Abstract
Objectives
The current standards for classifying eating disorders were primarily informed by adult, clinical study populations, while it is unknown whether an empirically based classification system can be supported across preadolescence through young adulthood. Using latent class analyses, we sought to empirically classify disordered eating in females from preadolescence to young adulthood, and assess the association between classes and adverse outcomes.
Methods
Latent class models were fit using observations from the 9,039 girls participating in the Growing Up Today Study, an on-going cohort following participants annually or biennially since 1996 when they were ages 9–14 years. Associations between classes and drug use, binge drinking, and depressive symptoms were assessed using generalized estimating equations.
Results
Across age groups, there was evidence of six classes: a large asymptomatic class, a class characterized by shape/weight concerns, a class characterized by overeating without loss of control, and three resembling full and subthreshold binge eating disorder, purging disorder, and bulimia nervosa. Relative prevalences of classes varied across developmental stages, with symptomatic classes increasing in prevalence with increasing age. Symptomatic classes were associated with concurrent and incident drug use, binge drinking, and high depressive symptoms.
Discussion
A classification system resembling broader definitions of DSM-5 diagnoses along with two further subclinical symptomatic classes may be a useful framework for studying disordered eating among adolescent and young adult females.
Keywords: eating disorder, latent class analysis, eating disorder not otherwise specified, purging disorder, binge eating disorder, classification
Valid case definitions are necessary to understand etiology and assess effectiveness of treatment and prevention strategies. However, achieving such validity is complicated for diseases and disorders that lack a definitive biological test or rely on symptom manifestations, such as eating and other psychiatric disorders1. To address this, investigators propose classification systems of variable utility with an understanding that there is no clear “gold standard” approach. For example, although case definitions based on DSM diagnoses may imperfectly model disordered eating, they can be invaluable to researchers and practitioners who hope to predict and understand the course of illness or response to treatment1,2.
However, it may be developmentally inappropriate to extrapolate classification approaches based on adult studies to understanding presentations in youth. For example, among adults there is one body mass index cut-off for obesity, but among children one must take into account age and gender to interpret whether a child’s body mass index is sufficiently elevated to be considered obese3. With eating disorders, it is possible that eating and weight concerns present differently and/or at subthreshold levels more frequently in preadolescence, adolescence, and young adulthood; if so, applying a classification system without acknowledgment of these differences could misrepresent the prevalence and public health impact, and may miss opportunities to identify causes, consequences, or correlates of the disorders. This could be particularly disconcerting in adolescence, which is when eating disorders often onset and perhaps an ideal time to intervene4,5.
One technique for empirical classification is latent class (LC) analysis, which clusters subjects based upon their observed response patterns into mutually-exclusive classes6. A compelling feature of the LC modeling approach is that, relative to other categorical and dimensional empirical classification approaches, LC analyses make relatively fewer and weaker assumptions. Specifically, LC analyses require that, while observed covariates may be highly correlated unconditionally, the observed covariates are uncorrelated within a class7. Although a strong assumption, clinical homogeneity within classes is an attractive feature. In contrast, dimensional approaches to classification, although often parsimonious and in certain circumstances more biologically plausible, require many additional assumptions about the distributions of and relationships between the observed covariates and unobserved dimensions. For example, dimensional approaches, such as exploratory factor analysis, require the assumption that the errors for factors are independent, have a mean of zero, have equal variance across factors, are multivariate normally distributed, and for orthogonal models, the factors are independent.
LC analysis has been a popular tool in addressing eating disorder classifications (see review by Crow et al 20117), but has been primarily employed in clinical samples of adult patients. As only a small minority of individuals who report disordered eating symptomatology in nationally- representative studies seek treatment for their eating/weight problems 4, it may often be preferable to draw inferences from community-based rather than treatment-seeking samples. Few LC studies have analyzed younger populations and most only included treatment-seeking cases. LC analysis has only been used in one community-based sample of youth, but the 12–23 year old females were analyzed together8. In order to identify possibly prodromal, subclinical, or additional presentations that may arise during the age periods of high incidence4,5, it is essential to evaluate possible classifications in more finely-grained age strata.
Several questions remain unanswered. Is it possible to develop an empirically based classification structure for female preadolscents, adolescents, and young adults? If so, would the classification structure vary across developmental stages, or could a similar set of classes be found throughout youth and young adulthood? Would these classes resemble those seen in empirically-based classification structures for adults? Would these classes be clinically relevant, i.e., would they be predictive of course or adverse outcomes? Answering these questions is essential for future research to understand the natural history of eating disorders and for improvements in early detection, prevention, and treatment. With all these questions in mind, the primary goal of the current study is to empirically derive an eating disorder classification structure for females across developmental stages using LC models, potentially allowing classification to vary through youth and young adulthood. To evaluate the predictive validity of this classification structure, we assessed the association between class membership and the co- occurrence and incidence of drug use, binge drinking, and high depressive symptoms.
METHODS
Sample
The Growing Up Today Study (GUTS) is an ongoing cohort study established in 1996. Participants are the children of women in the Nurses’ Health Study II (NHSII), a cohort of 116,608 nurses followed since 1989 at which point they were ages 25–43 years; details of NHSII have been reported previously9. Women participating in NHSII identified as having children ages 9–14 in 1996 were sent detailed letters with explanations of the purposes of GUTS and request for parental consent. Children of mothers who gave consent were mailed an invitation letter and questionnaire. Approximately 68% of the females (N=9,039 girls from 7,828 families) assented by returning completed questionnaires. These participants were sent questionnaires annually until 2001 and biannually thereafter. Field et al has previously described GUTS protocols and cohort 10. The study was approved by the Human Subjects Committee at Brigham and Women's Hospital and the analyses presented were approved by the Institutional Review Boards at Brigham and Women's Hospital and Children’s Hospital Boston.
For our LC models we restricted the sample to females with observations grouped into five age categories: preadolescence (ages 9–12 years), early adolescence (13–15), late adolescence (16–18), and two periods of young adulthood (19–22; 23–26). Because of the longitudinal nature of this on-going study that started following 9–14 year olds in 1996, we had 12,323, 18,048, 13,477, 12,965, and 4,363 observations from 5,671, 7,389, 6,607, 6,313, and 3,297 families during preadolescence, early adolescence, late adolescence, and the two young adulthood periods, respectively.
Indicators
Eating disorder symptoms were assessed by questionnaire at all study assessments. Questions on purging were adapted from the Youth Risk Behavior Surveillance System questionnaire11. Purging was assessed by asking how often in the past year the participant made herself throw up or used laxatives to keep from gaining weight. Binge eating was assessed with in two parts: participants were first asked about the frequency during the past year of eating a very large amount of food (i.e., overeating); participants who reported overeating were then asked whether they felt out of control during these episodes (loss of control [LOC]). The binge eating and purging questions have been validated in the GUTS cohort12. BMI was calculated from self- reported weight and height. When participants were less than 18 years, we used the age- and gender-specific thresholds from the International Obesity Task Force to classify whether participants were overweight or obese3. When participants were 18 or older, a BMI at or above 25 kg/m2 indicated the participant was overweight or obese. Underweight subjects were rare, and thus we did not separately classify low vs. normal weight. Shape/weight concerns were assessed using the subscale from the McKnight Risk Factor Survey, which has been validated among preadolescent and adolescent girls13. We used these five variables as indicators in our LC models: BMI category (overweight/obese vs. normal/thin), shape/weight concerns, overeating without LOC, binge eating (i.e., overeating with LOC), and purging. Bulimic behaviors (i.e., overeating, binge eating and purging) were categorized using frequencies as none to less than monthly, monthly but less than weekly, and at least weekly.
Outcomes
Three adverse outcomes associated with poorer functioning and long-term health consequences were assessed: drug use, binge drinking, and high depressive symptoms14–16.
Drug use questions were assessed in 1999, 2001, 2003, and 2007. Participants were asked about their use of illicit drugs, including: marijuana or hashish, cocaine, crack (1999, 2001 only), heroin, ecstasy, PCP (1999, 2001 only), GHB (1999, 2001, 2007 only), LSD, mushrooms, Ketamine (1999, 2001 only), crystal meth (2007 only), Rohypnol, and amphetamines. In 2007, participants were also asked about prescription drug use without a prescription. We defined drug use as any past-year use of any of the above drugs other than marijuana. Marijuana was excluded because we wanted to ensure the feeling of being unable to stop eating was due to disordered eating rather than to marijuana use. We further considered as a more severe outcome of frequent drug use, defined as use of any of the above-described drugs at a frequency of 11 or more times in the past year.
Binge drinking was assessed in 1998, 1999, 2000, 2001, 2003, and 2007. Participants who reported ever consuming alcohol were asked several questions regarding their drinking behavior, including past-year frequency of drinking four or more drinks within a few hours. Subjects who reported at least six such episodes were considered binge drinkers. To assess a more severe definition of binge drinking, we defined frequent binge drinking as twelve or more episodes in the past year.
High depressive symptoms were coded as the highest quintile on the McKnight Risk Factor Survey IV or the Center for Depression Scale 10, as these two scales were administered in different survey years13,17. Very high symptoms were similarly coded as the highest decile. Since it is unknown what proportion of these young people met criteria for a depressive disorder or were in need of treatment, we refer to this as high and very high depressive symptoms.
Analyses
LC methods classify response patterns using observed variables (“indicators”), relying on the assumption that the indicators are uncorrelated conditional upon some unobserved (latent) categorical variable (an assumption that provides clinical homogeneity within class). Subjects are assigned to the latent category that their observed response patterns indicate they are most likely to belong to. These methods allow for partially observed subjects to contribute to the model under a missing at random assumption 18, and can account for repeated measurements within the same subject as well as correlation between subjects (e.g., siblings).
LC models were fit using the above-mentioned five indicators. Using these indicators, models were fit successively increasing the number of classes, up through an 8-class solution. Models were fit for each of the five age groups separately, with no a priori restrictions made to find consistent classes across age groups. The Bayesian Information Criterion (BIC), adjusted BIC (ABIC), consistent Akaike Information Criterion (CAIC), minimum class sizes, and entropy were used to guide the optimal number of classes, with particular emphasis on minimizing CAIC while maintaining stable minimal class sizes (e.g., n>=25)19. Models accounted for repeated measures and within-family clustering. Analyses were completed in M-Plus version 6.11 and R version 2.15.1.
GEE models with working independence correlation and empirical variance were used to account for intrafamilial clustering and repeated measures when assessing the association between LC membership and drug use, binge drinking, and depressive symptoms, including both broad and more severe definitions of these outcomes. Associations were assessed both between the LC membership and any concurrent outcome, as well as between the LC membership and incident adverse outcomes assessed in the next survey (i.e., 1–2 years later).
RESULTS
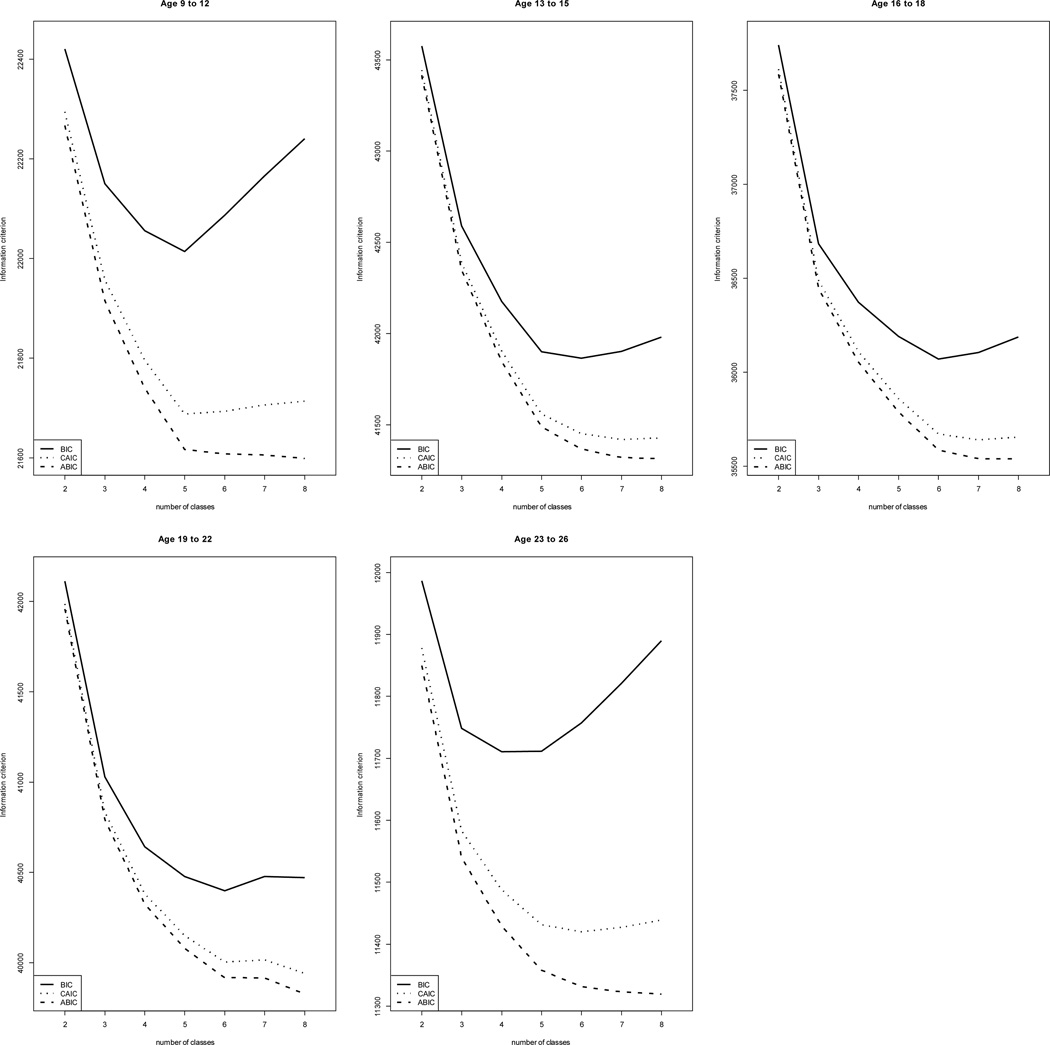
Across all age groups and most decision tools, we found general support for six-class solutions (Figure 1). Based upon BIC or CAIC alone, the best-fitting models for each age group varied primarily from five- to seven-class solutions; based upon the ABIC, the best-fitting models contained eight or more classes. Using as a decision rule the minimum CAIC for models where class sizes are all greater than N=25, the six-class solution was optimal for all age groups except ages 9–12; however, the five- and six-class solutions for ages 9–12 had substantially equivalent entropy and minimum median class probabilities. Across age groups, the minimum median class probabilities for the six-class solutions ranged from 0.57 to 0.83 (median=0.66). We will discuss the six-class solutions as the primary results hereafter, and remark when five- and seven-class solutions led to different conclusions.
Figure 1.
Information criteria and model information for latent class models by age group
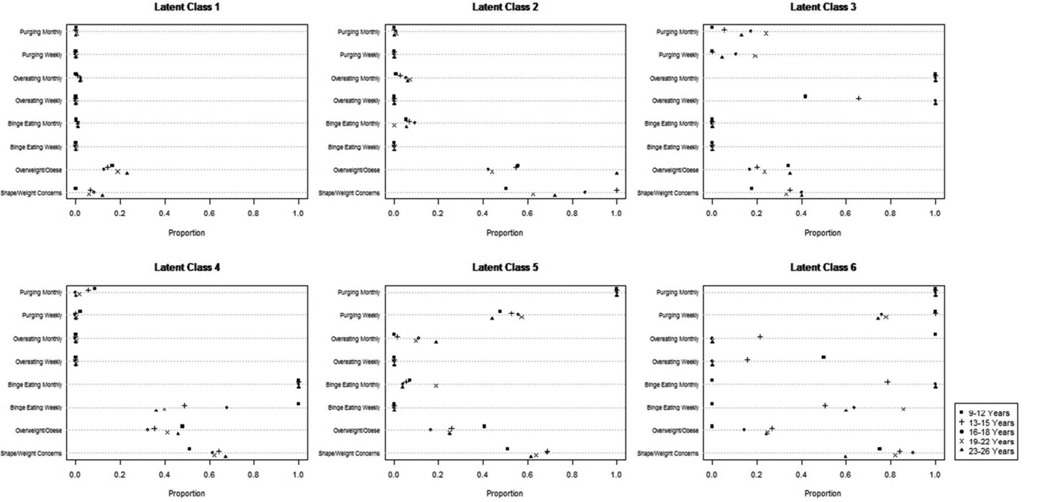
The six classes at each age group can be described as follows (Figure 2): LC1, an asymptomatic class, characterized by a low probability (e.g., <0.03) of all bulimic symptoms; LC2, a class characterized by a high probability of shape/weight concerns (e.g., >0.50) but no other prominent eating disorder symptoms (e.g., <0.10); LC3, a class characterized by a high probability of overeating (e.g., 1.00 of at least monthly) but no binge eating or purging; LC4, a class resembling subclinical and clinical binge eating disorder (BED) with high probabilities of binge eating (e.g., 1.00 of at least monthly) but no purging; LC5, a class resembling subclinical and clinical purging disorder (PD) with high probabilities of purging (e.g., 1.00 of at least monthly) but not binge eating; and LC6, a class resembling subclinical and clinical BN with high probabilities of both binge eating and purging (e.g., >0.75 of at least monthly; note for ages 9–12 this was defined by overeating without loss of control and purging). Five-class solutions generally identified five of these six, with no class resembling BN (LC6) or characterized by cognitive symptoms (LC2) in the younger and older age groups, respectively. Seven-class solutions were less consistent, sometimes featuring new groups characterized by low probabilities of one or more behaviors accompanied by features similar to the classes found in the six-class solution (e.g., purging and overeating; shape/weight concerns with low probability of binge eating) in addition to six classes that appeared similar to those seen in the six-class solution.
Figure 2.
Proportions endorsing each indicator by LC and age group
Although heuristically similar classes were found for all age groups (Table 1), relative prevalence estimates varied (chi-square with 20 df = 2,417, p<0.00001). The symptomatic classes (LC2, LC3, LC4, LC5, and LC6) increase in collective prevalence, e.g., from 5.96% for ages 9–12 to 21.22% for ages 19–22. LC6 is relatively non-existent at earlier ages, presenting in 0.03% and 0.37% of subjects at ages 9–12 and 13–15, respectively, while LC4 and LC5 are more prevalent at these earlier ages (e.g., 1.46 and 1.85% at age 13–15, respectively).
Table 1.
Prevalence of latent classes by age groups
| Number of Observations (%) | ||||||
|---|---|---|---|---|---|---|
| LC1 | LC2 | LC3 | LC4 | LC5 | LC6 | |
|
Ages 9–12 (nobs=12,323, nfam=5,671) |
11342 (94.04) |
799 (6.48) |
94 (0.76) |
47 (0.68) |
37 (0.30) |
4 (0.03) |
|
Ages 13–15 (nobs=18,048, nfam=7,389) |
16437 (91.07) |
833 (4.62) |
115 (0.64) |
264 (1.46) |
333 (1.85) |
66 (0.37) |
|
Ages 16–18 (nobs=13,477, nfam=6,607) |
12013 (89.14) |
649 (4.82) |
110 (0.82) |
187 (1.39) |
356 (2.64) |
162 (1.20) |
|
Ages 19–22 (nobs=12,965, nfam=6,313) |
10214 (78.78) |
1347 (10.39) |
125 (0.96) |
713 (5.50) |
455 (3.51) |
111 (0.86) |
|
Ages 23–26 (nobs=4,363, nfam=3,297) |
3858 (88.43) |
83 (1.90) |
25 (0.57) |
207 (4.74) |
96 (2.20) |
94 (2.15) |
Nfam = number of unique families represented in the age group
Nobs=number of observations
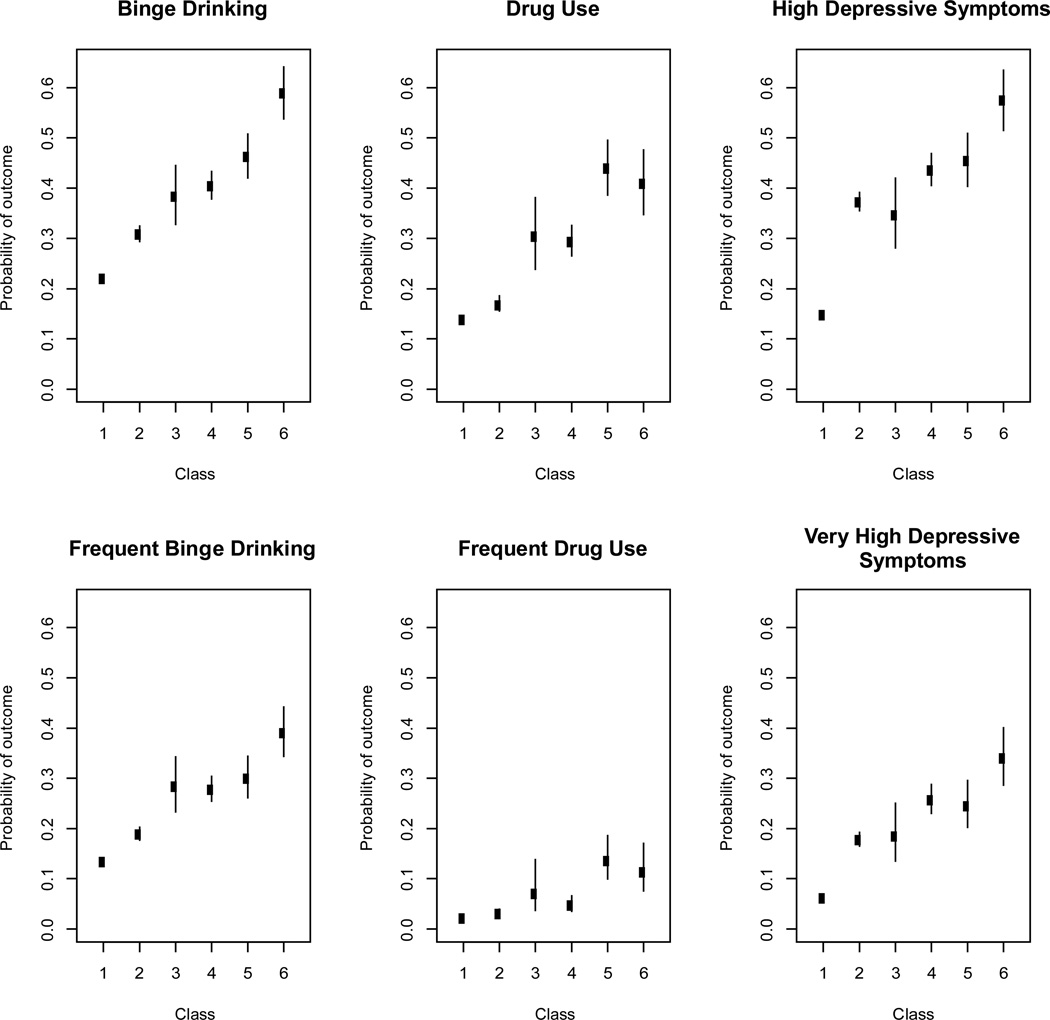
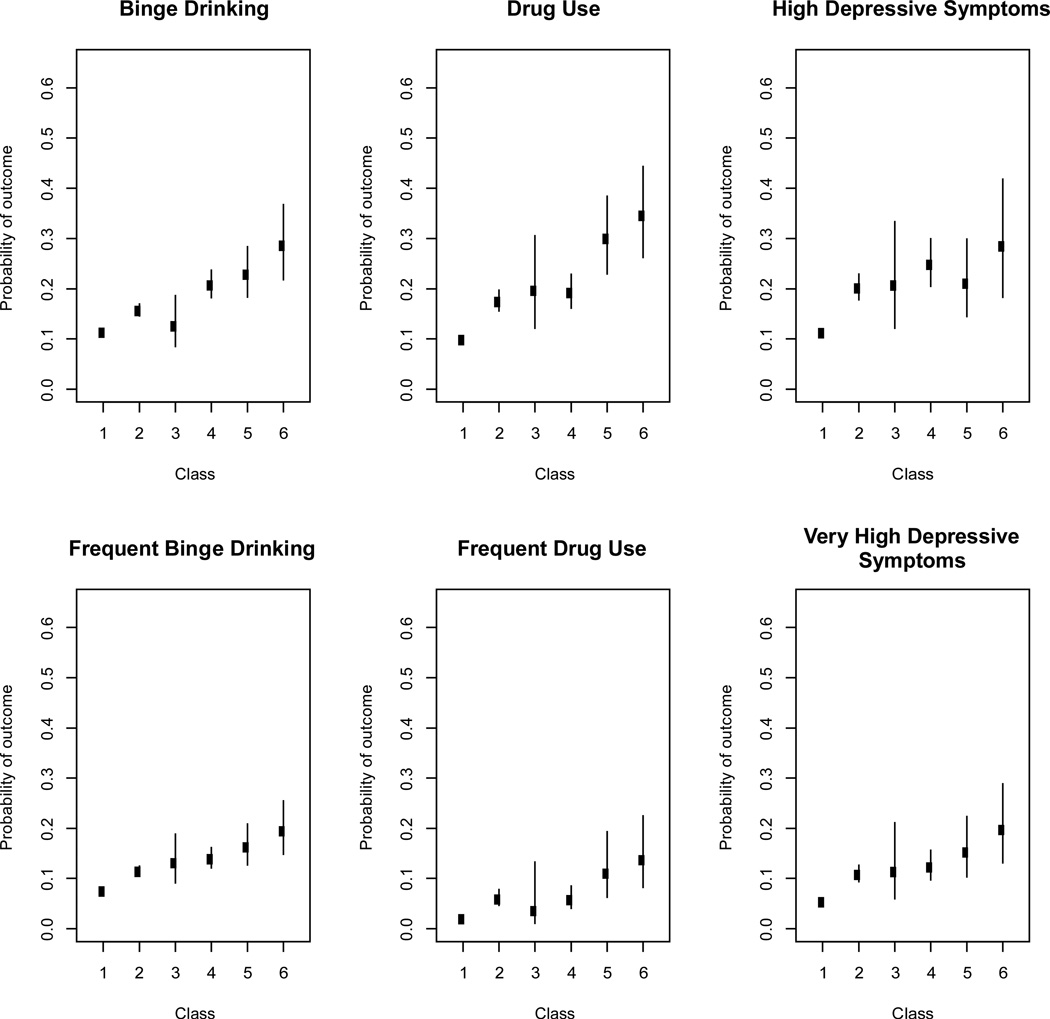
Because binge drinking, drug use, and depressive symptoms were not included on questionnaires until 1998 or 1999 (when only the youngest participants were ages 11–12) and follow-up for these analyses ends in 2007 (when only the oldest participants were ages 23–26), estimating the association between these outcomes and LC membership was not feasible for our youngest and oldest age groups. Given the similarity of class structure across age strata, we chose to estimate a 6-class model for all ages and assess associations with outcomes using this combined model. The probability of endorsing concurrent binge drinking, drug use, and high depressive symptoms by LC are presented in Figure 3; the probability of endorsing an incident outcome 1–2 years later by LC are presented in Figure 4. Generally, classes differentiate for all outcomes, with each of the five symptomatic classes (LC2–6) more likely to report outcomes compared to the asymptomatic class (LC1; e.g., 2- to 4-fold increased risk of high depressive symptoms). Among the symptomatic classes, classes generally differentiated themselves, with LC2 and LC6 having the lowest and highest probability of each outcome, respectively. This was true even for our more severe definitions of outcomes, although the absolute magnitude of differences was diminished. Similar associations were found in age-stratified models at ages 13– 15, 16–18, and 19–22 (results not shown).
Figure 3.
LC membership and concurrent adverse outcomes
Figure 4.
LC membership and incident adverse outcomes 1–2 years later
To understand the stability of these classes, in particular whether classes like LC2 were potentially prodromal, we performed post-hoc analyses to assess the transition probabilities between class membership during ages 9–12 years to class membership during ages 19–22 years. (Note that sample size prohibited performing a stable latent transition model, given there are over 10 million possible transition patterns across all our assessments.) Results are presented in Table 2. While the low prevalence of LC3, LC4, LC5, and LC6 at the first time point limit our interpretability of these girls’ transition probabilities, we see that, relative to LC1, girls in LC2 during preadolescence are more likely to be in LC3–6 a decade later (16.0 vs. 10.6%).
Table 2.
Transitions from latent classes in preadolescence (ages 9–12 years) to young adulthood (ages 19–22 years).
| Young Adulthood Class, N(%)* | ||||||
|---|---|---|---|---|---|---|
| Preadolescence Class |
LC1 | LC2 | LC3 | LC4 | LC5 | LC6 |
| LC1 | 3522 (79.4) |
442 (10.0) |
240 (5.4) | 152 (3.4) | 44 (1.0) | 34 (0.8) |
| LC2 | 186 (62.0) |
66 (22.0) | 19 (6.3) | 24 (8.0) | 2 (0.7) | 3 (1.0) |
| LC3 | 19 (73.1) | 2 (7.7) | 3 (11.5) | 2 (7.7) | 0 (0.0) | 0 (0.0) |
| LC4 | 17 (65.4) | 3 (11.5) | 4 (15.4) | 2 (7.7) | 0 (0.0) | 0 (0.0) |
| LC5 | 10 (58.8) | 5 (29.4) | 0 (0.0) | 1 (5.9) | 0 (0.0) | 1 (5.9) |
| LC6** | NA | NA | NA | NA | NA | NA |
For females who had multiple observations within the age group, the first observation was used.
No females were in LC6 in their first observation during ages 9–12 years.
DISCUSSION
Using LC analysis to classify data from a population-based sample of adolescent and young adult females, we observed six stable classes: a large asymptomatic class (LC1), a class characterized by shape/weight concerns (LC2), a class characterized by overeating (LC3), and three classes mirroring broad definitions of the previously-described eating disorder subtypes BED (LC4), PD (LC5), and BN (LC6). Each class, though supported at every developmental stage, varied in relative prevalence, with prevalence of symptomatic classes increasing with increasing age. Classes resembling BED (LC4), PD (LC5), and BN (LC6) were predictive of incident high depressive symptoms, binge drinking, and drug use. With particular attention to addressing classification through developmental stages, we therefore detail considerations for modeling disordered eating, provide suggestions for the measurement of eating disorders in community- and population-based non-clinical studies, and broadly discuss approaches to case definition through development when gold standards are imperfect.
Several changes to eating disorder criteria have been incorporated into the transition from the DSM-IV to the DSM-5, and our LC model suggests that many of these decisions have positive consequences for the measurement of disordered eating across development. The DSM- 5 includes BED as a specified disorder20, which is supported by our findings of a prevalent BED- like class associated with adverse outcomes. PD is not specified in the DSM-5, although it is described as an example of a “not-elsewhere-classified” diagnosis. Our LC resembling PD (LC5) had as high if not higher risks of adverse outcomes compared to the two classes resembling DSM-5-specified disorders (LC4 and LC6), aligning with other research supporting the clinical validity of PD21–23. Interestingly, individuals in the LC resembling PD (LC5) reported slightly less concurrent binge drinking and high depressive symptoms than did individuals in the LC resembling BN (LC6), but reported incidence of these outcomes as, if not more, frequently; thus, prior research on PD conducted in cross-sectional studies may have undervalued the predictive importance of a PD diagnosis to foreshadow future adverse outcomes. Our model identified two classes characterized by overeating either with (LC4) or without (LC3) LOC; differences between these classes support the importance of LOC in defining relevant subgroups24. Perhaps the most important finding of the current study results is that it is indeed feasible to apply consistent classification to preadolescents, adolescents, and young adults, particularly if broad definitions of BN, BED, and PD are included.
As models for disordered eating continually evolve, our findings highlight several important considerations for eating disorders measurement in epidemiologic research. Most epidemiologic tools for assessing eating disorders in large-scale studies rely on questionnaires or interviews with symptom checklists; often these measure only DSM-specified disorders and are not easily adapted to assess atypical or subthreshold presentations due to question wording and skip rule designs25–28. Moreover, epidemiologic studies in youth often directly apply these adult- based assessment tools, at best with some attention to appropriate question wording. Our results highlight the importance of assessing both purging and binge eating in all youth since many more adolescents engaged in only purging or only binge eating than engaged in both behaviors. We found that the relative size of the PD class increased at a younger age than the BED class, thus using many of the standard instruments that only assess purging among people who endorse binge eating would result in missing many eating disorder cases among adolescents and young adults. Further, studies of youth should measure symptom frequency broadly so that broader definitions may be considered. This is of particular importance for understanding the development of eating disorders. Our largest symptomatic class, characterized by shape/weight concerns alone (LC2), represents another challenge to epidemiologic researchers. Currently, these concerns alone would not be considered an eating disorder unless they were accompanied by underweight status (i.e., AN); however, it may be ill-advised to classify upwards of 10% of the study population as non-cases though they clearly exhibit some disordered eating features and are more likely than asymptomatic individuals to develop adverse outcomes. Moreover, this class may represent the earliest stages of an eating disorder and may be the ideal time to intervene. Indeed, when we assessed class stability between preadolescence and young adulthood, girls who were in LC2 were more likely than girls who were in the asymptomatic class to transition to classes resembling BED, or PD in adulthood.
Our LC analysis model is only one of the many proposed classification systems for eating disorders, and assessing its utility is no simple task. Previous investigators have commented on the utility of classification structures that lack a perfect gold standard, highlighting that the value of valid classification schemes lies in the labels’ power to predict course of illness and response to treatment, and to identify its causes and therefore potential prevention and intervention strategies1. Different models may identify different variations in certain predictors (e.g., genetic, environmental) or consequences (e.g., response to treatment, future course of illness, adverse outcomes)2. Numerous approaches have been suggested for eating disorders, from the DSM-IV and DSM-5 criteria sets to a single eating disorder category, continuum-based approaches, and variations of “lumping” and “splitting” individuals reporting disordered eating symptoms. Approaches have been validated to accomplish specific goals, but no single system best classifies individuals throughout their lifespan while trying to fully understand the underlying causes and the future course of these states. Our LC model provides an empirically-based classification scheme that applies well to female preadolescents, adolescents, and young adults. For researchers and practitioners working with female youth and young adults, our five symptomatic classes provide informative divisions of the population, particularly when used to predict future adverse outcomes or when constructs need to be consistent throughout development. That said, a more nuanced or continuum-based approach incorporated into this class structure could provide additional information predictive of the likely course and outcomes. For example, there is evidence from clinical studies that increased frequency of bulimic behaviors is associated with poorer outcomes20, and it has been more generally suggested that eating disorders may benefit from a staging or continua-based approach similar to that used to classify hypertension29. Incorporating such dimensions into a classification approach would likely be beneficial for the predictive validity of the classification structure, but we were limited by our sample size (large though it was) in terms of reliably evaluating this potential benefit.
This research is not without limitations. The cohort is mostly Caucasian and not representative with respect to socioeconomic status, thus results may not generalize. Although prevalence of eating disorders likely differs across race/ethnicity and socioeconomic status30, it is unclear whether types of presentations or associated risks also differ. Moreover, the results may not generalize to males. Recent research suggests that eating disorders may present differently in males compared to females4,31. The choice to focus the current study on girls and young women should not be viewed as neglectful of the importance of studying eating disorders in males, but rather as an awareness of the need to consider gender differences rather than assuming the same criteria apply to both genders. The study relies on self-report, and thus may be susceptible to symptom misclassification; however, GUTS eating disorder measures were previously validated against interviews, yielding high sensitivity, specificity, and negative predictive values (e.g., for purging: 0.73, 0.87, and 0.99, respectively). Due to power limitations, we were unable to consider “underweight” as a separate BMI category in our models, and are limited regarding conclusions for presentations characterized by low weight, including AN. AN, however, has a low prevalence in this sample and other population-based studies4,5,29; participants who meet criteria for the restrictive AN subtype likely clustered in the large LC2, providing another motivation to study LC2 further. The outcomes considered in this study (binge drinking, drug use, and high depressive symptoms) are self-reported without any measurement of impairment; therefore, we cannot distinguish whether persons experiencing those outcomes require treatment. However, using both concurrent and incident outcomes at various thresholds of severity, we were able to observe important distinctions between the classes; further research is needed to see whether such classes differentiate well with respect to other validators such as treatment response. Moreover, further research is needed to understand if age moderates the relationships between LC membership and our validators: in comparing the 13–15, 16–18, and 19–22 age subgroups, we saw no evidence that age moderated these associations, but were likely underpowered to appropriately address this important question. Finally, due to the nature of longitudinal studies, we had fewer observations in older than younger age groups because some subjects were lost to follow-up. Our models assume that such missing data occurs at random, which may not be the case. However, LC models (particularly in large samples) are relatively robust to violations of this assumption19. Thus, given the consistency of our findings, it is unlikely our general conclusions are affected by this missing, although we may have missed opportunities to identify rare classes that only onset in later ages. These limitations are likely outweighed by the strengths of this large prospective study. LC methods allowed us to incorporate study features (such as repeated/correlated measurements and partially observed data) that would not be feasible using less flexible classification methods. This is only the second LC analysis conducted in a population-based adolescent sample8, and the first to study multiple developmental periods. We studied prospective validators, arguably the most important yet least utilized type of validator for assessing the utility of classifications schemas for public health purposes7.
Creating classification systems that span developmental periods is a sensitive task, and using an age-independent system should be employed only with empirical support. Our study suggests several important potential directions for the classification and modeling of disordered eating as applied through development, including considering PD as a distinct and important entity, and taking a broader or more continuum-based perspective of frequency thresholds for bulimic behaviors. Our study also identifies individuals who report cognitive features of eating disorders in the absence of bulimic behaviors as an area for further public health research. Moreover, it may be advisable for clinicians treating adolescents and young adults to screen for cognitive symptoms of eating disorders, as well as bulimic behaviors, so they can identify patients at high risk for a range of adverse outcomes. Rather than viewing eating disorders as the distinct DSM-5 categories of AN, BN, BED, and “other”, researchers and practitioners may find a more nuanced view of classification to be useful, utilizing the presented model particularly for female youth and young adults.
Acknowledgements
Data collection was supported by research grants from the National Institutes of Health (MH087786, DK59570, DK46200, HL68041, and HD049889); the analysis was supported by MH087786.
Abbreviations
- AN
anorexia nervosa
- BED
binge eating disorder
- BN
bulimia nervosa
- DSM
Diagnostic and Statistical Manual
- EDNOS
eating disorder not otherwise specified
- GUTS
Growing Up Today Study
- LC
latent class
- LOC
loss of control
- NHSII
Nurses’ Health Study II
- PD
purging disorder
Footnotes
Financial Disclosures: The authors have indicated they have no financial relationships relevant to this article to disclose.
Contributor Information
Sonja A. Swanson, Department of Epidemiology, Harvard School of Public Health, Boston MA
Nicholas J. Horton, Department of Mathematics and Statistics, Amherst College, Amherst, MA
Ross D. Crosby, Neuropsychiatric Research Institute and Department of Clinical Neuroscience, University of North Dakota School of Medicine and Health Sciences, Fargo, ND
Nadia Micali, Behavioural and Brain Sciences Unit, Institute of Child Health, University College London, London, UK.
Kendrin R. Sonneville, Division of Adolescent Medicine, Department of Medicine, Boston Children’s Hospital and Harvard Medical School, Boston, MA
Kamryn Eddy, Harris Center for Education and Advocacy in Eating Disorders, Department of Psychiatry, Massachusetts General Hospital, Boston, MA; Harvard Medical School, Boston, MA.
Alison E. Field, Department of Epidemiology, Harvard School of Public Health, Boston MA Division of Adolescent Medicine, Department of Medicine, Boston Children’s Hospital and Harvard Medical School, Boston, MA; Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA.
REFERENCES
- 1.Crow SJ, Swanson SA, Peterson CB, Crosby R, Wonderlich SA, Mitchell JE. Latent structure analyses of eating disorder diagnoses: Critical review of results and methodologic issues. In: Striegel-Moore RH, Wonderlich SA, Walsh T, Mitchell JE, editors. Towards an Evidence Based Classification of Eating Disorders: American Psychiatric Association Monograph on Eating Disorders. American Psychiatric Publishing; 2011. pp. 103–120. [Google Scholar]
- 2.Pinheiro AP, Bulik CM, Sullivan PF, Machado PP. An empirical study of the typology of bulimic symptoms in young Portuguese women. Int J Eat Disord. 2008 Apr;41(3):251–258. doi: 10.1002/eat.20497. [DOI] [PubMed] [Google Scholar]
- 3.Solomon CG, Willett WC, Carey VJ, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. Jama. 1997 Oct 1;278(13):1078–1083. [PubMed] [Google Scholar]
- 4.Field AE, Camargo CA, Jr., Taylor CB, Berkey CS, Roberts SB, Colditz GA. Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics. 2001 Jan;107(1):54–60. doi: 10.1542/peds.107.1.54. [DOI] [PubMed] [Google Scholar]
- 5.Kann L, Warren CW, Harris WA, et al. Youth risk behavior surveillance-- United States, 1995. J Sch Health. 1996 Dec;66(10):365–377. doi: 10.1111/j.1746-1561.1996.tb03394.x. [DOI] [PubMed] [Google Scholar]
- 6.Field AE, Taylor CB, Celio A, Colditz GA. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. Int J Eat Disord. 2004 Jan;35(1):86–92. doi: 10.1002/eat.10220. [DOI] [PubMed] [Google Scholar]
- 7.Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord. 1999 Mar;25(2):195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 8.Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan MR, Berger AT, Wells BE, Cleland CM. Longitudinal associations between adolescent alcohol use and adulthood sexual risk behavior and sexually transmitted infection in the United States: assessment of differences by race. Am J Public Health. 2012 May;102(5):867–876. doi: 10.2105/AJPH.2011.300373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012 Jan 7;379(9810):55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- 11.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994 Mar-Apr;10(2):77–84. [PubMed] [Google Scholar]
- 12.Little R, Rubin D. Statistical analysis with missing data. 2nd edition. New York: John Wiley & Sons; 2002. [Google Scholar]
- 13.Swanson SA, Lindenberg K, Bauer S, Crosby RD. A Monte Carlo investigation of factors influencing latent class analysis: An application to eating disorder research. Int J Eat Disord. 2012 Jul;45(5):677–684. doi: 10.1002/eat.20958. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association DSM-5 Task Force. DSM-5 Development. 2012 www.dsm5.org, 2012.
- 15.Haedt AA, Keel PK. Comparing definitions of purging disorder on point prevalence and associations with external validators. Int J Eat Disord. 2010 Jul;43(5):433–439. doi: 10.1002/eat.20712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keel PK, Wolfe BE, Gravener JA, Jimerson DC. Co-morbidity and disorder- related distress and impairment in purging disorder. Psychol Med. 2008 Oct;38(10):1435–1442. doi: 10.1017/S0033291707001390. [DOI] [PubMed] [Google Scholar]
- 17.Keel PK, Haedt A, Edler C. Purging disorder: an ominous variant of bulimia nervosa? Int J Eat Disord. 2005 Nov;38(3):191–199. doi: 10.1002/eat.20179. [DOI] [PubMed] [Google Scholar]
- 18.Sonneville KR, Horton NJ, Micali N, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatr. 2013 Feb;167(2):149–155. doi: 10.1001/2013.jamapediatrics.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000 Jan;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Robins LN, Wing J, Wittchen HU, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988 Dec;45(12):1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 21.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. New York, NY: New York State Psychiatric Institute Biometrics Reseach Department; 1995. [Google Scholar]
- 22.Swanson SA, Brown TA, Crosby RD, Keel PK. What are we missing? The costs versus benefits of skip rule designs. Int J Methods Psychiatr Res. 2013 Sep 13; doi: 10.1002/mpr.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Field AE, Sonneville KR, Micali N, et al. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012 Aug;130(2):e289–e295. doi: 10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marques L, Alegria M, Becker AE, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2010 Jul 27; doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Field AE, Sonneville KR, Crosby RD, et al. Prospective associations of concerns about physique and the development of obesity, binge drinking, and drug use among adolescent boys and young adult men. JAMA Pediatr. 2014 Jan 1;168(1):34–39. doi: 10.1001/jamapediatrics.2013.2915. [DOI] [PMC free article] [PubMed] [Google Scholar]