Abstract
Objective
To pilot a psychological intervention adapted for older adults at-risk for suicide.
Design
A focused, uncontrolled, pre-to-post-treatment psychotherapy trial. All eligible participants were offered the study intervention.
Setting
Outpatient mental healthcare provided in the psychiatry department of an academic medical center in a mid-sized Canadian city.
Participants
Seventeen English-speaking adults 60 years or older, at- risk for suicide by virtue of current suicide ideation, death ideation, and/or recent self-injury.
Intervention
A 16-session course of Interpersonal Psychotherapy (IPT) adapted for older adults at-risk for suicide who were receiving medication and/or other standard psychiatric treatment for underlying mood disorders.
Measurements
Participants completed a demographics form, screens for cognitive impairment and alcohol misuse, a semi-structured diagnostic interview, and measures of primary (suicide ideation and death ideation), and secondary study outcomes (depressive symptom severity; social adjustment and support; psychological well-being), and psychotherapy process measures.
Results
Participants experienced significant reductions in suicide ideation, death ideation, and depressive symptom severity, and significant improvement in perceived meaning in life, social adjustment, perceived social support, and other psychological well-being variables.
Conclusions
Study participants experienced enhanced psychological well-being and reduced symptoms of depression and suicide ideation over the course of IPT adapted for older adults at-risk for suicide. Larger, controlled trials are needed to further evaluate the impact of this novel intervention and to test methods for translating and integrating focused interventions into standard clinical care with at-risk older adults.
Keywords: Suicide, suicide ideation, psychotherapy, treatment, Interpersonal Psychotherapy, IPT, psychological well-being, meaning in life
Older adults have high rates of suicide [1,2], necessitating focused clinical risk assessment and intervention [3,4]. Older adults are amenable to and respond well to psychological interventions [5-8]; however, only one trial of psychotherapy to date has been conducted exclusively targeting suicidal older adults [9]. We specifically conducted a small focused trial of Interpersonal Psychotherapy (IPT) adapted for older adults at-risk for suicide by virtue of expression of current suicide ideation, death ideation, or recent self-injury. Preliminary findings suggested that this intervention is feasible, tolerable, and safe, and has a positive impact on therapeutic change [9]. Significant reductions were observed in suicide ideation, death ideation, and depressive symptom severity [9]. We now extend and expand upon these preliminary findings by reporting complete study findings on primary (suicide ideation and death ideation) and secondary (depressive symptom severity) outcomes and therapeutic process variables (working alliance and treatment satisfaction) across pre- to post-treatment assessments, and investigating the stability of change over a 6-month follow-up period.
We have adapted IPT for the treatment of at-risk older adults, given empirical findings supporting its efficacy as an active or maintenance treatment for depression and in enhancing social adjustment among older adults [7-11], negative findings notwithstanding [12]. Findings from a secondary analysis of data from three treatment studies of late-life depression in mental healthcare settings [13,14], and from the multi-site PROSPECT study [15,16] demonstrated significant reduction or resolution of suicide ideation with standard IPT and/or antidepressants. Resolution of suicide ideation was slower and treatment less effective for individuals with a history of suicidal behavior or more severe suicide ideation, necessitating adaptation of IPT for at-risk individuals [13,16].
IPT is a conceptually relevant intervention for suicidal older adults, given the salience of interpersonal problems, perceived social support deficits, and difficulty adjusting to life transitions in the onset, exacerbation, and potential resolution of suicide risk in later life [17-19]. Theory and research suggest that attention to suicide risk factors may be insufficient to identify and intervene effectively with at-risk individuals. Following the call for a complementary focus on resiliency [20], we demonstrated that older adults expressing greater perceived meaning in life (MIL) and life satisfaction reported significantly less suicide ideation [21]. The positive effect of MIL was most robust at higher levels of depressive symptom severity [22]. IPT problem areas regarding death, losses, and transitions are consistent with existential concerns that may engender perceptions of meaninglessness [21-23]. We thus adapted IPT from existing treatment manuals [24,25] incorporating lessons learned from reports of suicide during psychotherapy [26,27], by making suicide a central focus of clinical discourse and incorporating safety precautions and ongoing surveillance of suicide risk and resiliency factors, including MIL and additional psychological well-being variables [9]. We further sought to individually tailor treatment to participants’ emotional and existential concerns, helping them attend to remaining sources of MIL, emphasizing enhancing, rebuilding, or cultivating meaningful relationships. Given that suicide ideation can wax and wane [13,28] and that risk for suicide is high following changes or discontinuation in depression care [29-31], we additionally investigated maintenance of therapeutic change over a 6-month follow-up period.
Methods
Procedures
Potential study participants were referred for eligibility assessment by clinical staff in inpatient, outpatient, and outreach geriatric psychiatry, consultation liaison, and medical services in London, Ontario, a Canadian city with a population over 350,000, 18% over 60 years of age [32]. Clinicians facilitated introductions to potential participants, consistent with a study protocol approved by The University of Western Ontario's Health Sciences Research Ethics Board. Eligible individuals were 60 years or older, spoke English, and reported current suicide ideation and/or death ideation to a referring clinician or had engaged in clinically-documented self-injury within the prior two years. Exclusion criteria included moderate to severe cognitive impairment (< 23 on the Mini-Mental State Examination or MMSE) [33] and/or advanced-stage dementia, a lifetime history of schizophrenia (SCID-I) [34], and an active substance misuse disorder that commenced prior to age 30 (SCID-I, and the Alcohol Use Identification Test or AUDIT) [35]. Presence of personality disorders was assessed with the SCID-II [36]; however, having a personality disorder was not a study exclusion criterion. Eligible participants had to refrain from additional psychotherapy during the trial, but were encouraged to continue psychotropic medication and case management visits with other mental healthcare provider(s). Assessment and treatment sessions took place in an academic medical center; participants recruited from inpatient settings could complete initial measures in-hospital, and those with transportation or mobility limitations could be assessed at home. The P.I. administered assessment measures and delivered the intervention, consistent with the pilot nature of this treatment adaptation study.
Assessments
Eligible participants completed a battery of measures as part of a comprehensive assessment of late-life suicide risk factors [3], including suicide ideation, death ideation, and depressive symptom severity at pre-, mid- (8 weeks), and post-treatment assessments (16 weeks). Participants later completed three- (n=16) and six-month follow-up assessments (n=9), investigating maintenance of treatment gains. Participants completed measures of therapeutic process variables, assessing therapeutic alliance and treatment satisfaction, at mid-treatment, post-treatment, and follow-up assessments. All measures were presented orally in order to standardize administration, given participant variability in vision, motor functioning, and comprehension. Assessment sessions lasted 45-90 minutes, on average. Participants were offered frequent breaks or multiple sittings, monitored for signs of distress, and provided with support and the opportunity to discontinue the assessment, if desired. Participants were reimbursed for their time and travel costs and treatment was provided free of charge, in order to reduce barriers to care and to study participation.
Safety Protocol
Safety concerns are paramount in research and clinical practice with individuals at-risk for suicide. Participants who expressed suicide ideation in session were helped to identify problems that contributed to suicide risk, and provided with emotional support and validation and assistance in making safer choices than engaging in suicidal behavior. When a participant revealed an imminent risk for self-harm, the therapy session shifted to focus on risk reduction and safety planning, and if risk remained elevated, the therapist accompanied the participant to emergency mental health services. This only occurred twice over the course of the study and in both cases facilitated enhanced care. All participants were offered the adapted intervention, precluding risk associated with randomization of suicidal individuals to a wait-list control condition [37]. Periodic feedback was provided to participants’ referral sources and potentially to other clinicians involved in the participant's care in order to increase vigilance to suicide risk, and recognizing the importance of communication between providers in decreasing suicide risk [26]. Pragmatic suggestions for means restriction (e.g., locking away pills or weapons) were provided to family members and/or other care-providers of participants at heightened risk for impulsive self-injury. IPT participants were provided with 24/7 access to the study therapist by cellular phone if experiencing heightened distress, severe suicide ideation, and/or if imminent self-harm was evident. Participants found this “lifeline” supportive and did not misuse it [9].
Intervention
Participants were offered a course of 16 once-weekly 50-60 minute sessions of outpatient IPT adapted for older adults at-risk for suicide [9]. The study therapist integrated the participant's suicide risk and resiliency factors into interpersonally-informed individualized case conceptualizations, a process not explicitly described in standard IPT manuals [7,25]. Central to psychotherapeutic intervention with suicidal individuals is the amelioration of intense psychological pain [38,39]. Using core IPT techniques of interpersonal incident analysis and communication analysis, participants were helped to clarify factors contributing to their psychological pain and to improve the expression of their interpersonal needs and help alleviate despair. Feelings of emptiness, worthlessness, hopelessness, and meaninglessness are common among suicidal older adults [21,23,40]. Opportunities were thus identified for enhancing social connections, engaging in meaningful activities, and reducing exposure to painful, invalidating, or self-defeating interpersonal interactions. Optional conjoint sessions were encouraged where appropriate. During the termination phase of treatment, participants were helped to focus on continuing to develop interpersonal relationships and meaningful post-therapy pursuits and to elicit social support and/or professional assistance when at-risk. Progress made in improving relationships and in reducing suicide ideation was also reviewed, as was the potential need for on-going care. Psychotherapy sessions were videotaped for review by study investigators, consistent with the aims of this treatment adaptation study. Session videotapes could also be reviewed by participants upon request. Given the benefit of on-going care for suicidal individuals and of continuation and maintenance IPT for depressed older adults [10,41], participants could request post-treatment IPT on an as-needed (booster), reduced frequency (maintenance), or weekly basis (continuation sessions).
Sample
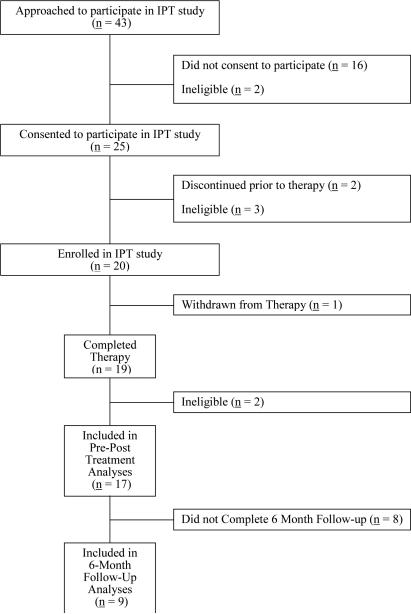
Forty-three individuals were referred for potential study participation over a two-and-a-half-year period; 25 met initial eligibility criteria and provided informed consent (see Figure). Five individuals were excluded who did not meet study inclusion criteria or opted out of the study prior to initiating psychotherapy. Data were removed for three participants who had begun a course of IPT yet no longer met study inclusion criteria. The most common reasons for exclusion from this study were cognitive impairment and alcohol misuse. We thus report pre-to-post-treatment data for 17 participants.
Figure.
Patient Recruitment Flowchart
Measures
Primary Outcome Measures
Suicide ideation was assessed with the Geriatric Suicide Ideation Scale (GSIS) [40], a 31-item, 5-point Likert-scored, multidimensional measure of late-life suicide ideation, with component subscales assessing Suicide Ideation, Death Ideation, Loss of Personal and Social Worth, and Perceived Meaning in Life (reverse-coded). The GSIS has demonstrated strong internal consistency for total (α=.93) and subscale scores (α=.82-.84), 1-2 month test-retest reliability (Pearson's r=.86 for the total scale and .75-.78 for the subscales, p<0.001; n=32), criterion validity differentiating mental health patients from non-patients, convergent validity with depression and hopelessness, and non-convergence with life satisfaction and psychological well-being [21,40,42-44]. The GSIS demonstrated strong internal consistency at this study's eligibility assessment for Total scores (α=.95; n=17), and Suicide Ideation (α=.88), Death Ideation (α=.90), Loss of Personal and Social Worth (α=.81), and Perceived Meaning in Life subscales (α=.90).
Secondary Outcome Measures
Depression symptom severity was assessed with a 24-item version of the clinician-rated Hamilton Rating Scale for Depression (Ham-D) [45,46] and the Center for Epidemiologic Studies Depression scale-Revised (CESD-R) [47], a 20-item self-report measure of presence and severity of depressive symptoms over the past two weeks. Internal consistency was high at this study's pre-treatment assessment for the Ham-D (α=.84) and CESD-R (α=.90).
Psychological well-being was assessed with Ryff's [48] 54-item multidimensional Psychological Well-Being scale (PWB), a 6-point Likert-scored measure with strong psychometric properties among middle-aged and older adults [49-51], including significant association with suicide ideation [21,40]. We report internal consistency for the present sample at pre-treatment assessment for PWB totals (α=.89; n=16) and 9-item Autonomy (α=.58; n=17), Personal Growth (α=.79; n=17), Self-Acceptance (α=.81; n=17), Environmental Mastery (α=.65; n=17), Positive Relations with Others (α=.82; n=16), and Purpose in Life subscales (α=.74; n=17).
Social functioning was assessed with the Social Adjustment Scale-Self-Report (SAS-SR) [52], a 54-item, 5-point measure of role performance, interpersonal friction, relations, and satisfaction in 6 areas: work for pay, housework, or student activities; social and leisure activities; and relations with one's extended family, partner, children, and/or family unit. Participants completed 1 of 3 sections pertaining to role activities, and up to 5 sections pertaining to their interpersonal relationships, as relevant. We report T-scores for participant SAS-SR totals and relevant subscales. Higher scores reflect poorer social functioning.
Social support was assessed with the 23-item Duke Social Support Index (DSSI) [53], a multidimensional self-report measure assessing Social Interaction (SI; 4 items), Perceived Social Support (PSS; 7 items), and Instrumental Support (ISS; 12 items). We assessed the internal consistency of the SI (α=.61), PSS (α=.70), and IS subscales (α=.78) at this study's pre-treatment assessment.
Psychotherapy Process Measures
Strength of the therapeutic alliance was assessed with the 36-item Working Alliance Inventory (WAI) [54]. Higher scores have been associated with improvement in brief psychotherapy [55]. The WAI had high internal consistency for Total scores (α=.97; n=15), and for Task (α=.93; n=17), Goal (α=.94; n=17), and Bond subscales (α=.86; n=15) at this study's mid-treatment assessment, which took place between sessions 8 and 9.
Treatment satisfaction was assessed with an internally consistent (α=.82 at this study's mid-treatment assessment; n=17) 10-item Treatment Satisfaction Survey, modified for the present study from a clinical survey of client satisfaction with mental healthcare.
Statistical Analyses
Descriptive statistics were computed for demographic and clinical variables, and presented as means and standard deviations for continuous variables and counts and percentages for categorical variables (see Table 1). Pre-to-post-treatment clinical change on primary and secondary study outcomes was assessed using paired-sample t-tests (see Tables 2 and 3), as was maintenance of treatment gains in suicide ideation from post-treatment to 6-month follow-up (see Table 4). Effect sizes of clinical change scores were computed using Hedges’ g, an unbiased estimator of effect size, using a pooled standard deviation of pre- and post-treatment scores. Measures of effect size were computed using Meta-Analysis 5.3 [56]; all other analyses were computed using SPSS version 20.0 for Windows, with the Type I error rate set at α=0.05, two-tailed.
Table 1.
Characteristics of Study Participants at Eligibility Assessment (N=17)
| Variable | M | SD | Range | N |
|---|---|---|---|---|
| Age | 70.1 | 5.4 | 60 – 84 | 17 |
| Number of Children | 3.0 | 1.5 | 0 – 6 | 17 |
| Number of Grandchildren | 4.0 | 3.4 | 0 – 13 | 17 |
| Health Rating | 4.2 | 1.4 | 2 – 6.5 | 17 |
| MMSE | 28.7 | 1.8 | 24 – 30 | 17 |
| AUDIT | 3.1 | 5.2 | 0 – 21 | 17 |
| Variable | N | % |
|---|---|---|
| Sex | ||
| Men | 8 | 47 |
| Women | 9 | 53 |
| Birthplace | ||
| North America | 14 | 82 |
| Europe/Australasia | 3 | 18 |
| Marital Status | ||
| Widowed | 3 | 18 |
| Married | 10 | 59 |
| Separated or Divorced | 4 | 24 |
| Currently in Romantic Relationship | ||
| Yes | 12 | 71 |
| Lives Alone | ||
| Yes | 5 | 29 |
| Education | ||
| Grade School | 3 | 18 |
| Some High School | 2 | 12 |
| College or Trade School | 5 | 29 |
| University | 2 | 12 |
| Graduate School | 4 | 24 |
| Religious Denomination | ||
| Protestant | 9 | 53 |
| Catholic | 6 | 35 |
| Do you consider yourself a religious person? | ||
| Yes | 12 | 71 |
| Employment Status | ||
| Retired | 15 | 88 |
| Referral Source | ||
| Geriatric Mental Health Provider | 11 | 65 |
| Geriatric Consultation-Liaison Team | 2 | 12 |
| Geriatric Medicine Provider | 4 | 24 |
| Axis I Mood Disorder, Lifetime | 17 | 100 |
| Major Depressive Disorder, Single Episode-Active | 2 | 12 |
| Major Depressive Disorder, Recurrent | 14 | 82 |
| Active | 11 | |
| Other Mood Disorder | 5 | 30 |
| Anxiety Disorder, Current | 14 | 82 |
| Active Axis I Mood Disorder and Axis I Comorbidity | 14 | 82 |
| Axis II Diagnoses | ||
| Present | 7 | 41 |
| Absent/Could Not Assess | 10 | 59 |
Note: Other Mood Disorder comprised Bipolar Affective Disorder and Dysthymic Disorder.
Table 2.
Paired-Sample Statistics on Primary and Secondary Clinical Outcomes (N = 17)
| Severity of Suicide Ideation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Treatment | Post-Treatment | |||||||||
| Variable | M | SD | M | SD | |Δ| | SE | 95% CI | |t|* | p | |g| |
| GSIS-Total | 83.2 | 22.2 | 71.9 | 22.0 | 11.2 | 3.2 | 4.4 to 18.1 | 3.49 | 0.003 | 0.50 |
| GSIS-SI | 25.1 | 7.0 | 22.2 | 7.8 | 2.9 | 1.3 | 0.1 to 5.7 | 2.20 | 0.043 | 0.38 |
| GSIS-DI | 14.2 | 5.9 | 12.0 | 4.7 | 2.2 | 1.0 | 0.1 to 4.4 | 2.24 | 0.040 | 0.40 |
| GSIS-LOSS | 21.2 | 4.9 | 18.0 | 6.0 | 3.2 | 1.0 | 1.2 to 5.3 | 3.37 | 0.004 | 0.57 |
| GSIS-MIL | 19.8 | 6.9 | 16.9 | 6.0 | 2.8 | 1.0 | 0.7 to 5.0 | 2.76 | 0.014 | 0.44 |
| Depression Symptom Severity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Treatment | Post-Treatment | |||||||||
| Variable | M | SD | M | SD | |Δ| | SE | 95% CI | |t| | p | |g| |
| HAMD | 23.8 | 9.2 | 15.2 | 9.7 | 8.6 | 2.2 | 3.9 to 13.3 | 3.84 | 0.001 | 0.89 |
| CESD-R | 23.6 | 13.7 | 14.1 | 14.5 | 9.6 | 2.5 | 4.3 to 14.8 | 3.88 | 0.001 | 0.66 |
df = 16
Note: |Δ| = absolute value of the mean change score; SE=Standard Error for the absolute mean change score; 95% CI=95% Confidence Interval around the absolute mean change score; |t| = absolute value of the t-score; |g| = absolute value of Hedges’ unbiased estimator of effect size; GSIS=Geriatric Suicide Ideation Scale; GSIS-TOT=GSIS Totals; GSIS-SI=GSIS Suicide Ideation subscale; GSIS-DI=GSIS Death Ideation subscale; GSIS-LOSS=GSIS Loss of Personal and Social Worth subscale; GSIS-MIL=GSIS Perceived Meaning in Life subscale; HAMD=Hamilton Rating Scale for Depression; CESD-R=Center for Epidemiologic Studies-Depression scale-Revised.
Table 3.
Paired-Sample Statistics on Secondary Study Outcomes of Psychological Well-Being (N=17).
| Pre-Tx | Post-Tx | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | |Δ| | SE | 95% CI | |t|* | p | |g| |
| SAS-TOT | 66.4 | (14.1) | 55.1 | (10.8) | 11.4 | 2.8 | 5.5 to 17.2 | 4.12 | 0.001 | 0.88 |
| SAS-WRa | 67.4 | (21.8) | 61.5 | (19.9) | 5.9 | 3.0 | −0.7 to 12.5 | 1.96 | 0.074 | 0.27 |
| SAS-SL | 59.5 | (15.1) | 50.2 | (10.6) | 9.3 | 2.7 | 3.6 to 15.0 | 3.43 | 0.003 | 0.70 |
| SAS-EF | 61.1 | (12.0) | 53.9 | (11.3) | 7.2 | 2.2 | 2.6 to 11.9 | 3.31 | 0.004 | 0.60 |
| SAS-PRb | 68.8 | (14.4) | 59.0 | (15.8) | 9.8 | 4.1 | 0.2 to 19.3 | 2.36 | 0.046 | 0.62 |
| SAS-FU | 59.2 | (16.8) | 50.5 | ( 8.0) | 8.7 | 3.9 | 0.5 to 16.9 | 2.26 | 0.038 | 0.65 |
| Duke-SI | 7.9 | ( 1.9) | 8.9 | ( 1.5) | 1.1 | 0.5 | − 2.1 to − 0.0 | −2.13 | 0.049 | 0.57 |
| Duke-PSS | 17.1 | ( 3.0) | 18.5 | ( 2.6) | 1.4 | 0.5 | − 2.5 to − 0.4 | −2.86 | 0.011 | 0.49 |
| Duke-IS | 19.6 | ( 2.9) | 21.4 | ( 3.9) | 1.8 | 0.9 | − 3.8 to 0.2 | −1.92 | 0.072 | 0.51 |
| PWB-TOT | 210.8 | (26.9) | 217.9 | (39.5) | 7.1 | 8.4 | −24.8 to 10.6 | 0.85 | 0.407 | 0.21 |
| PWB-EMc | 33.9 | ( 6.3) | 37.2 | ( 6.3) | 3.3 | 0.9 | − 5.3 to − 1.3 | 3.55 | 0.003 | 0.51 |
| PWB-SAc | 30.3 | ( 7.8) | 33.7 | ( 7.5) | 3.4 | 1.1 | − 5.7 to 1.1 | 3.18 | 0.007 | 0.43 |
| PWB-PRc | 38.6 | ( 7.3) | 40.4 | ( 6.2) | 1.8 | 1.1 | − 4.1 to 0.5 | 1.71 | 0.109 | 0.26 |
| PWB-PGc | 36.8 | ( 7.6) | 39.7 | ( 5.8) | 2.9 | 1.6 | − 6.2 to 0.5 | 1.83 | 0.088 | 0.42 |
| PWB-AUTc | 35.9 | ( 5.6) | 40.1 | ( 6.4) | 4.3 | 1.0 | − 6.4 to − 2.2 | 4.34 | 0.001 | 0.68 |
| PWB-PILc | 35.1 | ( 7.0) | 37.5 | ( 6.4) | 2.4 | 1.2 | − 4.9 to 0.1 | 2.06 | 0.059 | 0.35 |
df = 16, unless stated otherwise.
n = 13, (df = 12)
n = 9, (df = 8)
n = 15, (df = 14)
Note: Pre-Tx=Pre-Treatment scores; Post-Tx=Post-treatment scores; |Δ| = absolute value of the mean change score; SE=Standard Error for the absolute mean change score; 95% CI=95% Confidence Interval around the absolute mean change score; |t| = absolute value of the t-score; |g| = absolute value of Hedges’ unbiased estimator of effect size; SAS=Social Adjustment Scale Self-Report T-scores; SAS-TOT=SAS Totals; SAS-WR=SAS Work Role subscale; SAS-SL=SAS Social and Leisure subscale; SAS-EF=SAS External Family Relations subscale; SAS-PR=SAS Primary Relationship subscale; SAS-FU=SAS Family Unit subscale; Duke=Duke Social Support Index; Duke-SI=Duke Social Interactions subscale; Duke-PSS=Duke Perceived Social Support subscale; Duke-IS=Duke Instrumental Support subscale; PWB=Ryff's Multidimensional Measure of Psychological Well-Being; PWB-TOT=PWB Totals; PWB-EM=PWB Environmental Mastery subscale; PWB-SA=PWB Self-Acceptance subscale; PWB-PR=PWB Positive Relations with Others subscale; PWB-PG=PWB Personal Growth subscale; PWB-AUT=PWB Autonomy subscale; PWB-PIL=PWB Purpose in Life subscale.
Table 4.
Paired-Sample Statistics Assessing Maintenance of Treatment Gains for Suicide Ideation (N = 9)
| Post-Tx | 6-Mos F/U | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | |Δ| | SE | 95% CI | |t|* | p | |g| |
| GSIS-Total | 75.0 | (27.6) | 61.4 | (22.6) | 13.6 | 4.4 | 3.5 to 23.6 | 3.11 | 0.014 | 0.51 |
| GSIS-SI | 24.4 | ( 9.2) | 19.8 | ( 7.0) | 4.7 | 1.6 | 0.9 to 8.4 | 2.89 | 0.020 | 0.54 |
| GSIS-DI | 12.9 | ( 6.1) | 10.3 | ( 5.6) | 2.6 | 1.0 | 0.2 to 4.9 | 2.48 | 0.038 | 0.42 |
| GSIS-LOSS | 18.7 | ( 7.5) | 15.8 | ( 6.7) | 2.9 | 2.0 | −1.6 to 7.4 | 1.48 | 0.178 | 0.39 |
| GSIS-MIL | 16.9 | ( 7.5) | 14.0 | ( 5.1) | 2.9 | 1.1 | 0.4 to 5.3 | 2.73 | 0.026 | 0.43 |
df = 8.
Note: Post-Tx=Post-treatment scores; 6-Mos F/U=Six-Month Follow-Up Assessment scores; |Δ| = absolute value of the mean change score; SE=Standard Error for the absolute mean change score; 95% CI=95% Confidence Interval around the absolute mean change score; |t| = absolute value of the t-score; |g| = absolute value of Hedges’ unbiased estimator of effect size; GSIS=Geriatric Suicide Ideation Scale; GSIS-TOT=GSIS Totals; GSIS-SI=GSIS Suicide Ideation subscale; GSIS-DI=GSIS Death Ideation subscale; GSIS-LOSS=GSIS Loss of Personal and Social Worth subscale; GSIS-MIL=GSIS Perceived Meaning in Life subscale.
Results
Sample Characteristics at Study Eligibility Assessment
Seventeen older adults completed a course of adapted IPT (see Table 1). A majority (65%) reported health ratings in the “good” to “extremely good” range on a 7-point perceived health scale (M=4.2, SD=1.4). The most common physical comorbidities reported on a brief medical history data form were arthritis (71%) and hypertension (47%).
All study participants had a history of mood disorder, including 16 (94%) with Major Depressive Disorder, and 14 (82%) with an active mood disorder and active Axis I co-morbidity. Seven (41%) had an Axis II diagnosis. Participant suicide ideation ratings were approximately 0.5-1 standard deviation above the mean for mental health patients in the GSIS scale development sample [40], reflecting this sample's elevated suicide risk. Six participants reported having ever attempted suicide (41%) on a suicide behavior profile we have used in our previous research [57], and two others reported having aborted a suicide attempt. One participant reported 5 lifetime suicide attempts, and two were inconclusive as to the number of times they had tried to kill themselves. Six reported having a current suicide plan.
Pre-to-Post-Treatment Change
Outcomes analyses indicated a significant reduction in participant suicide ideation from pre-to-post-treatment assessment (see Table 2). GSIS total scores decreased by an average of 11.2 points per participant, yielding an effect size (g) of 0.50. Significant pre-to-post-treatment reductions were also observed for the GSIS Suicide Ideation, Death Ideation, Loss of Personal and Social Worth, and the reverse-coded GSIS Perceived Meaning in Life scores.
Findings indicated a significant pre-to-post-treatment reduction in participant depressive symptom severity on the clinician-rated Hamilton and self-rated CESD-R scales. Depression scores were nearly halved between pre- and post-treatment assessments (see Table 2).
Table 3 reveals significant increases in participant social adjustment (SAS-SR), enjoyment of social and leisure activities, improved relations with a significant other and with one's family unit and extended family. Improvement in participants’ work relations did not reach statistical significance; however, fewer participants completed this section than the others, likely due to retirement. We also detected a significant improvement in participant social interactions and in perceived social support on the Duke Social Support Index, but not in instrumental support. Changes in participants’ overall psychological well-being scores (PWB) and positive relations with others were not significant; however, participants experienced a significant improvement in environmental mastery, self-acceptance, and autonomy, and marginal improvement in personal growth and purpose in life. Taken together with findings of enhanced MIL on the GSIS, these findings suggest an improvement in participant well-being over the course of treatment.
Therapeutic Process
Analyses of post-treatment therapeutic process data revealed a strong therapeutic alliance; participants reported an average score of 6.1 out of a total possible 7 points on the Working Alliance Inventory (WAI; SD=0.7; Range: 5.0-7.0), and similar high scores on the WAI Task (M=6.1, SD=0.8; Range: 4.5-7.0), Bond (M=6.2, SD=0.6; Range: 5.1-7.0), and Goal subscales (M=5.9, SD=0.7; Range: 4.8-7.0). Participants further reported high treatment satisfaction at post-treatment (M=47.7, SD=2.5; Range: 41.0-50.0).
Longer Term Outcomes
We next assessed maintenance of participant treatment gains from post-treatment (i.e., after the 16th session) to 6-month follow-up assessments (see Table 4). Nine individuals completed this assessment; the remainder was lost to follow-up. Findings suggested a further significant reduction in suicide ideation over the six-month follow-up period for GSIS totals and for Suicide Ideation, Death Ideation, and Perceived Meaning in Life subscales. Further reduction in GSIS Loss of Personal and Social Worth scores did not reach statistical significance.
Discussion
The purpose of the present study was to assess therapeutic change and maintenance of treatment gains in suicide ideation, depressive symptom severity, and psychological well-being among participants in a 16-week course of IPT adapted for older adults at-risk for suicide. We extended the promising preliminary findings of our small trial of adapted IPT [9], demonstrating significant reduction in suicide ideation and depressive symptom severity and improvement in meaning in life, social adjustment, and additional psychological well-being variables over the course of treatment and extending over a 6-month period of follow-up.
Participants endorsed a substantial reduction in suicide ideation across all dimensions of our primary outcome measure. Normative data from the scale's development study demonstrated an 8-12 point difference in GSIS totals between psychiatric and medical patients and between medical patients and community-residing older adults [40], supporting the clinical significance of the 11-point reduction in GSIS scores observed among the current trial's participants. Study participants specifically endorsed reduction in the presence or severity of thoughts of suicide and the wish to die, factors conceptually [58] and empirically associated with risk for death by suicide [59]. Participants additionally endorsed a significant reduction in a sense of having lost one's personal and social worth, reflecting enhanced mental health and well-being in the context of age-related life transitions and decreased burden, a variable significantly associated with suicide risk in later life [23,42]. Significant improvement in perceptions of meaning in life, an existential variable negatively associated with depression, hopelessness, suicide ideation, and the wish to hasten death [21,60,61], and positively associated with psychological well-being and longevity [22,62-64], further attests to the potential benefit of adapted IPT for at-risk older adults.
Despite a reduction in suicide ideation over the course of this intervention, participants’ post-treatment GSIS totals (M=71.9, SD=22.0) were within range for mental health patients in the GSIS scale development sample (M=67.4, SD=13.8; [40]), attesting to this sample's extreme initial suicide ideation ratings and supporting the need for on-going treatment for those with residual suicide ideation. Six-month follow-up data indicated significant additional reduction in suicide ideation scores beyond the 16-session course of IPT, suggesting maintenance or continued treatment gains associated with adapted IPT. This conclusion must be tempered by our small sample size and by participant attrition.
Study participants experienced significant reduction in depressive symptom severity, yielding moderate to large treatment effects attesting to an antidepressant property of adapted IPT. We used multiple measures of depressive symptom severity, given differences in reporting style associated with self- versus clinician-ratings of depressive symptoms among older adults [65]. Clinician ratings of significant improvement in participant depressive symptoms provide additional credence to the self-report data. All study participants met diagnostic criteria for a mood disorder and were receiving treatment with psychotropic medication; hence study findings reflect the potential added benefit of adapted IPT beyond standard clinical treatment of late-life depression. Research supports associations between depressive symptom severity and older adult suicide ideation [40,42,66] and death by suicide [67,68], further suggesting the clinical relevance of these findings.
Most depressed older adults do not die by suicide, attesting to the need to better understand and seek to enhance psychological resiliency, so as to improve psychological well-being and decrease suicide risk. A secondary goal of this study was thus to assess potential therapeutic change in perceived social support and meaning in life, factors shown to be negatively associated with suicide risk among older adults [18,21,60]. Participants endorsed significant improvement in social adjustment, perceived meaning in life, and additional psychological well-being variables, including self-acceptance, perceived environmental mastery, and autonomy. Participants endorsed significant enhancement of perceived social support and social interactions, suggesting that treatment effectively increased both the quantity and subjective quality of their social relations.
The present study comprises a small initial pre-to-post-treatment pilot study, necessitating extension to a larger sample. We had not initially anticipated finding significant changes in study outcomes over the course of this trial given limitations associated with conducting parametric analyses with small sample sizes. Nevertheless, as a “proof-of-concept,” this study is not without limitations. Our primary study hypothesis was confirmed, as suicide ideation scores decreased significantly over the course of this trial; however, inclusion of multiple repeated-measures comparisons likely increased the Family-wise error rate in our analyses. The study therapist recruited and assessed the study participants; this lack of blinding and potential for demand characteristics should be addressed in future research. Given this study's promising findings, a randomized trial is warranted, comparing adapted IPT to an enhanced Care As Usual control group, in order to assess specific effects of the study intervention as compared with non-specific treatment effects associated with increased attention and support. A larger trial would further enable investigation of potential demographic and clinical moderators of treatment outcome. Given the movement in many Western countries towards incorporating less highly-trained clinicians into frontline care, it would also be useful to determine if clinicians other than doctoral level psychologists or psychiatrists could implement with fidelity [69] this adaptation of IPT for older adults at-risk for suicide.
Study findings support the potential effectiveness of adapted IPT in reducing suicide ideation, death ideation, and depressive symptom severity, and enhancing MIL and psychological well-being among at-risk older adults. These positive findings suggest that IPT may be an effective treatment option for at-risk older adults and may ultimately help reduce suicide risk in this high-risk group. Given promising findings supporting community outreach [70-72] and collaborative care trials in identifying and reducing or resolving depression, suicide ideation, and mortality among older adults [73,74], and a typical lengthy delay in translating promising research findings into clinical services [75], research is needed investigating the translation and integration of focused interventions targeting at-risk older adults into frontline healthcare settings.
ACKNOWLEDGEMENTS
Work on this study was funded in part by an American Foundation for Suicide Prevention (AFSP) Young Investigator award (MJH), an AFSP Pfizer research travel award (MJH), a Canadian Institutes for Health Research (MJH) New Investigator Award through the Institute of Aging and Institute of Gender and Health (MJH), and an Ontario Ministry of Research and Innovation Early Research Award (MJH), and United States Public Health Service grant K24MH072712 (PRD). We appreciate the assistance of colleagues who referred potential study participants, and of study research assistants who assisted with data entry and analysis. Sincere thanks to all of our study participants. Study findings were presented at meetings of the American Association for Geriatric Psychiatry in Savannah, Georgia in March of 2010, the American Association of Suicidology in Orlando, Florida in April of 2010, the Academic Research Day of The University of Western Ontario Department of Psychiatry in London, Ontario in June of 2010, the 4th National Conference of the Canadian Coalition for Seniors’ Mental Health in Halifax, Nova Scotia in September of 2010, and as part of the Edwin Shneidman Research Award Address at the annual meeting of the American Association of Suicidology in Portland, Oregon in April of 2011.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No disclosures to report.
References
- 1.Conwell Y, Heisel MJ. The elderly. In: Simon RI, Hales RE, editors. The American Psychiatric Publishing Textbook of Suicide Assessment and Management. Second Edition. Author; Arlington, VA: 2012. pp. 367–388. [Google Scholar]
- 2.National Center for Injury Prevention and Control WISQARS Fatal Injury Reports, National and Regional. 1999-2010 Available at: http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html.
- 3.Canadian Coalition for Senior's Mental Health . National Guidelines for Seniors’ Mental Health: The Assessment of Suicide Risk and Prevention of Suicide. CCSMH; Toronto: 2006. [Google Scholar]
- 4.Heisel MJ, Duberstein PR. Suicide Prevention in Older Adults. Clin Psychol-Sci Pr. 2005;12:242–259. [Google Scholar]
- 5.Areán PA, Alvidres J, Barrera A, Robinson GS, Hicks S. Would older medical patients use psychological services? The Gerontologist. 2002;42:392–398. doi: 10.1093/geront/42.3.392. [DOI] [PubMed] [Google Scholar]
- 6.Gum AM, Areán PA, Hunkeler E, et al. Depression treatment preferences in older primary care patients. The Gerontologist. 2006;46:14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- 7.Hinrichsen GA, Clougherty KF. Interpersonal psychotherapy for depressed older adults. American Psychological Association; Washington, DC: 2006. [Google Scholar]
- 8.Pinquart M, Duberstein PR, Lyness JM. Treatments for late-life depressive conditions: A meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006:1493–1501. doi: 10.1176/ajp.2006.163.9.1493. [DOI] [PubMed] [Google Scholar]
- 9.Heisel MJ, Duberstein PR, Talbot NL, King DA, Tu XM. Adapting interpersonal psychotherapy for older adults at risk for suicide: Preliminary findings. Prof Psychol Res Pract. 2009;40:156–164. doi: 10.1037/a0014731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenze EJ, Drew MA, Mazumdar S, et al. Combined pharmacotherapy and psychotherapy as maintenance treatment for late-life depression: Effects on social adjustment. Am J Psychiatry. 2002;159:466–468. doi: 10.1176/appi.ajp.159.3.466. [DOI] [PubMed] [Google Scholar]
- 11.van Schaik A, van Marwijk H, Ader H, et al. Interpersonal psychotherapy for elderly patients in primary care. Am J Geriatr Psychiatry. 2006;14:777–786. doi: 10.1097/01.JGP.0000199341.25431.4b. [DOI] [PubMed] [Google Scholar]
- 12.Reynolds CF, III, Dew MA, Pollock BG, et al. Maintenance treatment of depression in old age. N Engl J Med. 2006;354:1130–1138. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 13.Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF., III Occurrence and course of suicidality during short-term treatment of late-life depression. Arch Gen Psychiatry. 2003;60:610–617. doi: 10.1001/archpsyc.60.6.610. [DOI] [PubMed] [Google Scholar]
- 14.Szanto K, Mulsant BH, Houck PR, et al. Emergence, persistence, and resolution of suicidal ideation during treatment of depression in old age. J Affect Disord. 2007;98:153–161. doi: 10.1016/j.jad.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Alexopoulos GS, Reynolds CF, III, Bruce ML, et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. Am J Psychiatry. 2009;166:882–890. doi: 10.1176/appi.ajp.2009.08121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruce ML, Ten Have TR, Reynolds CF, III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. A randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 17.Cukrowicz KC, Cheavens JS, Van Orden KA, Ragain RM, Cook RL. Perceived burdensomeness and suicide in older adults. Psychol Aging. 2011;26:331–338. doi: 10.1037/a0021836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Purcell B, Heisel MJ, Speice J, Franus N, Conwell Y, Duberstein PR. Family connectedness moderates the association between living alone and suicide ideation in a clinical sample of adults 50 years and older. Am J Geriatr Psychiatry. 2012;20:717–723. doi: 10.1097/JGP.0b013e31822ccd79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiktorsson S, Runeson B, Skoog I, Östling S, Waern M. Attempted suicide in the elderly: Characteristics of suicide attempters 70 years and older and a general population comparison group. Am J Geriatr Psychiatry. 2010;18:57–67. doi: 10.1097/JGP.0b013e3181bd1c13. [DOI] [PubMed] [Google Scholar]
- 20.Heisel MJ. Suicide and its prevention among older adults. Can J Psychiatry. 2006;51:143–154. doi: 10.1177/070674370605100304. [DOI] [PubMed] [Google Scholar]
- 21.Heisel MJ, Flett GL. Psychological resilience to suicide ideation among older adults. Clin Gerontol. 2008;31:51–70. [Google Scholar]
- 22.Heisel MJ, Flett GL. Meaning in life and resilience to suicidal thoughts among older adults. In: Wong PTP, Wong LCJ, McDonald M, Klaassen D, editors. The Positive Psychology of Meaning and Spirituality. INPM Press; Abbotsford, BC: 2007. pp. 183–196. [Google Scholar]
- 23.Van Orden KA, Bamonti PM, King DA, Duberstein PR. Does perceived burdensomeness erode meaning in life among older adults? Aging Ment Health. 2012;16:855–860. doi: 10.1080/13607863.2012.657156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stuart S, Robertson M. Interpersonal Psychotherapy: A clinician's guide. Arnold; London: 2003. [Google Scholar]
- 25.Weissman MM, Markowitz JC, Klerman GL, editors. Comprehensive Guide to Interpersonal Psychotherapy. Basic Books; New York: 2000. [Google Scholar]
- 26.Hendin H, Haas AP, Maltsberger JT, Koestner B, Szanto K. Problems in psychotherapy with suicidal patients. Am J Psychiatry. 2006;163:67–72. doi: 10.1176/appi.ajp.163.1.67. [DOI] [PubMed] [Google Scholar]
- 27.Pallaskorpi SK, Isometsä ET, Henriksson MM, Suominen KH, Lönnqvist JK. Completed suicide among subjects receiving psychotherapy. Psychother Psychosom. 2005;74:388–391. doi: 10.1159/000087789. [DOI] [PubMed] [Google Scholar]
- 28.Cukrowicz KC, Duberstein PR, Vannoy SD, Lynch TR, McQuoid DR, Steffens DC. Course of suicide ideation and predictors of change in depressed older adults. J Affect Disord. 2009;113:30–36. doi: 10.1016/j.jad.2008.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Erlangsen A, Zarit SH, Tu X, Conwell Y. Suicide among older psychiatric inpatients : An evidence-based study of a high-risk group. Am J Geriatr Psychiatry. 2006;14:734–741. doi: 10.1097/01.JGP.0000225084.16636.ec. [DOI] [PubMed] [Google Scholar]
- 30.Karvonen K, Räsänen P, Hakko H, et al. Suicide after hospitalization in the elderly: A population based study of suicides in Northern Finland between 1988-2003. Int J Gertiatr Psychiatry. 2008;23:135–141. doi: 10.1002/gps.1853. [DOI] [PubMed] [Google Scholar]
- 31.Valenstein M, Kim HM, Ganoczy D, et al. Higher-risk periods for suicide among VA patients receiving depression treatment: Prioritizing suicide prevention efforts. J Affect Disord. 2009;112:50–58. doi: 10.1016/j.jad.2008.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Statistics Canada. 2006 Community Profiles. Ottawa. 2007 Statistics Canada Catalogue no. 92-591-XWE. [Google Scholar]
- 33.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 34.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSMIV Axis I disorders-patient edition (SCID-I/P, Version 2.0 4/97 revision) Biometrics Research Department, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- 35.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption – II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 36.First MB, Spitzer RL, Gibbon M, et al. The structured clinical interview for DSM-III-R personality disorders (SCID II). Part II. Multi-site test-retest reliability study. J Pers Disord. 1995;9:92–104. [Google Scholar]
- 37.Mishara BL, Weisstub DN. Ethical and legal issues in suicide research. Int J Law Psychiatry. 2005;28:23–41. doi: 10.1016/j.ijlp.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 38.Leenaars A. Psychotherapy with suicidal people: The commonalities. Arch Suicide Res. 2006;10:305–322. doi: 10.1080/13811110600790710. [DOI] [PubMed] [Google Scholar]
- 39.Shneidman ES. The suicidal mind. Oxford University Press; New York: 1996. [Google Scholar]
- 40.Heisel MJ, Flett GL. The development and initial validation of the Geriatric Suicide Ideation Scale. Am J Geriatr Psychiatry. 2006;14:742–751. doi: 10.1097/01.JGP.0000218699.27899.f9. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds CF, III, Frank E, Perel J, et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: A randomised controlled trial in patients older than 59 years. JAMA. 1999;281:39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- 42.Jahn DR, Cukrowicz KC, Linton K, Prabhu F. The mediating effect of perceived burdensomeness on the relation between depressive symptoms and suicide ideation in a community sample of older adults. Aging Ment Health. 2011;15:214–220. doi: 10.1080/13607863.2010.501064. [DOI] [PubMed] [Google Scholar]
- 43.Neufeld E, O'Rourke N, Donnelly M. Enhanced measurement sensitivity of hopeless ideation among older adults at risk of self-harm: Reliability and validity of Likert-type responses to the Beck Hopelessness Scale. Aging Ment Health. 2010;14:752–756. doi: 10.1080/13607860903421052. [DOI] [PubMed] [Google Scholar]
- 44.Segal DL, Marty MA, Meyer WJ, Coolidge FL. Personality, suicidal ideation, and reasons for living among older adults. J Gerontol B Psychol Sci Soc Sci. 2012;67:159–166. doi: 10.1093/geronb/gbr080. [DOI] [PubMed] [Google Scholar]
- 45.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams JBW. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 47.Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M. Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESDR). In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 3rd ed. Erlbaum Associates; Hillsdale, NJ: 2004. Chapter 40. [Google Scholar]
- 48.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of Psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. [Google Scholar]
- 49.Clark PJ, Marshall VW, Ryff CD, Wheaton B. Measuring psychological well-being in the Canadian Study of Health and Aging. Int Psychogeriatr. 2001;13:79–90. doi: 10.1017/s1041610202008013. [DOI] [PubMed] [Google Scholar]
- 50.Kafka GJ, Kozma A. The construct validity of Ryff's Scales of Psychological Well-Being (SPWB) and their relationship to measures of subjective well-being. Soc Indic Res. 2002;57:171–190. [Google Scholar]
- 51.Ryff CD, Keyes CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 52.Weissman MM. SAS-SR: Social Adjustment Scale-Self-Report Manual. Multi-Health Systems; Canada: 1999. [Google Scholar]
- 53.Koenig HG, Westlund RE, George LK. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics. 1993;34:61–69. doi: 10.1016/S0033-3182(93)71928-3. [DOI] [PubMed] [Google Scholar]
- 54.Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. J Couns Psychol. 1989;36:223–233. [Google Scholar]
- 55.Stevens CL, Muran JC, Safran JD, Gorman BS, Winston A. Levels and patterns of the therapeutic alliance in brief psychotherapy. Am J Psychother. 2007;61:109–129. doi: 10.1176/appi.psychotherapy.2007.61.2.109. [DOI] [PubMed] [Google Scholar]
- 56.Schwarzer R. Manual for the meta-analysis computer programs (Research Report) Freie Universität Berlin, Institut für Psychologie; Berlin: 1989. Available at http://userpage.fu-berlin.de/~health/manual.pdf. [Google Scholar]
- 57.Duberstein PR, Conwell Y, Seidlitz L, Denning DG, Cox C, Caine ED. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J Gerontol. 2000;55B:P18–P26. doi: 10.1093/geronb/55.1.p18. [DOI] [PubMed] [Google Scholar]
- 58.Links PS, Heisel MJ, Quastel A. Is suicide ideation a surrogate endpoint for geriatric suicide? Suicide Life Threat Behav. 2005;35:193–205. doi: 10.1521/suli.35.2.193.62870. [DOI] [PubMed] [Google Scholar]
- 59.Waern M, Beskow J, Runeson B, Skoog I. Suicidal feelings in the last year of life in elderly people who commit suicide. Lancet. 1999;354:917–918. doi: 10.1016/S0140-6736(99)93099-4. [DOI] [PubMed] [Google Scholar]
- 60.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psychooncology. 2010;19:21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lapierre S, Dubé M, Bouffard L, Alain M. Addressing suicidal ideations through the realization of meaningful personal goals. Crisis. 2007;28:16–25. doi: 10.1027/0227-5910.28.1.16. [DOI] [PubMed] [Google Scholar]
- 62.Fry PS. Religious involvement, spirituality and personal meaning for life: Existential predictors of psychological wellbeing in community-residing and institutional care elders. Aging Ment Health. 2000;4:375–387. [Google Scholar]
- 63.Krause N. Meaning in life and mortality. J Gerontol B Psychol Sci Soc Sci. 2009;64B:517–527. doi: 10.1093/geronb/gbp047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.O'Connor BP, Vallerand RJ. Psychological adjustment variables as predictors of mortality among nursing home residents. Psychol Aging. 1998;13:368–374. doi: 10.1037//0882-7974.13.3.368. [DOI] [PubMed] [Google Scholar]
- 65.Duberstein PR, Heisel MJ. Personality traits and the reporting of affective disorder symptoms in depressed patients. J Affect Disord. 2007;103:165–171. doi: 10.1016/j.jad.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 66.Vannoy SD, Duberstein P, Cukrowicz K, Lin E, Fan MY, Unützer J. The relationship between suicide and late-life depression. Am J Geriatr Psychiatry. 2007;15:1024–1033. doi: 10.1097/JGP.0b013e3180cc2bf1. [DOI] [PubMed] [Google Scholar]
- 67.Pompili M, Innamorati M, Masotti V. Suicide in the elderly: A psychological autopsy study in a North Italy area (1994-2004). Am J Geratr Psychiatry. 2008;16:727–735. doi: 10.1097/JGP.0b013e318170a6e5. [DOI] [PubMed] [Google Scholar]
- 68.Waern M, Runeson BS, Allebeck P, et al. Mental disorder in elderly suicides: A case-control study. Am J Psychiatry. 2002;159:450–455. doi: 10.1176/appi.ajp.159.3.450. [DOI] [PubMed] [Google Scholar]
- 69.Perepletchikova F, Treat TA, Kazdin AE. Treatment integrity in psychotherapy research: Analysis of the studies and examination of the associated factors. J Consult Clin Psychol. 2007;75:829–841. doi: 10.1037/0022-006X.75.6.829. [DOI] [PubMed] [Google Scholar]
- 70.Chan SS, Leung VPY, Tsoh J, et al. Outcomes of a two-tiered multifaceted elderly suicide prevention program in a Hong Kong Chinese community. Am J Geriatr Psychiatry. 2011;19:185–196. doi: 10.1097/JGP.0b013e3181e56d0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lapierre S, Erlangsen A, Waern M. A systematic review of elderly suicide prevention programs. Crisis. 2011;32:88–98. doi: 10.1027/0227-5910/a000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Oyama H, Sakashita T, Ono Y, Goto M, Fujita M, Koida J. Effect of community-based intervention using depression screening on elderly suicide risk: A meta-analysis of the evidence from Japan. Community Ment Health J. 2008;44:311–320. doi: 10.1007/s10597-008-9132-0. [DOI] [PubMed] [Google Scholar]
- 73.Raue PJ, Morales KH, Post EP, Bogner HR, Ten Have T, Bruce ML. The wish to die and 5-year mortality in elderly primary care patients. Am J Geratr Psychiatry. 2010;18:341–350. doi: 10.1097/JGP.0b013e3181c37cfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Unützer J, Tang L, Oishi S, et al. Reducing suicidal ideation in depressed older primary care patients. J Am Geriatr Soc. 2006;54:1550–1556. doi: 10.1111/j.1532-5415.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- 75.Agency for Health Research and Quality [February 16, 2012];Translating Research Into Practice (TRIP)-II. Agency for Health Research and Quality. 2001 Available at http://www.ahrq.gov/research/trip2fac.htm.