower adiposity and appetite1,2 and also greater dietary restraint and emotional disinhibition in girls.18 In contrast, authoritative attempts to encourage eating (i.e., making high demands on children but in a responsive manner,20) may sometimes be associated with healthier eating styles and healthier body weights.21
Non-nutritive feeding behaviors include instrumental feeding, which may be defined as using food in a “means-end” contingency, and emotional feeding, i.e. using food to influence the child’s emotions. Studies using the Instrumental and Emotional feeding scales of the Parental Feeding Style Questionnaire (PFSQ22) have reported associations with greater child snacking,23 as well as greater tendency to overeat, and greater emotional eating.24
Associations between parent feeding behavior and child eating behavior seem to differ substantially depending on the feeding measures used, and in particular depending on whether authoritative or authoritarian styles of feeding control are assessed, but no studies have explicitly contrasted authoritarian and authoritative versions of the same broad feeding strategy. We therefore assessed a range of different parent feeding behaviors, along with children’s appetitive traits, in a large UK community sample of preschoolers. We predicted that: (1) authoritarian (but not authoritative) limiting would be associated with higher food responsiveness (an index of external eating and over-valuation of food); (2) authoritarian (but not authoritative) promoting would be associated with higher satiety responsiveness (an indicator of low appetite); (iii) instrumental and emotional feeding would be associated with higher food responsiveness.
Method
Participants and Procedures
Twelve London primary schools were chosen to represent a range of socioeconomic deprivation, indexed by student eligibility for Free School Meals, a government benefit available to lower-income families. Parents/primary caregivers (hereafter referred to as parents) were sent letters about the study and given the option of excluding their child. Questionnaires were distributed and reminders sent to those who did not respond within two weeks. Children were weighed and measured at school on the day of questionnaire distribution.
Measures
Demographic and Anthropometric Characteristics
Demographic questions were included in the parent questionnaire and children’s ages calculated by subtracting their date of birth from the date of questionnaire completion. Trained researchers weighed and measured children using TANITA digital scales (Tanita Corp., Tokyo, Japan) and a Leicester height measure (Seca, Birmingham, UK). BMI z-scores and centiles were calculated with reference to 1990 UK growth reference curves, and IOTF weight categories were generated.25
Child Eating Behavior
Two scales from the Child Eating Behaviour Questionnaire26 were included: Child [C] Satiety responsiveness (Example item:My child gets full easily) and Food responsiveness (e.g., Given the choice, my child would eat most of the time). Parents responded to each question using a 1–5 Likert scale with the end-points Never and Always. The CEBQ has been well-validated, with sub-scales demonstrating good internal consistency and test-retest reliability,26 validity against behavioral measures27 and high stability/continuity over time.28
Parental Feeding Behavior
Scales from two published feeding questionnaires were administered. Parental [P] Restriction, Monitoring, and Pressure to eat (henceforth referred to as Pressuring) scales were taken from the CFQ.17 Parental Prompting to eat (henceforth referred to as Prompting), Emotional feeding, and Instrumental feeding scales were drawn from the PFSQ.22 Of the scales measuring parental limiting of intake, Restriction was considered relatively authoritarian, and Monitoring authoritative. Of those measuring parental promotion of intake, Pressuring was considered authoritarian, and Prompting (which contains items such as Do you praise your child if he/she eats what you give him/her?) authoritative. Response options were 0–4 Likert scales with the endpoints Disagree and Agree, or Never and Always.
Statistical Analysis
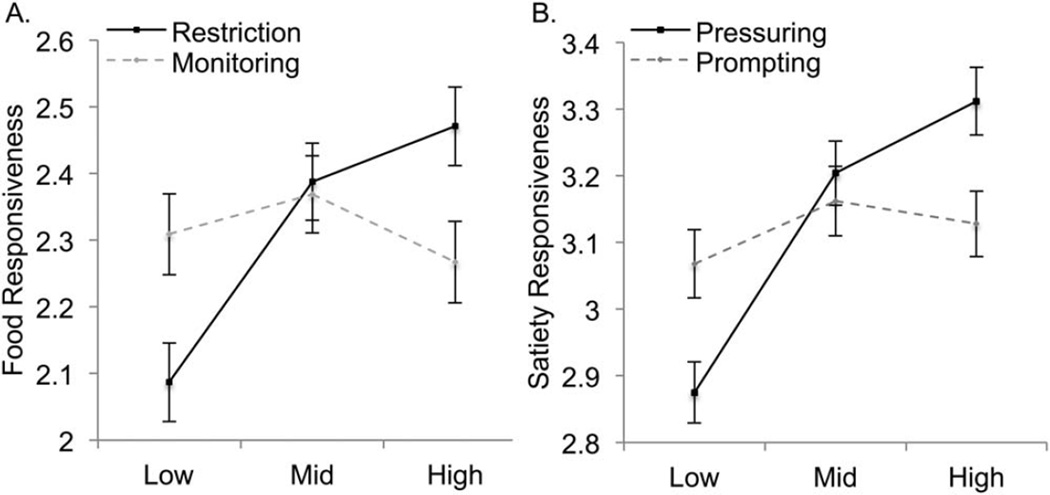
Analyses were conducted using SPSS v. 22. Item means were created for all parent feeding and child eating behavior scales. Paired t-tests were used to compare mean levels of authoritarian vs. authoritative forms of parental limiting (P-Restriction vs. P-Monitoring) and promoting (P-Pressuring vs. P-Prompting) of intake. Multiple regression models were used to test linear relationships between (i) authoritarian and authoritative measures of parental limiting of intake, and C-Food responsiveness, (ii) authoritarian and authoritative measures of parental promoting of intake, and C-Satiety responsiveness, and (iii) the two different measures of parental non-nutritive feeding (P-Instrumental feeding, P-Emotional feeding), and C-Food responsiveness, all controlling for child BMI z score. To compare effects between authoritarian and authoritarian measures, we examined 95% confidence intervals (CIs) for standardized regression coefficients, and to investigate the relative effects of authoritarian and authoritative strategies, we repeated regression analyses (i) and (ii) including both authoritarian and authoritative measures in the same model (i.e., P-Restriction and P-Monitoring for (i), P-Pressuring and P-Prompting for (ii)). To illustrate the main parental feeding–child appetite relationships we created approximately equal tertiles for parent feeding scores, and ran individual univariate ANOVAs, controlling for child BMI z score (Fig. 1).
Figure 1.
A: Parental limiting of intake (Restriction vs. Monitoring tertiles) and child Food responsiveness, adjusting for child BMI z score. B: Parental promoting of intake (Pressuring vs. Prompting tertiles) and child Satiety responsiveness, adjusting for child BMI z score.
Results
Response Rates
Questionnaires were distributed to 1,088 parents in total. After two reminders, 541 parents returned the questionnaire, giving an absolute response rate of 50% (541/1,088). However, since only 64% of the total sample (n = 698) had children with English as a first language the effective questionnaire response rate is likely nearer 78% (541/698). Children’s height and weight was assessed for 827 (76%) of the 1,088 children present on the day of data collection, and children’s height and weight was available for 439 (81%) of the 541 questionnaire respondents. The final sample size is therefore 439.
Sample Characteristics
Full sample characteristics are described elsewhere. 29 To summarize, 55% of children were male and mean age was 4.4 SD 0.6 (range 3–6 years). Mean BMI was 16.8±1.9 (range 13–31 kg/m2), and mean z score relative to 1990 UK reference data was 0.67±1.12, with 20% of children overweight and 9% obese according to IOTF criteria. Ninety-four percent of parents reported that they were the mother of the child, and parents were more ethnically diverse (65% white British) and better educated (26% with a degree or higher qualification) than the general UK population.30 Mean CEBQ scores were 2.32±0.73 (range 1–5) for C-Food responsiveness, and 3.11±0.63 (range 1.11–4.89) for C-Satiety responsiveness.
Parental Feeding and Child Eating Behavior
Parental Limiting of Intake and Child Eating Behavior
Mean P-Monitoring scores (3.01±0.83) were higher than P-Restriction scores (2.45±0.88) (t[431] = −10.7), and P-Monitoring and P-Restriction were positively correlated (r = .21, p <.001). Individual multiple regressions controlling for child BMI z-score demonstrated that P-Restriction showed a positive association with C-Food responsiveness while P-Monitoring did not (Table 1, Fig. 1), and 95% CIs for standardized regression coefficients did not overlap, suggesting a significant difference in the degree of association for each feeding behavior. Results remained similar in the joint model containing both feeding behaviors, suggesting independence of associations with child eating behavior.
TABLE 1.
Multiple regression analyses showing linear relationships between parental feeding behaviors and children’s appetitive traitsa
| B | SE | β (95% CI) | t | p | n | |
|---|---|---|---|---|---|---|
| Parental limiting of intake as predictor of child Food Responsiveness | ||||||
| Restriction | 0.204 | 0.038 | 0.248 (0.173, 0.323) | 5.37 | <.001 | 432 |
| Monitoring | 0.010 | 0.042 | 0.012 (−0.071, 0.095) | 0.247 | .81 | 428 |
| Parental promoting of intake as predictor of child Satiety Responsiveness | ||||||
| Pressuring | 0.191 | 0.026 | 0.335 (0.284, 0.386) | 7.49 | <.001 | 433 |
| Prompting | 0.105 | 0.058 | 0.087 (0.027, 0.201) | 1.81 | .07 | 430 |
| Parental non-nutritive feeding as predictor of child Food Responsiveness | ||||||
| Instrumental feeding | 0.201 | 0.043 | 0.217 (0.132, 0.302) | 4.63 | <.001 | 428 |
| Emotional feeding | 0.191 | 0.044 | 0.205 (0.119, 0.291) | 4.37 | <.001 | 430 |
Table gives results from individual multiple regression analyses containing each parental feeding behavior, controlling for child BMI z-score.
Parental Promoting of Intake and Child Eating Behavior
Mean P-Prompting scores (3.05±0.60) were higher than P-Pressuring scores (2.00±1.09) (t[432] = −17.9), and scores on each scale were not correlated. Individual multiple regressions controlling for BMI z-score revealed that P-Pressuring showed a positive association with C-Satiety responsiveness while P-Prompting did not (Table 1, Fig. 1). 95% CIs for standardized regression coefficients did not overlap, and results were similar in the joint model containing both feeding behaviors.
Parental Non-nutritive Feeding and Child Eating Style
Mean P-Instrumental feeding scores were 1.19±0.79 and mean P-Emotional feeding scores were 0.86±0.78. Individual multiple regressions controlling for child BMI z-score demonstrated that both P-Instrumental feeding and P-Emotional feeding showed positive associations with C-Food responsiveness (Table 1, Fig. 1).
Discussion
In this large survey, higher parental Restriction was associated with higher child Food responsiveness, and higher Pressuring with higher Satiety responsiveness, while their authoritative equivalents were not significantly related to child appetite. Higher levels of both Emotional and Instrumental feeding were associated with higher child Food responsiveness, and all results were independent of child BMI z score. Our results are consistent with previous studies.1,2,18,23,24 However, they also highlight how associations differ crucially according to the feeding behavior, and style, assessed.
Of the scales measuring parental limiting of intake, one (CFQ-Restriction) suggests an authoritarian style of control, as well as the perception of responding to avid appetite in children (e.g. I have to be sure that my child does not eat too many high fat foods), while the other (CFQ-Monitoring, e.g. How much do you keep track of the sweets that your child eats?) suggests more subtle, authoritative methods. Possibly, authoritarian forms of restriction heighten a child’s responsiveness to less healthy, high-calorie foods. Alternatively, high child appetite may inspire rigid restrictive feeding. In contrast, Monitoring may be exercised regardless of the child’s eating styles, with no apparent negative consequences for appetite.
Of the scales measuring parental promoting of intake, CFQ-Pressure to eat describes authoritarian attempts to control feeding, as well as perceived responding to low child appetite (e.g., If I did not guide or regulate my child’s intake he would not eat enough), while the PFSQ-Prompting to eat scale taps more covert, child-responsive forms of encouragement. In our study, Pressuring could therefore have tapped into a child-responsive behavior that increased with the child’s lack of interest in food, while Prompting probed a more normative parental behavior that was unrelated to appetite.
Although causal relationships are unclear from this cross-sectional data, our CFQ-Restriction results, and to some degree our PFSQ-Instrumental and Emotional feeding findings, are broadly consistent with eating disorder theories positing that excessive parental control over feeding may teach children to ignore their internal hunger and satiety cues, leading to overeating in response to external (e.g., social or emotional) cues.13,14
Study strengths include a large sample size, diverse sample, the use of multiple, well-established, validated measures of parent feeding and child appetite, and the fact that we have demonstrated good correspondence between parent ratings of child appetite and laboratory measures of children’s eating behavior in a sub-group of this particular sample.27 Limitations include the cross-sectional design, the relatively low estimated response rate (between 50 and 78%), and the lack of population representativeness. Since our focus was appetite, we did not measure disordered eating styles (e.g., restraint, disinhibition, emotional eating) or weight control behaviors in children, which could also have shown associations with the assessed parent feeding behaviors. Further, given the reliance on parent-report, we cannot rule out the possibility that some of our results could primarily reflect parental characteristics such as the need for control.
To conclude, our results confirm the existence of style-dependent associations between parental feeding and appetitive traits/characteristics in children. They also highlight the promise of evaluating specific, well-characterized parent feeding behaviors as potentially modifiable influences on child eating pathology that could help prevent eating disorder development. However, prospective data are needed to evaluate potential long-term impacts of parent feeding behaviors on offspring eating and weight disorder outcomes.
Acknowledgments
Supported by funding from the NIH (K99DK088360, R00DK088360), MRC and CRUK.
The authors are very grateful to Jane Wardle for her contributions to the design of the study.
References
- 1.Carnell S, Kim Y, Pryor K. Fat brains, greedy genes, and parent power: A bio-behavioural risk model of child and adult obesity. Int Rev Psychiatry. 2012;24:189–199. doi: 10.3109/09540261.2012.676988. [DOI] [PubMed] [Google Scholar]
- 2.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neumark-Sztainer D, Wall M, Story M, Sherwood NE. Five-year longitudinal predictive factors for disordered eating in a population-based sample of overweight adolescents: Implications for prevention and treatment. Int J Eat Disord. 2009;42:664–672. doi: 10.1002/eat.20733. [DOI] [PubMed] [Google Scholar]
- 4.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 5.Lilenfeld LR, Kaye WH, Greeno CG, Merikangas KR, Plotnicov K, Pollice C, et al. A controlled family study of anorexia nervosa and bulimia nervosa: Psychiatric disorders in first-degree relatives and effects of proband comorbidity. Arch Gen Psychiatry. 1998;55:603–610. doi: 10.1001/archpsyc.55.7.603. [DOI] [PubMed] [Google Scholar]
- 6.Carnell S, Haworth CM, Plomin R, Wardle J. Genetic influence on appetite in children. Int J Obes (Lond) 2008;32:1468–1473. doi: 10.1038/ijo.2008.127. [DOI] [PubMed] [Google Scholar]
- 7.Klump KL, Wonderlich S, Lehoux P, Lilenfeld LR, Bulik CM. Does environment matter? A review of nonshared environment and eating disorders. Int J Eat Disord. 2002;31:118–135. doi: 10.1002/eat.10024. [DOI] [PubMed] [Google Scholar]
- 8.Garcia de Amusquibar AM, De Simone CJ. Some features of mothers of patients with eating disorders. Eat Weight Disord. 2003;8:225–230. doi: 10.1007/BF03325018. [DOI] [PubMed] [Google Scholar]
- 9.Ammaniti M, Lucarelli L, Cimino S, D’Olimpio F, Chatoor I. Maternal psychopathology and child risk factors in infantile anorexia. Int J Eat Disord. 2010;43:233–240. doi: 10.1002/eat.20688. [DOI] [PubMed] [Google Scholar]
- 10.van den Berg PA, Keery H, Eisenberg M, Neumark-Sztainer D. Maternal and adolescent report of mothers’ weight-related concerns and behaviors: Longitudinal associations with adolescent body dissatisfaction and weight control practices. J Pediatr Psychol. 2010;35:1093–1102. doi: 10.1093/jpepsy/jsq042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pike KM, Rodin J. Mothers, daughters, and disordered eating. J Abnorm Psychol. 1991;100:198–204. doi: 10.1037//0021-843x.100.2.198. [DOI] [PubMed] [Google Scholar]
- 12.Blissett J, Haycraft E. Parental eating disorder symptoms and observations of mealtime interactions with children. J Psychosom Res. 2011;70:368–371. doi: 10.1016/j.jpsychores.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Birch LL, Fisher JO, Davison KK. Learning to overeat: Maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78:215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sinton MM, Birch LL. Weight status and psychosocial factors predict the emergence of dieting in preadolescent girls. Int J Eat Disord. 2005;38:346–354. doi: 10.1002/eat.20176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park RJ, Senior R, Stein A. The offspring of mothers with eating disorders. Eur Child Adolesc Psychiatry. 2003;12(Suppl 1):I110–I119. doi: 10.1007/s00787-003-1114-8. [DOI] [PubMed] [Google Scholar]
- 16.Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? Int J Eat Disord. 2014;47:310–314. doi: 10.1002/eat.22189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 18.Carper JL, Orlet Fisher J, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35:121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- 19.Jansen PW, Roza SJ, Jaddoe VW, Mackenbach JD, Raat H, Hofman A, et al. Children’s eating behavior, feeding practices of parents and weight problems in early childhood: Results from the population-based Generation R Study. Int J Behav Nutr Phys Act. 2012;9:130. doi: 10.1186/1479-5868-9-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: Parenting styles in a child-feeding context. Appetite. 2005;44:83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Vollmer RL, Mobley AR. Parenting styles, feeding styles, and their influence on child obesogenic behaviors and body weight. A review. Appetite. 2013;71:232–241. doi: 10.1016/j.appet.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 22.Wardle J, Sanderson S, Guthrie CA, Rapoport L, Plomin R. Parental feeding style and the inter-generational transmission of obesity risk. Obes Res. 2002;10:453–462. doi: 10.1038/oby.2002.63. [DOI] [PubMed] [Google Scholar]
- 23.Sleddens EF, Kremers SP, De Vries NK, Thijs C. Relationship between parental feeding styles and eating behaviours of Dutch children aged 6–7. Appetite. 2010;54:30–36. doi: 10.1016/j.appet.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Rodgers RF, Paxton SJ, Massey R, Campbell KJ, Wertheim EH, Skouteris H, et al. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: A prospective study. Int J Behav Nutr Phys Act. 2013;10:24. doi: 10.1186/1479-5868-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole TJ, Bellizzi MC, Flegal K, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children’s Eating Behaviour Questionnaire. J Child Psychol Psychiatry. 2001;42:963–970. doi: 10.1111/1469-7610.00792. [DOI] [PubMed] [Google Scholar]
- 27.Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: Validation of the child eating behaviour questionnaire. Appetite. 2007;48:104–113. doi: 10.1016/j.appet.2006.07.075. [DOI] [PubMed] [Google Scholar]
- 28.Ashcroft J, Semmler C, Carnell S, van Jaarsveld CH, Wardle J. Continuity and stability of eating behaviour traits in children. Eur J Clin Nutr. 2008;62:985–990. doi: 10.1038/sj.ejcn.1602855. [DOI] [PubMed] [Google Scholar]
- 29.Carnell S, Wardle J. Associations between multiple measures of parental feeding and children’s adiposity in United Kingdom preschoolers. Obesity (Silver Spring) 2007;15:137–144. doi: 10.1038/oby.2007.513. [DOI] [PubMed] [Google Scholar]
- 30.Sproston K, Primatesta P, editors. Health Survey for England 2002. Vol. 3. London: methodology and documentation. The Stationery Office; 2003. [Google Scholar]