Abstract
This study asks: 1. What are the relationships between types of living arrangements and psychological well-being for older adults? and 2. How do these relationships differ by gender? Data come from the 2010 wave of the National Health Interview Survey and include non-institutionalized adults age 65 and older (n=4,862). Dependent variables include self-rated quality of life and psychological distress. The study finds that older adults living alone or with others fare worse than those living with a spouse only. Yet, the outcomes of different types of living arrangements for older adults vary by gender. Women living with others are at greater risk of worse quality of life and serious psychological distress than men. Programs and policies must be responsive to the diverse needs of this population, rather than attempting a “one-size-fits-all” approach to housing and community-based services designed to promote older adults’ psychological well-being and independence.
Keywords: Living arrangements, distress, older adults, mental health, quality of life, psychological distress, gender
Older adults (defined here as adults age 65 and older) are at a decreased risk of depression compared with younger adults (Fiske, Wetherell, & Gatz, 2009). However, those older adults who suffer from depression are especially vulnerable to poor health outcomes and diminished quality of life. They have an increased risk of suicide compared with younger adults (Fiske et al., 2009; National Institute of Mental Health (NIMH), 2007) and require particular attention in research, practice, and policy. Understanding depression and mental health in older adults is complex. There is evidence that older adults are less accurate at recognizing symptoms of depression than their younger counterparts, (Wetherell et al., 2009) and are more likely to display physical, somatic symptoms of the disorder than affective ones (Fiske et al., 2009). In order to fully understand older adults’ mental health and well-being, it is necessary to move beyond one-dimensional methods of measurement and to probe for both psychological distress and general quality of life. Further, it is essential to consider life circumstances and context in order to accurately understand and act on the mental health of older adults.
Access to appropriate resources is essential for anyone to function in daily life, but may be especially so for older adults who have increased likelihoods of declining physical health and increasing functional impairments. Such resources may be material or financial, as in personal wealth and assets, community physical environment, or access to local, state, and federal programs. Resources may also come in the form of social capital, with social support being an essential resource for many older adults to lessen the risk of social isolation and to provide companionship, caregiving, and assistance. However, access to and benefit from such resources is not distributed uniformly throughout the population, but has a distinctly non-random allocation based on one’s personal demographics, household composition, and place of residence (Kawachi & Berkman, 2001; Klinenberg, 2003). And, not all older adults require the same type or quantity of resources – many are able to function independently in the community without any help – nor does social isolation affect everyone in the same way (Klinenberg, 2012). This paper attempts to further our understanding some of the nuances involved in the relationship between one potential resource mechanism, living arrangements (operationalized here as household composition), and psychological well-being.
Differences by Gender and Individual Characteristics
Living arrangements and social isolation are not uniformly distributed, but are instead patterned by various demographic characteristics. For instance, while older women are more likely to live alone or be partner-less than older men (The Federal Interagency Forum on Aging-Related Statistics, 2010; Waite & Das, 2010), older men living alone are at an increased risk of being socially isolated (Klinenberg, 2003; Klinenberg, 2012). This can be attributed to the vulnerable status of many older men living alone, including living in poverty or being marginalized, and to gendered pattern of social interactions. Women are conditioned to build strong social support networks outside of marriage, while men are often dependent on their spouse for social support (Klinenberg, 2012). If men become widowed, they are therefore at increased risk of social isolation, compared with widowed women. In fact, some women living alone may have better mental health outcomes than women living with a spouse or others (Michael, Berkman, Colditz, & Kawachi, 2001).
Social isolation is also patterned by other individual characteristics including race/ethnicity, functional status, and age. For example, a 2005 study of older adults found Black men and women to be at the greatest risk of social isolation and low social capital resources (Locher et al., 2005). And, declining physical health and functional impairments increase the risk of social isolation by limiting one’s ability to interact with others outside of the home or by necessitating a move to a more accessible home environment. A 2009 study of older adults with and without physical disabilities found that those with disabilities were at greater risk of loneliness and social isolation than adults without disabilities across different types of living arrangements (Russell, 2009). Further, social isolation may contribute to increased functional impairment (Clarke, Frasure-Smith, Lesperance, & Bourassa, 2000), causing a vicious cycle for the most vulnerable older adults. Age is closely tied to functional status, as the risk of disability and functional impairment rises significantly with age. Current estimates report that 40 percent of all older adults have some functional impairment and that health status declines with age (The Federal Interagency Forum on Aging-Related Statistics, 2010).
Living Arrangements
Beyond individual characteristics, one’s living arrangements can have a profound effect on one’s quality of life and mental health (Joutsenniemi, Martelin, Martikainen, Pirkola, & Koskinen, 2006; Sereny, 2011; Greenfield & Russell, 2011). Who one lives with will influence his or her patterns of everyday social interactions (or lack thereof), as well as immediately available resources (social and otherwise). Most non-institutionalized older adults fall into one of just a few categories of living arrangements: living alone, living with a partner/spouse only, living with a spouse and others (such as adult children), and living with others only (usually in a multigenerational family situation). Which arrangement one falls into is influenced by socio-economic and demographic characteristics (Sereny, 2011; Gurak & Kritz, 2010) and there is evidence that having concordance with one’s preferred arrangement leads to better health outcomes (Sereny, 2011). Each type of living arrangement presents particular opportunities and challenges and is worth exploring in more detail to better understand the relationship to social isolation, mental health, and well-being.
Living alone
Older adults living alone constitute nearly one-third of the older adult population (The Federal Interagency Forum on Aging-Related Statistics, 2010), although there is a wide gender gap in this statistic: 40 percent of women, but only 20 percent of men, over the age of 65 live alone (Klinenberg, 2012; The Federal Interagency Forum on Aging-Related Statistics, 2010). This gender gap is due, largely, to the biological predisposition for women to outlive their husbands, leaving many more widows than widowers to contend with life alone. Living alone does not produce uniform consequences for everyone, though. Some people prefer it and simply want more services to cater to such lifestyles (Klinenberg, 2012). In fact, in some instances, living alone may lead to better mental health than living with others (Hughes & Gove, 1981). Others find creative ways to manage life and to access appropriate resources, getting by even when living alone was not necessarily one’s preference (Loe, 2011). Some research even finds that women living alone actually have better well-being than those living with a spouse (Michael et al., 2001). For others, though, who live alone and are not well-connected with their communities, living alone can be a profoundly isolating experience, leading to increased vulnerability for a variety of poor health outcomes (Klinenberg, 2003; Klinenberg, 2012).
In his study of individuals affected by the July 1995 Chicago heat wave, sociologist Eric Klinenberg found that older men constituted a disproportionate number of victims who perished in the heat wave, largely because they were socially isolated and not well-connected with their neighbors or communities, despite living in a large metropolitan area with theoretically ample resources and services (Klinenberg, 2003). Other studies have found living alone to be associated with increased risk of worse mental health outcomes, including depression and anxiety (Wilmoth & Chen, 2003; Dean, Kolody, Wood, & Matt, 1992; Mui, 1999; Sun, Lucas, Meng, & Zhang, 2011); loneliness, especially among men (Greenfield & Russell, 2011); and higher poverty rates than their counterparts living with a spouse (The Federal Interagency Forum on Aging-Related Statistics, 2010). Therefore, living alone may be a positive experience, and indeed an intentional choice for many older adults, but it may also be a risk factor for social isolation and poor mental health among those who lack strong social support resources.
Living with a spouse or partner
Older adults living with a spouse or partner constitute another 70 percent of men and 40 percent of women (The Federal Interagency Forum on Aging-Related Statistics, 2010). Research finds that outcomes for this group – both mental and physical health – tend to be the best of any living arrangement (Davis, Moritz, Neuhaus, Barclay, & Gee, 1997; Davis, Murphy, Neuhaus, Gee, & Quiroga, 2000; Greenfield & Russell, 2011). However, this group is uniquely vulnerable to health issues, should one partner develop a functional impairment. Often in these situations, the burden of unpaid caregiving falls to the healthier spouse and the experience of caring for a frail and ailing spouse can, in itself, be socially isolating, with research indicating that spousal caregivers have more depressive symptoms, lower well-being, and worse physical health outcomes than other caregivers (Pinquart & Sorensen, 2011). Even this is not uniformly true, however, with some caregivers reporting better outcomes than non-caregivers (Robison, Fortinsky, Kleppinger, Shugrue, & Porter, 2009). Further, the effects of living with a spouse appear to be different depending on demographic characteristics, such as race/ethnicity, immigrant status (Wilmoth & Chen, 2003), age, (Davis et al., 2000) and gender, with men having better outcomes from living with a spouse than their female counterparts (Davis, 1990; Davis et al., 2000).
Living with others
The third category, those older adults who live with others – usually relatives – comprises a diverse group. These are often older adults who have moved back in with children or have had children move in with them to provide caregiving in the wake of declining health and functional status. The distribution of this population varies widely by gender, age, race/ethnicity, and geographical context (de Jong Gierveld & van Tilburg, 1999; The Federal Interagency Forum on Aging-Related Statistics, 2010). This group has been found to be particularly vulnerable to poor mental health outcomes and loneliness, especially when compared with older adults living with a spouse only (Wilmoth & Chen, 2003; Greenfield & Russell, 2011). Even among this population, outcomes vary widely, though, with some research showing that older adults in multigenerational households fare better than those in single-generation households (Silverstein, Cong, & Li, 2006). And, gender disparities persist among this population, with women in this group experiencing worse physical and mental health outcomes than men (Hughes & Waite, 2002). More research is needed on this population, especially as there is currently an increasing trend toward Americans living in multi-generational households following a steady decline in such arrangements between 1940 and 1980 (Taylor et al., 2010). Further, it is useful to examine differences between those who live with others and a spouse vs. those who live with others without a spouse, as those in the latter category demonstrate worse outcomes (Hughes & Waite, 2002).
Conceptually, there are several reasons why living arrangements might impact psychological well-being. The most intuitive may be social interaction, or lack thereof, provided within the home environment. This interaction may be positive, preventing social isolation and providing meaningful engagement and emotional support. For example, older adults may have mutually beneficial companionship with those they live with, including behaviors such as eating meals together, enjoying leisure activities, and exchanging information, all of which are important for quality of life (Barker, 2002). However, household social interaction may also have adverse consequences, as in the case of relational conflict and stressful obligations (Hughes & Gove, 1981).
Living arrangements are also closely tied to caregiving responsibilities. Older adults may receive care from those they live with, or they may act as caregivers for others in the house, for example, for a spouse with functional impairments or for grandchildren (Administration on Aging, 2012; Institute on Medicine, 2008). Living with others may help to disperse caregiving burdens, which can otherwise have a detrimental impact on mental health (Pinquart & Sörensen, 2003). And, for older adults with functional impairments, living with others may be helpful in having care needs met, including instrumental support with activities of daily living and household chores. Finally, living arrangements are related to socioeconomic status, which is associated with mental health in older adults (Koster et al., 2006). Older adults living alone are more likely to be poor than those living with a spouse or others (Issa & Zedlewski, 2011) and those living with others are able to share economic resources. However, poorer families living together may experience crowded conditions within the household if, for example, they take in an older adult who needs care. Such crowding could lead to stress and poor mental health outcomes (Regoeczi, 2008; Gómex-Jacinto & Hombrados-Mendieta, 2002).
Research Objectives
While the literature on living arrangements and associated outcomes among older adults is persuasive, much of it is limited by looking at particular populations or within a narrow geographic context. Further, few studies have investigated general quality of life and psychological distress and their associations with living arrangements. A better understanding of how living arrangements contribute to the psychological well-being of older adults is important and increasingly urgent for designing policies and programs as the U.S. population ages at an unprecedented rate. This paper seeks to add to our understanding of the association between living arrangements and psychological well-being among older adults by investigating the following research questions using nationally-representative survey data: 1. What are the relationships between types of living arrangements and two dependent variables: psychological distress and quality of life? and 2. How do these relationships differ for men and women?
METHODS
Data
Data for this study come from the Integrated Health Interview Series (IHIS) (Ruggles et al., 2010), a publicly-available harmonized version of the National Health Interview Survey (NHIS), which has been collected annually by the National Center for Health Statistics since 1969. Data for this analysis come from the 2010 wave of the IHIS, as this wave includes detailed questions on quality of life from a Quality of Life Supplement. The Supplement was fielded to one-quarter of those respondents who had been randomly selected for the NHIS Sample Adult survey. The NHIS response rate for sample adults, taking into account household and family non-response was 60.8 percent (National Center for Health Statistics, 2011). The data is population weighted to account for complex sampling and non-response.
Sample
The sample consists of civilian, non-institutionalized individuals living in the U.S. For these analyses, it was further restricted to individuals age 65 and older who completed questions on psychological distress and quality of life and had no missing responses on any covariates, resulting in a sample size of 4,862, equating to a weighted population of 18,200,061.
Dependent Variables
This paper examines two main dependent variables: self-rated quality of life and serious psychological distress. Quality of life is measured with a five-item Likert scale answering the question, “In general, would you say your quality of life is…” Response options included “excellent”, “very good”, “good”, “fair”, and “poor”. For these analyses, “excellent” was coded as “5” and “poor” was coded as “1”. Psychological distress was measured using the Kessler 6 (K6) scale, which was designed to measure non-specific psychological distress among NHIS respondents (Kessler et al., 2002). The K6 provides valid and reliable results across major demographic populations (Kessler et al., 2002; Furukawa, Kessler, Slade, & Andrews, 2003). It has been commonly used to measure psychological distress in older adults (Sorkin, Pham, & Ngo-Metzger, 2009; Lim & Taylor, 2005; Shih, Hootman, Strine, Chapman, & Brady, 2006; McGuire et al., 2009) and is associated with future health outcomes, including mortality (Pratt, 2009). Sample respondents were asked how often they experienced six different symptoms within the past 30 days: feeling that everything was an effort, feeling hopeless, feeling nervous, feeling restless, feeling sad, and feeling worthless. Each question was scaled from “0” to “4” with “0” representing “none of the time” and “4” representing “all of the time”. Responses to all six questions were tallied, with a possible range of responses from “0” to “24”. A score of “13” or higher indicates serious psychological distress (Kessler et al., 2002). While it would be possible to use the K6 as a continuous scale, using the dichotomous cut-off of 13 allows consistency across and comparisons with other studies of serious psychological distress (Kessler et al., 2002; Sorkin et al., 2009; Pratt, 2009; Shih et al., 2006; McGuire et al., 2009). It is important to include both dependent variables in these analyses as there is evidence that older adults may experience and perceive depressive symptoms and distress differently than younger adults (Wetherell et al., 2009) and one measure may not provide a complete picture of older adults’ mental health. Using both quality of life and psychological distress allows for more robust comparisons with the rest of the population, while potentially gaining a more accurate picture of the predictors of older adults’ well-being.
Independent Variables
The main independent variable of interest is respondents’ living arrangements, which was constructed as a four-category variable combining household composition and marital status, following the previous convention on living arrangements among older adults (Hughes & Waite, 2002). The sample included 175 respondents who were categorized as “cohabiting”. For purposes of analyses, these respondents were all treated as married and were combined with the two married subgroups. If respondents had a household size of 1, they were categorized as living alone; if respondents had a household size of 2 and were coded as married or cohabiting and living with a spouse/partner, they were categorized as living with a spouse only; if respondents had a household size >2 and were married or cohabiting, they were categorized as living with a spouse and others; and if respondents had a household size >1 and were coded as not married or cohabiting, they were categorized as living with others only. 7.7 percent of those living with others were living with non-family members. For those living with others, the most common arrangement was living with an adult child, but other relationships included sibling, grandparent, aunt/uncle, and housemate/roommate.
A variety of demographic characteristics were also included. These included age; sex (1=female); and educational attainment (1=less than a high school degree; 2=high school degree; 3=some college; 4=college degree or more). Race/ethnicity were constructed according to the Office of Management and Budget (OMB) guidelines for smallest group assignment (Office of Management and Budget (OMB), 2010), with Hispanic/Latino ethnicity trumping race so that respondents were coded into only one category each. Poverty status was constructed using the IHIS’s imputed poverty variable. The IHIS provides five imputations and for this analysis, the mean of the five was taken to construct poverty level. For individuals living alone or with non-relatives, the poverty status indicates their individual ratio to the federal poverty threshold. For individuals living with a spouse or other family members, the poverty variable takes the entire family income into account when constructing the ratio. To include contextual/spatial characteristics that may point to underlying cultural context and state or region-based policies, the analysis includes region of residence: Northeast; North Central/Midwest; South; and West. Finally, self-rated physical health was included as a control. This is especially important as older adults may experience mental illness and psychological distress as somatic symptoms (Fiske et al., 2009).
Analysis
Bivariate relationships were tested using Pearson’s chi-squared tests of significance. Separate multivariate models were calculated to predict quality of life and psychological distress. Because quality of life is measured on a five-category scale, nested ordered logistic regression models were estimated with results reported as odds ratios (>1 indicates higher odds of reporting better quality of life). First, living arrangements were entered into the model on their own, with living with a spouse/partner as the reference category. Next, demographic characteristics were added, followed by self-rated physical health. Educational attainment, ratio to the federal poverty threshold, and self-rated physical health were all entered as continuous variables (in each case, a higher score indicates less hardship). Finally, region was added into the models. Serious psychological distress was modeled as a binary variable, using a series of nested logistic regression models with results reported as odds ratios (>1 indicates higher odds of having serious psychological distress). In these models controls were added in the same sequence as the previous analysis. In each case, living with a spouse/partner only was the reference category. Finally, because previous literature indicates differing effects of living arrangements by gender, analyses were run separately for men versus women, with adjusted odds ratios of better quality of life and serious psychological distress reported. All analyses were conducted in Stata, using survey weights to account for the complex sampling design and to provide adjusted standard errors.
RESULTS
The sample is divided across types of living arrangements, with 36 percent living alone, 50 percent living with a spouse/partner only, 5 percent living with a spouse/partner and others, and 10 percent living with others only. The mean household size for those living with others was 3.2 people, and the mode was 2 people, likely an adult child with an aging parent. Table 1 provides sample characteristics. Differences across living arrangement categories were significant (p<0.001) in each category. The average age of the sample is significantly older among those who live alone. And, those living alone are more likely to live in poverty than respondents in the other three categories. Those living with others only have lower educational attainment, are more likely to be non-White, and have worse self-rated physical health than those living alone or with a spouse/partner. Close to one-third of all respondents lived in the South, and regional differences were most pronounced among those living with a spouse only or living with others only.
Table 1.
Sample Characteristics
| Living with spouse only | Living alone | Living with spouse and others | Living with others only | P-Value | |
|---|---|---|---|---|---|
|
|
|||||
| Frequency of living arrangement | 0.357 | 0.496 | 0.049 | 0.098 | |
| Age (M) | 73.1 | 76.1 | 72.2 | 75.2 | <0.001 |
| Female | 0.462 | 0.714 | 0.367 | 0.774 | <0.001 |
| Education | <0.001 | ||||
| Less than high school | 0.141 | 0.221 | 0.273 | 0.319 | |
| High school | 0.346 | 0.349 | 0.304 | 0.329 | |
| Some college | 0.245 | 0.251 | 0.189 | 0.205 | |
| College and beyond | 0.268 | 0.179 | 0.235 | 0.147 | |
| Family poverty status | <0.001 | ||||
| <100% of poverty threshold | 0.027 | 0.146 | 0.084 | 0.138 | |
| 100–200% of poverty threshold | 0.140 | 0.288 | 0.208 | 0.248 | |
| 200–300% of poverty threshold | 0.217 | 0.261 | 0.262 | 0.228 | |
| 300–400% of poverty threshold | 0.262 | 0.139 | 0.157 | 0.200 | |
| >400% of poverty threshold | 0.355 | 0.166 | 0.289 | 0.186 | |
| Race/ethnicity | <0.001 | ||||
| White | 0.871 | 0.829 | 0.584 | 0.623 | |
| Black/African American | 0.049 | 0.096 | 0.140 | 0.189 | |
| Native American/Alaskan Native | 0.004 | 0.004 | 0.000 | 0.005 | |
| Asian | 0.028 | 0.020 | 0.098 | 0.033 | |
| Hispanic/Latino | 0.048 | 0.051 | 0.178 | 0.150 | |
| Self-rated physical health | <0.001 | ||||
| Poor | 0.042 | 0.043 | 0.036 | 0.097 | |
| Fair | 0.151 | 0.172 | 0.192 | 0.268 | |
| Good | 0.319 | 0.341 | 0.392 | 0.342 | |
| Very good | 0.313 | 0.299 | 0.271 | 0.190 | |
| Excellent | 0.175 | 0.145 | 0.109 | 0.103 | |
| Region | <0.001 | ||||
| Northeast | 0.172 | 0.225 | 0.154 | 0.178 | |
| North Central/Midwest | 0.266 | 0.255 | 0.201 | 0.171 | |
| South | 0.372 | 0.328 | 0.321 | 0.381 | |
| West | 0.190 | 0.192 | 0.325 | 0.270 | |
Statistics calculated using weighted sample (population N=18,200,061; sample n=4,862).
P-value denotes significant differences between living arrangements.
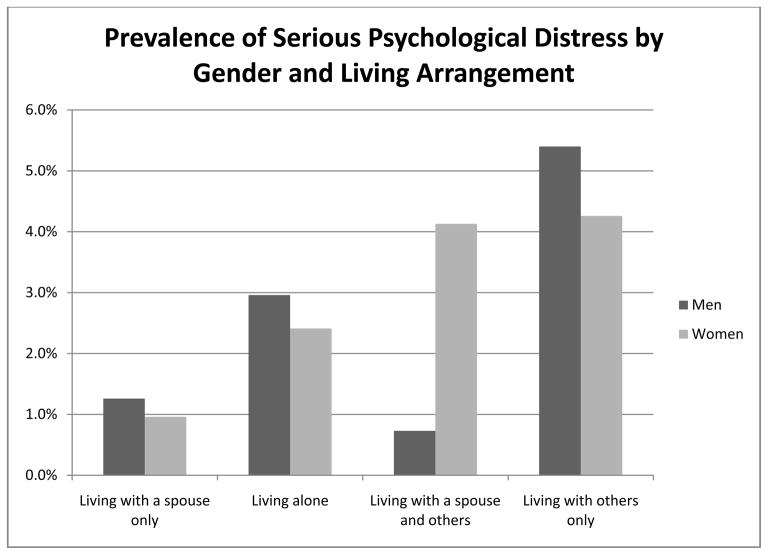
Figure 1 illustrates the prevalence of serious psychological distress by living arrangement and gender. Living with others only was associated with the highest prevalence of serious psychological distress among men (5.4 percent), while living with others with or without a spouse were both associated with rates of serious psychological distress just over 4 percent among women. Differences between living arrangements in rates of distress are significant at p<0.001 for men and women.
Figure 1.
Prevalence of Serious Psychological Distress by Gender and Type of Living Arrangement
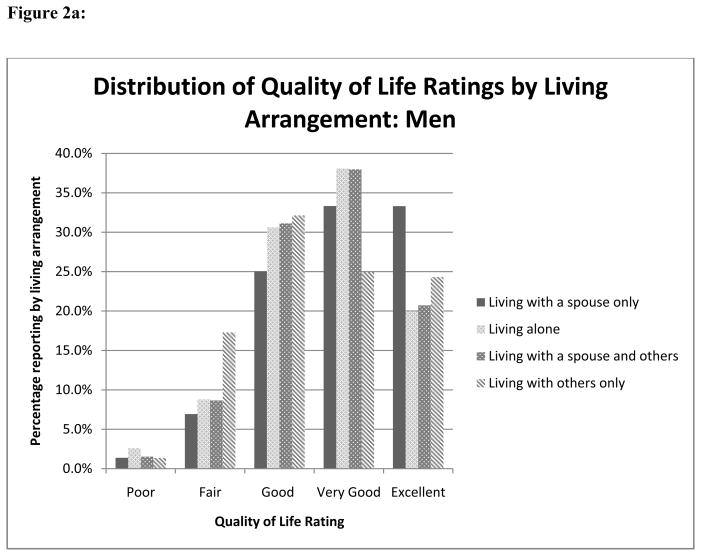
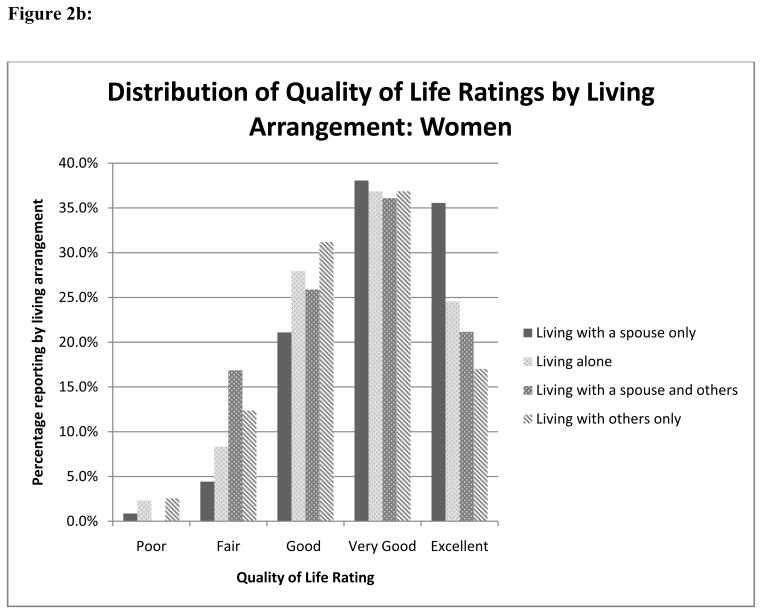
Figures 2a and 2b show the distribution of quality of life ratings by type of living arrangement separately for men and women. Among men, 33.3 percent of those living with a spouse/partner only reported excellent quality of life, while between 20–25 percent of those in the other three arrangements reported excellent. 18.6 percent of men living with others only reported fair or poor quality of life, compared with 8.3 percent of those living with a spouse/partner only. Trends were similar among women, where the best situation was again living with a spouse/partner only (35.6 percent of those women reported excellent quality of life compared with 17 percent of those living with others only). However, the relationship between fair/poor quality of life and living with a spouse/partner and others appeared stronger for women than men (16.9 vs. 10.2 percent).
Figure 2.
Figure 2a: Distribution of Quality of Life Ratings by Living Arrangement: Men
Figure 2b: Distribution of Quality of Life Ratings by Living Arrangement: Women
Table 2 presents the results of the ordered logistic regression models predicting quality of life. Results are presented as odds ratios with 95 percent confidence intervals. In Model 1, living alone and living with others are both significantly associated with poorer quality of life, compared with those individuals living with a spouse/partner only. Model 2 added demographic control variables. Being older, Black, Native American, and Asian are all associated with worse odds of better quality of life. In contrast, being female, having higher educational attainment, and being further from the federal poverty line are all associated with better quality of life. Model 3 added physical health, which appears to mediate some of the effects of race/ethnicity and age on quality of life and is itself strongly associated with better quality of life with an odds ratio greater than 3. Finally, Model 4 added geographical context. While living arrangements remain significantly associated with quality of life (with those living with a spouse only fairing far better than the other three categories), we can see that place also plays a role, at least in the North Central/Midwest and Southern regions, where residents had significantly better odds of better quality of life compared with their counterparts in the Northeast.
Table 2.
Nested Ordered Logistic Regression Models Predicting Odds of Reporting Better Quality of Life
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
|
|
||||
| Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
|
|
|
||||
| Living arrangement (Ref: With spouse only) | ||||
| Living alone | 0.62*** (0.54, 0.70) |
0.79** (0.69, 0.91) |
0.70*** (0.61, 0.80) |
0.71*** (0.61, 0.81) |
| Living with spouse and others | 0.55*** (0.43, 0.70) |
0.71** (0.55, 0.91) |
0.71* (0.54, 0.93) |
0.72* (0.54, 0.94) |
| Living with others only | 0.45*** (0.37, 0.54) |
0.61*** (0.49, 0.75) |
0.72** (0.58, 0.90) |
0.74** (0.60, 0.92) |
| Age | 0.99* (0.98, 1.00) |
1.00 (0.99, 1.01) |
1.00 (0.99, 1.01) |
|
| Female | 1.24*** (1.10, 1.39) |
1.19** (1.05, 1.34) |
1.18** (1.05, 1.34) |
|
| Educational attainment | 1.37*** (1.29, 1.46) |
1.22*** (1.15, 1.30) |
1.23*** (1.15, 1.31) |
|
| Ratio to poverty threshold | 1.28*** (1.21, 1.34) |
1.16*** (1.10, 1.22) |
1.12*** (1.10, 1.23) |
|
| Race/ethnicity (Reference=White) | ||||
| Black/African American | 0.75** (0.64, 0.89) |
1.01 (0.85, 1.21) |
0.99 (0.82, 1.18) |
|
| Native American/Alaskan Native | 0.29** (0.13, 0.66) |
0.49 (0.17, 1.40) |
0.52 (0.18, 1.48) |
|
| Asian | 0.51*** (0.41, 0.65) |
0.63*** (0.49, 0.81) |
0.68** (0.52, 0.88) |
|
| Hispanic/Latino | 0.86 (0.71, 1.06) |
0.97 (0.78, 1.20) |
1.00 (0.81, 1.25) |
|
| Physical health (1=poor; 5=excellent) | 3.00*** (2.79, 3.22) |
3.00*** (2.79, 3.23) |
||
| Region (Reference=Northeast) | ||||
| North Central/Midwest | 1.26** (1.06, 1.49) |
|||
| South | 1.22* (1.04, 1.44) |
|||
| West | 1.03 (0.86, 1.23) |
|||
Statistics calculated using weighted sample (population N=18,200,061; sample n=4,862).
Differences significant at
p<0.05;
p<0.01;
p<0.001.
Table 3 presents odds ratios with 95 percent confidence intervals for the nested logistic regression models predicting serious psychological distress. In Model 1, living alone and living with others only are both significantly associated with higher odds of serious psychological distress compared with those living with a spouse/partner. These relationships hold across Models 2–4, with those living with others only exhibiting particularly strong odds of serious psychological distress, compared with their counterparts living with a spouse/partner. Older age, more education and wealth, better physical health, and being Black/African American are all associated with lower odds of serious psychological distress across the models.
Table 3.
Nested Logistic Regression Models Predicting Odds of Serious Psychological Distress
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
|
|
||||
| Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
|
|
|
||||
| Living arrangement (Ref: With spouse only) | ||||
| Living alone | 2.32** (1.35, 3.99) |
1.86* (1.03, 3.35) |
1.95* (1.08, 3.51) |
1.90* (1.05, 3.44) |
| Living with spouse and others | 1.78 (0.66, 4.83) |
1.36 (0.47, 3.91) |
1.47 (0.52, 4.19) |
1.43 (0.51, 4.06) |
| Living with others only | 4.17*** (2.22, 7.81) |
3.16** (1.60, 6.25) |
2.57** (1.31, 5.05) |
2.49** (1.27, 4.91) |
| Age | 0.96* (0.93, 0.99) |
0.96* (0.93, 0.99) |
0.96* (0.93, 0.99) |
|
| Female | 0.89 (0.57, 1.38) |
0.97 (0.63, 1.51) |
0.98 (0.63, 1.52) |
|
| Educational attainment | 0.65*** (0.51, 0.82) |
0.75* (0.60, 0.94) |
0.74** (0.59, 0.93) |
|
| Ratio to poverty threshold | 0.71*** (0.59, 0.85) |
0.80* (0.66, 0.97) |
0.79* (0.65, 0.97) |
|
| Race/ethnicity (Reference=White) | ||||
| Black/African American | 0.57 (0.31, 1.05) |
0.45* (0.24, 0.84) |
0.45* (0.24, 0.85) |
|
| Native American/Alaskan Native | 5.71 (0.91, 35.87) |
2.95 (0.31, 28.49) |
2.6 (0.27, 25.26) |
|
| Asian | 1.00 (0.38, 2.61) |
0.77 (0.29, 2.06) |
0.68 (0.24, 1.91) |
|
| Hispanic/Latino | 1.01 (0.56, 1.83) |
0.95 (0.52, 1.73) |
0.86 (0.46, 1.60) |
|
| Physical health (1=poor; 5=excellent) | 0.44*** (0.33, 0.58) |
0.44*** (0.33, 0.59) |
||
| Region (Reference=Northeast) | ||||
| North Central/Midwest | 0.59 (0.30, 1.16) |
|||
| South | 0.88 (0.50, 1.54) |
|||
| West | 0.99 (0.54, 1.84) |
|||
Statistics calculated using weighted sample (population N=18,200,061; sample n=4,862).
Differences significant at
p<0.05;
p<0.01;
p<0.001.
Finally, Table 4 presents sub-group analyses by gender. Results are presented as adjusted odds ratios with 95 percent confidence intervals. For men, living alone was associated with lower odds of better quality of life (.72), compared with those living with a spouse/partner only. But, odds did not differ for those living with others (with or without a spouse/partner). For women, however, odds of better quality of life were significantly lower for all three categories compared with those living with a spouse/partner only. For men, there were no significant differences in odds of serious psychological distress by living arrangement, but for women, living with others only was associated with significantly higher odds of serious psychological distress (3.18).
Table 4.
Stratified Analyses by Gender Predicting Quality of Life and Serious Psychological Distress
| Better Quality of Life | Serious Psychological Distress | |||
|---|---|---|---|---|
|
|
||||
| Men | Women | Men | Women | |
|
|
||||
| Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
Adjusted OR (95% CI) |
|
|
|
||||
| Living arrangement (Ref: With spouse only) | ||||
| Living alone | 0.72** (0.59, 0.89) |
0.68*** (0.56, 0.83) |
1.85 (0.85, 4.03) |
2.12 (0.87, 5.20) |
| Living with spouse and others | 0.77 (0.55, 1.09) |
0.64* (0.41, 0.98) |
0.49 (0.11, 2.10) |
3.44 (0.86, 13.75) |
| Living with others only | 0.96 (0.62, 1.48) |
0.67** (0.52, 0.87) |
1.71 (0.64, 4.59) |
3.18* (1.20, 8.44) |
| Age | 1.00 (0.99, 1.01) |
1.00 (0.99, 1.01) |
0.98 (0.93, 1.03) |
0.95* (0.91, 0.99) |
| Educational attainment | 1.26*** (1.14, 1.39) |
1.21*** (1.11, 1.31) |
0.80 (0.54, 1.17) |
0.70* (0.53, 0.94) |
| Ratio to poverty threshold | 1.18*** (1.09, 1.28) |
1.15*** (1.07, 1.24) |
0.77 (0.56, 1.05) |
0.81 (0.63, 1.05) |
| Race/ethnicity (Reference=White) | ||||
| Black/African American | 0.98 (0.73, 1.30) |
1.01 (0.80, 1.26) |
0.46 (0.19, 1.15) |
0.42 (0.17, 1.01) |
| Native American/Alaskan Native | 0.42 (0.07, 2.38) |
0.56 (0.15, 2.07) |
Omitted - |
4.50 (0.34, 60.05) |
| Asian | 0.72 (0.48, 1.09) |
0.65* (0.46, 0.92) |
0.60 (0.06, 6.15) |
0.73 (0.25, 2.11) |
| Hispanic/Latino | 1.08 (0.77, 1.51) |
0.96 (0.72, 1.28) |
0.93 (0.37, 2.38) |
0.77 (0.33, 1.79) |
| Physical health (1=poor; 5=excellent) | 2.76*** (2.47, 3.09) |
3.19*** (2.90, 3.51) |
0.29*** (0.16, 0.54) |
0.53*** (0.38, 0.74) |
| Region (Reference=Northeast) | ||||
| North Central/Midwest | 1.34* (1.02, 1.77) |
1.20 (0.97, 1.50) |
0.51 (0.14, 1.79) |
0.60 (0.26, 1.38) |
| South | 1.24 (0.95, 1.61) |
1.21 (0.97, 1.49) |
0.85 (0.30, 2.40) |
0.86 (0.44, 1.68) |
| West | 1.02 (0.77, 1.37) |
1.04 (0.83, 1.31) |
1.13 (0.39, 3.24) |
0.90 (0.43, 1.89) |
Notes: Quality of life is modeled with ordered logistic regression (5=excellent; 1=poor). AOR>1 means higher odds of better QOL. Serious psychological distress is modeled with logistic regression (1=has SPD). AOR>1 means higher odds of SPD.
Native American/Alaskan Native omitted for SPD for men due to rarity SPD among NA/AN men in sample.
Statistics calculated using weighted sample (population N=18,200,061; sample n=4,862).
Differences significant at
p<0.05;
p<0.01;
p<0.001.
DISCUSSION
The primary finding of this paper is that there are significant differences in psychological well-being for older adults, depending on type of living arrangement, and that those relationships differ by gender. The current focus of much of the policy agenda around housing an aging population focuses on “aging-in-place”, or keeping older adults in their own homes as they age. While this is a laudable goal, given that the majority of older adults would prefer to remain in their homes (AARP Public Policy Institute, 2010), it is clear that the effects of living arrangements are not uniform across the entire older adult population. While this study does not provide for a comparison between those older adults that live alone while aging-in-place with those who move to an institutional setting, it is clear that the nearly two-thirds of older adults who do live alone or with others in the community are a vulnerable population deserving of attention in policy and research. Interventions may seek to bolster access to social support and other resources that may make it easier for older adults to manage life alone or without a spouse/partner.
Further, while this paper clearly demonstrates that older adults living alone are at greater risk for psychological distress and worse quality of life than their counterparts living with a spouse/partner only, greater attention should also be paid to older adults who live with others. There is an increasing trend of older adults living in multi-generational households (Taylor et al., 2010) and these individuals may be at particular risk for depression and poor quality of life. In each measure in these analyses, this group fared worse than both older adults living with a spouse/partner only and as poorly as those living alone. These results were especially strong when there was no spouse/partner present in the household. These findings held true for quality of life, even when controlling for health status, which may contribute to older adults living with younger generations. Much attention has been paid in research and policy to the plight of younger caregivers, but more attention may be warranted toward the well-being of the older adults being cared for. Further, this study’s results demonstrate that while older adults may have social capital resources available by virtue of living with others, the effect of such resources is not automatically positive. Specially, the finding that women living with others, with or without a spouse/partner, have lower quality of life than those living with a spouse only indicate a negative association of with living with others for women. This is consistent with other research demonstrating that the impact of social support can vary by demographic characteristics (e.g., gender) and that such support can sometimes have a negative effect (Kawachi & Berkman, 2001).
Additionally, this paper demonstrates that the outcome of different types of living arrangements for older adults is not uniform across the population, but varies by demographic and place characteristics. Higher socioeconomic status (measured by higher educational attainment and income) was consistently associated with better quality of life and lower risk of psychological distress. Meanwhile, results were mixed for racial/ethnic background: Asian respondents had a consistently higher risk of lower quality of life, while Black/African American respondents had a consistently lower risk of psychological distress. Not surprisingly, better health status was consistently associated with better quality of life and less risk of psychological distress. And, living in the North Central/Midwest and South were associated with better quality of life compared with those in the Northeast. Policies and programs must not only pay attention to the unique challenges and opportunities inherent in different living arrangements, but they must be tailored to meet the various needs of a diverse population of older adults.
This paper also illustrates the importance of looking at multiple measures of well-being for older adults. Measuring only quality of life or psychological distress would lead to incomplete conclusions. While the two measures are related, more robust differences between living arrangements can be observed for quality of life. This may be because older adults are less likely than their younger counterparts to report depressive symptoms and psychological distress (Fiske et al., 2009). Therefore, using only the latter measures may miss important differences in older adults’ psychological well-being.
While this paper demonstrates clear differences between older adults’ well-being based on their living arrangements and gender, it has important limitations to consider. First, the cross-sectional nature of the data do not allow for identification of those adults who have moved or recently lost a spouse/partner. While living arrangements themselves may drive well-being, it is also important to consider the potential effects of loss of one’s home or partner. Future research should employ longitudinal data to control for the impact of moving from one residence to another or losing a spouse/partner. Additionally, the cross-sectional nature of the analyses makes it impossible to determine causality. While this paper demonstrates a clear association between living arrangements and psychological well-being, it is not possible to ascertain the direction of the effect. For example, for some older adults, living arrangements may lead to diminished well-being while for others, psychological distress may precipitate a move, as in the case of an adult child taking in parent with poor mental health. And, because this study looks only at the non-institutionalized population of older adults, it may be missing those most at risk of poor mental health outcomes and may be underestimating the impact of living arrangements. However, policies affecting nursing homes and other institutions differ in meaningful ways from those affecting the community-based population, making it important to focus research on the two groups separately.
Future research should further analyze the well-being of older adults living with others by type of household composition. It is possible that outcomes for those living with an adult child differ in meaningful ways from those living with a grandchild, other relative, or non-relative. As multi-generational households become more common, it will become increasingly important to understand variations in their effects. Finally, it is impossible to fully understand the impact of social capital for older adults through quantitative analysis alone. Qualitative and mixed methods may help to better understand the specific benefits and challenges derived from various living arrangements for different populations of older adults. With a quickly growing older adult population, the need for high quality research and responsive policies has never been more urgent. The response must include a robust understanding of demographic trends, health policy, and resulting health outcomes.
Acknowledgments
This manuscript was supported by the Integrated Health Interview Series project at the Minnesota Population Center (NIH grants #R01HD046697 and #R24HD041023), funded through grants from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD).
References
- AARP Public Policy Institute. Housing policy solutions to support aging in place. Washington, DC: AARP; 2010. [Google Scholar]
- Administration on Aging. A Profile of Older Americans: 2012. Washington, DC: AoA Administration for Community Living; 2012. [Google Scholar]
- Barker JC. Neighbors, friends, and other nonkin caregivers of community-living dependent elders. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2002;57(3):S158–S167. doi: 10.1093/geronb/57.3.s158. [DOI] [PubMed] [Google Scholar]
- Clarke SP, Frasure-Smith N, Lesperance F, Bourassa MG. Psychosocial factors as predictors of functional status at 1 year in patients with left ventricular dysfunction. Research in Nursing & Health. 2000;23(4):290–300. doi: 10.1002/1098-240x(200008)23:4<290::aid-nur5>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Davis MA. Living arrangements and dietary quality of older U.S. adults. Journal of the American Dietetic Association. 1990;90(12):1667–1672. [PubMed] [Google Scholar]
- Davis MA, Moritz DJ, Neuhaus JM, Barclay JD, Gee L. Living arrangements, changes in living arrangements, and survival among community dwelling older adults. American Journal of Public Health. 1997;87(3):371–377. doi: 10.2105/ajph.87.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MA, Murphy SP, Neuhaus JM, Gee L, Quiroga SS. Living arrangements affect dietary quality for U.S. adults aged 50 years and older: NHANES III 1988–1994. The Journal of Nutrition. 2000;130(9):2256–2264. doi: 10.1093/jn/130.9.2256. [DOI] [PubMed] [Google Scholar]
- de Jong Gierveld J, van Tilburg T. Living arrangements of older adults in the Netherlands and Italy: Coresidence values and behaviour and their consequences for loneliness. Journal of Cross-Cultural Gerontology. 1999;14(1):1–24. doi: 10.1023/a:1006600825693. [DOI] [PubMed] [Google Scholar]
- Dean A, Kolody B, Wood P, Matt GE. The influence of living alone on depresion in elderly Persons. Journal of Aging and Health. 1992;4(1):3–18. [Google Scholar]
- Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annual Review of Clinical Psychology. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychological Medicine. 2003;33(2):357–362. doi: 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- Gómez-Jancinto L, Hombrados-Mendieta I. Multiple effects of community and household crowding. Journal of Environmental Psychology. 2002;22(3):233–246. [Google Scholar]
- Greenfield EA, Russell D. Identifying living arrangements that heighten risk for loneliness in later life: Evidence from the U.S. national social life, health, and aging project. Journal of Applied Gerontology. 2011;30(4):524–534. [Google Scholar]
- Gurak DT, Kritz MM. Elderly Asian and Hispanic foreign- and native-born living arrangements: Accounting for differences. Research on Aging. 2010;32(5):567–594. doi: 10.1177/0164027510377160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes M, Gove WR. Living alone, social integration, and mental health. American Journal of Sociology. 1981;87(1):48–74. doi: 10.1086/227419. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ. Health in household context: Living arrangements and health in late middle age. Journal of Health and Social Behavior. 2002;43(1):1–21. [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Retooling for an Aging America: Building the Healthcare Workforce. Washington, DC: National Academy of Sciences; 2008. [Google Scholar]
- Issa P, Zedlewski SR. Poverty among Older Americans, 2009. Washington, DC: The Urban Institute; 2011. [Google Scholar]
- Joutsenniemi K, Martelin T, Martikainen P, Pirkola S, Koskinen S. Living arrangements and mental health in Finland. Journal of Epidemiology and Community Health. 2006;60(6):468–475. doi: 10.1136/jech.2005.040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Social ties and mental health. Journal of Urban Health : Bulletin of the New York Academy of Medicine. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Klinenberg E. Heat wave: A social autopsy of disaster in Chicago. Chicago, IL: University of Chicago Press; 2003. [DOI] [PubMed] [Google Scholar]
- Klinenberg E. Going solo: The extraordinary rise and surprising appeal of living alone. New York, NY: The Penguin Press; 2012. [Google Scholar]
- Koster A, Bosma H, Kempen GIJM, Penninx BWJH, Beekman ATF, Deeg DJH, van Eijk JThM. Socioeconomic differences in incident depression in older adults: The role of psychosocial factors, physical health status, and behavioral factors. Journal of Psychosomatic Research. 2006;61(5):619–627. doi: 10.1016/j.jpsychores.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Lim K, Taylor L. Factors associated with physical activity among older people - a population-based study. Preventive Medicine. 2005;40(1):33–40. doi: 10.1016/j.ypmed.2004.04.046. [DOI] [PubMed] [Google Scholar]
- Locher JL, Ritchie CS, Roth DL, Baker PS, Bodner EV, Allman RM. Social isolation, support, and capital and nutritional risk in an older sample: Ethnic and gender differences. Social Science & Medicine (1982) 2005;60(4):747–761. doi: 10.1016/j.socscimed.2004.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loe M. Aging our way: Lessons for living from 85 and beyond. New York, NY: Oxford University Press; 2011. [Google Scholar]
- McGuire LC, Strine TW, Vachirasuclekha S, Anderson LA, Berry JT, Mokdad AH. Modifiable characteristics of a healthy lifestyle and chronic health conditions in older adults with or without serious psychological distress, 2007 Behavioral Risk Factor Surveillance System. International Journal of Public Health. 2009;54(Suppl 1):84–93. doi: 10.1007/s00038-009-0011-4. [DOI] [PubMed] [Google Scholar]
- Michael YL, Berkman LF, Colditz GA, Kawachi I. Living arrangements, social integration, and change in functional health status. American Journal of Epidemiology. 2001;153(2):123–131. doi: 10.1093/aje/153.2.123. [DOI] [PubMed] [Google Scholar]
- Mui AC. Living alone and depression among older Chinese immigrants. Journal of Gerontological Social Work. 1999;30(3–4):147–166. [Google Scholar]
- National Center for Health Statistics. NHIS survey description. 2011 Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf.
- National Institute of Mental Health (NIMH) Older adults: Depression and suicide facts (fact sheet) 2007 Retrieved from http://www.nimh.nih.gov/health/publications/older-adults-depression-and-suicide-facts-fact-sheet/index.shtml.
- Office of Management and Budget (OMB) Standards for the classification of federal data on race and ethnicity. 2010 Retrieved 2/13, 2011. [Google Scholar]
- Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18(2):250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging. 2011;26(1):1–14. doi: 10.1037/a0021863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt LA. Serious psychological distress, as measured by the K6, and mortality. Annals of Epidemiology. 2009;19(3):202–209. doi: 10.1016/j.annepidem.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Robison J, Fortinsky R, Kleppinger A, Shugrue N, Porter M. A broader view of family caregiving: Effects of caregiving and caregiver conditions on depressive symptoms, health, work, and social isolation. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2009;64(6):788–798. doi: 10.1093/geronb/gbp015. [DOI] [PubMed] [Google Scholar]
- Regoeczi WC. Crowding in context: An examination of the differential responses of men and women to high-density living environments. Journal of Health and Social Behavior. 2008;49(3):254–268. doi: 10.1177/002214650804900302. [DOI] [PubMed] [Google Scholar]
- Ruggles SJ, Alexander T, Genadek K, Goeken R, Schroeder MB, Sobek M. Integrated public use microdata series: Version 5.0 [machine-readable database] Minneapolis, MN: Minnesota Population Center [producer and distributer]; 2010. [Google Scholar]
- Russell D. Living arrangements, social integration, and loneliness in later life: The case of physical disability. Journal of Health and Social Behavior. 2009;50(4):460–475. doi: 10.1177/002214650905000406. [DOI] [PubMed] [Google Scholar]
- Sereny M. Living arrangements of older adults in China: The interplay among preferences, realities, and health. Research on Aging. 2011;33(2):172–204. [Google Scholar]
- Shih M, Hootman JM, Strine TW, Chapman DP, Brady TJ. Serious psychological distress in U.S. adults with arthritis. Journal of General Internal Medicine. 2006;21(11):1160–1166. doi: 10.1111/j.1525-1497.2006.00573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein M, Cong Z, Li S. Intergenerational transfers and living arrangements of older people in rural china: Consequences for psychological well-being. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2006;61(5):S256–66. doi: 10.1093/geronb/61.5.s256. [DOI] [PubMed] [Google Scholar]
- Sorkin DH, Pham E, Ngo-Metzger Q. Racial and ethnic differences in the mental health needs and access to care of older adults in California. Journal of the American Geriatrics Society. 2009;57(12):2311–2317. doi: 10.1111/j.1532-5415.2009.02573.x. [DOI] [PubMed] [Google Scholar]
- Sun X, Lucas H, Meng Q, Zhang Y. Associations between living arrangements and health-related quality of life of urban elderly people: A study from China. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2011;20(3):359–369. doi: 10.1007/s11136-010-9752-z. [DOI] [PubMed] [Google Scholar]
- Taylor P, Passel J, Fry R, Morin R, Wang W, Velasco G, Dockterman D. The return of the multi-generational family household. Washington, DC: Pew Research Center; 2010. [Google Scholar]
- The Federal Interagency Forum on Aging-Related Statistics. Older Americans 2010: Key indicators of well-being. 2010 Retrieved from http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2010_Documents/docs/OA_2010.pdf.
- Waite L, Das A. Families, social life, and well-being at older ages. Demography. 2010;47(1):S87–S109. doi: 10.1353/dem.2010.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherell JL, Petkus AJ, McChesney K, Stein MB, Judd PH, Rockwell E, Patterson TL. Older adults are less accurate than younger adults at identifying symptoms of anxiety and depression. The Journal of Nervous and Mental Disease. 2009;197(8):623–626. doi: 10.1097/NMD.0b013e3181b0c081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth JM, Chen P. Immigrant status, living arrangements, and depressive symptoms among middle-aged and older adults. Journal of Gerontology: Social Sciences. 2003;58(5):S305–S313. doi: 10.1093/geronb/58.5.s305. [DOI] [PubMed] [Google Scholar]