Abstract
Context:
Stress fractures of the foot and ankle are a common problem encountered by athletes of all levels and ages. These injuries can be difficult to diagnose and may be initially evaluated by all levels of medical personnel. Clinical suspicion should be raised with certain history and physical examination findings.
Evidence Acquisition:
Scientific and review articles were searched through PubMed (1930-2012) with search terms including stress fractures and 1 of the following: foot ankle, medial malleolus, lateral malleolus, calcaneus, talus, metatarsal, cuboid, cuneiform, sesamoid, or athlete.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
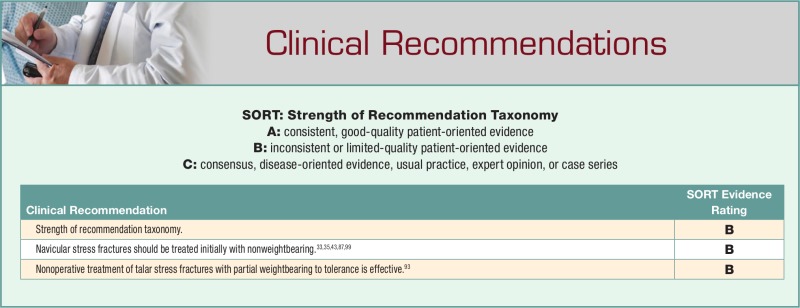
Stress fractures of the foot and ankle can be divided into low and high risk based upon their propensity to heal without complication. A wide variety of nonoperative strategies are employed based on the duration of symptoms, type of fracture, and patient factors, such as activity type, desire to return to sport, and compliance. Operative management has proven superior in several high-risk types of stress fractures. Evidence on pharmacotherapy and physiologic therapy such as bone stimulators is evolving.
Conclusion:
A high index of suspicion for stress fractures is appropriate in many high-risk groups of athletes with lower extremity pain. Proper and timely work-up and treatment is successful in returning these athletes to sport in many cases. Low-risk stress fracture generally requires only activity modification while high-risk stress fracture necessitates more aggressive intervention. The specific treatment of these injuries varies with the location of the stress fracture and the goals of the patient.
Keywords: stress fracture, athlete, foot, ankle
Introduction, Epidemiology, and Basic Science
Stress fractures are relatively uncommon injuries, accounting for approximately 1% to 7% of all athletic injuries.12,35 The incidence of these injuries is rising due to earlier and longer participation in sports, the emergence of more extreme sporting activities, and the heightened awareness of the diagnosis.55
In contrast to acute fractures, which typically occur with a single maximal load, stress fractures occur due to repetitive, submaximal loading of a bone, leading to microfractures that are unable to heal due to bone resorption and bone formation imbalances.12 A bone responds to stress on a continuum from a stress reaction to a fracture.12,13 The initial stage of bone failure is generally called a stress reaction. This diagnosis is made in a symptomatic patient who has bone scan or magnetic resonance imaging (MRI) evidence of bone reactive changes without a true fracture line.12,13 If the repetitive loading continues, the stress reaction can go on to a true stress fracture.12,13 This mechanism of injury explains the higher incidence of stress fractures among military recruits, runners, and those involved in jumping sports, though any activity with repetitive loading can lead to stress fractures.8,12,13,17,35 Most bones have reported cases of stress fractures, but the lower extremities have the highest prevalence.12 In a study of 320 athletes, the tibia (49.1%), tarsals (25.3%), and metatarsals (8.8%) were the most frequently involved bones affected by a stress fracture.58
Intrinsic and extrinsic factors have been described when determining the etiology of a stress fracture (Table 1). Intrinsic factors consist of the patient’s anatomy and biology including cavus feet, leg length discrepancies, excessive forefoot varus tarsal coalitions, a prominent posterior calcaneal process, tight heel cords, poor bone density or vascular supply, and abnormal hormonal levels.35,46,55 Extrinsic factors such as type of activity, excessive or new training regimens, equipment and footwear issues, training surfaces and techniques, and nutrition can also play a role.35,46,55 Several studies have described the biomechanical effects of muscle fatigue as a possible factor in the development of stress fractures.96,102 Continued training after muscle fatigue changes loading patterns of the foot based on force plate studies and is postulated to be a factor in stress-related injuries.102
Table 1.
| Intrinsic Factors | Extrinsic Factors |
|---|---|
| Cavus feet | Type of activity |
| Leg length discrepancies | Excessive/new training regimen |
| Excessive forefoot varus | Poor equipment/footwear |
| Tarsal coalitions | Improper technique |
| Prominent posterior calcaneal process | Type of training surface |
| Tight heel cords | Sleep deprivation |
| Osteopenia/osteoporosis | |
| Poor vascular supply | |
| Abnormal hormonal levels |
Female individuals have a higher incidence of stress fractures.35,46,71,72,90 Anatomically, a wider pelvis and more common genu valgum results in a compensatory increased Q-angle and often foot pronation.5,55 On average, female individuals have 25% less muscle mass than male individuals, which can focus forces on to a smaller area of bone with less muscle protection.55 The “female athlete triad” (eating disorder, amenorrhea, and osteoporosis) is found among competitive female athletes, particularly those involved in long-distance running, figure skating, and gymnastics.5,28,30,35 High-level endurance athletes from both sexes are in danger of osteoporosis based on the effects of estrogen and testosterone on bone remodeling; low levels of sex steroids have been measured following rigorous training sessions in both male and female athletes.101 Sex steroids normally inhibit osteoclasts and enhance osteoblasts, thereby slowing the resorption process; subphysiologic levels correlate with low bone mineral density.101
Two main categories, low and high (Table 2), have been used to determine the relative risk of either going on to complete fracture or to nonunion and aid in guiding the work-up and treatment of stress fractures.12,13,35 Low-risk stress fractures, such as those of the calcaneus, have a better prognosis and can often be diagnosed clinically and treated with activity modification.12,13,35 Those at high risk, such as the navicular, talus, medial malleolus, proximal fifth metatarsal, and sesamoids, will often need more advanced imaging, periods of nonweightbearing, and possibly surgical fixation.12,13,35
Table 2.
| High Risk | Low Risk |
|---|---|
| Medial malleolus | Calcaneus |
| Talus | Cuboid |
| Navicular | Cuneiforms |
| Fifth metatarsal base | Lateral malleolus |
| Sesamoid |
History, Physical Examination, and Imaging
Patients typically present with a progressive onset of pain with weightbearing activity over a period of days to weeks.43 History may include a rapid increase in mileage, intensity, or duration of activity; changes in playing surface or sport or inadequate rest periods should raise the suspicion of a stress fracture.8,12,13,18,35,46,55,58,62,63,90,96 A thorough history including diet, nutrition, medications, daily activities, footwear, and menstrual cycles in female athletes should be discussed.5,8,12,13,24,35,46,90 On physical examination, pain with weightbearing or range of motion of a joint near a stress fracture may be elicited, point tenderness is almost universal, and in more superficial areas, edema, warmth, ecchymosis, or even a palpable callus may be present.8,12,13,18,35,46,55,58,62,63,90,96 Assessment of limb alignment and length discrepancies, gait, passive range of motion, tendon function, and callosities provides information about repetitive stresses placed on the symptomatic area.16 Noting alignment of the ankle in neutral, cavovarus, or planovalgus and determining fixed or flexible deformities can provide insight into the underlying causes of the pathology.16 Stiff joints as well as ligamentous laxity are a sign of improper forces across a joint, postulated to put the patient at higher risk of stress fracture.16
Imaging studies including radiographs, computed tomography (CT) scans, MRI, and bone scintigraphy can be helpful when the diagnosis is questionable or stress fracture is suspected in a high-risk bone given the possible sequelae of a missed or late diagnosis.12 Plain films will often be negative for the first 2 weeks following a stress fracture, until resorption, sclerosis, or callus formation occurs.12,13 Radionuclide bone scan has been shown to be a sensitive imaging modality since the 1970s.12,78,81 Changes can be seen within 48 to 72 hours of injury.81 Uptake in all 3 phases of a technetium-99m diphosphonate scan is characteristic of a stress reaction/fracture and can be differentiated from soft tissue injury, which will only show increased uptake in the first phase (angiographic and blood pool/soft tissue imaging, respectively).81 MRI has replaced bone scan as the imaging modality of choice in many settings and gives superior specificity and resolution over bone scintigraphy.73 CT scan can be used to identify incomplete and complete fractures but cannot aid in identification of stress reactions.73 However, CT scan is thought to be more helpful than MRI in following the healing of stress fractures.91 Burne et al19 proposed that as a stress fracture heals, the initial edema and hematoma seen well on MRI for diagnosis is replaced by sclerosis, which is better seen on CT scan. This, in combination with a thick periosteum in some locations, impairs the ability of MRI to pick up some subtle fracture lines.91 Therapeutic ultrasound can also be used as an adjunct to the physical examination. Although previously thought to have poor sensitivity and specificity, a recent trial found increased pain with the application of therapeutic ultrasound at the site of a stress injury to have a positive predictive value of 99% (sensitivity, 81.9%; specificity, 66.6.%).77
High-Risk Stress Fractures
Some foot and ankle stress fractures have a relatively low propensity for spontaneous healing due to various factors such as blood supply, shearing forces across their surface, and location.12,35,46 Strict nonweightbearing, immobilization, and, not uncommonly, surgery are frequently needed to obtain a solid union.12,35,46
Medial Malleolus
Stress fractures of the medial malleolus are uncommon and generally found in athletes involved in running, jumping, and kicking sports, although abnormal forces at the ankle due to tibial and talar osteophytes have also been implicated.42,89,91 The first series of 6 patients reported by Shelbourne in 1988 described medial malleolar tenderness, ankle effusion, pain during running activities, and a vertical radiolucent line extending from the plafond on radiographs.91 Although most medial malleolar stress fractures occur in skeletally mature patients, adolescent cases have been reported.89
A patient with concerning symptoms but negative radiographs should undergo a bone scan or MRI (Figure 1). An incomplete fracture on MRI or a positive bone scan can be treated with cast immobilization and nonweightbearing.75,89,91 Although most of these injuries will heal with appropriate nonoperative treatments, internal fixation may be considered to allow earlier return to competitive sports, often within 1 to 2 months.52,75,89,91 Several series of medial malleolar stress fractures in athletes showed that both time to healing and return to sport were longer in the nonoperative group.89
Figure 1.
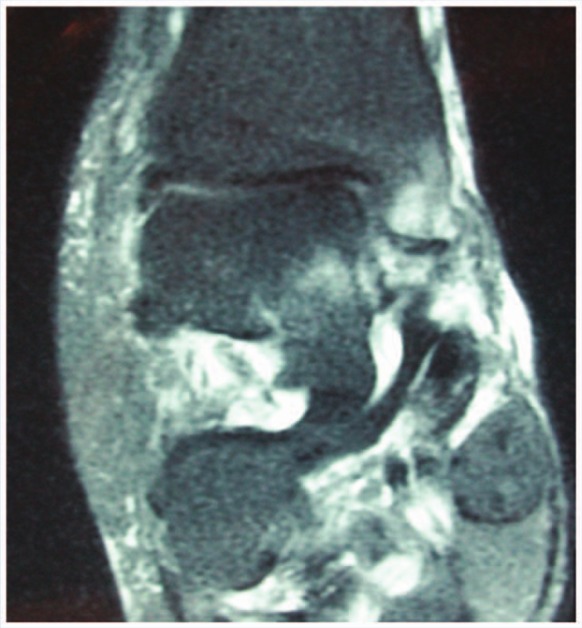
T2-weighted MRI showing high signal in the medial malleolus.
Talus
Talar stress fractures were first described in 1965 by McGlone.60 It is a relatively rare injury; athletes and military recruits performing repetitive axial loading activities are most prone to this injury.82,93,94 Advanced imaging, particularly MRI, is often required to obtain a diagnosis (Figure 2).14,93,94 Physical examination findings are variable, including point tenderness, ankle effusion, or soft tissue swelling.14,60,93,94 Excessive subtalar pronation or plantar flexion is noted clinically in many patients with lateral process stress injuries due to impingement of the lateral process of the calcaneus on the posterolateral talus.14 The superior part of the talar head is most frequently involved, and the posterolateral talar body fracture will usually be seen extending into the subtalar joint.14,93
Figure 2.
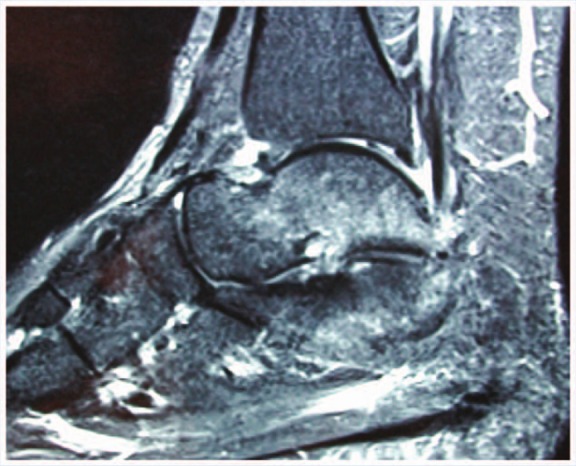
T2-weighted MRI showing high signal in the talus.
A retrospective review of Finnish military recruits found 56 talar stress injuries (reactions and fractures). Five patients had bilateral injuries, and 44 had other associated lower extremity stress injuries. Sixty-seven percent were in the talar head, 25% in the body, and 8% in the posterior portion, similar to previous reports.93 Talar head injury was associated with navicular stress injury, upper talar body with calcaneal injury, and posterior talus with posterior impingement and a symptomatic os trigonum.93 Patients treated nonoperatively (NSAIDs, relative rest, partial weightbearing as tolerated) until asymptomatic did well, with a mean duration of treatment of 64 days.94 In contrast, others recommended a minimum of 6 weeks of nonweightbearing for this injury due to concern for delayed healing and avascular necrosis.14 There is no established treatment algorithm for talar stress fractures given the lack of scientific analysis and outcomes. Although orthotics are not used for treatment, patients with excessive pronation may benefit from orthotics to reduce lateral loading, given the coincidence of pronation and lateral talar stress fractures in some series.14,16
Navicular
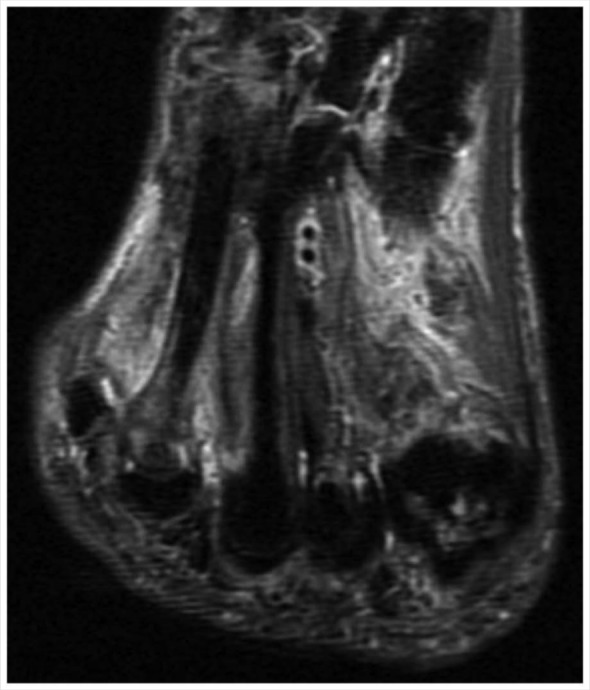
Navicular stress fractures are currently considered high risk due to the rate of nonunion.12,35 Patients are usually involved in explosive sprinting or jumping activities and complain of pain at the dorsum of the midfoot or along the medial longitudinal arch with activity.99 Swelling, erythema, and ecchymosis are less reliable, but point tenderness at the dorsal aspect of the navicular known as N-spot tenderness is the most consistent finding.12,35 Clinical suspicion should prompt radiographic evaluation, and advanced imaging should be obtained if initial radiographs are negative.33,99 MRI (Figure 3) and bone scan provide no additional benefit over CT.19,31 The fracture line usually extends from the proximal dorsal border in a plantar and distal direction in the sagittal plane.19,33 The central third of the navicular is a watershed area between blood supplies coming from medial and lateral vessels.99 This may lead to slower healing of physiologic microfractures in this central area and increase the risk of a stress fracture.99 During walking and running, this region is also subjected to shear forces from the first and second metatarsals (through the cuneiforms) along the convex surface distally and the talus at the concave surface proximally.33,35 Anatomical risk factors include a relatively long second metatarsal, pes cavus, metatarsus adductus, medial narrowing of the talonavicular joint, talar beaking, and limited subtalar or ankle motion.44
Figure 3.

T2-weighted MRI showing high signal in the navicular.
Small studies have supported both nonoperative and operative treatment.33,35,43,87,99 Nonoperative treatment typically includes nonweightbearing in a short leg cast.33,35,43,87,99 Operative treatment entails open reduction and internal fixation with or without bone grafting.33,35,43,87,99 One of the first studies reviewing this injury found good results in patients treated with nonweightbearing in a short leg cast.99 In a review of 86 navicular stress fractures in athletes, only 26% treated with activity modification versus 86% with nonweightbearing in a short leg cast returned to sports.43 Six patients initially underwent surgical treatment, and 5 returned to sports at an average of 3.8 months. They concluded that nonweightbearing in a short leg cast was the standard of care, though acknowledged that time to return to sport was shorter with initial surgical intervention. In an evaluation of 22 patients, 11 of 13 navicular stress fractures healed with nonweightbearing in short leg cast, and 8 returned to sport at an average of 4.3 months.87 All 9 treated with initial internal fixation, with or without bone grafting, returned to sport at an average of 3.1 months.87 In 19 navicular stress fractures, 6 treated with a nonweightbearing short leg cast healed and returned to sports at 4 months; all 13 undergoing open reduction internal fixation (ORIF) returned at 4.1 months.86 In these 2 studies, they found no significant difference in outcome or time to return to sports.86 In a recent systematic review, outcomes including radiographic healing, clinical healing, and time from onset of symptoms to return to activity were compared for 3 different treatment strategies.98 Regimens of weightbearing, nonweightbearing in short leg cast, and surgical intervention were analyzed, with no statistically significant difference between nonweightbearing in short leg cast and surgical intervention. Weightbearing treatments were inferior in all outcome measurements. This study concluded that an initial 6 to 8 weeks of nonweightbearing in a short leg cast should be the standard of care for navicular stress fractures.98 Despite this recommendation, it should be noted that displaced fractures may have a higher risk of nonunion and poorer outcomes even with surgical treatment.59
Metatarsal
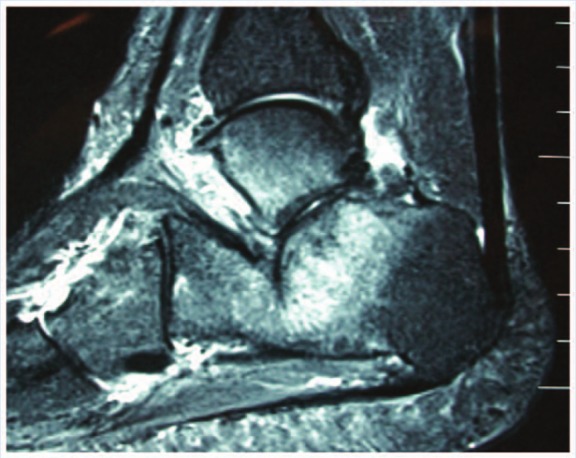
These stress fractures occur most frequently in the second and third metatarsals and are relatively common.12,13,35,46 They are considered high or low risk, depending on location.12,13,35,46 Common in runners, military recruits, ballet dancers, and basketball players, like most, patients will report a recent increase in training.1,8,12,13,16,17,21-23,29,31,32,35,38,39,46,48,55,58,62,64,67,74,77,79,85,90,97,102,104 Forefoot pain with weightbearing, inability to toe walk, point tenderness, and swelling are present on examination.1,8,12,13,16,17,21-23,29,31,32,35,38,39,46,48,55,58,62,64,67,74,77,79,85,90,97,102,104 Radiographic work-up with plain films of the foot may show callus formation about the metatarsal at around 2 weeks.1,12,13,16,17,22,23,29,34,38,39,46,55,58,62,67,74,85 As with other stress fractures, increased uptake on bone scan should be isolated to the affected bone; MRI (Figure 4) can differentiate between stress reaction or fracture and soft tissue abnormalities.35,46,85
Figure 4.
T2-weighted MRI showing high signal in the distal fourth metatarsal.
Distal second metatarsal stress fractures are most common.16 During walking and running, the second metatarsal assumes the highest bending strain and shear force.38 The fixed bases and proximal hinged metatarsophalangeal joints create a bending moment at the proximal diaphysis during the stance phase of gait.38,61 A relatively long second metatarsal and an excessively mobile first ray (Morton foot) increase this force even further.38,55,61 Additionally women have a higher middle forefoot loading force than men.79 These anatomical and biomechanical characteristics may play a role in the development of stress fractures.38,79 A recent cadaveric biomechanical study showed that both custom and semicustom orthotics decrease tension and shear strain on the second metatarsal, with custom orthotics being superior.61 Clinical studies from military recruits show benefit from orthotics.31,66 Treatment of established distal metatarsal stress fractures is usually initially conservative with activity modification for 6 to 8 weeks with gradual return to sports when asymptomatic.16 The addition of a stiff-soled shoe, midfoot taping, walker boot, or short leg walking cast can increase comfort.13,16,35
Second and Third Metatarsal Base
Metatarsal base stress fractures are most common in female ballet dancers.1,22 The insidious onset of vague midfoot pain is often overlooked or misdiagnosed.1,22,39,64,67,74,85 The second and third metatarsals are most at risk during ballet in the en pointe position due to the locking of the second metatarsal base and cuneiforms in extreme plantar flexion.1,22,39,64,67,74,85 Intrinsic risk factors include a pronated foot and poor ankle plantarflexion causing a so-called over-pointe foot with compensatory plantarflexion through the Lisfranc joint.1 This shifts the center of gravity anterior to the metatarsal shaft, creating more force at the base. Four female ballet dancers with midfoot pain were treated successfully with a short period of immobilization and rest, and 1 required operative debridement of necrotic bone.64 Several subsequent studies have also reported good results and return to dancing with nonoperative management, ranging from a wooden-soled shoe to short leg walking cast.67,74 The incidence of nonunion is low.22,67,85 Comorbidities including diabetes, chronic steroid use, the female athlete triad, cancer, and metabolic bone disease are associated with a higher rate of nonunion.22 Ballet trainees treated with medium energy external shock wave and ultrasound along with a period of 3 to 5 weeks of weightbearing rest had a 100% return to dancing at a mean 4.6 weeks and return to full pointe at a mean 18 days later without subsequent pain or nonunion.1 Overall, nonsurgical management seems to yield good results with nonweightbearing or weightbearing in a regular shoe or short leg cast.1,22,39,64,67,74,85 Surgical treatment of nonunion following nonoperative treatment may include drilling procedures and open reduction internal fixation.85
Fifth Metatarsal
The typical presentation of fifth metatarsal stress fractures differs from acute fractures clinically and radiographically. Pain has usually been present for several weeks, and the fracture is classically located at the diaphyseal-metaphyseal junction.97 Repetitive adduction force with the ankle in plantarflexion often causes these stress fractures due to the pull of the plantar fascia. As such, they are frequently seen in basketball players.12,29,35,77,104 A description of lateral foot pain, tenderness about the fifth metatarsal base, and pain with passive inversion stretch are clues to the diagnosis.12,29,35,77,104 A cavovarus foot or restricted hindfoot eversion is thought to predispose patients to fifth metatarsal base stress fractures by increasing the force on the lateral aspect of the foot.35 Torg et al created a classification system for these more distal fifth metatarsal base stress fractures based on history and radiographic appearance that helps to guide treatment.97 Type I fractures are acute fractures by history and have sharp fracture lines with no radiographic signs of healing. Type II fractures are considered delayed unions. There is no history of previous fracture, but radiographs show periosteal new bone, resorption, and sclerosis at the fracture line. Type III fractures are considered nonunions. History reveals history of pain with recurrent symptoms, likely representing repetitive insults, and on plain films, the fracture line is widened with medullary canal replaced by sclerosis. Initial treatment recommendations of nonweightbearing in a short leg cast for Type I injuries and curettage and bone grafting for Type II and III injuries were based on Torg’s experience with 46 fractures.97 Operative treatment has yielded good results using an intramedullary malleolar screw, and tension band wiring has been used with similar outcomes.29,51 Placement of these screws can be technically challenging as the surgeon inserts a straight screw into the curved proximal metatarsal. Intraoperative fracture of the metatarsal shaft, bicortical penetration, and skin irritation proximally are potential complications of intramedullary fixation. Seven to 10 weeks postoperatively is a reasonable goal for return to full sport activity following screw fixation and has led to screw fixation for not only Torg Type II and III, but also Type I for a faster return to sports.29,77 Curettage and bone grafting in addition to screw fixation is also an option for Type II and III surgical treatment.12,35 In a study of elite athletes, a plantar gapping of the fracture of >1 mm increases time to union (71 vs 126 days) postsurgical fixation.50 Currently, it is recommended that Type I injuries undergo a 6- to 8-week trial of nonweightbearing in a short leg cast and Type II and III injuries undergo surgical fixation.77,97 An exception is a high-level athlete who wishes to return to sport sooner, in which case surgical fixation of an acute stress fracture may be considered.77 These patients must be warned though that refracture in spite of intramedullary fixation is possible, and returning too soon is a risk factor.48,104 Functional bracing or orthotics upon return to sports may reduce the high rate of refracture seen in that series.48,104
Sesamoid
The medial sesamoid is more commonly injured because of its position directly under the first metatarsal head.9 Activities involving repetitive, forceful dorsiflexion of the toes are most commonly associated.9,16 Swelling or even bulging soft tissues may be present, and pain is reproduced with forced dorsiflexion.9,16 Radiographic differential includes bipartite sesamoid, which is difficult to distinguish on plain films but is seen in 5% to 30% of the general population.9,16 Sagittal cuts on CT scan may be superior to MRI or bone scan when advanced imaging is needed.9 Initial treatments include shoe modification, immobilization, cessation of sport, partial or nonweightbearing, systemic anti-inflammatories, and steroid injections.9,16,76,100 Operative treatment including sesamoidectomy,88,100 partial sesamoidectomy,9,80 closed reduction and percutaneous screw placement,11 curettage, and bone grafting3 with success rates of 90% to 100% union and 100% return to sports.3,9,11,80,88,100 Surgical complications include hallux valgus and flexor hallucis brevis tendon dysfunction, so careful dissection of the sesamoid out of the flexor tendon sheath is important.9,76,88,100
Low-Risk Stress Fractures
Low-risk stress fractures of the foot include those of the calcaneus cuboid, cuneiform bones, and the lateral malleolus, each of which usually heals with nonoperative management.13,16,18,21,35,46,57,58,63,105 Low-risk stress fractures of the foot are common in patients undergoing new occupations or physical training regimens involving repetitive motion.13,18,58,62,63
Calcaneus
The incidence of calcaneal stress fractures is highest in military recruits and long-distance runners.35,40,95,106 A positive calcaneal compression test with some amount of swelling is usually present.35,40,49,103 The diagnosis is often missed initially because of similarity to plantar fasciitis, Baxter nerve entrapment and insertional achilles tendonitis, atrophic heel pad and retrocalcaneal bursitis, and in adolescents, Sever disease or calcaneal apophysitis.35 Plain films will often show a sclerotic or radiolucent line after 2 to 3 weeks of symptoms, and a bone scan or MRI could be helpful to rule out soft tissue diagnoses (Figure 5).35,95,106 Calcaneal stress fractures can be adequately treated with activity modification without casting or surgical intervention.40,49,103 In a more recent Finnish military study of 34 stress injuries (reactions and fractures), 65% were associated with talar, cuboid, or navicular stress injuries. Nonoperative management was used in all patients; recruits were asymptomatic at an average of 77 days. They concluded that these injuries can be treated nonoperatively with suspension from activity only.106
Figure 5.
T2-weighted MRI showing high signal in the calcaneus.
Cuneiforms, Cuboid, Lateral Malleolus
Cuneiform stress fractures were first reported in 1936 as a march fracture of the medial cuneiform.18,62,63 Stress fractures of the middle and lateral cuneiform have also been reported.21,63 Unlike bones with a diaphysis, the cuneiform and cuboid may not display the usual periosteal callus.18,62,63 Instead, stress fractures may appear as a transverse sclerotic zone.18,62,63 MRI is the imaging of choice if plain films are unremarkable.18 These injuries will demonstrate the fracture line with bone marrow edema on both T2- and T1-weighted images.13,18,35,62
The 2 forces responsible for cuneiform stress fractures are bending and compression.18,63 Bending forces are applied across the cuneiforms due to their location in the midfoot. The medial cuneiform lies in the axis of the first metatarsal and is susceptible to compression-type stress fractures.18,63 Body weight passes through this axis, and muscular insertions on each side of the first cuneiform exert strong opposing forces across a small area.18,63 The lateral cuneiform is the keystone of the arch with 6 articulations leading to several force vectors across this bone.18,63
The mainstay of treatment of low-risk stress fractures is nonoperative.13,35,46,58,62,63 Initially, partial weightbearing from 2 to 6 weeks with or without immobilization is recommended until pain has abated during weightbearing activities.13,35,46,58,63
Other Treatments
Bisphosphonates
Bisphosphonates have the potential to decrease the incidence of stress fractures by decreasing bone turnover by inhibiting osteoclast function.4,32,65 However, a prospective, randomized trial of 324 military recruits showed no difference in the incidence of stress fractures of the lower extremities between those receiving prophylactic risedronate and placebo.65 There was a trend toward a harmful effect of alendronate treatment in an animal study, possibly due to inhibition of remodeling of microfractures from woven to lamellar bone.4 The 25-year experience of the Israeli Army on prevention of stress fractures showed sleep minimums and training modifications, but not bisphosphonate treatment, decreased the incidence of stress fractures.32
Bone Stimulators
There are 2 types of stimulators, electromagnetic stimulators and ultrasound stimulators.
Electromagnetic stimulators generate electromagnetic fields with coils on either side of the fracture.15 Mechanical stresses cause fluid flow around and through bones that induces electrical currents around cells, which can open calcium channels in cell membranes increasing calmodulin, thus increasing cell proliferation.15 Very few controlled studies are available that evaluate the efficacy of these stimulators in stress fractures. One such study found no significant difference in time to healing between placebo and those using an electromagnetic stimulator.6 However, when higher grade stress fractures were compared exclusively, there was significantly shorter time to healing noted, though power was not sufficient to draw conclusions.6 When compliance was adequate, electromagnetic stimulators correlated to shorter healing time.6 Despite some early promising results, electromagnetic stimulators have not been shown conclusively to enhance healing in stress fractures.
Pulsed ultrasound bone stimulators can increase vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF), which promote angiogenesis, and increase alkaline phosphatase, bone sialoprotein, and intracellular calcium (markers of bone metabolism).45 Most studies report on acute fractures. A systematic review of pulsed ultrasound showed low to moderate grade evidence for a positive effect: there was a 33.6% decrease in radiographic healing time.20 Stress fractures may respond differently to pulsed ultrasound because they heal through intramembranous remodeling instead of endochondral remodeling as acute fractures do. Literature specifically on stress fractures treated with pulsed ultrasound is sparse.53,83 In a military study of 43 tibial shaft stress fractures, there was no significant difference in time to healing using low-intensity pulsed ultrasound.83 In a rat ulnar stress fracture model, low-intensity pulsed ultrasound alone produced better results than ultrasound and NSAIDs combined as well as controls.53
Oral Contraceptives
Low levels of sex steroids are associated with low bone mineral density.26,101 Abnormally low levels of sex hormones are seen for 24 to 48 hours in endurance athletes following rigorous training sessions, and secondary amenorrhea causes a hormone deficient state.26,101 Hormone replacement therapy via oral contraceptive pills (OCPs) is controversial. Data suggest that hormone replacement in amenorrheic women and endurance athletes improves bone mineral density.25-27 A randomized study of 150 young female runners with low-dose OCP or no treatment showed that oligo- and amenorrheic runners who used OCPs gained 1% bone mineral density (BMD) per year.24 Stress fracture incidence trended lower in the OCP group, but was not significant. A military study of female recruits found a fivefold increase in lower extremity stress fractures in women who had been amenorrheic, though OCP use did not have a significant protective effect.100
If OCPs are used in exercise-induced hypoestrogenic amenorrhea, other factors such as nutrition status or other hypothalamic perturbations should be worked up and may require treatment, as energy status, calcium intake, and body mass index have proven to be independent predictors of improved BMD and normal bone turnover.24,25,34
Calcium and Vitamin D
Calcium and vitamin D can improve BMD but are not definitively proven to prevent stress fractures.8,23,24,47,68,72,84 In track and field athletes and military recruits, no significant difference was found with increased calcium and vitamin D intake and incidence of all types of stress fractures.8 One of the largest studies on the topic showed that in female military recruits, 2000 mg of calcium and 800 IU of vitamin D daily had a 20% lower incidence of stress fractures during basic training than those taking a placebo.47 Another group found that each cup of skim milk consumed daily by female distance runners lowered the rate of stress fracture by 62%.72 These reports support several previous studies suggesting that low dietary calcium and vitamin D is associated with increased risk of stress fracture, and adequate intake or supplementation can reduce the risk of stress fractures.68,94 The recommended daily dose of calcium depends on age, while vitamin D intake is more controversial.2,37,69,70 A specific amount of calcium and vitamin D needed to prevent stress fractures has not been determined. In some studies, daily supplementation of 500 to 800 mg of calcium and 400 to 800 IU vitamin D improves BMD and decreases fracture (not specifically stress fracture) risk significantly.10,36
Calcitonin
Calcitonin inhibits osteoclasts, the offending agent in the imbalanced remodeling process of stress fractures.40,41,54,56 Increased BMD and biomechanical properties has been shown with calcitonin, but its role in stress fracture prevention or healing is controversial.40,41,54,56
Orthotics
Several biomechanical studies have shown predictable, repetitive stress patterns in the foot and ankle with weightbearing.61,79 However, there is inconclusive data to support orthotics for prevention of stress fractures of the foot and ankle.31,32,66,92 A systematic review of 5 articles on orthotics and stress fractures concluded that orthotic use reduced the overall rate of stress fractures of the proximal femur and tibia in military personnel; no conclusion could be made regarding prevention in stress fractures of the foot and ankle.92
Conclusion
Stress fractures of the foot and ankle in athletes are relatively uncommon at 1% of all athletic injuries.12 However, a heightened awareness of this condition by coaches, athletic trainers, therapists, and physicians along with more rigorous training has contributed to an increasing incidence of stress fractures.55 A change in training conditions, such as increased time or distance, new impact activities, training surface, technique, and poor nutrition, is a contributing factor in the development of stress fractures.35 Additionally, in the female athletic population, coaches, athletes, and families should be educated and alerted to the adverse effects of eating disorders and hormonal abnormalities.5,24,26,101 The type of injury (high and low risk) as well as the demands of the patient will drive nonoperative versus operative treatment.12,13,35 There are mixed results with bone stimulators,6,7,20,45,53,83 bisphosphonates,4,32,65 hormone replacement,24-27,90,101 and dietary supplementation of calcium and vitamin D8,48,68,72,84 for prevention or treatment of stress fractures of the foot and ankle. There are no data to support or refute the use of calcitonin.
Footnotes
The following authors declared potential conflicts of interest: Selene G. Parekh, MD, MBA, is a consultant for Orthohelix.
References
- 1. Albisetti W, Perugia D, De Bartolomeo O, Tagliabue L, Camerucci E, Calori GM. Stress fractures of the base of the metatarsal bones in young trainee ballet dancers. Int Orthop. 2010;34:51-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Academy of Orthopaedic Surgeons. Recommended calcium and vitamin D intake. http://orthoinfo.aaos.org/topic.cfm?topic=A00317. Published 2000. Accessed August 26, 2010
- 3. Anderson RB, McBryde AM, Jr. Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997;18:293-296 [DOI] [PubMed] [Google Scholar]
- 4. Barrett JG, Sample SJ, McCarthy J, Kalsheur VL, Muir P, Prokuski L. Effect of short-term treatment with alendronate on ulnar bone adaptation to cyclic fatigue loading in rats. J Orthop Res. 2007;25:1070-1077 [DOI] [PubMed] [Google Scholar]
- 5. Barrow GW, Saha S. Menstrual irregularity and stress fractures in collegiate female distance runners. Am J Sports Med. 1988;16:209-216 [DOI] [PubMed] [Google Scholar]
- 6. Beck BR, Matheson GO, Bergman G, et al. Do capacitively coupled electric fields accelerate tibial stress fracture healing? A randomized controlled trial. Am J Sports Med. 2008;36:545-553 [DOI] [PubMed] [Google Scholar]
- 7. Benazzo F, Mosconi M, Beccarisi G, Galli U. Use of capacitative coupled electric fields in stress fractures in athletes. Clin Orthop Relat Res. 1995;310:145-149 [PubMed] [Google Scholar]
- 8. Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996;24:810-818 [DOI] [PubMed] [Google Scholar]
- 9. Biedert R, Hintermann B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int. 2003;24:137-141 [DOI] [PubMed] [Google Scholar]
- 10. Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293:2257-2264 [DOI] [PubMed] [Google Scholar]
- 11. Blundell CM, Nicholson P, Blackney MW. Percutaneous screw fixation for fractures of the sesamoid bones of the hallux. J Bone Joint Surg Br. 2002;84:1138-1141 [DOI] [PubMed] [Google Scholar]
- 12. Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8:344-353 [DOI] [PubMed] [Google Scholar]
- 13. Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-111 [DOI] [PubMed] [Google Scholar]
- 14. Bradshaw C, Khan K, Brukner P. Stress fracture of the body of the talus in athletes demonstrated with computer tomography. Clin J Sports Med. 1996;6:48-51 [DOI] [PubMed] [Google Scholar]
- 15. Brighton CT, Wang W, Seldes R, Zhang G, Pollack SR. Signal transduction in electrically stimulated bone cells. J Bone Joint Surg Am. 2001;83:1514-1523 [DOI] [PubMed] [Google Scholar]
- 16. Brockwell J, Yeung Y, Griffith JF. Stress fractures of the foot and ankle. Sports Med Arthrosc Rev. 2009;17:149-159 [DOI] [PubMed] [Google Scholar]
- 17. Brukner P, Bradshaw C, Khan KM, White S, Crossley K. Stress fractures: a review of 180 cases. Clin J Sports Med. 1996;6:85-89 [PubMed] [Google Scholar]
- 18. Bui-Mansfield LT, Thomas WR. Magnetic resonance imaging of stress injury of the cuneiform bones in patients with plantar fasciitis. J Comput Assist Tomogr. 2009;33:593-596 [DOI] [PubMed] [Google Scholar]
- 19. Burne SG, Mahoney CM, Forster BB, Koehle MS, Taunton JE, Khan KM. Tarsal navicular stress injury: long-term outcome and clinicoradiologic correlation using both computed tomography and magnetic resonance imaging. Am J Sports Med. 2005;33:1875-1881 [DOI] [PubMed] [Google Scholar]
- 20. Busse JW, Kaur J, Mollon B, et al. Low intensity pulsed ultrasonography for fractures: systematic review of randomized controlled trials. BMJ. 2009;27:338-351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Childress HM. March fractures of the lower extremity. Report of a case of March fracture of a cuneiform bone. War Medicine. 1943;4:152-160 [Google Scholar]
- 22. Chuckpaiwong B, Cook C, Nunley JA. Stress fractures of the second metatarsal base occur in nondancers. Clin Orthop Relat Res. 2007;461:197-202 [DOI] [PubMed] [Google Scholar]
- 23. Cline AD, Jansen GR, Melby CL. Stress fractures in female Army recruits: implications of bone density, calcium intake, and exercise. J Am Coll Nutr. 1998;17:128-135 [DOI] [PubMed] [Google Scholar]
- 24. Cobb KL, Bachrach LK, Sowers M, et al. The effect of oral contraceptives on bone mass and stress fractures in female runners. Med Sci Sports Exerc. 2007;39:1464-1473 [DOI] [PubMed] [Google Scholar]
- 25. Cumming DC. Exercise-induced amenorrhea, low bone density, and estrogen replacement therapy. Arch Int Med. 1996;156:2193-2195 [PubMed] [Google Scholar]
- 26. Cumming DC, Cumming CE. Estrogen therapy and female athletes: current issues. Sports Med. 2001;31:1025-1031 [DOI] [PubMed] [Google Scholar]
- 27. De Cree C, Lewin R, Ostyn M. Suitability of cyproterone acetate in the treatment of osteoporosis associated with athletic amenorrhea. Int J Sports Med. 1988;9:187-192 [DOI] [PubMed] [Google Scholar]
- 28. De Souza MJ, West SL, Jamal SA, Hawker GA, Gundberg CM, Williams NI. The presence of both an energy deficiency and estrogen deficiency exacerbate alterations of bone metabolism in exercising women. Bone. 2008;43:140-148 [DOI] [PubMed] [Google Scholar]
- 29. DeLee JC, Evans JP, Julian J. Stress fracture of the fifth metatarsal. Am J Sports Med. 1983;11:349-353 [DOI] [PubMed] [Google Scholar]
- 30. Duckham RL, Peirce N, Meyer C, Summers GD, Cameron N, Brooke-Wavell K. Risk factors for stress fracture in female endurance athletes: a cross-sectional study. BMJ Open. 2012;2:e001920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Finestone A, Giladi M, Elad H, et al. Prevention of stress fractures using custom biomechanical shoe orthoses. Clin Orthop Relat Res. 1999;360:182-190 [DOI] [PubMed] [Google Scholar]
- 32. Finestone A, Milgrom C. How stress fracture incidence was lowered in the Israeli army: a 25-year struggle. Med Sci Sports Exerc. 2008;40(suppl 11):S630-635 [DOI] [PubMed] [Google Scholar]
- 33. Fitch KD, Blackwell JB, Gilmour WN. Operation for non-union of stress fracture of the tarsal navicular. J Bone Joint Surg Br. 1989;71:105-110 [DOI] [PubMed] [Google Scholar]
- 34. Fredericson M, Kent K. Normalization of bone density in a previously amenorrheic runner with osteoporosis. Med Sci Sports Exerc. 2005;37:1481 [DOI] [PubMed] [Google Scholar]
- 35. Gehrmann RM, Renard RL. Current concepts review: stress fractures of the foot. Foot Ankle Int. 2006;27:750-757 [DOI] [PubMed] [Google Scholar]
- 36. Grados F, Brazier M, Kamel S, et al. Effects on bone mineral density of calcium and vitamin D supplementation in elderly women with vitamin D deficiency. Joint Bone Spine. 2003;70:203-208 [DOI] [PubMed] [Google Scholar]
- 37. Greer FR, Krebs NF, American Academy of Pediatrics Committee on Nutrition. Optimizing bone health and calcium intakes of infants, children, and adolescents. Pediatrics 2006;117:578-585 [DOI] [PubMed] [Google Scholar]
- 38. Gross TS, Bunch RP. A mechanical model of metatarsal stress fracture during distance running. Am J Sports Med. 1989;17:669-674 [DOI] [PubMed] [Google Scholar]
- 39. Harrington T, Crighton KJ, Anderson IF. Overuse ballet injury of the base of the second metatarsal. A diagnostic problem. Am J Sports Med. 1993;21:591-598 [DOI] [PubMed] [Google Scholar]
- 40. Hullinger CW. Insufficiency fractures of the calcaneus. J Bone Joint Surg. 1944;26:751-757 [Google Scholar]
- 41. Jiang Y, Zhao J, Geusens P, et al. Femoral neck trabecular microstructure in ovariectomized ewes treated with calcitonin: MRI microscopic evaluation. J Bone Miner Res. 2005;20:125-130 [DOI] [PubMed] [Google Scholar]
- 42. Jowett AJ, Birks C, Blackney M. Medial malleolar stress fracture secondary to chronic ankle impingement. Foot Ankle Int. 2008;29:716-721 [DOI] [PubMed] [Google Scholar]
- 43. Khan KM, Fuller PJ, Brukner PD, Kearney Burry HC. Outcome of conservative and surgical management of navicular stress fracture in athletes. Eighty-six cases proven with computerized tomography. Am J Sports Med. 1992;20:657-666 [DOI] [PubMed] [Google Scholar]
- 44. Khan KM, Brukner PD, Kearney C, Fuller PJ, Bradshaw CJ, Kiss ZS. Tarsal navicular stress fracture in athletes. Sports Med. 1994;17:65-76 [DOI] [PubMed] [Google Scholar]
- 45. Khan Y, Laurencin CT. Fracture repair with ultrasound: clinical and cell-based evaluation. J Bone Joint Surg Am. 2008;90(suppl 1):S138-144 [DOI] [PubMed] [Google Scholar]
- 46. Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk factors for recurrent stress fractures in athletes. Am J Sports Med. 2001;29:304-310 [DOI] [PubMed] [Google Scholar]
- 47. Lappe J, Cullen D, Haynatzki G, Recker R, Ahlf R, Thompson K. Calcium and vitamin D supplementation decreases incidence of stress fractures in female navy recruits. J Bone Miner Res. 2008;23:741-749 [DOI] [PubMed] [Google Scholar]
- 48. Larson CM, Almekinders LC, Taft TN, Garrett WE. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am J Sports Med. 2002;30:55-60 [DOI] [PubMed] [Google Scholar]
- 49. Leabhart JW. Stress fractures of the calcaneus. J Bone Joint Surg. 1959;41:1285-1290 [PubMed] [Google Scholar]
- 50. Lee KT, Park YU, Young KW, Kim JS, Kim JB. The plantar gap: another prognostic factor for fifth metatarsal stress fracture. Am J Sports Med. 2012;40:915-919 [DOI] [PubMed] [Google Scholar]
- 51. Lee KT, Park YU, Young KW, Kim JS, Kim JB. Surgical results of 5th metatarsal stress fracture using modified tension band wiring. Knee Surg Sports Traumatol Arthrosc. 2011;19:853-857 [DOI] [PubMed] [Google Scholar]
- 52. Lempainen L, Liimatainen E, Heikkila, et al. Medial malleolar stress fracture in athletes: diagnosis and operative treatment. Scand J Surg. 2012;101:261-264 [DOI] [PubMed] [Google Scholar]
- 53. Li J, Waugh LJ, Hui SL, Warden SJ. Low-intensity pulsed ultrasound and nonsteroidal anti-inflammatory drugs have opposing effects during stress fracture repair. J Orthop Res. 2007;25:1559-1567 [DOI] [PubMed] [Google Scholar]
- 54. Li X, Luo X, Yu N, Zeng B. Effects of salmon calcitonin on fracture healing in ovariectomized rats. Saudi Med J. 2005;28:60-64 [PubMed] [Google Scholar]
- 55. Maitra RS, Johnson DL. Stress fractures clinical history and physical examination. Clin Sports Med. 1997;16:260-274 [DOI] [PubMed] [Google Scholar]
- 56. Manabe T, Mori S, Mashiba T, et al. Eel calcitonin (elcatonin) suppressed callus remodeling but did not interfere with fracture healing in the femoral fracture model of cynomolgus monkeys. J Bone Miner Metab. 2009;27:295-302 [DOI] [PubMed] [Google Scholar]
- 57. Maseritz IH. March foot associated with undescribed changes of the internal cuneiform and metatarsal bones. Arch Surg. 1936;32:49-64 [Google Scholar]
- 58. Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, Macintyre JG. Stress fractures in athletes: a study of 320 cases. Am J Sports Med. 1987;15:46-58 [DOI] [PubMed] [Google Scholar]
- 59. McCormick JJ, Bray CC, Davis WH, Cohen BE, Jones CP, Anderson RB. Clinical and computed tomography evaluation of surgical outcomes in tarsal navicular stress fractures. Am J Sports Med. 2011;39:1741-1748 [DOI] [PubMed] [Google Scholar]
- 60. McGlone JJ. Stress fracture of the talus. J Am Podiatr Med Assoc. 1965;55:814-817 [DOI] [PubMed] [Google Scholar]
- 61. Meardon SA, Edwards B, Ward E, Derrick TR. Effects of custom and semi-custom foot orthotics on second metatarsal bone strain during dynamic gait stimulation. Foot Ankle Int. 2009;30:998-1004 [DOI] [PubMed] [Google Scholar]
- 62. Meurman KOA. Less common stress fractures in the foot. Br J Radiol. 1981;54:1-7 [DOI] [PubMed] [Google Scholar]
- 63. Meurman KOA, Elfving S. Case reports: stress fracture of the cuneiform bones. Br J Radiol. 1980;53:157-160 [DOI] [PubMed] [Google Scholar]
- 64. Micheli LJ, Sohn RS, Solomon R. Stress fractures of the second metatarsal involving Lisfranc’s joint in ballet dancers. A new overuse injury of the foot. J Bone Joint Surg Am. 1985;67:1372-1375 [PubMed] [Google Scholar]
- 65. Milgrom C, Finestone A, Novack V, et al. The effect of prophylactic treatment with risedronate on stress fracture incidence among infantry recruits. Bone. 2004;35:418-424 [DOI] [PubMed] [Google Scholar]
- 66. Milgrom C, Giladi M, Kashtan H, et al. A prospective study of the effect of a shock-absorbing orthotic device on the incidence of stress fractures in military recruits. Foot Ankle. 1985;6:101-104 [DOI] [PubMed] [Google Scholar]
- 67. Muscolo L, Migues A, Slullitel G, Costa-Paz M. Stress fracture nonunion at the base of the second metatarsal in a ballet dancer: a case report. Am J Sports Med. 2004;32:1535-1537 [DOI] [PubMed] [Google Scholar]
- 68. Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Ann Intern Med. 1990;113:754-759 [DOI] [PubMed] [Google Scholar]
- 69. National Institutes of Health Office of Dietary Supplements. Dietary supplement fact sheet calcium. http://ods.od.nih.gov/factsheets/calcium. Published 2009. Accessed August 26, 2010
- 70. National Institutes of Health Office of Dietary Supplements. Dietary supplement fact sheet vitamin D. http://ods.od.nih.gov/factsheets/vitamind. Published 2009. Accessed August 26, 2010
- 71. Nattiv A. Stress fractures and bone health in track and field athletes: J Sci Med Sport. 2000;3:268-279 [DOI] [PubMed] [Google Scholar]
- 72. Nieves JW, Melsop K, Curtis M, et al. Nutritional factors that influence change in bone density and stress fracture risk among young female cross-country runners. PM R. 2010;2:740-750 [DOI] [PubMed] [Google Scholar]
- 73. Niva MH, Sormaala MJ, Kiuru MJ, Haataja R, Ahovuo JA, Pihlajamaki HK. Bone stress injuries of the ankle and foot: an 86-month magnetic resonance imaging-based study of physically active young adults. Am J Sports Med. 2007;35:643-649 [DOI] [PubMed] [Google Scholar]
- 74. O’Malley MJ, Hamilton WG, Munyak J, DeFranco MJ. Stress fractures at the base of the second metatarsal in ballet dancers. Foot Ankle Int. 1996;17:89-94 [DOI] [PubMed] [Google Scholar]
- 75. Orava S, Karpakka J, Taimela S, Hulkko A, Permi J, Kujala U. Stress fracture of the medial malleolus. J Bone Joint Surg Am. 1995;77:362-365 [DOI] [PubMed] [Google Scholar]
- 76. Pagenstert GI, Valderrabano V, Hintermann B. Medial sesamoid nonunion combined with hallux valgus in athletes: a report of two cases. Foot Ankle Int. 2006;27:135-140 [DOI] [PubMed] [Google Scholar]
- 77. Papalada A, Malliaropoulos N, Tsitas K, et al. Ultrasound as a primary evaluation tool of bone stress injuries in elite track and field athletes. Am J Sports Med. 2012;40:915-919 [DOI] [PubMed] [Google Scholar]
- 78. Porter DA, Duncan M, Meyer SJ. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete: a clinical and radiographic evaluation. Am J Sports Med. 2005;33:726-733 [DOI] [PubMed] [Google Scholar]
- 79. Prather JL, Nusynowitz ML, Snowdy HA, Hughes AD, McCartney WH, Bagg RJ. Scintigraphic findings in stress fractures. J Bone Joint Surg Am. 1977;59:869-874 [PubMed] [Google Scholar]
- 80. Queen RM, Abbey AN, Chuckpaiwong Nunley JA. Plantar loading comparisons between women with a history of second metatarsal stress fractures and normal controls. Am J Sports Med. 2009;37:390-395 [DOI] [PubMed] [Google Scholar]
- 81. Rodeo SA, Warren RF, O’Brien SJ, Pavlov H, Hanks GA. Diastasis of bipartite sesamoids of the first metatarsophalangeal joint. Foot Ankle. 1993;14:425-434 [DOI] [PubMed] [Google Scholar]
- 82. Rossi F, Dragoni S. Talar body fatigue stress fractures: three cases observed in elite female gymnasts. Skeletal Radiol. 2005;34:389-394 [DOI] [PubMed] [Google Scholar]
- 83. Rue JP, Armstrong DW, III, Frassica FJ, Deafenbaugh M, Wilckens JH. The effect of pulsed ultrasound in the treatment of tibial stress fractures. Orthopedics. 2004;27:1192-1195 [DOI] [PubMed] [Google Scholar]
- 84. Ruffing JA, Cosman F, Zion M, et al. Determinants of bone mass and bone size in a large cohort of physically active young adult men. Nutr Metab(Lond). 2006;15:3-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Sarimo J, Orava S, Alanen J. Operative treatment of stress fractures of the proximal second metatarsal. Scand J Med Sci Sports. 2007;17:383-386 [DOI] [PubMed] [Google Scholar]
- 86. Saxena A, Fullem B. Navicular stress fractures: a prospective study on athletes. Foot Ankle Int. 2006;27:917-921 [DOI] [PubMed] [Google Scholar]
- 87. Saxena A, Fullem B, Hannaford D. Results of treatment of 22 navicular stress fractures and a new proposed radiographic classification system. J Foot Ankle Surg. 2000;22:581-584 [DOI] [PubMed] [Google Scholar]
- 88. Saxena A, Krisdakumtorn T. Return to activity after sesamoidectomy in athletically active individuals. Foot Ankle Int. 2003;24:415-419 [DOI] [PubMed] [Google Scholar]
- 89. Shabat S, Smapson KB, Mann G, et al. Stress fractures of the medial malleolus—review of the literature and report of a 15 year-old gymnast. Foot Ankle Int. 2002;23:647-650 [DOI] [PubMed] [Google Scholar]
- 90. Shaffer RA, Rauh MJ, Brodine SK, Trone DW, Macera CA. Predictors of stress fractures in young female recruits. Am J Sports Med. 2006;34:108-115 [DOI] [PubMed] [Google Scholar]
- 91. Shelbourne KD, Fisher DA, Rettig AC, McCarroll JR. Stress fractures of the medial malleolus. Am J Sports Med. 1988;16:60-63 [DOI] [PubMed] [Google Scholar]
- 92. Snyder RA, DeAngelis JP, Koester MC, Spindler KP, Dunn WR. Does shoe insole modification prevent stress fracture? A systematic review. HSS J. 2009;5:92-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamaki HK. Bone stress injuries of the talus in military recruits. Bone. 2006;39:199-204 [DOI] [PubMed] [Google Scholar]
- 94. Sormaala MJ, Niva MH, Kiuru MJ, Maatila VM, Pihlajamaki HK. Outcomes of stress fractures of the talus. Am J Sports Med. 2006;34:1809-1814 [DOI] [PubMed] [Google Scholar]
- 95. Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamaki HK. Stress injuries of the calcaneus detected with magnetic resonance imaging in military recruits. J Bone Joint Surg Am. 2006;88:2237-2242 [DOI] [PubMed] [Google Scholar]
- 96. Stanitski CL, McMaster JH, Scranton PE. On the nature of stress fractures. Am J Sports Med. 1978;6:391-396 [DOI] [PubMed] [Google Scholar]
- 97. Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am. 1984;66:209-214 [PubMed] [Google Scholar]
- 98. Torg JS, Moyer J, Gaughan JP, Boden BP. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010;38:1048-1053 [DOI] [PubMed] [Google Scholar]
- 99. Torg JS, Pavlov H, Cooley LH. Stress fractures of the tarsal navicular. A retrospective review of twenty-one cases. J Bone Joint Surg Am. 1982;64:700-712 [PubMed] [Google Scholar]
- 100. Van Hal ME, Keene JS, Lange TA, Clancy WG, Jr. Stress fractures of the great toe sesamoids. Am J Sports Med. 1982;10:122-128 [DOI] [PubMed] [Google Scholar]
- 101. Voss LA, Fadale PD, Hulstyn MJ. Exercise-induced loss of bone density in athletes. J Am Acad Orthop Surg. 1998;6:349-357 [DOI] [PubMed] [Google Scholar]
- 102. Weist R, Eils E, Rosenblum D. The influence of muscle fatigue on electromyogram and plantar pressure patterns as an explanation for the incidence of metatarsal stress fractures. Am J Sports Med. 2004;32:1893-1898 [DOI] [PubMed] [Google Scholar]
- 103. Wilson ES, Katz FN. Stress fractures. An analysis of 250 consecutive cases. Radiology 1969;. 92: 481-486 [DOI] [PubMed] [Google Scholar]
- 104. Wright RW, Fischer DA, Shively RA, Heidt RS, Nuber GW. Refracture of proximal fifth metatarsal (Jones) fracture after intramedullary screw fixation in athletes. Am J Sports Med. 2000;28:732-736 [DOI] [PubMed] [Google Scholar]
- 105. Yu JS, Solmen J. Stress fractures associated with plantar fascia disruption: two cases involving the cuboid. J Comput Assist Tomogr. 2001;25:971-974 [DOI] [PubMed] [Google Scholar]
- 106. Yu JS, Spignos D, Tomczak R. Foot pain after a plantar fasciotomy: an MR analysis to determine potential causes. J Comput Assist Tomogr. 1999;23:707-712 [DOI] [PubMed] [Google Scholar]


