Abstract
Purpose
We aimed to determine if baseline sedentary behavior was associated with changes in BMI over 9 years.
Methods
Participants were enrolled into the NIH-AARP Diet and Health study in 1995–1996 (median age 63) and BMI was reported at baseline and 9 years later (n=158,436). Sitting time (<3 [referent], 3–4, 5–6, 7–8 or ≥9 h/d), television viewing (None, <1, 1–2, 3–4, 5–6, 7–8, or ≥9 h/d) and the covariates (age, sex, race, education, smoking, moderate-to-vigorous physical activity, caloric intake, and sleep duration) were reported at baseline. We used longitudinal quantile regression to model changes at the 10th, 25th, 50th, 75th and 90th BMI percentiles.
Results
More sitting at baseline was associated with additional increases in BMI over time and the association was stronger at the upper BMI percentiles (e.g. <3h/d [referent] vs. 5–6 h/d sitting additional increases: 50th percentile = 0.41 kg/m2, 95% CI: 0.34, 0.48 & 90th percentile = 0.85 kg/m2, 95% CI: 0.72, 0.98). Similar associations were observed between more television viewing at baseline and additional increases in BMI over time (e.g., no television [referent] vs. 3–4 h/d of television: 50th percentile= 1.96 kg/m2, 95% CI: 1.77, 2.15 & 90th percentile = 2.11 kg/m2, 95% CI: 1.49, 2.73).
Conclusion
Reducing sedentary behavior could help prevent an increase in BMI in adulthood, especially at the upper percentiles of the BMI distribution, and thereby reduce the prevalence of obesity.
Keywords: Adult, longitudinal, obesity, sitting, television
Introduction
It is estimated that 36% of adults in the U.S. are currently obese (9). In the 1960s the prevalence of adult obesity was 13% (10) and the three-fold rise in obesity over the last 50 years has had untoward health and economic consequences (38, 39). Notably, an increase in time spent in sedentary behavior coincided with the rise in obesity (23) and there is emerging evidence that sedentary behavior may have contributed to the increase in adult obesity (24).
Sedentary behaviors include any waking behavior characterized by low energy expenditure, while in a sitting or reclining posture (25, 31). The majority of waking hours are spent in sedentary behavior, even if moderate-to-vigorous physical activity (MVPA) guidelines are met (19, 25), and television viewing is one of the most common sedentary behaviors reported in leisure-time (25). Observational studies have reported positive associations between sedentary behavior and the mean body mass index (BMI) or BMI categories (3, 7, 14, 21, 22, 26, 33, 37), but the majority of studies are cross-sectional that cannot establish temporal precedence (3, 7, 22, 26, 33, 37). Further, associations with the mean BMI may reflect changes at the lower and/or upper percentiles of the BMI distribution and it is of primary interest to investigate the upper percentiles of the BMI distribution when studying obesity. Categorizing individuals into normal, overweight and obese groups based on their BMI recognizes the importance of the upper percentiles of the BMI distribution. However, such categorization considers those within a category as homogeneous and considers individuals in proximity to a category cutoff, but on opposite sides, as being very different when they are very similar (1).
Quantile regression is an analytic approach that does not require participants to be placed into BMI categories, and can test if there is an association between sedentary behavior at the median BMI and other percentiles of the BMI distribution (28). Therefore, the purpose of our study was to determine if sedentary behavior was associated with changes in BMI over 9 years, by modeling percentiles across the BMI distribution.
Methods
Participants were enrolled in the NIH-AARP Diet and Health Study (30). The NIH-AARP Diet and Health Study was initiated in 1995–1996 when 3.5 million questionnaires were mailed to AARP members, aged 50–71 years old, residing in six states (CA, FL, LA, NC, NJ, and PA) and two metropolitan areas (Atlanta, GA and Detroit, MI). The baseline questionnaire was completed by 567,169 men and women (30). Within 6 months individuals who did not have self-reported history of colon, prostate, and breast cancer received a risk factor questionnaire in the mail, which was completed by 334,906 men and women. We excluded those who had a proxy reporter complete their questionnaires (n=10,383). We then excluded those who reported having cancer (n=16,082), or poor health (n=4,382), as such individuals may have experienced changes in weight as a consequence of their poor health. We then excluded those with missing baseline BMI (n=6,181) and baseline BMIs <14 kg/m2 or >60 kg/m2 (n=586), as such BMIs are not representative of the general population. We then excluded, in the following order, those with unknown sitting and television viewing hours (n=2,301); unknown race (n=3,153); unknown education level (n=6,224); unknown smoking dose data (n=8,810); unknown MVPA data (n=3,073); those consuming < 300 calories per day and >5900 calories per day (n=1,306); and unknown sleep duration data (n=273). After these exclusions a total of 272,152 participants remained. To be included in our study the participants also had to have reported their weight on the follow-up questionnaire that was completed between 2004 and 2006 (n=158,696). Follow-up BMIs <14 kg/m2 (n=223) or >60 kg/m2 (n=37) at follow-up were excluded leaving a total of 158,436 participants for our longitudinal study. The Special Studies Institutional Review Board of the National Cancer Institute approved the study. Questionnaire completion was considered to imply informed consent.
The participants self-reported their height and weight on the baseline and follow-up questionnaire and these data were used to calculate BMI (kg/m2). There is high correlation between BMI calculated from self-reported and objectively measured height and weight (r >0.9) (20). There is also high correlation between BMI and dual energy X-ray absorptiometry estimated fat mass (36).
Sitting time was used in our study to provide an estimate of total daily sedentary behavior. Participants reported their daily sitting hours (<3, 3–4, 5–6, 7–8, or 9+ h/d) in response to the following question on the risk factor questionnaire, “During a typical 24-hour period during the past 12 months, how much time did you spend sitting?” Television viewing is a common leisure-time sedentary behavior. Participants reported their television viewing hours (None, <1, 1–2, 3–4, 5–6, 7–8, or 9+ h/d) in response to the following question on the risk factor questionnaire, “During a typical 24-hour period over the past 12 months, how much time did you spend watching television or video?”
Participants self-reported their gender, age, race (Non-Hispanic White, Non-Hispanic Black, Hispanic, or Asian/Pacific Islander/American Indian/Alaskan Native), and education level (<8 years, 8–11 years, High School Diploma, Some College, or College/Postgraduate Degree). These demographic covariates were included because younger, white men with higher education levels are more likely to have lower BMI (9), and time spent in sedentary behavior varies across demographic groups (19). Smoking was self-reported (never, 1–10, 11–20, 21–30, 31–40, 41–60, or ≥60 cigarettes per day) and was included as a covariate because it has been associated with BMI and sedentary behavior (15). Participants also self-reported the frequency with which they engaged in MVPA (never, rarely, weekly but <1h/wk, 1–3 h/wk, 4–7 h/wk, or >7 h/wk) in response to the following question at baseline: “How often did you participate in moderate and vigorous physical activities in the past 10 years?” Self-reported dietary patterns were measured using a 124-item food frequency questionnaire at baseline and daily caloric intakes were estimated based on their responses (35). Self-reported sleep duration (<5, 5–6, 7–8, or ≥9 h/d) was assessed at baseline with the following question: “During a typical 24 hour period over the past 12 months, how many hours did you spend sleeping at night?” Caloric intake, MVPA, and sleep duration were included as covariates to determine if any association between sedentary behavior and BMI was independent of MVPA, an increase in caloric intake, or a reduction in sleep duration (4, 25, 32).
Medians and interquartile ranges are presented to describe the continuous variables and frequencies and percentages are presented to describe the categorical variables. Quantile regression was used to address the aims of the study. This analytical method is related to linear regression, but rather than estimating the association between a predictor and the mean of a continuous outcome variable, the median and any other percentile of the continuous outcome variable can be modeled (28). The regression coefficients from quantile regression are interpreted in the same way as those from linear regression (i.e. the coefficient represents the change in the outcome variable for a one unit change in the predictor). The data were re-arranged into the long-format, with a time variable created to represent baseline (time=0) and follow-up (time=1), and the correlation between repeated BMI measures was taken into account (5). BMI was modeled as the dependent variable and time and sedentary behavior were included as predictors; associations at the 10th, 25th, 50th, 75th and 90th BMI percentiles were specifically investigated. The following covariates were included in the models: baseline age, gender, race, education level and baseline smoking dose (model 1); plus baseline MVPA, baseline caloric intake, and baseline sleep duration (model 2). Change in the mean BMI was also modeled to allow for comparison to be made with the quantile regression findings, using generalized estimating equation (GEE). All models were performed separately for sitting time and television viewing, except for model 3 which included both sedentary behaviors. The analyses were completed using Stata 12.0 (StataCorp LP, College Station, TX).
Results
The characteristics of the study participants are presented in Table 1. The median age at baseline was 63.3 years, 59.7% were men, 93.5% were non-Hispanic white, and 39.5% had a college or graduate degree. The median BMI at baseline was 26.3 kg/m2 and most participants reported sitting for 3–4 and 5–6 hours per day (57.4%), and most participants reported watching television for 3–4 hours per day (44.4%) (Table 1). Participants in the highest BMI quartile at baseline reported more sitting and more television viewing compared to participants in the lowest BMI quartile at baseline (Table 1).
Table 1.
Baseline characteristics of the participants
| Body Mass Index (BMI) Quartiles | |||||
|---|---|---|---|---|---|
| Total Sample (n=158,696) |
1st Quartile (n=40,110) |
2nd Quartile (n=40,540) |
3rd Quartile (n=39,812) |
4th Quartile (n=38,234) |
|
| Age, median (IQR), y | 62.6 (57.8, 66.5) | 62.7 (57.8, 66.7) | 63.0 (58.2, 66.7) | 62.8 (58.0, 66.6) | 61.8 (57.3, 65.9) |
| Height, median (IQR), m | 1.73 (1.65, 1.80) | 1.70 (1.63, 1.78) | 1.73 (1.65, 1.80) | 1.75 (1.68, 1.80) | 1.73 (1.63, 1.80) |
| Weight, median (IQR), kg | 79.0 (68.1, 89.0) | 63.6 (56.8, 70.4) | 75.4 (68.1, 81.7) | 84.0 (76.7, 89.9) | 96.2 (87.2, 106.2) |
| BMI, median (IQR), kg/m2 | 26.0 (23.7, 29.1) | 22.3 (21.0, 23.0) | 25.0 (24.4, 25.6) | 27.5 (26.7, 28.3) | 31.9 (30.3, 34.5) |
| Gender, N (%) | |||||
| Male | 92,810 (58.5) | 17,612 (43.9) | 26,237 (64.7) | 26,941 (67.7) | 22,020 (57.6) |
| Female | 65,886 (41.5) | 22,498 (56.1) | 14,303 (35.3) | 12,871 (32.3) | 16,214 (42.4) |
| Race, N (%) | |||||
| Non-Hispanic White | 149,953 (94.5) | 38,116 (95.0) | 38,421 (94.8) | 37,603 (94.5) | 35,813 (93.7) |
| Non-Hispanic Black | 4,313 (2.72) | 623 (1.55) | 879 (2.17) | 1,153 (2.90) | 1,658 (4.34) |
| Hispanic | 2,321 (1.46) | 478 (1.19) | 656 (1.62) | 653 (1.64) | 534 (1.40) |
| Asian/AI/AN/PI | 2,109 (1.33) | 893 (2.23) | 584 (1.44) | 403 (1.01) | 229 (0.60) |
| Education, N (%) | |||||
| <8 years | 5,652 (3.56) | 1,047 (2.61) | 1,345 (3.32) | 1,456 (3.66) | 1,804 (4.72) |
| 8–11 years | 27,977 (17.6) | 6,489 (16.2) | 6,601 (16.3) | 7,043 (17.7) | 7,844 (20.5) |
| High School Diploma | 15,658 (9.87) | 3,667 (9.14) | 3,850 (9.50) | 4,000 (10.1) | 4,141 (10.8) |
| Some College | 37,366 (23.6) | 9,124 (22.8) | 9,111 (22.5) | 9,445 (23.7) | 9,686 (25.3) |
| College/Postgraduate | 72,043 (45.4) | 19,783 (49.3) | 19,633 (48.4) | 17,868 (44.9) | 14,759 (38.6) |
| Sitting, N (%) | |||||
| <3 h/d | 30,308 (19.1) | 8,767 (21.9) | 7,996 (19.7) | 7,579 (19.0) | 5,966 (15.6) |
| 3–4 h/d | 46,070 (29.0) | 11,989 (29.9) | 12,068 (29.8) | 11,662 (29.3) | 10,351 (27.1) |
| 5–6 h/d | 44,539 (28.1) | 10,785 (26.9) | 11,378 (28.1) | 11,372 (28.6) | 11,004 (28.8) |
| 7–8 h/d | 24,236 (15.3) | 5,734 (14.3) | 5,968 (14.7) | 5,974 (15.0) | 6,560 (17.2) |
| ≥9 h/d | 13,543 (8.53) | 2,835 (7.07) | 3,130 (7.72) | 3,225 (8.10) | 4,353 (11.4) |
| Television, N (%) | |||||
| None | 1,303 (0.82) | 593 (1.48) | 325 (0.80) | 211 (0.53) | 174 (0.46) |
| <1 h/d | 10,642 (6.71) | 3,990 (9.95) | 2,968 (7.32) | 2,173 (5.46) | 1,511 (3.95) |
| 1–2 h/d | 48,034 (30.3) | 13,900 (34.7) | 13,195 (32.6) | 11,711 (29.4) | 9,228 (24.1) |
| 3–4 h/d | 69,621 (43.9) | 16,112 (40.2) | 17,634 (43.5) | 18,271 (45.9) | 17,604 (46.0) |
| 5–6 h/d | 22,691 (14.3) | 4,376 (10.9) | 5,205 (12.8) | 5,881 (14.8) | 7,229 (18.9) |
| 7–8 h/d | 3,582 (2.26) | 643 (1.60) | 686 (1.69) | 867 (2.18) | 1,386 (3.63) |
| ≥9 h/d | 2,823 (1.78) | 496 (1.24) | 527 (1.30) | 698 (1.75) | 1,102 (2.88) |
AI, American Indian; AN, Alaskan Native; BMI, body mass index, IQR, interquartile range; PI, Pacific Islanded
Changes in the BMI distribution occurred from baseline to follow-up (Tables 2 and 3, time coefficients). The 10th BMI percentile was lower at follow-up, the 25th BMI percentile remained stable, and the 50th, 75th, and 90th BMI percentiles were greater at follow-up. On average, BMI increased by 0.18 kg/m2 between baseline and follow-up as indicated by the GEE time coefficients (Tables 2 and 3).
Table 2.
Longitudinal associations between sitting time and specific BMI percentiles changes over 9 years
| Body Mass Index (BMI, kg/m2) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantile Regression | GEE | |||||||||||||
| 10th Percentile | 25th Percentile | 50th Percentile | 75th Percentile | 90th Percentile | Mean | |||||||||
| b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | |||
| Model 1 | Intercept | 24.9 | 24.6, 25.2 | 27.1 | 26.8, 27.4 | 30.5 | 30.2, 30.8 | 35.7 | 35.3, 36.1 | 42.2 | 41.6, 42.8 | 31.9 | 31.6, 32.2 | |
| Time | −0.19 | −0.21, −0.17 | −0.02 | −0.03, 0.00 | 0.15 | 0.13, 0.17 | 0.30 | 0.27, 0.32 | 0.47 | 0.42, 0.51 | 0.18 | 0.17, 0.19 | ||
| Sitting | <3 h/d | Ref | Ref | Ref | Ref | Ref | Ref | |||||||
| 3–4 h/d | 0.15 | 0.09, 0.22 | 0.19 | 0.13, 0.25 | 0.27 | 0.21, 0.32 | 0.48 | 0.39, 0.56 | 0.61 | 0.48, 0.74 | 0.38 | 0.32, 0.44 | ||
| 5–6 h/d | 0.27 | 0.21, 0.34 | 0.36 | 0.29, 0.42 | 0.51 | 0.45, 0.57 | 0.80 | 0.72, 0.87 | 1.11 | 0.96, 1.26 | 0.67 | 0.60, 0.73 | ||
| 7–8 h/d | 0.29 | 0.22, 0.36 | 0.40 | 0.33, 0.46 | 0.63 | 0.56, 0.70 | 1.09 | 1.01, 1.18 | 1.64 | 1.47, 1.80 | 0.89 | 0.82, 0.97 | ||
| ≥ 9 h/d | 0.44 | 0.34, 0.54 | 0.63 | 0.55, 0.72 | 1.09 | 0.99, 1.18 | 1.88 | 1.75, 2.02 | 2.99 | 2.74, 3.24 | 1.51 | 1.42, 1.60 | ||
| Model 2 | Intercept | 25.1 | 24.7, 25.6 | 27.6 | 27.2, 27.9 | 31.5 | 31.2, 31.8 | 37.3 | 36.8, 37.9 | 44.0 | 43.2, 44.9 | 33.0 | 32.6, 33.3 | |
| Time | −0.19 | −0.21, −0.17 | −0.02 | −0.04, −0.01 | 0.14 | 0.12, 0.16 | 0.32 | 0.30, 0.35 | 0.49 | 0.45, 0.53 | 0.18 | 0.17, 0.19 | ||
| Sitting | <3 h/d | Ref | Ref | Ref | Ref | Ref | Ref | |||||||
| 3–4 h/d | 0.12 | 0.05, 0.19 | 0.15 | 0.08, 0.21 | 0.24 | 0.17, 0.31 | 0.41 | 0.33, 0.48 | 0.57 | 0.44, 0.70 | 0.33 | 0.27, 0.39 | ||
| 5–6 h/d | 0.22 | 0.16, 0.29 | 0.29 | 0.22, 0.35 | 0.41 | 0.34, 0.48 | 0.65 | 0.58, 0.72 | 0.85 | 0.72, 0.98 | 0.54 | 0.48, 0.61 | ||
| 7–8 h/d | 0.19 | 0.13, 0.26 | 0.26 | 0.18, 0.33 | 0.46 | 0.39, 0.53 | 0.79 | 0.69, 0.88 | 1.19 | 1.05, 1.34 | 0.67 | 0.59, 0.74 | ||
| ≥ 9 h/d | 0.31 | 0.20, 0.43 | 0.45 | 0.37, 0.52 | 0.76 | 0.67, 0.85 | 1.32 | 1.19, 1.45 | 2.15 | 1.93, 2.37 | 1.12 | 1.03, 1.21 | ||
| Model 3 | Intercept | 24.5 | 24.1, 24.9 | 26.9 | 26.5, 27.4 | 30.39 | 29.9, 30.9 | 35.69 | 35.1, 36.3 | 42.03 | 41.0, 43.1 | 32.2 | 31.8, 32.7 | |
| Time | −0.17 | −0.19, −0.15 | −0.01 | −0.03, 0.01 | 0.15 | 0.13, 0.17 | 0.32 | 0.29, 0.35 | 0.46 | 0.42, 0.50 | 0.18 | 0.17, 0.19 | ||
| Sitting | <3 h/d | Ref | Ref | Ref | Ref | Ref | Ref | |||||||
| 3–4 h/d | 0.03 | −0.04, 0.09 | 0.01 | −0.05, 0.07 | 0.05 | −0.00, 0.11 | 0.18 | 0.10, 0.25 | 0.31 | 0.18, 0.44 | 0.15 | 0.08, 0.21 | ||
| 5–6 h/d | 0.07 | 0.00, 0.13 | 0.07 | 0.01, 0.12 | 0.10 | 0.04, 0.15 | 0.25 | 0.16, 0.34 | 0.37 | 0.26, 0.49 | 0.22 | 0.16, 0.29 | ||
| 7–8 h/d | 0.07 | −0.01, 0.14 | 0.03 | −0.05, 0.10 | 0.12 | 0.05, 0.19 | 0.34 | 0.25, 0.44 | 0.59 | 0.40, 0.79 | 0.32 | 0.24, 0.40 | ||
| ≥ 9 h/d | 0.14 | 0.05, 0.23 | 0.19 | 0.11, 0.26 | 0.38 | 0.30, 0.46 | 0.82 | 0.70, 0.94 | 1.46 | 1.22, 1.71 | 0.73 | 0.64, 0.82 | ||
GEE, generalized estimating equation. Data presented are beta coefficients (b) and 95% confidence intervals (95% CI). The intercept is the predicted BMI at baseline for the referent group (ref). The time coefficient is code 0 for baseline and 1 for follow-up and so represents the change in BMI from baseline to follow-up. The sitting/television coefficients represent the difference in BMI for each sitting/television category relative to the referent group. Model 1 adjusted for age, gender, race, education and smoking dose. Model 2 adjusted for covariates in Model 1 plus MVPA, calories and sleep duration. Model 3 adjusted covariates in Model 2 plus television viewing.
Table 3.
Longitudinal associations between television viewing and specific BMI percentiles changes over 9 years
| Body Mass Index (BMI, kg/m2) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantile Regression | GEE | |||||||||||||
| 10th Percentile | 25th Percentile | 50th Percentile | 75th Percentile | 90th Percentile | Mean | |||||||||
| Model 1 | Intercept | 24.6 | 24.3, 25.0 | 26.8 | 26.5, 27.1 | 30.1 | 29.8, 30.4 | 35.7 | 35.2, 36.1 | 43.2 | 42.3, 44.1 | 32.0 | 31.6, 32.4 | |
| Time | −0.19 | −0.21, −0.16 | −0.01 | −0.03, 0.01 | 0.15 | 0.13, 0.17 | 0.29 | 0.27, 0.32 | 0.45 | 0.40, 0.50 | 0.18 | 0.17, 0.19 | ||
| Television | None | Ref | Ref | Ref | Ref | Ref | Ref | |||||||
| <1 h/d | 0.37 | 0.13, 0.61 | 0.42 | 0.23, 0.60 | 0.58 | 0.38, 0.78 | 0.49 | 0.24, 0.75 | −0.06 | −0.67, 0.55 | 0.37 | 0.12, 0.62 | ||
| 1–2 h/d | 0.89 | 0.65, 1.12 | 1.03 | 0.85, 1.19 | 1.29 | 1.10, 1.48 | 1.44 | 1.19, 1.69 | 1.03 | 0.41, 1.65 | 1.16 | 0.92, 1.40 | ||
| 3–4 h/d | 1.23 | 0.99, 1.47 | 1.50 | 1.33, 1.67 | 1.96 | 1.77, 2.15 | 2.31 | 2.05, 2.57 | 2.11 | 1.49, 2.73 | 1.88 | 1.64, 2.12 | ||
| 5–6 h/d | 1.52 | 1.27, 1.77 | 1.90 | 1.72, 2.08 | 2.58 | 2.38, 2.79 | 3.19 | 2.92, 3.45 | 3.40 | 2.78, 4.01 | 2.59 | 2.35, 2.84 | ||
| 7–8 h/d | 1.55 | 1.27, 1.77 | 2.10 | 1.91, 2.28 | 3.28 | 3.02, 3.54 | 4.16 | 3.87, 4.45 | 4.53 | 3.74, 5.31 | 3.26 | 2.99, 3.54 | ||
| ≥9 h/d | 1.38 | 1.07, 1.69 | 2.26 | 2.06, 2.46 | 3.42 | 3.19, 3.65 | 4.41 | 4.01, 4.81 | 5.36 | 4.52, 6.20 | 3.38 | 3.09, 3.67 | ||
| Model 2 | Intercept | 24.7 | 24.2, 25.2 | 27.2 | 26.8, 27.6 | 30.9 | 30.5, 31.3 | 36.8 | 36.3, 37.4 | 44.4 | 43.2, 45.5 | 32.8 | 32.4, 33.2 | |
| Time | −0.20 | −0.22, −0.17 | −0.03 | −0.05, −0.01 | 0.14 | 0.12, 0.16 | 0.31 | 0.28, 0.34 | 0.44 | 0.40, 0.49 | 0.18 | 0.17, 0.19 | ||
| Television | None | Ref | Ref | Ref | Ref | Ref | Ref | |||||||
| <1 h/d | 0.35 | 0.12, 0.58 | 0.41 | 0.24, 0.59 | 0.56 | 0.33, 0.80 | 0.53 | 0.20, 0.86 | 0.13 | −0.52, 0.78 | 0.38 | 0.14, 0.63 | ||
| 1–2 h/d | 0.86 | 0.65, 1.08 | 0.99 | 0.83, 1.16 | 1.25 | 1.03, 1.47 | 1.44 | 1.11, 1.77 | 1.11 | 0.45, 1.78 | 1.14 | 0.90, 1.38 | ||
| 3–4 h/d | 1.19 | 0.98, 1.40 | 1.44 | 1.28, 1.60 | 1.87 | 1.65, 2.09 | 2.23 | 1.88, 2.57 | 2.08 | 1.41, 2.74 | 1.79 | 1.55, 2.02 | ||
| 5–6 h/d | 1.46 | 1.23, 1.68 | 1.79 | 1.62, 1.97 | 2.38 | 2.16, 2.61 | 2.97 | 2.62, 3.31 | 3.11 | 2.45, 3.78 | 2.38 | 2.14, 2.62 | ||
| 7–8 h/d | 1.48 | 1.20, 1.76 | 1.94 | 1.74, 2.14 | 2.93 | 2.66, 3.21 | 3.69 | 3.29, 4.09 | 4.06 | 3.23, 4.88 | 2.92 | 2.64, 3.19 | ||
| ≥9 h/d | 1.24 | 0.96, 1.52 | 2.07 | 1.87, 2.27 | 3.12 | 2.83 (3.41 | 3.90 | 3.47, 4.34 | 4.53 | 3.52, 5.53 | 3.01 | 2.73, 3.30 | ||
| Model 3 | Intercept | 24.5 | 24.1, 24.9 | 26.9 | 26.5, 27.4 | 30.4 | 29.9, 30.9 | 35.69 | 35.1, 36.3 | 42.03 | 41.0, 43.1 | 32.2 | 31.8, 32.7 | |
| Time | −0.17 | −0.19, −0.15 | −0.01 | −0.03, 0.01 | 0.15 | 0.13, 0.17 | 0.32 | 0.29, 0.35 | 0.46 | 0.42, 0.50 | 0.18 | 0.17, 0.19 | ||
| Television | None | Ref | Ref | Ref | Ref | Ref | Ref | |||||||
| <1 h/d | 0.35 | 0.09, 0.61 | 0.39 | 0.21, 0.57 | 0.57 | 0.39, 0.75 | 0.54 | 0.14, 0.94 | 0.25 | −0.34, 0.85 | 0.42 | 0.17, 0.66 | ||
| 1–2 h/d | 0.87 | 0.63, 1.11 | 0.97 | 0.80, 1.15 | 1.25 | 1.08, 1.42 | 1.45 | 1.04, 1.85 | 1.20 | 0.64, 1.76 | 1.18 | 0.95, 1.42 | ||
| 3–4 h/d | 1.18 | 0.95, 1.42 | 1.41 | 1.23, 1.58 | 1.85 | 1.68, 2.02 | 2.18 | 1.79, 2.57 | 2.07 | 1.53, 2.60 | 1.79 | 1.56, 2.03 | ||
| 5–6 h/d | 1.43 | 1.18, 1.68 | 1.74 | 1.56, 1.91 | 2.33 | 2.14, 2.51 | 2.84 | 2.44, 3.24 | 2.94 | 2.40, 3.48 | 2.32 | 2.08, 2.56 | ||
| 7–8 h/d | 1.44 | 1.15, 1.72 | 1.85 | 1.57, 2.14 | 2.80 | 2.56, 3.04 | 3.51 | 3.08, 3.94 | 3.72 | 3.11, 4.33 | 2.80 | 2.52, 3.07 | ||
| ≥9 h/d | 1.25 | 0.93, 1.57 | 2.00 | 1.76, 2.24 | 2.99 | 2.71, 3.26 | 3.62 | 3.06, 4.17 | 3.98 | 3.31, 4.65 | 2.88 | 2.59, 3.16 | ||
GEE, generalized estimating equation. Data presented are beta coefficients (b) and 95% confidence intervals (95% CI). The intercept is the predicted BMI at baseline for the referent group (ref). The time coefficient is code 0 for baseline and 1 for follow-up and so represents the change in BMI from baseline to follow-up. The sitting/television coefficients represent the difference in BMI for each sitting/television category relative to the referent group. Model 1 adjusted for age, gender, race, education and smoking dose. Model 2 adjusted for covariates in Model 1 plus MVPA, calories and sleep duration. Model 3 adjusted covariates in Model 2 plus sitting time.
Changes in the BMI distribution over time were influenced by time spent sitting at baseline, particularly at the upper percentiles of the BMI distribution (Table 2, model 1). For example, compared to sitting for less than 3 hours per day, sitting for 5–6 hours per day was associated with an additional increase in BMI over time by 0.51 kg/m2 (95% CI: 0.45, 0.57) at the 50th BMI percentile and with an additional increase in BMI over time by 1.11 kg/m2 (95% CI: 0.96, 1.26) at the 90th BMI percentile. In this example, the sitting coefficient at the 50th BMI percentile was smaller than the sitting coefficient at the 90th BMI percentile (−0.60, 95% CI: −0.75, −0.46, p<0.0001). The corresponding mean increase in BMI over time was 0.67 kg/m2 (95% CI: 0.60, 0.73) for 5–6 hours of sitting at baseline relative to less than 3 hours of sitting at baseline (Table 2, GEE model 1).
Changes in the BMI distribution over time were also influenced by time spent watching television at baseline, particularly at the upper tail of the BMI distribution (Table 3, model 1). For example, compared to watching no television, watching 3–4 hours of television per day at baseline was associated with an additional increase in BMI over time by 1.96 kg/m2 (95% CI: 1.77, 2.15) at the 50th BMI percentile and with an additional increase in BMI over time by 2.11 kg/m2 (95% CI: 1.49, 2.73) at the 90th BMI percentile. The corresponding mean increase in BMI over time was 1.88 kg/m2 (95% CI: 1.64, 2.12) for 3–4 hours of television viewing at baseline relative to no television viewing at baseline (Table 3, GEE model 1).
Dose-response relationships were observed between more sitting and more television viewing at baseline and additional increases in BMI over time (Tables 2 and 3). Further, the associations between more baseline sitting time/television viewing and greater increases in BMI over time remained after adjusting for MVPA, caloric intake, and sleep duration (Tables 2 and 3, model 2), and when both television viewing and sitting time were included in the same model (Tables 2 and 3, model 3).
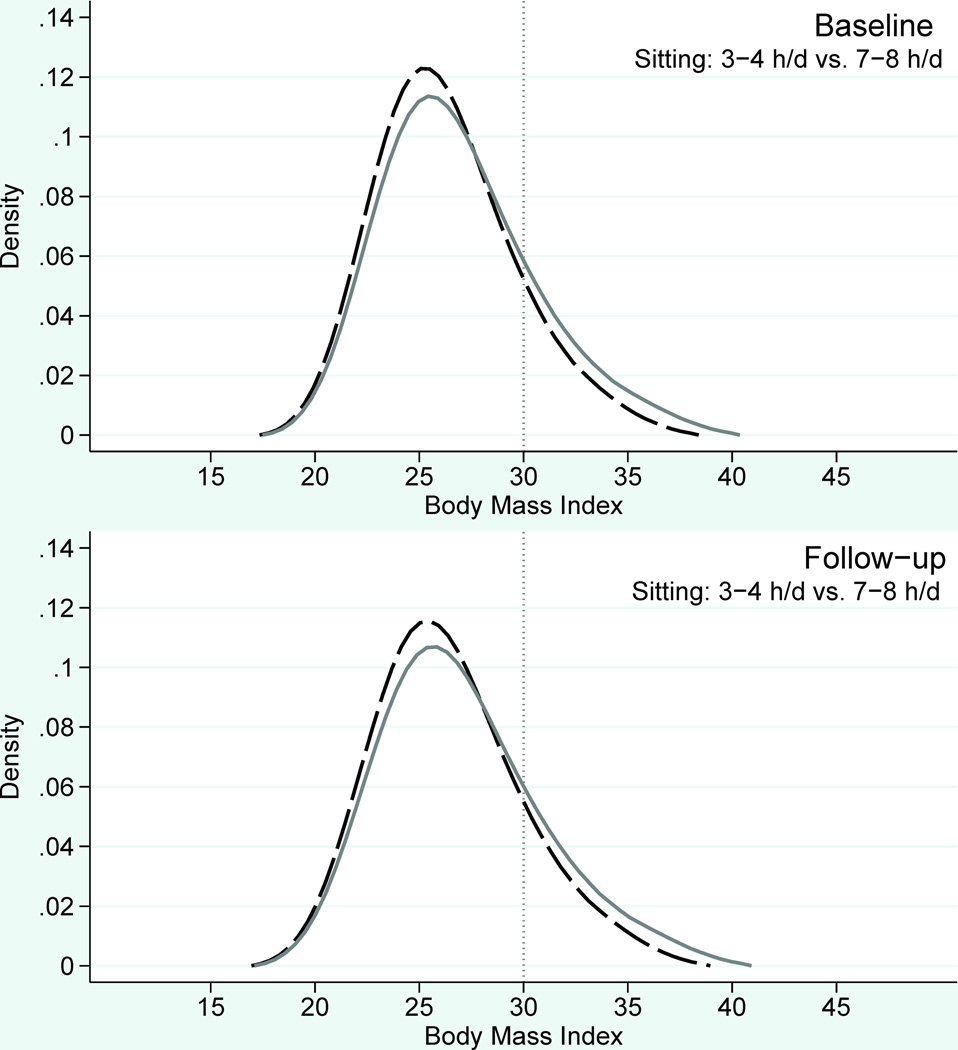
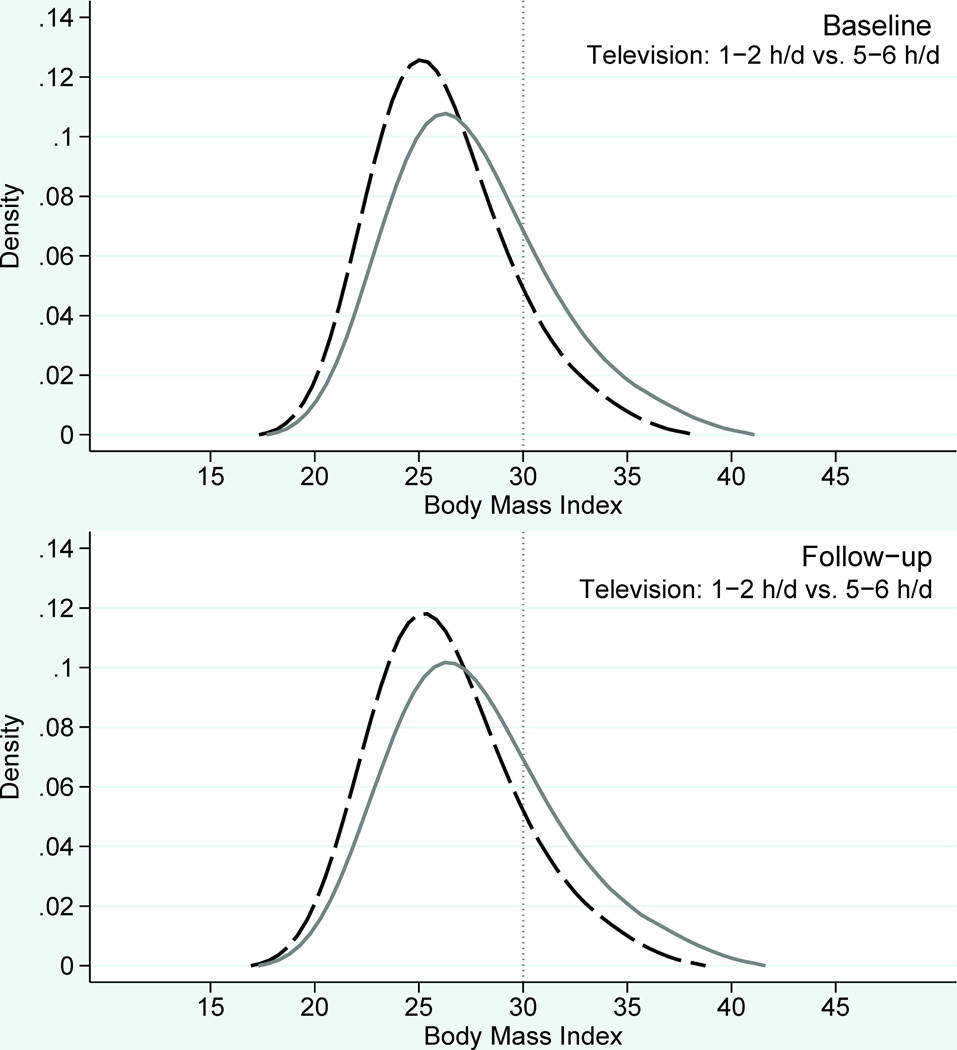
To illustrate the overall study findings BMI distributions are shown in Figure 1. The stronger associations observed between sedentary behavior and BMI at the upper percentiles of the BMI distribution translates to a greater shift to lower BMI values at the upper tail of the BMI distribution with less time spent in sedentary behavior (Figure 1).
Figure 1.
Predicted leftward shift at the upper tail of the BMI distribution to lower BMI values with less time spent sitting (left column) and less time spent watching television (right column) among NIH-AARP Diet and Health Study participants (n=158,436). Baseline corresponds to 1995–1996 and follow-up corresponds to 2004–2006. The solid grey line illustrates the predicted BMI distribution if all participants were seated for 7–8 hours per day (left column) and if all participants watched television for 5–6 hours per day (right column). The dashed black line illustrates the predicted BMI distribution if all participants were seated for 3–4 hours per day (left column) and if all participants watch television for 1–2 hours per day (right column).
Discussion
We sought to determine in a prospective study whether sedentary behavior at baseline was associated with changes in the BMI distribution in adults. We assessed measures of overall sitting time and television viewing and controlled for established obesity risk factors that included MVPA, caloric intake and sleep duration. We present evidence that more time spent in sedentary behavior at baseline was associated with additional increases in BMI over time, especially at the upper percentiles of the BMI distribution, in a dose-response manner. These novel findings add to the growing consensus that reducing time spent in sedentary behavior could help to prevent obesity at the population level.
Previous cross-sectional studies have reported associations between more time spent in sedentary behavior and higher BMI in adults (3, 7, 22, 26, 33, 37). Importantly, those studies cannot establish temporal precedence. Prospective studies have found that more sedentary behavior increases the risk of BMI defined obesity over time, but those studies did not investigate percentiles across the BMI distribution (14, 21). In our longitudinal study, we observed that more time spent in sedentary behavior at baseline was associated with additional increases in BMI over time, and those additional increases were greater at the upper percentiles of the BMI distribution. Therefore, reducing sedentary behavior at the population level could lower the proportion in the population with a BMI at or above 30 kg/m2 by shifting the upper percentiles of the BMI distribution to lower values. This change in the shape of the BMI distribution would have been missed had we only modeled mean BMI changes and indicates that population level reductions in sedentary behavior could be especially beneficial for preventing excessive BMI gains in the upper percentiles of the BMI distribution.
The associations we observed between more sedentary behavior and higher BMI were independent of caloric intake, sleep duration, and MVPA. It is therefore possible that spending too much time in sedentary behavior independently lowers physical activity energy expenditure by displacing light intensity physical activity, potentially leading to a state of positive energy balance and obesity (17, 25). Therefore, substituting time spent in sedentary behavior for light intensity physical activity could increase energy expenditure and reduce BMI (6, 13). Indeed, walking workstations have been shown to increase energy expenditure by 100 kcal per hour compared to when seated at a desk (18), and the use of such workstations has been associated with weight loss (16). In addition, estimated energy expenditure during a one hour television viewing period was 148 kcal per hour when stepping during commercials was allowed, compared to 81 kcal per hour when no stepping and only sitting was allowed (34).
However, when we included both sitting time and television viewing in the same model, both sedentary behaviors remained associated with greater increases in BMI over time. Reduced energy expenditure could still explain the sitting time association, but this may be insufficient to fully explain the television viewing associations with BMI (i.e. reduced energy expenditure while sitting does not fully explain why watching television increases BMI). Television viewing often occurs in the evening prior to going to bed (4), and there is emerging evidence that misalignment between the sleep-wake cycles and circadian body clocks could lead to obesity (29). Further, snacking often occurs during television viewing and eating at night has been associated with obesity, particularly in animal models (11). We do not have data regarding the time of day television viewing and eating occurred and so we cannot directly test these hypotheses. It would be interesting to determine if circadian misalignment partly explains why television viewing associates with adult obesity.
While our data supports the hypothesis that sedentary behavior is associated with greater increases in BMI over time and that there are plausible explanations for our observations, we cannot exclude the possibility of reverse–causality. Two studies have suggested that obesity can lead to an increase in sedentary behavior (8, 27), but these studies have some limitations that should be considered. For example, Ekelund et al. used an objective physiological measure (heart rate (HR) flex) to estimate sedentary behavior and found that: 1) baseline BMI and sedentary behavior were positively correlated, 2) baseline sedentary behavior was unrelated to future BMI, and 3) baseline BMI was associated with future sedentary behavior (8). However, the protocol to determine HR flex and thus sedentary behavior changed between baseline and follow-up. Notably, estimated baseline sedentary behavior (30–34% of waking time) was substantially lower than the follow-up estimate (47–55% of waking time) (8). The baseline estimate was also substantially lower compared to other studies that have objectively estimated sedentary behavior using accelerometers (19, 40). While Ekelund et al. rightly highlighted concerns about reverse-causality, changes in the sedentary behavior measurement methodology between baseline and follow-up makes interpretation of this study challenging (8). Similarly, Pulsford et al. reported evidence that past obesity status predicted more television viewing, but there was an absence of cross-sectional associations between sedentary behavior and BMI in their data making interpretation of this study also challenging (27).
A second possibility that we cannot exclude is that a bi-directional positive feedback loop exists between sedentary behavior and BMI. Indeed, the stronger associations we observed between sedentary behavior and BMI at the upper percentiles of the BMI distribution could be indicative of such a positive feedback relationship. Prospective studies with better measures of sedentary behavior are needed to test this hypothesis and replicate or refute the findings from this and earlier studies.
Strengths of our study include the large sample size and the inclusion of a follow-up measure of BMI. We adjusted for time spent in MVPA, caloric intake and sleep duration, and to the best of our knowledge only one other study involving adults included these three covariates when investigating the association between sedentary behavior and BMI (21). However, these covariates were self-reported and residual confounding may exist. The use of quantile regression allowed for the study of the BMI distribution and the stronger association between sedentary behavior and BMI at the upper percentiles of the BMI distribution would not have been observed had the mean BMI, or BMI categories, been modeled (28). Limitations of our study include the use of self-reported height and weight to calculate BMI. Self-reported BMI and objectively measured BMI are highly correlated (r>0.9) (20), however, replication of our study using objectively measured height and weight and other obesity phenotypes (skinfolds, waist circumference, and fat mass) would help to confirm our findings. We included two self-reported measures of sedentary behavior (sitting time and television viewing), but validity and reliability data for the specific questions used are unavailable. However, there is evidence that study participants are able to report their sitting and television viewing times (2, 12), and Atkin et al. concluded in a review of methods to measure sedentary behavior that single-item questions are suitable for use in health-related epidemiological research (2). Caloric intake was derived from a food frequency questionnaire and underestimation of calories consumed is a potential limitation, especially among obese participants. Our sample comprised of U.S. adults, 50–71 years old at baseline, and most were non-Hispanic white and well educated. It is not known if the same associations would be observed among other populations.
In our sample of adults, spending more time in sedentary behavior at baseline was associated with a greater increase in BMI over time, particularly at the upper percentiles of the BMI distribution. Importantly the associations observed were independent of MVPA, caloric intake, sleep duration. Therefore, public health strategies that target reductions in sedentary behavior could contribute to reducing the prevalence of obesity at the population level.
Acknowledgments
This work is supported by Award Number F32CA162847 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. The results of the present study do not constitute endorsement by ACSM.
Footnotes
Disclosure of Funding: National Institutes of Health (NIH)
Conflict of Interest: None to report
References
- 1.Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332(7549):1080. doi: 10.1136/bmj.332.7549.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atkin AJ, Gorely T, Clemes SA, et al. Methods of Measurement in epidemiology: sedentary Behaviour. Int J Epidemiol. 2012;41(5):1460–1471. doi: 10.1093/ije/dys118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banks E, Lim L, Seubsman SA, Bain C, Sleigh A. Relationship of obesity to physical activity, domestic activities, and sedentary behaviours: cross-sectional findings from a national cohort of over 70,000 Thai adults. BMC Public Health. 2011;11:762. doi: 10.1186/1471-2458-11-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basner M, Dinges DF. Dubious bargain: trading sleep for Leno and Letterman. Sleep. 2009;32(6):747–752. doi: 10.1093/sleep/32.6.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buchinsky M. Estimating the asymptotic covariance matrix for quantile regression models: a Monte Carlo study. Journal of Econometrics. 1995;68:303–338. [Google Scholar]
- 6.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Du H, Bennett D, Li L, et al. Physical activity and sedentary leisure time and their associations with BMI, waist circumference, and percentage body fat in 0.5 million adults: the China Kadoorie Biobank study. Am J Clin Nutr. 2013;97(3):487–496. doi: 10.3945/ajcn.112.046854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ. Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr. 2008;88(3):612–617. doi: 10.1093/ajcn/88.3.612. [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 10.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes (Lond) 1998;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 11.Hatori M, Vollmers C, Zarrinpar A, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15(6):848–860. doi: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults' sedentary time in population-based studies. Am J Prev Med. 2011;41(2):216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 14.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289(14):1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 15.Kaufman A, Augustson EM, Patrick H. Unraveling the Relationship between Smoking and Weight: The Role of Sedentary Behavior. J Obes. 2012;2012:735465. doi: 10.1155/2012/735465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koepp GA, Manohar CU, McCrady-Spitzer SK, et al. Treadmill desks: A 1-year prospective trial. Obesity (Silver Spring) 2013;21(4):705–711. doi: 10.1002/oby.20121. [DOI] [PubMed] [Google Scholar]
- 17.Levine JA, Lanningham-Foster LM, McCrady SK, et al. Interindividual variation in posture allocation: possible role in human obesity. Science. 2005;307(5709):584–586. doi: 10.1126/science.1106561. [DOI] [PubMed] [Google Scholar]
- 18.Levine JA, Miller JM. The energy expenditure of using a "walk-and-work" desk for office workers with obesity. Br J Sports Med. 2007;41(9):558–561. doi: 10.1136/bjsm.2006.032755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAdams MA, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring) 2007;15(1):188–196. doi: 10.1038/oby.2007.504. [DOI] [PubMed] [Google Scholar]
- 21.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mummery WK, Schofield GM, Steele R, Eakin EG, Brown WJ. Occupational sitting time and overweight and obesity in Australian workers. Am J Prev Med. 2005;29(2):91–97. doi: 10.1016/j.amepre.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 23.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pate RR, O'Neill JR, Lobelo F. The evolving definition of "sedentary". Exerc Sport Sci Rev. 2008;36(4):173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 26.Proper KI, Cerin E, Brown WJ, Owen N. Sitting time and socio-economic differences in overweight and obesity. Int J Obes (Lond) 2007;31(1):169–176. doi: 10.1038/sj.ijo.0803357. [DOI] [PubMed] [Google Scholar]
- 27.Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon MM. Sitting behavior and obesity: evidence from the Whitehall II study. Am J Prev Med. 2013;44(2):132–138. doi: 10.1016/j.amepre.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rehkopf DH. Quantile regression for hypothesis testing and hypothesis screening at the dawn of big data. Epidemiology. 2012;23(5):665–667. doi: 10.1097/EDE.0b013e318261f7be. [DOI] [PubMed] [Google Scholar]
- 29.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 30.Schatzkin A, Subar AF, Thompson FE, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions : the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125. doi: 10.1093/aje/154.12.1119. [DOI] [PubMed] [Google Scholar]
- 31.Sedentary Behaviour Research N. Letter to the editor: standardized use of the terms "sedentary" and "sedentary behaviours". Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 32.Sisson SB, Shay CM, Broyles ST, Leyva M. Television-viewing time and dietary quality among U.S. children and adults. Am J Prev Med. 2012;43(2):196–200. doi: 10.1016/j.amepre.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 33.Stamatakis E, Hirani V, Rennie K. Moderate-to-vigorous physical activity and sedentary behaviours in relation to body mass index-defined and waist circumference-defined obesity. Br J Nutr. 2009;101(5):765–773. doi: 10.1017/S0007114508035939. [DOI] [PubMed] [Google Scholar]
- 34.Steeves JA, Thompson DL, Bassett DR., Jr Energy cost of stepping in place while watching television commercials. Med Sci Sports Exer. 2012;44(2):330–335. doi: 10.1249/MSS.0b013e31822d797e. [DOI] [PubMed] [Google Scholar]
- 35.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires : the Eating at America's Table Study. Am J Epidemiol. 2001;154(12):1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 36.Sun Q, van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB. Comparison of dual-energy x-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am J Epidemiol. 2010;172(12):1442–1454. doi: 10.1093/aje/kwq306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thorp AA, Healy GN, Owen N, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004 –2005. Diabetes Care. 2010;33(2):327–334. doi: 10.2337/dc09-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 39.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wijndaele K, Orrow G, Ekelund U, et al. Increasing objectively measured sedentary time increases clustered cardiometabolic risk: a 6 year analysis of the ProActive study. Diabetologia. 2014;57(2):305–312. doi: 10.1007/s00125-013-3102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]