Abstract
Background
Meniscus allograft transplantation (MAT) is primarily undertaken to relieve the symptoms associated with meniscal deficiencies. However, its ability to restore normal knee joint contact mechanics under physiological loads is still unclear.
Purpose
To quantify the dynamic contact mechanics associated with 2 commonly used fixation techniques in MAT of the medial compartment: transosseous suture fixation via bone plugs and suture-only fixation at the horns.
Study Design
Controlled laboratory study.
Methods
Physiological loads to mimic gait were applied across 7 human cadaveric knees on a simulator. A sensor placed on the medial tibial plateau recorded dynamic contact stresses under the following conditions: (1) intact meniscus, (2) MAT using transosseous suture fixation via bone plugs at the anterior and posterior horns, (3) MAT using suture-only fixation, and (4) total medial meniscectomy. A “remove-replace” procedure was performed to place the same autograft for both MAT conditions to minimize the variability in graft size, geometry, and material property and to isolate the effects of the fixation technique. Contact stress, contact area, and weighted center of contact stress (WCoCS) were quantified on the medial plateau throughout the stance phase.
Results
Knee joint contact mechanics were sensitive to the meniscal condition primarily during the first half of the gait cycle. After meniscectomy, the mean peak contact stress increased from 4.2 ± 1.2 MPa to 6.2 ± 1.0 MPa (P = .04), and the mean contact area decreased from 546 ± 132 mm2 to 192 ± 122 mm2 (P = .01) compared with the intact meniscus during early stance (14% of the gait cycle). After MAT, the mean contact stress significantly decreased with bone plug fixation (5.0 ± 0.7 MPa) but not with suture-only fixation (5.9 ± 0.7 MPa). Both fixation techniques partially restored the contact area, but bone plug fixation restored it closer to the intact condition. The location of WCoCS in the central cartilage region (not covered by the meniscus) shifted peripherally throughout the stance phase. Bone plug fixation exhibited correction to this peripheral offset, but suture-only fixation did not.
Conclusion
Under dynamic loading, transosseous fixation at the meniscal horns provides superior load distribution at the involved knee compartment after meniscal transplantation compared with suture-only fixation. Particular attention should be directed to the ability of medial MAT to function during the early stance phase.
Clinical Relevance
Transosseous fixation via bone plugs provides superior load distribution of a transplanted meniscal allograft compared with suture fixation alone at time zero.
Keywords: meniscus, sports trauma, knee, mechanics, simulated gait
The meniscus of the knee facilitates joint articulation by providing congruency, joint stability, proprioception, and lubrication.27 After meniscal tears, the changes that occur in knee mechanics have been implicated as a primary cause of early-onset osteoarthritis.29,30 Meniscus allograft transplantation (MAT) is undertaken primarily to relieve pain; in addition, an underlying intention is to redistribute the joint loads across the involved compartment in the hope of restoring normal contact mechanics in the transplanted meniscal joint. While MAT has demonstrated pain relief and functional improvement in up to 70% of patients,42 the ability of this surgical procedure to restore normal knee contact mechanics during daily activities has yet to be investigated.12
Many variables have been identified as factors that can influence the clinical performance of MAT (graft size, bone geometry, fixation technique, level of activity, limb alignment, etc),4,14,35 but the fixation technique is most readily under the control of the operating surgeon.12,28 There are 2 fixation modalities commonly used in medial MAT: (1) transosseous suture fixation via bone plugs in which 2 bone plugs are prepared at the anterior and posterior horns of the graft,35 and (2) suture-only fixation at the meniscal horns in which the graft is sutured at the anterior and posterior horns and those sutures are drawn through transtibial bone tunnels and tied over a bone bridge. A recent prospective study on 88 patients who underwent MAT showed that meniscal allografts using bony fixation had a reduced incidence of extrusion compared with those using suture-only fixation.1 Previous static, unidirectional, cadaveric studies by Alhalki et al4,5 have also shown that by using bone plug fixation, the knee contact stress and contact area were closer to normal than for suture-only fixation in the medial tibial compartment; similar results were also found in the lateral compartment.31 By using a finite element model that mimicked uniaxial forces across the knee joint, Haut Donahue et al17 demonstrated that among all variables, stiffness of the horn attachment (≥2000 N/mm) was vital for re-creating the “normal” contact stresses on the tibial plateau, whereas Hunt et al18 found no significant difference in the pull-out strength of bone plug versus suture-only fixation of the posterior horn. While these studies shed light on the effect of MAT fixation on performance under simplified, unidirectional, and static loading conditions related to full extension, the effect of fixation on the ability of MAT to carry and distribute joint loads during dynamic physiological loading conditions such as gait, during which higher flexion angles are simulated, is still unclear.
The objective of this study was to quantify the dynamic contact mechanics associated with 2 commonly utilized graft fixation techniques in MAT of the medial compartment: transosseous suture fixation via bone plugs and suture-only fixation at the meniscal horns. It was hypothesized that both techniques would improve knee joint contact mechanics relative to the meniscectomized condition but that only transosseous suture fixation via bone plugs would restore intact knee contact mechanics. To test these hypotheses, the peak contact stress, weighted center of contact stress (WCoCS), and contact area on the medial tibial plateau of human cadaveric knees were characterized throughout the stance phase of simulated gait.
MATERIALS AND METHODS
Dynamic Cadaveric Knee Model
A modified load-controlled Stanmore KC Knee Joint Simulator (University College London, London, UK) was used for this study.9,13,41 It was programmed to apply dynamic axial forces, anterior/posterior forces, internal/external torques, and controlled flexion angles (Figure 1) to mimic the activity of gait, according to International Organization for Standardization 14243-1.40 Seven fresh-frozen cadaveric knees were inspected for visible evidence of chondral defects and meniscal or ligament damage, and only those with a normal appearance were selected for this study. The knees were stripped of overlying soft tissue down to the level of the joint capsule. The capsule and all ligaments were maximally preserved around the knee, while the patella and extensor mechanism were carefully removed. The femur and tibia were transected using an oscillating saw, leaving approximately 10 cm above and below the joint line. A 2.5-mm Kirschner wire was drilled through the epicondylar axis of the femur using fluoroscopic guidance. The pin was aligned with the flexion/extension axis of the knee simulator, and the tibia-fibula and femur were potted into their respective fixtures using polymethyl methacrylate bone cement (Figure 2, A and B).
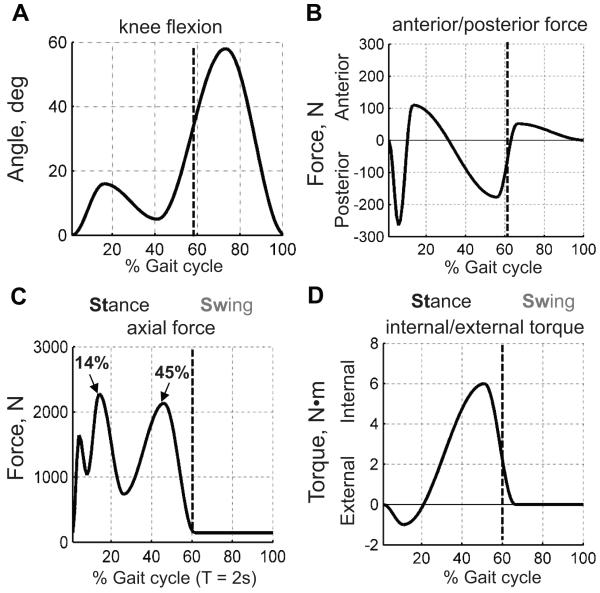
Figure 1.
Inputs of the dynamic knee simulator. The simulator applies (A) flexion/extension rotation, (B) anterior/posterior force, (C) axial force, and (D) internal/external torque. The forces and torques were applied on the tibia, and flexion and extension were applied on the femur. The other degrees of freedom, varus/valgus rotation and medial/lateral translation, were not controlled.
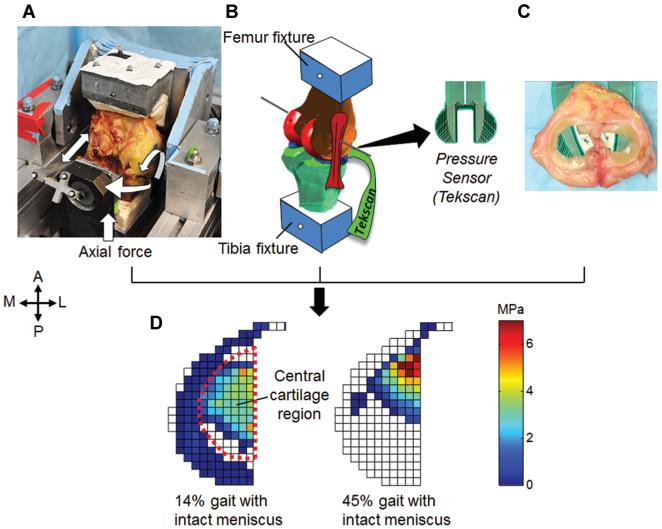
Figure 2.
Cadaveric model. (A) Photograph of a specimen on the Stanmore knee simulator. The simulator was driven by gait loads as described in Figure 1. (B) A Kirschner wire was pinned through the geometric epicondylar axis with the guidance of radiography and was used to align the knee position on the simulator. (C) The knee was augmented with a pressure sensor (Tekscan), while the soft tissues were carefully preserved (photograph was taken after dissection of the knee). (D) Real-time contact stresses on the tibial plateaus were collected at 100 Hz.
The normal contact stress across the tibial plateau was measured using a thin electronic sensor containing an array of piezoelectric pressure-sensing elements sealed within a thin plastic sheet (Model 4010N, Tekscan Inc, Boston, Massachusetts, USA) (Figure 2C). After calibration, the sensor had a mean saturation pressure of 9.22 ± 1.50 MPa and sensitivity of 0.05 MPa. The sensor was augmented with plastic adhesive tape to serve as tabs for suture fixation. It was sealed between 2 layers of Tegaderm adhesive dressing (3M Inc, Minneapolis, Minnesota, USA) and conditioned under 90 psi in an air bladder. Calibration was performed on a servohydraulic materials testing machine (MTS, Eden Prairie, Minnesota, USA) under 2 loads, approximating 20% and 80% of the maximum load expected during testing, after a “power calibration” procedure provided with the system software.11 Approximately 1-cm incisions were made in the meniscotibial ligaments and joint capsule tissue anteriorly and posteriorly of both menisci. The sensor was slightly curled at the edge of the maximum width, and the knee was flexed so that a gap opened at the anterior side of the knee joint. This method allowed the sensor to be passed underneath the menisci from anterior to posterior with minimal disruption of the meniscocapsular attachments. The sensor tabs were sutured in place using 3-0 Ethibond sutures (Ethicon Inc, Somerville, New Jersey, USA) via the tibial insertion of the anterior cruciate ligament (ACL) and the posteroinferior capsule. Sensor placement and position were checked between conditions using a custom caliper, which was attached through a drill hole in the cement mantle of the tibial potting block.
Test Conditions
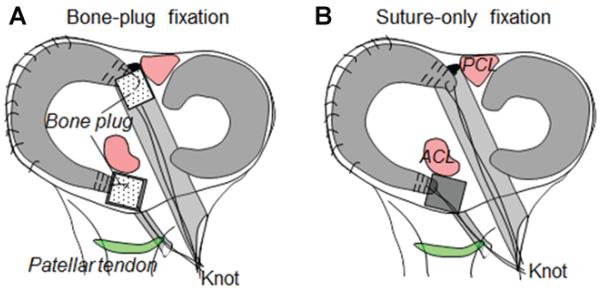
Contact mechanics were quantified for each of the following sequential conditions: (1) intact meniscus, (2) transosseous suture fixation via bone plugs (Figure 3A), (3) bone tunnel suture fixation in which the bone plugs were detached from the meniscal horns and the meniscus was fixed at the horns with sutures passing through the bone tunnels (hereafter called suture-only fixation) (Figure 3B), and (4) medial meniscectomy. To isolate the effects of the fixation technique on knee joint contact mechanics, we performed a “remove-replace” method in which the native medial meniscus was excised out of the knee in its entirety and then fixed back in place using those 2 different fixation methods described above.
Figure 3.
Schematic diagram of the fixation procedures. (A) Transosseous suture fixation via bone plugs. (B) Bone tunnel suture fixation.
To remove the medial meniscus, a No. 15 blade was used to circumferentially release the medial meniscus at the meniscocapsular junction. Anterior and posterior horn attachment sites were osteotomized to preserve bone plugs that were later used for bone plug fixation. The anterior bone plug was created using a quarter-inch osteotome and a mallet to create a 1 × 1 × 1–cm3 bone plug centered on the attachment site of the anterior horn of the medial meniscus. The center position of the posterior horn attachment was first drilled with a 2.7-mm guide pin using an ACL tibial guide for pin placement. An incision was created in the capsule just medial to the posterior cruciate ligament (PCL), and the PCL was retracted laterally. The tibial guide was brought in anteriorly through the inter-condylar notch, and the pin was drilled from the proximal lateral tibia. This guide pin was then overdrilled with a cannulated coring reamer (Arthrex, Naples, Florida, USA), which produced a cylindrical bone plug of 10 mm in diameter. This same 2.7-mm guide pin was also used to drill a bone tunnel through the base of the anterior bone plug to pass sutures down through the bone plug and into the proximal tibia.
Before testing the MAT conditions, the removed meniscus was prepared by placing No. 5 Ethibond sutures through the 2.7-mm tunnel at the center of each bone plug and a separate set of sutures through the anterior and posterior horns of the meniscus using a modified Kessler configuration.21 In brief, this configuration was created as follows: a suture was passed through the sectioned surface of the meniscal attachment, looped out through the outer edge at the interface between the attachment and the horn, traversed through midsubstance meniscal tissue to the inner edge, and finally passed back through the attachment, exiting through the cut surface. For the bone plug condition, the bone plugs were reduced back to their respective insertions using the bone plug sutures (BPS). The meniscus was repaired back to the capsule using 2-0 Ethibond sutures placed in a horizontal mattress configuration spaced evenly into the anterior horn, body, and posterior horn of the meniscus. After the BPS condition was tested, the bone plugs were subsequently detached from both horns using a No. 15 blade, leaving the bone plugs in situ. The modified Kessler sutures previously placed through the anterior and posterior horns were passed through the previously created 2.7-mm tunnels and tensioned manually until the anterior and posterior horns were anatomically reduced to their insertion sites. These sutures were then tied to each other over a bone bridge and then tested (suture-only condition). After this, the medial meniscus and sutures were completely removed from the knee, and the meniscectomy condition was tested.
Outcome Measures and Data Analysis
For each specimen and each test condition, the contact stress perpendicular to the surface of the sensor at each sensing element across the tibial plateau was recorded during continuous gait cycles at 100 Hz. Because the sensor and knee simulator reached steady state within 4 to 7 gait cycles,13 20 continuous gait cycles were collected, and the mean of the last 3 cycles was used. The following parameters were quantified using a custom Matlab program (MathWorks Inc, Natick, Massachusetts, USA): (1) peak contact stress, (2) total contact area, and (3) WCoCS throughout the stance phase of gait.16 The term “weighted center of contact stress” was developed as a surrogate for the location of the center of contact, and it takes into account not only the regions on the tibial plateau that experience contact but also the magnitude of contact stress experienced across the plateau. Greater weights were assigned to sensels with higher contact stresses and smaller weights to peripheral sensels with lower contact stresses. In this way, WCoCS takes into account both the locations and magnitudes of the contact stresses (equation 1) and is therefore more robust, reproducible, and less influenced by lower stresses that occur at the periphery of the joint:
| (1) |
where si denotes the contact stress at sensel i, and pi denotes the sensel position in the local coordinate system (Figure 2D). By using this method, the trajectories of the WCoCS along the peripheral/central and anterior/posterior directions were determined.
To measure the WCoCS in the central region of tibial articular cartilage, which is not normally covered by the meniscus, the region was defined by tracing the boundary of the meniscus on the stress map at 14% of gait when the medial meniscus was maximally loaded (Figure 2D). An assumption was made here that the meniscus’ movement on the medial plateau was small compared with the femoral condyle’s movement.
Statistical Analysis
The results of peak contact stress and contact area were compared between intact, meniscectomized, and MAT conditions using the Kruskal-Wallis test (nonparametric 1-way analysis of variance [ANOVA]). The WCoCS at different meniscal conditions was compared with the intact meniscus using the Mann-Whitney test. For the Kruskal-Wallis test with a significant χ2 statistic, post hoc analysis was performed by using the Dunn multiple comparison test. The level of significance was set at P < .05.
RESULTS
Among the 7 knees, all conditions (intact, bone plug, suture only, and meniscectomy) were successfully tested for 5 knees. A BPS trial was missing from 1 knee because of an accidental cut of the bone plug at 1 meniscal horn. For another, knee sensor dislocation occurred during meniscectomy, so this condition for this knee was excluded from data analysis. To determine if we had sufficient power to detect the increase in peak contact stress at 14% of the gait cycle, a post hoc power analysis was performed using an α of .05 and a sample size of ± (given 1 knee was missing the BPS trial and another was missing the meniscectomy trial) following a 1-way ANOVA study design. The analysis revealed that the power of our study was 95%, assuming a standard deviation of 0.89 in each group.
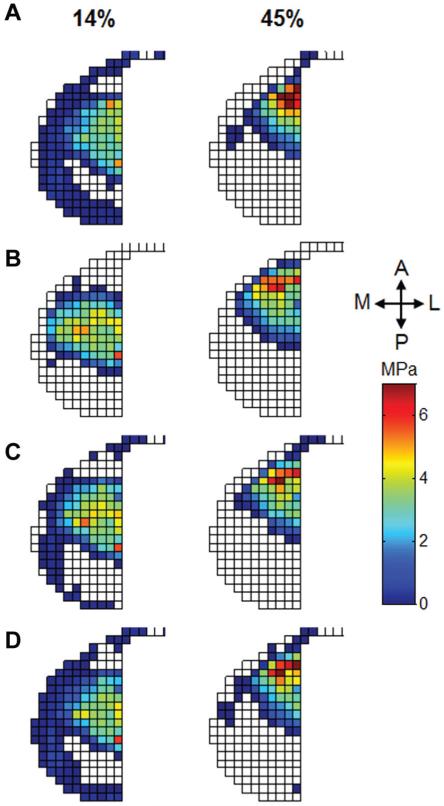
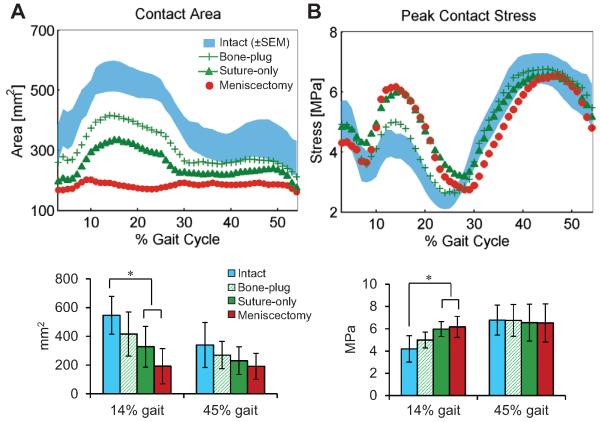
After medial meniscectomy, the normal distribution of contact stresses on the medial plateau was disrupted as shown in the stress maps of a typical specimen (Figure 4, A and B). Collectively, the mean contact area was significantly reduced primarily during the early stance phase (from 546 ± 132 mm2 to 192 ± 122 mm2; P = .01) when the axial load reached its first peak (14% of the gait cycle) (Figure 5A). During this phase, BPS fixation increased the contact area more than suture-only fixation, although the contact area was not fully restored by either procedure. During the late stance phase, however, the contact area was not significantly affected by meniscal condition (from 30% of the gait cycle to toe-off). At 14% of the gait cycle, the mean peak contact stress on the medial tibial plateau significantly increased from 4.2 ± 1.2 MPa to 6.2 ± 1.0 MPa (P < .01) after meniscectomy (Figure 5B). Only BPS fixation (vs suture-only fixation) successfully reduced the peak contact stress during the early stance phase. During the second half of the stance phase, however, the peak contact stress was not significantly affected by either meniscectomy or meniscal transplantation.
Figure 4.
Stress maps on the medial plateau for a typical knee under different meniscal conditions at 14% and 45% of the gait cycle. (A) The intact knee. A reduction in the contact area was observed after medial meniscectomy (B) at 14% of gait, while minimal changes were found at 45% of gait. Compared with suture-only fixation (C), bone plug fixation (D) exhibited better restoration in the contact area.
Figure 5.
(A) Reduction in the contact area and (B) increase in peak contact stress across the medial tibial plateau throughout the stance phase of gait. The plots on the top show the mean curves for each condition; the shaded area of the intact condition indicates the standard error (shaded areas on the other curves were removed for better readability). The plots on the bottom show the values (mean ± standard deviation) of each condition at 14% and 45% of gait. *Statistically significant difference (P < .05).
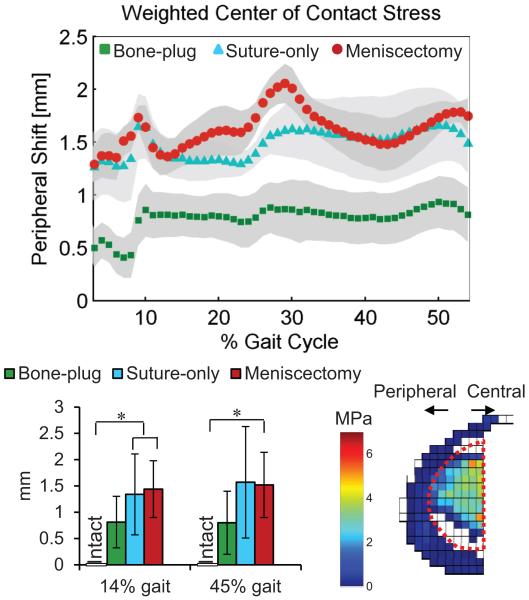
After medial meniscectomy, the location of the WCoCS significantly shifted (P = .02) to the peripheral zone of the tibial plateau relative to the intact knees throughout the whole stance phase (Figure 6), while there was no obvious change in the anterior/posterior direction. Only BPS fixation exhibited an effective correction to this peripheral offset.
Figure 6.
Peripheral shift (relative to the intact condition) of the weighted center of contact stress within the central cartilage region throughout the stance phase of gait. The plot on the top shows the mean curve for each condition; the shaded area of the intact condition indicates the standard error. The plot on the bottom shows the peripheral shift (mean ± standard deviation) of each condition at 14% and 45% of gait. *Statistically significant difference (P < .05) compared with the baseline intact condition.
DISCUSSION
Total medial meniscectomy resulted in an increase in peak contact stress and a decrease in the contact area during the first half of the gait cycle. Meniscectomy also resulted in a significant shift in the location of the WCoCS from the central to peripheral zone on medial tibial cartilage, which is uncovered by meniscectomy. The findings support our hypothesis that meniscal transplantation would result in some restoration of contact mechanics, but the degree of restoration was dependent on the method of fixation. Transosseous fixation using bone plugs at both the anterior and posterior horns resulted in superior contact mechanics that more closely approximated that of the intact condition than fixation with sutures alone.
Previous studies designed to assess the functional mechanics of meniscal grafts have typically used static or quasistatic uniaxial loads that ranged in magnitude from 1 to 2 kN.4,5,14,20,33 While the magnitudes of the applied axial force in those studies were in the physiological range, the tests did not capture the multidirectional dynamic loading environment of the knee joint. Significantly increased peak contact stresses and decreased contact areas have also been previously reported after full resection of the posterior horn of the medial meniscus under static axial loads at different flexion angles (0°, 30°, and 60°).25,38 Yet, in reality, the alteration in secondary knee motions, such as changes in internal/external rotation and anterior/posterior translation during walking, should also be considered. As the medial meniscus plays an important role in limiting anterior/posterior tibial translation,3,39 predictable changes in kinematic changes, primarily in anterior/posterior translation,7 might be expected to occur after meniscectomy. Thus, a more sophisticated load setting that incorporates the multidirectional forces experienced at the knee during physiological loading situations would help us to better understand the problems after meniscal injuries and after surgical interventions. We have previously modified a knee simulator to apply synchronized axial force, internal/external torque, and anterior/posterior force as a function of flexion angle that simulates gait and used it to assess the functional mechanics of meniscal tears of the posterior aspect of the medial and lateral menisci.9,10 In the current study, we augmented the model with a sensor capable of recording contact stresses at a high sampling frequency (100 Hz), thus allowing us to study the effect of meniscal transplantation during the dynamic loading environment of gait (gait cycle = 2 seconds), which considered segmental inertia and joint viscosity.
As expected, the peak contact stress increased significantly after meniscectomy by approximately 48% compared with that of the intact condition. This is close to that reported by Dienst et al,14 who found a 50% to 60% increase in the peak contact stress with the knee in full extension and at 30° of flexion, but is lower than that measured by Paletta et al,33 who quantified increases of up to 200% after meniscectomy, and by Baratz et al,8 who found an approximate 235% increase. The contact area on the tibial surface also decreased with meniscectomy (40%-65%), which is within the range previously reported.5,14,33 In addition, we have demonstrated that the changes in contact stress and contact area associated with meniscectomy were most pronounced during the first half of stance, which has not thus far been reported in the literature. This finding indicates that the medial meniscus mainly carries loads during the early stance phase of walking, which is also shown in the stress maps (14% vs 45% of the gait cycle) (Figure 4). Our finding is consistent with that of a recent study in which the authors reported that cartilage under the posterior horn of the medial meniscus mainly carries loads during the early stance phase.44 During early stance, the tibia was subjected to an anteriorly directed force, a low axial rotatory torque (Figure 1), and a low flexion angle. This combination of forces resulted in a situation in which the femoral condyles were supported mainly by the posterior aspects of the menisci, resulting in a higher force transmitted by the medial meniscus. However, after 30% of the gait cycle, the direction of the anterior/posterior force shifted posteriorly, while the internal rotatory torque increased, causing an increase in internal rotation of the tibia, as has been reported in previous in vivo kinematic studies.37,45 Tibial internal rotation tends to move the medial tibiofemoral contact location anteriorly.22,23 Because the asymmetric “C-shaped” medial meniscus is much thinner anteriorly and less readily absorbs the joint load compared with the posterior area, the internally rotated tibial position during the late stance phase might have unloaded the posterior portion of the medial meniscus from the femoral condyle.
Between these 2 commonly utilized fixation techniques, BPS fixation better restored knee joint contact mechanics than suture-only fixation in the early phase of stance. Given the wedge-shaped geometry of the meniscus, stiff fixation sites are required to avoid the tendency of the meniscus to extrude under high axial loads.4,17 While the exact mechanism by which changes in contact mechanics lead to tissue degeneration is unclear, we sought to assess if the location of contact was significantly affected by the meniscal condition. Thus, we developed the term “WCoCS,” which takes into account both the stress magnitude at each sensing element and its location. By using this term as opposed to the geometric center of contact, the influence of sensels that are marginally loaded will be minimized. This allows for more accurate tracking of the center of contact when the meniscus is partially/minimally loaded. We observed that the mean curve of the WCoCS moved from a central position on the medial tibial plateau in the intact condition to a more peripheral location after meniscectomy. This change in location occurred throughout the entirety of the stance phase and varied little through the cycle. No changes in the anterior/posterior position of the WCoCS were noted throughout the stance phase of gait. Once again, bone plug fixation showed an improvement compared with the suture-only fixation and meniscectomy conditions in restoring a more normal WCoCS. The alteration of the contact location shifts the high contact stresses to the peripheral zones of the medial tibial plateau, where articular cartilage is thinner compared with that in the central zones,6,26 which may have important implications for chondral degeneration in meniscus-deficient patients.34
The method of surgical fixation of whole meniscal allografts remains controversial. This is in part because numerous methods of meniscal transplant fixation techniques have been described and used in different clinical situations.24,32,36 These include meniscal allografts fixed with sutures alone, separate anterior and posterior bone plugs, and various machined bone bridges (dove-tail, key-hole, bridge-in-slot) between the anterior and posterior horns, which are slotted into the tibial plateau for fixation. Clinically, the surgical goal of MAT, to relieve symptoms in the meniscus-deficient compartment, has been achieved with equal efficacy by both fixation techniques in the short to medium term.2 Prospective randomized controlled trials projected from the medium to long term with a focus on objective quantifiable cartilage/joint health status are required to comprehensively assess the ability of both fixation techniques to demonstrate a chondroprotective effect. Unfortunately, these studies are lacking. In the interim, any attempts to relate joint health to commonly reported clinical subscales in long-term MAT studies are undermined by the fact that clinical scores have not been shown to directly correlate with radiological or magnetic resonance imaging parameters of cartilage status,43 that there exists considerable variability in patient populations, and that there is a lack of consensus regarding objective outcome criteria after MAT.15,19 In this basic science study, we designed a self-controlled comparison aimed at isolating the effect of fixation technique on postoperative outcomes. The methods of fixation tested in this study were selected because, unlike in the lateral meniscus where the anterior and posterior horns are in close proximity and the preferred technique is to use a single machined bone bridge, in the medial meniscus, both methods of fixation are common, but there has been little clinical evidence to differentiate the functional mechanics of these 2 techniques.
Several limitations need to be recognized in this study. First, to provide an element of parity in graft positioning and for experimental convenience, we “reused” the 10-mm bone tunnel of the posterior horn for the suture pathway in suture-only fixation. Yet, we did not observe any “off-center” displacement of the meniscus as the sutures are tied over the bone bridge. Second, to minimize the variability in graft size, geometry, and material property and to isolate the effects of the fixation technique, we performed a “remove-replace” method in which we used the same autograft for both MAT conditions. However, the “ideal” meniscal autograft with the geometry and material properties exactly matching those of the original tissue is not practical to obtain in a clinical setting. Third, there was no standardization of the tensioning procedure for sutures that were used in both the bone plug and the suture-only conditions. We manually tensioned both the anterior and posterior horn suture limbs and then tied them together. Finally, while the WCoCS is a numerical representation of the location of the center of contact stress, it is influenced by the magnitude of contact stresses, particularly in the peripheral regions of the joint.
CONCLUSION
Transosseous fixation via bone plugs provides superior load distribution of a transplanted meniscal allograft compared with suture fixation alone at time zero. The meniscus functions to carry joint loads mainly in the early phase of stance, suggesting that particular attention should be directed to the ability of meniscal repair or replacement strategies to function during this phase.
ACKNOWLEDGMENT
The authors thank the Clark & Kirby Foundations and the Russell Warren Chair in Tissue Engineering. They also thank Joe Nguyen for help with statistical analysis.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under award numbers R01AR057343, T32-AR007281-27, and KL2 TR000458. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1.Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40(7):1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 2.Abat F, Gelber PE, Erquicia JI, Tey M, Gonzalez-Lucena G, Monllau JC. Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1516–1522. doi: 10.1007/s00167-012-2032-4. [DOI] [PubMed] [Google Scholar]
- 3.Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39(10):2187–2193. doi: 10.1177/0363546511416597. [DOI] [PubMed] [Google Scholar]
- 4.Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med. 1999;27(3):320–328. doi: 10.1177/03635465990270030901. [DOI] [PubMed] [Google Scholar]
- 5.Alhalki MM, Hull ML, Howell SM. Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft: a human cadaveric study. Am J Sports Med. 2000;28(3):370–376. doi: 10.1177/03635465000280031501. [DOI] [PubMed] [Google Scholar]
- 6.Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009;91(Suppl 1):95–101. doi: 10.2106/JBJS.H.01408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arno S, Hadley S, Campbell KA, et al. The effect of arthroscopic partial medial meniscectomy on tibiofemoral stability. Am J Sports Med. 2013;41(1):73–79. doi: 10.1177/0363546512464482. [DOI] [PubMed] [Google Scholar]
- 8.Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14(4):270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 9.Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92(6):1398–1408. doi: 10.2106/JBJS.I.00539. [DOI] [PubMed] [Google Scholar]
- 10.Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of radial tears of the lateral meniscus: implications for treatment. Arthroscopy. 2012;28(3):372–381. doi: 10.1016/j.arthro.2011.08.287. [DOI] [PubMed] [Google Scholar]
- 11.Brimacombe JM, Wilson DR, Hodgson AJ, Ho KC, Anglin C. Effect of calibration method on Tekscan sensor accuracy. J Biomech Eng. 2009;131(3):034503. doi: 10.1115/1.3005165. [DOI] [PubMed] [Google Scholar]
- 12.Brophy RH, Matava MJ. Surgical options for meniscal replacement. J Am Acad Orthop Surg. 2012;20(5):265–272. doi: 10.5435/JAAOS-20-05-265. [DOI] [PubMed] [Google Scholar]
- 13.Cottrell JM, Scholten P, Wanich T, Warren RF, Wright TM, Maher SA. A new technique to measure the dynamic contact pressures on the tibial plateau. J Biomech. 2008;41(10):2324–2329. doi: 10.1016/j.jbiomech.2008.04.024. [DOI] [PubMed] [Google Scholar]
- 14.Dienst M, Greis PE, Ellis BJ, Bachus KN, Burks RT. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med. 2007;35(1):34–42. doi: 10.1177/0363546506291404. [DOI] [PubMed] [Google Scholar]
- 15.Elattar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P. Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):147–157. doi: 10.1007/s00167-010-1351-6. [DOI] [PubMed] [Google Scholar]
- 16.Gilbert S, Chen T, Hutchinson ID, et al. Dynamic contact mechanics on the tibial plateau of the human knee during activities of daily living [published online November 16, 2013] J Biomech. doi: 10.1016/j.jbiomech.2013.11.003. doi:10.1016/j.jbiomech.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haut Donahue TL, Hull ML, Rashid MM, Jacobs CR. How the stiffness of meniscal attachments and meniscal material properties affect tibiofemoral contact pressure computed using a validated finite element model of the human knee joint. J Biomech. 2003;36(1):19–34. doi: 10.1016/s0021-9290(02)00305-6. [DOI] [PubMed] [Google Scholar]
- 18.Hunt S, Kaplan K, Ishak C, Kummer FJ, Meislin R. Bone plug versus suture fixation of the posterior horn in medial meniscal allograft transplantation: a biomechanical study. Bull NYU Hosp Joint Dis. 2008;66(1):22–26. [PubMed] [Google Scholar]
- 19.Hutchinson ID, Moran CJ, Potter HG, Warren RF, Rodeo SA. Restoration of the meniscus: form and function [published online August 22, 2013] Am J Sports Med. doi: 10.1177/0363546513498503. doi:10.1177/0363546513498503. [DOI] [PubMed] [Google Scholar]
- 20.Ihn JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993;17(4):214–218. doi: 10.1007/BF00194181. [DOI] [PubMed] [Google Scholar]
- 21.Kessler I, Nissim F. Primary repair without immobilization of flexor tendon division within the digital sheath: an experimental and clinical study. Acta Orthop Scand. 1969;40(5):587–601. doi: 10.3109/17453676908989524. [DOI] [PubMed] [Google Scholar]
- 22.Koo S, Andriacchi TP. The knee joint center of rotation is predominantly on the lateral side during normal walking. J Biomech. 2008;41(6):1269–1273. doi: 10.1016/j.jbiomech.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kozanek M, Hosseini A, Liu F, et al. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–1884. doi: 10.1016/j.jbiomech.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee AS, Kang RW, Kroin E, Verma NN, Cole BJ. Allograft meniscus transplantation. Sports Med Arthrosc. 2012;20(2):106–114. doi: 10.1097/JSA.0b013e318246f005. [DOI] [PubMed] [Google Scholar]
- 25.Lee SJ, Aadalen KJ, Malaviya P, et al. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34(8):1334–1344. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 26.Li G, Park SE, DeFrate LE, et al. The cartilage thickness distribution in the tibiofemoral joint and its correlation with cartilage-to-cartilage contact. Clin Biomech (Bristol, Avon) 2005;20(7):736–744. doi: 10.1016/j.clinbiomech.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011;32(30):7411–7431. doi: 10.1016/j.biomaterials.2011.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matava MJ. Meniscal allograft transplantation: a systematic review. Clin Orthop Relat Res. 2007;455:142–157. doi: 10.1097/BLO.0b013e318030c24e. [DOI] [PubMed] [Google Scholar]
- 29.McCann L, Ingham E, Jin Z, Fisher J. Influence of the meniscus on friction and degradation of cartilage in the natural knee joint. Osteoarthritis Cartilage. 2009;17(8):995–1000. doi: 10.1016/j.joca.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 30.McDermott I. Meniscal tears, repairs and replacement: their relevance to osteoarthritis of the knee. Br J Sports Med. 2011;45(4):292–297. doi: 10.1136/bjsm.2010.081257. [DOI] [PubMed] [Google Scholar]
- 31.McDermott ID, Lie DT, Edwards A, Bull AM, Amis AA. The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc. 2008;16(6):553–560. doi: 10.1007/s00167-008-0503-4. [DOI] [PubMed] [Google Scholar]
- 32.Packer JD, Rodeo SA. Meniscal allograft transplantation. Clin Sports Med. 2009;28(2):259–283. viii. doi: 10.1016/j.csm.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 33.Paletta GA, Jr, Manning T, Snell E, Parker R, Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee: a biomechanical study. Am J Sports Med. 1997;25(5):692–698. doi: 10.1177/036354659702500519. [DOI] [PubMed] [Google Scholar]
- 34.Potter HG, Rodeo SA, Wickiewicz TL, Warren RF. MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology. 1996;198(2):509–514. doi: 10.1148/radiology.198.2.8596858. [DOI] [PubMed] [Google Scholar]
- 35.Rodeo SA. Meniscal allografts: where do we stand? Am J Sports Med. 2001;29(2):246–261. doi: 10.1177/03635465010290022401. [DOI] [PubMed] [Google Scholar]
- 36.Saltzman BM, Bajaj S, Salata M, et al. Prospective long-term evaluation of meniscal allograft transplantation procedure: a minimum of 7-year follow-up. J Knee Surg. 2012;25(2):165–175. doi: 10.1055/s-0032-1313738. [DOI] [PubMed] [Google Scholar]
- 37.Scanlan SF, Chaudhari AM, Dyrby CO, Andriacchi TP. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech. 2010;43(9):1817–1822. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seitz AM, Lubomierski A, Friemert B, Ignatius A, Durselen L. Effect of partial meniscectomy at the medial posterior horn on tibiofemoral contact mechanics and meniscal hoop strains in human knees. J Orthop Res. 2012;30(6):934–942. doi: 10.1002/jor.22010. [DOI] [PubMed] [Google Scholar]
- 39.Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee: effects of partial versus total excision. J Bone Joint Surg Am. 1986;68(1):71–79. [PubMed] [Google Scholar]
- 40.Taylor SJ, Perry JS, Meswania JM, Donaldson N, Walker PS, Cannon SR. Telemetry of forces from proximal femoral replacements and relevance to fixation. J Biomech. 1997;30(3):225–234. doi: 10.1016/s0021-9290(96)00141-8. [DOI] [PubMed] [Google Scholar]
- 41.van Houtem M, Clough R, Khan A, Harrison M, Blunn GW. Validation of the soft tissue restraints in a force-controlled knee simulator. Proc Inst Mech Eng H. 2006;220(3):449–456. doi: 10.1243/09544119JEIM57. [DOI] [PubMed] [Google Scholar]
- 42.Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R. Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87(4):715–724. doi: 10.2106/JBJS.C.01344. [DOI] [PubMed] [Google Scholar]
- 43.Verdonk PC, Verstraete KL, Almqvist KF, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):694–706. doi: 10.1007/s00167-005-0033-2. [DOI] [PubMed] [Google Scholar]
- 44.Wang H, Chen T, Torzilli P, Warren R, Maher S. Dynamic contact stress patterns on the tibial plateaus during simulated gait: a novel application of normalized cross correlation. J Biomech. 2014;47(2):568–574. doi: 10.1016/j.jbiomech.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang H, Fleischli JE, Zheng NN. Transtibial versus anteromedial portal technique in single-bundle anterior cruciate ligament reconstruction: outcomes of knee joint kinematics during walking. Am J Sports Med. 2013;41(8):1847–1856. doi: 10.1177/0363546513490663. [DOI] [PubMed] [Google Scholar]