Abstract
Background:
Hair restoration surgery (HRS) is a very promising and sought after aesthetic procedure with very few complications. Complications may occur in the donor or the recipient area, and it may be due to surgical or idiopathic causes.
Aim:
The aim was to analyze the complications in male patients who underwent HRS for androgenetic alopecia (AGA).
Materials and Methods:
We conducted a retrospective analysis of male patients who underwent HRS for AGA from December 2010 to August 2014. Data were collected from the registers, telephonic enquiry and electronic mails. All complications during and after surgery, and their subjective feeling about hair growth was recorded.
Results:
Seventy-three patients were included in the analysis. A total of 65 patients had undergone follicular unit transplant, 7 patients underwent FUE, and one patient had body hair transplantation. Postoperative edema was found in 42.47% of patients, followed by sterile folliculitis in 23.29% of patients, wide donor scar in 15.07% of patients, bacterial folliculitis and numbness/paresthesia in 10.96% of patients. Other complications such as raised scar, hiccups, pruritus, excessive bleeding were found in isolated cases.
Conclusion:
Thorough preoperative evaluation, skillful surgical techniques, good communication and postoperative follow-up go a long way in giving satisfactory outcome with fewer complications in HRS.
Keywords: Hair restoration surgery, complications, androgenetic alopecia
INTRODUCTION
Hair transplantation surgery is a promising and permanent method of hair restoration among the many treatment options for Androgenetic alopecia (AGA). Serious complications arising from surgical hair restoration (SHR) are relatively uncommon following well-performed and well-planned surgery.[1] As the number of surgeries continues to rise, so too will the total number of complications that occur in the course of these operations and beyond, presenting major challenges to novice and seasoned surgeons alike.[2]
A complication is defined as an adverse event that is not considered to be a common or usual occurrence, and which requires a change in methodology. Complications may arise because of surgical procedure per se, because of surgeons planning and technical errors or because of patients' physiology or compliance errors.[1] Complications can occur both in the recipient as well as the donor site.
There are isolated case reports focusing on complicating factors, such as persistent hiccups, von Willebrand disease, hereditary angiodema, herpes zoster, and malignant hyperthermia, all manifesting themselves during or after hair transplant. Complications of the procedure have included alterations in scars (cobblestoning, riding [elevation of skin in the transplanted area], and various degrees of fibrosis and/or keloids), pigmentation disturbances, hair kinking (deformity of the hair posthair transplant), arteriovenous fistulas, dehiscence, scar enlargement and necroses (described in donor and in receptor sites), areas of postoperative folliculitis, scalp infection, and osteomyelitis of the cranium.[3]
In our study, we did a retrospective analysis of all the hair transplant surgeries performed in our institute, in order to report the type and frequency of complications occurring during or after the hair transplantation procedure. We have also reviewed the literature regarding the cause and prevention of such complications.
MATERIALS AND METHODS
This study was a retrospective analysis of patients who underwent hair restoration surgery (HRS), between December 2010 and August 2014 in our department of dermatology. Approval from the Ethical committee of Institutional Review Board was obtained. Only men who underwent HRS for AGA were included in the study. Data were collected from information recorded in the register, follow-up of patients, telephonic enquiry and mailed photographs. Out of the 197 patients who underwent HRS for AGA, only 73 patients' data was available and was included in the study [Figure 1]. Rest of the patients' data was not available either due to lack of entry of registration details like address and phone numbers, or due to lack of response from the patients through person, phone or electronic mails. Of the 73 patients, 65 had undergone Follicular unit hair transplantation by strip harvesting method follicular unit transplant (FUT), 7 patients had undergone HRS by Follicular unit extraction method FUE and 1 patient had undergone body hair transplantation (BHT).
Figure 1.
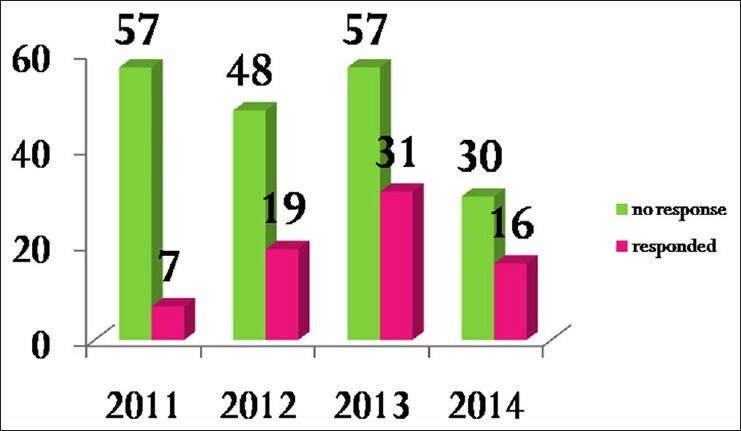
Patients' response/inclusion rate in each year
Surgical technique
All patients trimmed their hair short prior to the surgery. Anxiolytics, pain killer and antibiotics were administered at the start of surgery. Strict surgical asepsis was taken care of and Ring block anesthesia was administered to the donor area using a combination of xylocaine and bupivacaine. This was followed by the tumescent injection which was a mixture of bupivacaine with adrenaline, saline/ringer lactate and triamcinalone acetate. After this follicles were harvested by either strip or extraction method using micromotor punches, from the safe donor area. After strip harvesting, the donor area was closed using 3-0 vicryl rapide by the trichophytic closure method. Strip was slivered and follicular units were dissected and stored in chilled saline/ringer lactate until implantation. Supra orbital and supra trochlear block was given to anesthetize the recipient area. Tumescent solution was also injected into the recipient area. Slits were made using Kolkata slits of width 1.2 mm and 1.4 mm. Follicular units were implanted into the slits using two forceps. All patients received postoperative antibiotic therapy, oral corticosteroids and analgesic medications. Dressing on the donor area was removed after 10 days. Patients were followed-up in the immediate postoperative period, at 3, 7, and 14 days, and then monthly up to 1-year postoperatively.
All complications during the surgery and after the surgery were recorded by the method of data collection as mentioned above.
RESULTS
Of the 73 patients included in the study, 65 patients underwent FUT, 7 patients underwent FUE and 1 patient had BHT. The mean age was 30.06 years with the youngest one who underwent HRS being 21 years and the oldest being 60 years. The various complications seen in patients are shown in the Figure 2. Postoperative edema [Figure 3] was the most frequent complication which was found in 31 (42.47%) patients. This was followed by sterile folliculitis [Figure 4] in the recipient area in 17 (23.29%) patients, wide donor scar [Figure 5] in 11 (15.07%) patients, numbness/paresthesia and bacterial folliculitis in 8 (10.96%) patients each. Other complications like raised donor scar [Figure 6], postoperative hiccups, skin texture changes in the recipient area, excessive bleeding during surgery, syncope, postoperative pruritus were seen in very few patients. 44 (60.27%) patients gave a subjective report of less than 50% growth of the transplanted hair with 20 (27.4%) of them less than 25% growth. Wound dehiscence in the donor area was found in one patient. One patient had bleaching of his recipient area with discolored hair growth due to excessive use of hydrogen peroxide by the patient himself in order to remove crusts. It became normal after shaving and regrowth [Figure 7]. One patient had developed severe adverse drug reaction to cefotaxime that was given postoperatively [Figure 8]. He had developed necrosis of the skin in the left temporal region which left a bad scar. One patient had developed postoperative depigmentation in the recipient area [Figure 9].
Figure 2.
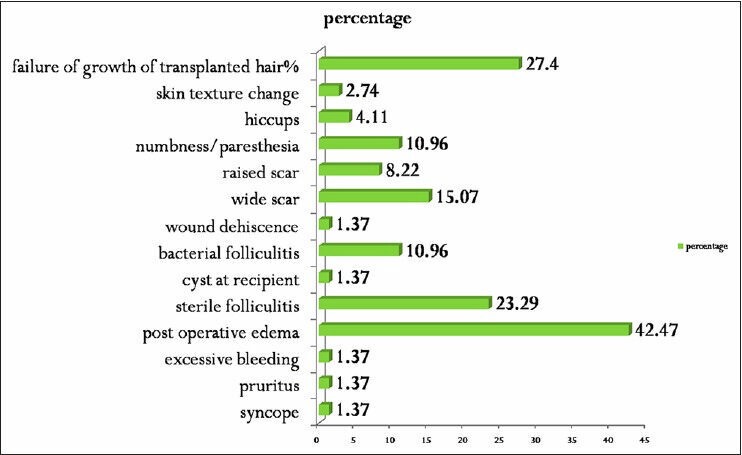
Frequency and type of complications
Figure 3.

Postoperative edema
Figure 4.

Sterile Folliculitis
Figure 5.

Wide donor scar
Figure 6.

Raised donor scar
Figure 7.

Bleaching of hair due to excess Hydrogen peroxide usage to remove crusts
Figure 8.

Adverse drug reaction to cefotaxime
Figure 9.

Postoperative depigmentation in recipient area
DISCUSSION
Complications in HRS are very low compared to other aesthetic surgical procedures. But there are wide varieties of possible complications that are less severe and manageable. Though there are isolated case reports of various complications of HRS, there are no published reports of significant size detailing the frequency of complications in large series.
In the preoperative period, there are many factors that influence the outcome of the surgery. If those factors are not evaluated adequately and the surgery is performed, the stage is set for complications to occur.[2] The surgeon should counsel the patients thoroughly regarding the procedure, possible complications and expectations. Personality disorders like body dismorphic disorder and other red flag signs[3] must be identified before considering them for surgery.
Excessive bleeding and infection either in the donor or recipient area is a general complication. In our study, this was found in just 1.37% patients. During the preoperative evaluation, patients should be screened for history of bleeding diathesis, for intake of aspirin, nonsteroidal anti-inflammatory agents, Vitamin E, alcohol, anabolic steroids, or other anticoagulative agents.[4] Topical minoxidil and smoking must be stopped at least 2 weeks prior to the surgery. Intraoperative recipient-site bleeding is not uncommon and can, usually, be minimized by injection with epinephrine-containing tumescent solutions.[5]
Infections of the scalp are very rare because it is well vascularized. Serious infections occur in less than 1% of cases and are, usually, associated with poor hygiene, excessive crust formation, or preexisting medical risk factors.[6] Folliculitis was observed in the majority of patients in a study conducted by Sandro et al.[7] and Unger[8] reported a folliculitis rate of 20% of his study group. In our study bacterial folliculitis in the donor, area was found in 10.96% patients which occurred even up to 8 months after surgery. There are several measures to be followed for prevention and infection control: Clean and decontaminated operating room; use of sterilized material; donor area asepsis, use of disposable instruments, and antibiotic prophylaxis.[2] Sterile folliculitis in the recipient area is a frequent complication seen weeks or months after transplantation. In our study, it was found in 23.29% of patients. The causes are not clear. Theories include “ingrown” hair, foreign body reactions, epithelium logged into slit sites during recipient site creation, piggybacked grafts and the “idiopathic” intrinsic properties of the host scalp.[9] In the majority of cases, the pathogen cannot be cultured from the lesions, and hence the name sterile folliculitis. They are, usually, managed by oral antibiotics, warm compresses and unroofing the cysts.
In our study, we found postoperative edema as the most common complication (42.47%). Swelling or edema of forehead or eyelids is a common consequence of HRS, especially 2-6 days after the operation. In some cases, this edema is so severe that patient cannot open his/her eyes [Figure 3]. This may cause both morbidity and a delay in returning to normal life and work.[10] Many methods have been recommended to reduce the edema, which include both physical methods and administration of steroids. Physical methods include the use of firm headband, maintaining semi-lay down position postoperatively,[11] applying adhesive tapes below hair line and usage of ice packs or bags of frozen peas. Usage of steroid may be by oral route, intramuscular injection and/or adding steroid to the local anesthetic. However, none of these methods has been found fully satisfactory. In our study we have found this complication in spite of adding steroid to tumescent mixture, headband, postoperative short-term oral steroids and advice of postoperative semi-lay down position.
The various possible complications that can occur in the donor area are wide scars, cross hatch scars [Figure 10], keloid scars, donor site depletion, wound dehiscence, necrosis, postoperative effluvium/shock loss, hypoesthesia, neuralgia or hematoma.[1] In our study, wide donor scar was found in 15.07% patients followed by numbness/paresthesia (10.96%) and bacterial folliculitis (10.96%) in the donor area. Donor area complications are due to improper donor harvesting like, too wide a strip, too much tension during closure, poor location, transection of hair follicles, transection of blood and nerve supply and improper undermining.[4] With today's large grafting sessions, more donor tissue is required to obtain the surgical goals (number of grafts).Wider (1.5-2 cm) and longer (>30 cm) donor strips are harvested for this reason.[1] The Mayer-Pauls scalp elasticity scale measures the laxity of donor scalps and for each value recommends a corresponding maximum strip width.[12] This scale is a guide for the estimation of the donor area that can be safely closed with minimal tension. If a wound is under tension, the wound should be closed in a delayed fashion rather than undermined or forcefully drawn close, both of which can lead to necrosis, unpredictable hair loss in the donor area, and additional scarring.[4]
Figure 10.

Cross hatched donor scar
Hiccups are found in few patients after HRS, which may develop immediately after the procedure and last for about 48 h to a week, because of the patient's dorsal placement. They can also result from excessive air aspiration consequent to stimulation of diaphragmatic muscle movements by very excited or vocal patients.[13] In our study, hiccups was found in 4.11% patients.
Hypopigmentation can occur in either the donor or recipient areas. Recipient-site hypopigmentation is more prevalent with larger slits, and can be especially problematic when low graft yields fail to produce sufficient hair for adequately camouflaging the scalp.[1] In our study one, patient had developed postoperative hypopigmentation [Figure 9] in the recipient area.
In spite of the surgeons' best efforts and surgical techniques, poor growth of transplanted hair and dissatisfaction of patients is a common problem faced by hair transplant surgeons. It is very difficult to attribute the reason for limited growth. Not to diminish the importance of good preoperative and postoperative care, an in-depth analysis of the individual steps in the operating room from the harvesting of donor tissue, graft dissection, through the implantation phase of grafts, usually reveals significant insights into the problem.[2] That is because the hair follicle is most likely to be rendered unviable during this interval as a result of dehydration,[14] trauma to the graft, prolonged out of body time,[15] harmful effects of toxins such as sterile water, povidone iodine, folliculitis, factor X[16] and dense placement of grafts. The underwhelming response may also be due to patient growth characteristics, hypertension, diabetes, and smoking. Some individuals can also experience limited hair growth in the central area of the scalp versus other peripheral areas because of the relative hypovascularization in the central area.[7] In our study, 44 (60.27%) patients gave a subjective report of less than 50% growth of the transplanted hair with 20 (27.4%) of them less than 25% growth.
We also found some rare, unexpected complications like adverse drug reaction to cefotaxime leading to necrosis and scarring, and bleaching of hair due to excess application of hydrogen peroxide, in our study.
This study throws a light on the types and frequency of complications that may occur in HRS. Complications in HRS are very less, but the surgeons must always be vigilant because unexpected adverse events can always occur. Thorough preoperative evaluation, good surgical skills, and efficient management of any complication that may surface during or after the surgery will lead to a satisfactory outcome.
ACKNOWLEDGMENT
Dr. Shilpa, Dr. Savitha, Dr. Nirmal, Dr. Madhura, Dr. Nithin, Dr. Sujaya, Dr. Ranjitha, Dr. Chitrika GB, Dr. Sashidhar, Dr. Asha, Dr. Leelavathy, Dr. Nataraj HV, all the patients who cooperated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Konior RJ. Complications in hair-restoration surgery. Facial Plast Surg Clin North Am. 2013;21:505–20. doi: 10.1016/j.fsc.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 2.David PM. Complications in hair restoration surgery. Oral Maxillofac Surg Clin North Am. 2009;21:119–48. doi: 10.1016/j.coms.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Musgrave R, Gradinger G. Symposium on Problems and Complications in Aesthetic Plastic Surgery of the Face. St. Louis: Mosby; 1984. pp. 3–5. [Google Scholar]
- 4.Lam SM. Complications in hair restoration. Facial Plast Surg Clin North Am. 2013;21:675–80. doi: 10.1016/j.fsc.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Coleman WP, 3rd, Klein JA. Use of the tumescent technique for scalp surgery, dermabrasion, and soft tissue reconstruction. J Dermatol Surg Oncol. 1992;18:130–5. doi: 10.1111/j.1524-4725.1992.tb02444.x. [DOI] [PubMed] [Google Scholar]
- 6.Farjo N. Infection control and policy development in hair restoration. Hair Transplant Forum Int. 2008;18:141–4. [Google Scholar]
- 7.Sandro S, Gonçalves AJ, Américo HJ, Flavia HJ. Surgical complications in hair transplantation a series of 533 procedures. Aesthet Surg J. 2009;29:72–6. doi: 10.1016/j.asj.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Unger WP. Hair Transplantation. 3rd ed. New York: Dekker; 1995. Complications of hair transplantation; pp. 363–74. [Google Scholar]
- 9.Vogel JE, Jimenez F, Cole J, Keene SA, Harris JA, Barrera A, et al. Hair restoration surgery: The state of the art. Aesthet Surg J. 2013;33:128–51. doi: 10.1177/1090820X12468314. [DOI] [PubMed] [Google Scholar]
- 10.Gholamali A, Sepideh P, Susan E. Hair Transplantation: Preventing Post-operative Oedema. J Cutan Aesthet Surg. 2010;3:87–9. doi: 10.4103/0974-2077.69018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker NP. Textbook of Dermatology. 6th ed. Oxford: Blackwell Science; 1998. [Google Scholar]
- 12.Mayer M, Pauls T. Scalp elasticity scale. Hair Transplant Forum Int. 2005;15:122–3. [Google Scholar]
- 13.Arnold J, Stough DB, Haber RS. Hair Replacement. St. Louis: Mosby; 1996. Hiccups following surgery of the scalp. Complications; pp. 332–4. [Google Scholar]
- 14.Gandelman M, Mota AL, Abrahamsohn PA, De Oliveira SF. Light and electron microscopic analysis of controlled injury to follicular unit grafts. Dermatol Surg. 2000;26:25–30. doi: 10.1046/j.1524-4725.2000.99161.x. [DOI] [PubMed] [Google Scholar]
- 15.Limmer R. Hair Replacement. St. Louis: Mosby Press; 1996. Micrograft survival; pp. 147–9. [Google Scholar]
- 16.Shiell R. Hair Transplantation. St. Louis: Mosby; 1996. Poor Hair Growth after Hair Transplantation: The Factor X; pp. 314–6. [Google Scholar]


