Abstract
Background:
Several dermoscopic findings in alopecia areata (AA) are characteristic and aid in the diagnosis of this disease. Studies evaluating the clinical significance of these findings in AA in dark-skinned individuals are sparse. There is no literature of correlation of dermoscopic findings to severity of disease.
Aims:
The aim was to determine the dermoscopic findings of AA in dark skinned individuals and to assess whether certain dermoscopic findings correlate with disease activity and severity.
Materials and Methods:
Totally 116 patients with AA were included in the study. After a thorough clinical history and examination to note type, severity and activity of the disease, dermoscopy was performed using a Heine Delta 20 dermoscope (Heine optotechnik,Herrsching, Germany) and the results were noted in a proforma. Statistical analysis was performed using SPSS13 software using appropriate statistical tools.
Results:
Dermoscopic findings were nearly similar to that described in western literature. Yellow dots (YDs) were found to be highly sensitive for diagnosis, increased frequency being seen in Indian prepubertal patients when compared with western literature. YDs/field of vision (FOV) were found more frequently in severe types of AA. There was no correlation of dermoscopic findings to severity of disease.
Conclusion:
Dermoscopic features are similar to that described in the literature. However, YDs are seen in higher frequency. YDs/FOV could serve as dermoscopic criteria to grade severity of AA.
Keywords: Alopecia areata, black dots, coudability hair, dermoscopy, tapering hair, yellow dots
INTRODUCTION
Alopecia areata (AA) is a common, non-scarring, autoimmune, chronic, inflammatory disease involving hair follicles characterized by hair loss on the scalp and/or body.[1] Clinically, the disease manifests as patchy alopecia, diffuse alopecia, reticulate alopecia, ophiasis, ophiasis inversus, alopecia totalis or alopecia universalis. Nail changes (diffuse fine nail pitting, longitudinal ridging, thin and brittle finger and toe nails, and trachyonychia) may be seen in 3-30% of the patients.
In general, clinical diagnosis of AA is made based on the typical pattern of hair loss, which can be supported by the presence of characteristic exclamation mark hair on light microscopy. However, in some cases, the clinical diagnosis may not be straightforward where invasive techniques (biopsy) may be more appropriate but are frequently not well accepted by patients; especially children.[2]
Recently, dermoscopy has established itself as a useful aid in the diagnosis of AA. The literature on dermoscopic features of AA in Indian patients is scanty. The correlation of dermoscopic features with severity of disease has not been looked into in previous studies on AA. Elucidation of dermoscopic features that are highly correlated with severe disease could help in developing dermoscopic predictors of severe disease or poor prognosis. The objective of our study was to document the dermoscopic features of AA in Indian patients and to analyze the correlation of dermoscopic features with severity of disease.
MATERIALS AND METHODS
All consecutive patients diagnosed with AA between August 2010 and August 2012 were included in the study after taking written informed consent. The patients with co-existent androgenetic alopecia or history of any treatment during the past 2 months were excluded from the study. A convenience sample size of 100 was chosen for this descriptive study. A detailed history was taken, and thorough clinical examination was done. The diagnosis was made by two independent dermatologists. The diagnosis was established by clinical examination in most of the cases and biopsy in ten patients. Localized patchy alopecia was defined as 1-3 patches of alopecia and multiple patchy hair losses as more than three patches of alopecia. The activity of AA was classified as progressive or nonprogressive according to the change in hair loss over the past month. This classification was used as the aim of our study was to correlate dermoscopic features with severity and prognosis of the disease. The various patterns of AA were noted as patchy, diffuse, ophiasis, totalis, and universalis. The hair pull test was performed in all patients with AA. The severity of AA was graded as S1 to S5 according to the guidelines of the National AA Foundation.[3]
Dry dermoscopy was done with a Heine Delta 20 dermoscope (Heine optotechnik, Herrsching, Germany) which was followed by wet dermoscopy. Liquid paraffin was used as the immersion media. The dermoscopic features that were looked for were yellow dots (YDs), black dots, exclamation mark hair, short vellus hair, circle hair and coudablity hair. The differentiation of YDs and white dots was done by consensus among two independent dermatologists. The number of YDs in a field of vision (YD/FOV) was counted for each patient from the most active margin of the alopecic patch. The active margin was determined by the hair pull test. Coudablity hair were scored using the scoring system of Inui et al.[4]
Statistical analysis was performed using SPSS13 software (SPSS, Chicago, IL, USA). Categorical variables were assessed using the Chi-square test and Fisher's exact test and continuous variables were assessed using Spearman rank correlation. Sensitivity and specificity of the various dermoscopic findings in comparison to skin biopsy were estimated. This study was cleared by the institute ethical committee.
RESULTS
A total of 116 patients were enrolled. These included 61 males and 55 females. The mean age of the patients with AA was 25.3 ± 19.7 years (ranging from 1 to 55 years and a median of 25 years). One hundred and ten patients had Fitzpatrick type V and 6 had type IV skin. The various types of AA seen in our study were patchy localized (76, 65.5%), patchy multiple (26, 22.41%), ophiasis (5, 4.31%), totalis (3, 2.58%), universalis (3, 2.58%) and diffuse (n = 3, 2.58%). One hundred and three patients had progressive and 13 had non progressive AA. Regarding the extent of hair loss; 84 had S1, 12 had S2, 5 had S3, 12 had S4 and 03 had S5 grade of AA. Fourteen (12.0%) patients had a prior episode of AA. Nine (7.7%) patients had a family history of AA (8 had patchy AA and 1 had alopecia universalis). There was no gender difference in any clinical type of AA.
Dermoscopic features of alopecia areata
YDs (104, 89.6%), short vellus hair (91, 78.4%), black dots (36, 31.0%), exclamation mark hair (23, 19.8%), broken hair (15, 12.9%) and circle hairs [Figures 1–4] (8) were seen by dermoscopy in the present study. It was seen that ninety-four patients had a coudability score of 0, 6 had a score of 1, 9 had a score of 2 and 7 had a score of 3. There was no specific dermoscopic pattern noted in the various types of AA [Table 1].
Figure 1.
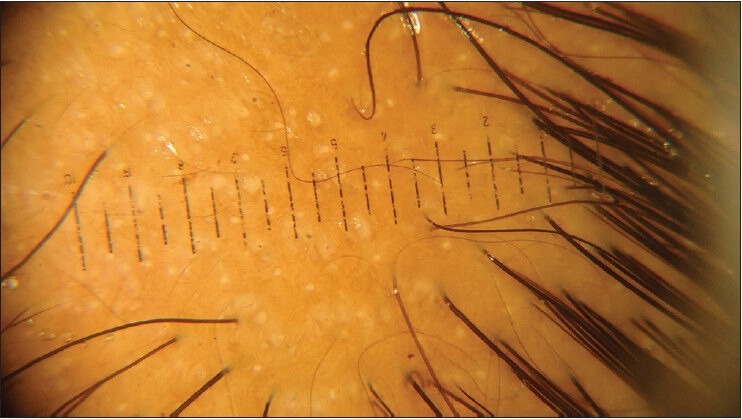
Larger yellow dots and smaller white dots seen on dermoscopy
Figure 4.

Circle hairs seen on dermoscopy
Table 1.
Dermoscopic features seen in all types of AA
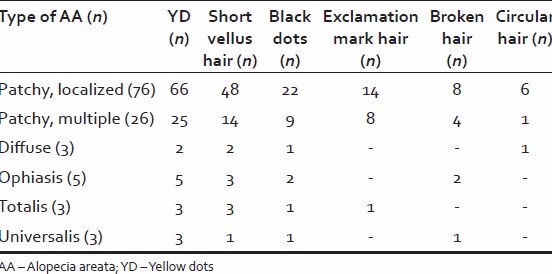
Figure 2.
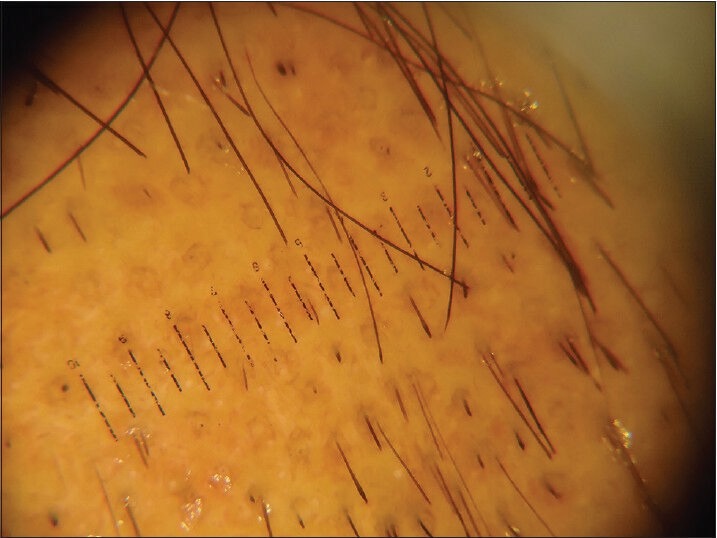
Coudability hairs and exclamation mark hairs
Figure 3.
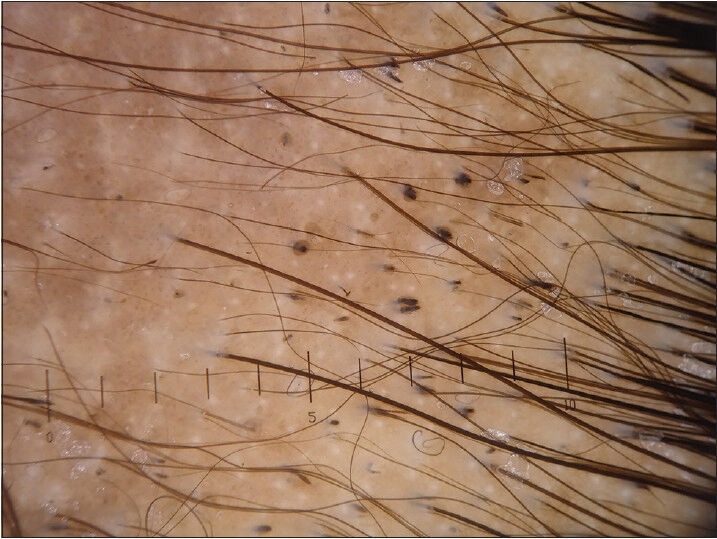
Black dots and short vellus hairs
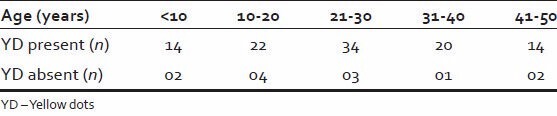
Yellow dots were found to be sensitive (89.6%) and specific (88.6%) dermoscopic markers for the diagnosis of AA. Diagnostic sensitivity increased to 97.4% when short vellus hair was included with YDs in dermoscopic evaluation. YDs were found to be distributed among all age groups [Table 2]. It was even seen in children less than 10 years of age. In view of the high number of YDs, dermoscopy was also done in other causes of alopecia to check if YDs were more common in this demographic population. However, only 10.1% of patients with other diseases showed YDs in comparison to 89.6% of patients with AA (P < 0.00001).
Table 2.
Distribution of YD among the different age groups
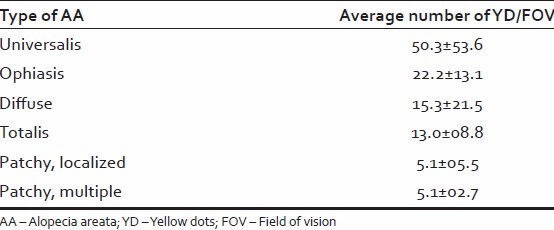
The mean number of YD/FOV was 7.53 ± 12.31. The mean YD/FOV was highest in alopecia universalis (50.3 ± 53.6), followed by ophiasis (22.2 ± 13.1). The least number of YDs was found in patchy alopecia [Table 3]. The number of YD/FOV did not differ significantly in progressive or nonprogressive alopecia (P = 0.5351). It was observed that the number of YD/FOV correlated significantly with the severity of alopecia (P < 0.0001).
Table 3.
Mean YD/FOV according to the type of AA
The individual dermoscopic findings did not correlate with the activity or extent of AA. Even the coudability score did not correlate with the disease activity (P = 0.72) or extent (P = 0.58).
DISCUSSION
Common dermoscopic findings of AA reported in the literature are YDs, black dots, short vellus hairs, exclamation mark hair and broken hair. Peter et al.[5] in their study of AA patients from a tertiary care center in South India, reported that the commonest dermoscopic finding was black dots (75%), followed by broken hairs (67%) and YDs (42%). In our study, YDs and short vellus hairs, were more commonly seen when compared to other dermoscopic findings. Inui et al.,[6] in their dermoscopic study of 300 Japanese patients with AA, reported 72.7% frequency of short vellus hair, 63.7% of YDs, 45.7% of broken hair, 44.3% of black dots and 31.7% of tapering hair. However, a prior study was done by Mane et al.[2] reported similar findings to the present study.
Yellow dots were found to be 89.6% sensitive for the diagnosis of AA, according to our study. de Moura et al.[7] reported the presence of YDs in 95% of AA patients in all stages of the disease and stated that YDs were a specific finding for slopecia areata. However, other studies did not report the same results. Mane et al., on the other hand, did a study on the same demographic population as ours and reported similar results with regard to YDs. Hence, YDs are found in higher numbers in Indian patients with AA. We propose that this could be explained by the south Indian practice of oiling hair.
Yellow dots represent distension of affected follicular infundibulum with keratinous material and sebum.[4] Because of underdeveloped sebaceous glands in prepubertal children, YDs are sparsely seen in children with AA. However, in the present study, 82.35% of patients' up to 15 years of age showed YDs on dermoscopy. The higher prevalence of YDs in the present study could perhaps be explained by the local practice of oiling hair that could resemble a YD on scalp dermoscopy. This has also been reported by Tosti and Duque-Estrada.[8]
Our results showed that YDs together with short vellus hairs were seen in 97.4% patients, suggesting that this combination enhances the sensitivity of diagnosis of AA. The fact that a combination of dermoscopic findings can increase the diagnostic sensitivity of AA was also noted in several other studies.[2,5,9] This combination of findings could be very useful in the pediatric population to avoid skin biopsies for diagnosis.
Miteva and Tosti[10] described circle hairs on dermoscopy in AA, which are nothing but short vellus hairs, which have a tendency to become coiled. In our study, these circle hairs were seen in eight patients with AA. We substantiate the usefulness of this finding in the diagnosis of AA even in darker population.
Inui et al.[6] reported black dots, YDs and short vellus hairs to be useful severity markers of AA. Lacarrubba et al.[9] in their dermoscopic study of AA reported that exclamation mark hairs, broken/cadaverized hairs were found most commonly in acute AA and their presence indicated progressive disease activity. On the other hand, short vellus hairs indicated hair regrowth and disease remission. In the present study, black dots, exclamation mark hairs, broken hairs, YDs and short vellus hair showed no correlation with the disease activity or severity of AA. Similar results were reported by Mane et al.[2] and Peter et al.[5] Inui et al.[4] described coudable hair to be a useful marker for disease activity in AA and a substitute for the hair pull test. This however was in contrast to the findings of the present study.
In the present study YD/FOV showed a significant correlation with the severity of disease. Dermoscopic assessment for the number of YD/FOV could be included in the evaluation of AA as it could serve as a guide to subclassify AA based on the severity and extent of involvement, and also to serve as a prognostic indicator. The high frequency of YDs in our study and the study by Mane et al. suggest that YDs are very important dermoscopic feature in south Indian patients with AA. However, YDs were seen in only 10.1% (22/218) of south Indian patients with other alopecias and hair disorders. This suggests that YDs are significant in the diagnosis of AA. The increased frequency of YDs could be explained by the practice of oiling hair; however, they are still sensitive in the diagnosis of AA. A limitation of this study is that the dermoscopy was not done in healthy controls to look at the normal dermoscopic patterns in Indian patients.
CONCLUSION
The most common dermoscopic features of AA in Indian patients are YDs and short vellus hairs. YDs/FOV is associated with severity of disease in Indian patients. This study also highlights the potential influence of hair care practices in the interpretation of scalp dermoscopic findings. Further studies are required to confirm the usefulness of YD/FOV, as well as to establish the normal dermoscopic patterns of scalp in the general population.
Footnotes
Source of Support: Financial assistance from JIPMER, Puducherry, India in the form of Intramural Research Fund to the corresponding author for this research work is gratefully acknowledged
Conflict of Interest: None declared.
REFERENCES
- 1.Harries MJ, Sun J, Paus R, King LE., Jr Management of alopecia areata. BMJ. 2010;341:c3671. doi: 10.1136/bmj.c3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mane M, Nath AK, Thappa DM. Utility of dermoscopy in alopecia areata. Indian J Dermatol. 2011;56:407–11. doi: 10.4103/0019-5154.84768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olsen EA, Hordinsky MK, Price VH, Roberts JL, Shapiro J, Canfield D, et al. Alopecia areata investigational assessment guidelines - Part II. National Alopecia Areata Foundation. J Am Acad Dermatol. 2004;51:440–7. doi: 10.1016/j.jaad.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 4.Inui S, Nakajima T, Itami S. Coudability hairs: A revisited sign of alopecia areata assessed by trichoscopy. Clin Exp Dermatol. 2010;35:361–5. doi: 10.1111/j.1365-2230.2009.03510.x. [DOI] [PubMed] [Google Scholar]
- 5.Peter D, George L, Pulimood SA. Trichoscopic features of various types of alopecia areata in India: Application of a hand-held dermoscope. Australas J Dermatol. 2013;54:198–200. doi: 10.1111/j.1440-0960.2012.00942.x. [DOI] [PubMed] [Google Scholar]
- 6.Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: Analysis of 300 cases. Int J Dermatol. 2008;47:688–93. doi: 10.1111/j.1365-4632.2008.03692.x. [DOI] [PubMed] [Google Scholar]
- 7.de Moura LH, Duque-Estrada B, Abraham LS, Barcaui CB, Sodre CT. Dermoscopy findings of alopecia areata in an African-American patient. J Dermatol Case Rep. 2008;2:52–4. doi: 10.3315/jdcr.2008.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tosti A, Duque-Estrada B. Dermoscopy in hair disorders. J Egypt Women Dermatol Soc. 2010;7:1–4. [Google Scholar]
- 9.Lacarrubba F, Dall'Oglio F, Rita Nasca M, Micali G. Videodermatoscopy enhances diagnostic capability in some forms of hair loss. Am J Clin Dermatol. 2004;5:205–8. doi: 10.2165/00128071-200405030-00009. [DOI] [PubMed] [Google Scholar]
- 10.Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;65:91–8. doi: 10.1016/j.jaad.2012.02.013. [DOI] [PubMed] [Google Scholar]


