Abstract
Context:
Injuries of the first metatarsophalangeal (hallux MP) joint can be debilitating in the athletic population. Turf toe and plantar plate injuries are typically diagnosed similarly. However, variance in injury mechanism as well as compromised integrity of soft tissue and ligamentous structures make it difficult to accurately diagnose specific hallux MP injuries. Recent literature has supported the use of both radiographic imaging and the Lachman test as reliable indicators of joint instability in the presence of hallux MP injuries. To date, research supporting specific rehabilitation interventions and return-to-play decision making for hallux MP injuries has been limited to case studies and suggested guidelines from literature reviews. There is limited evidence suggesting specific criteria for surgical and nonsurgical decision making in conjunction with rehabilitation progressions to return an athlete to sport when managing hallux MP injuries.
Evidence Acquisition:
A literature search was performed using Medline, PubMed, and Google Scholar to find and review articles from 1970 to 2013 that addressed the basic anatomy of the plantar plate, injuries to this anatomical structure, and the evaluation, diagnosis, surgical and nonsurgical management, and rehabilitation of these injuries, specifically in the athletic population. Medical information for each case was gathered from electronic medical records from the individual athletes cited in this case series, which included imaging reports, rehabilitation documentation, and both evaluation and surgical reports. No statistical analysis was used.
Study Design:
Case series.
Level of Evidence:
Level 4.
Results:
Treatment plans for each case varied depending on surgical and nonsurgical intervention and rehabilitation outcomes. However, each athlete was able to return to sports-specific activities.
Conclusion:
Successful outcomes for hallux MP injuries are contingent on thorough evaluation, appropriate clinical decision making with regard to surgical versus nonsurgical treatment planning, and a multidisciplinary team approach for ensuring a safe return to sport.
Strength-of-Recommendation Taxonomy (SORT):
C.
Keywords: plantar plate, turf toe, rehabilitation
Injuries that involve the first metatarsophalangeal (hallux MP) joint can significantly affect foot mechanics and gait. While the commonly recognized mechanism of injury involving the hallux is a hyperextension force on a fixed foot,2 valgus force or axial loading can further complicate the injury because of increased involvement of capsular, ligamentous, or sesamoid structures. Injury to the sesamoids or to the plantar plate (Figure 1),18 the ligament that connects the proximal phalanx to the metatarsal head, can lead to both chronic pain and an unstable joint. Commonly referred to as a “turf toe injury,”4,7-9 the increased incidence of injury can be attributed to light, flexible footwear; artificial surfaces; and sports that require repetitive loading of the hallux MP joint.4,7-9 Additional precipitating factors include prior hallux MP injury, foot pronation, flattening of the hallux MP joint, increased toe box flexibility, decreased number of cleats in the shoe, and hallux degenerative joint disease.4,7-9 Sport position has also been previously discussed as a risk factor for metatarsophalangeal joint injuries.16,17 Numerous studies have reported the incidence of turf toe injuries in college football athletes who played on artificial surfaces.4,7,9 The first prevalence study of turf toe injuries in professional football athletes reported that 36 of 80 professional football athletes had sustained a turf toe injury at some point in their professional or collegiate careers; a higher percentage of these injuries occurred in athletes whose teams used artificial turf on their home field.17 There was an increased incidence of a pes planus foot type in cases of turf toe injuries. Subsequently, professional football athletes with a history of turf toe injury appear to have less hallux MP dorsiflexion.5 Similar injuries have also been reported in soccer, wrestling, basketball, and dancing because of repetitive loading during activities that require push-off and change of direction.2,10,11,18 The ability to perform sports-related activities is challenged as the severity of injury and recovery timelines are highly variable and difficult to assess accurately.2 Untreated injuries to the hallux MP joint can eventually lead to a permanent decrease in range of motion and osteoarthritis.13 The Lachman test of the great toe is an important clinical exam used to determine the stability of the plantar plate.14
Figure 1.
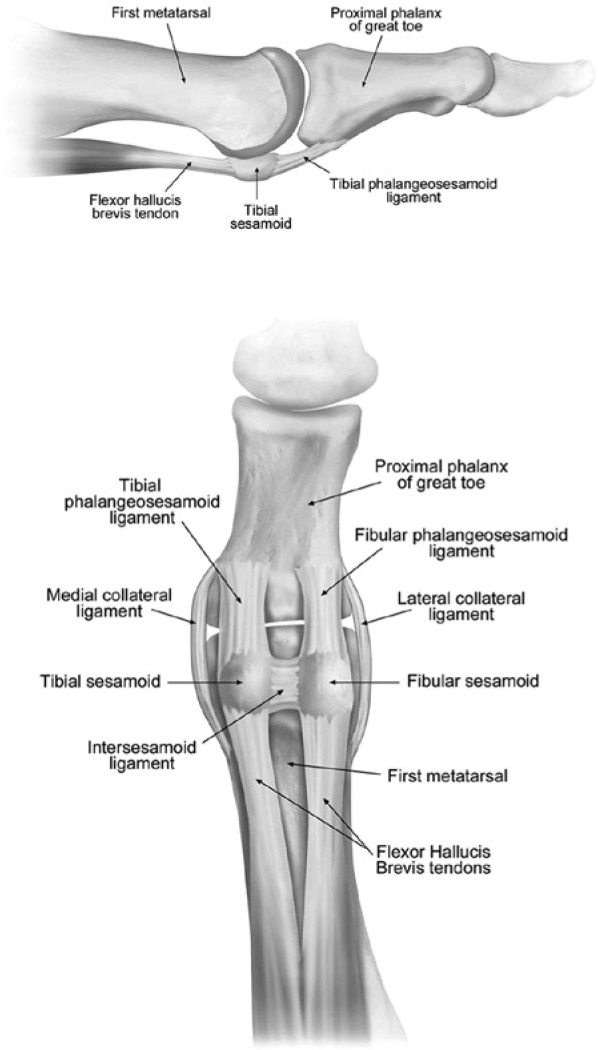
Anatomy of the plantar plate. Reprinted with permission from Waldrop et al.18
This is a case series of 5 Division 1 male collegiate athletes with injuries of the hallux MP joint. This report compares the intervention strategies and outcomes when managing injuries involving the hallux MP joint.
Case 1
A 19-year-old (height, 175 cm; weight, 86 kg) running back sustained an injury 4 weeks into preseason football camp when he was tackled from behind while making a catch, resulting in dorsiflexion at the talocrural joint with forced hyperextension at the MP joint. He felt a “pop” and had increased pain when bearing weight on his right foot. He had swelling and tenderness to palpation along the hallux MP joint along with decreased active range of motion compared with his left side. The Lachman test of the toe was negative, indicating at least partial integrity of the plantar plate. Radiographic stress view showed minimal proximal migration (Figure 2). Magnetic resonance imaging (MRI) confirmed partial ligament disruption (Figure 3). The tibial sesamoid ligament and the flexor musculature of the toe and foot were uninjured. The injury was diagnosed as a grade 2 partial tear of the plantar plate ligament. Initial management utilized plantar flexion taping of the hallux MP joint (Figure 4) and a CAM boot (Foam Walker, Air Cast; DJO Global, Vista, California) with insole and toe cutout (Figure 5) for the first 2.5 weeks before progressing to partial weightbearing at week 3 and full weightbearing at week 4, as symptoms allowed. The toe cutout allowed the great toe to remain plantar flexed and minimized dorsiflexion-directed force on the MP joint during this weightbearing progression. Radiographs at week 4 indicated improved approximation of the plantar plate ligament, as demonstrated by decreased proximal translation of the sesamoids on lateral dorsiflexion view (Figure 6). Low-grade joint mobilizations were performed, and taping of the first MP joint was continued to protect the injured structures during weightbearing.1 Full weightbearing was allowed with use of a carbon graphite shank and customized orthotic with toe cutout in the athlete’s regular cross-training shoe. At week 6, the athlete had decreased symptoms and improved active range of motion (ROM) of his hallux MP joint. He was cleared to progress into jogging and agility drills as well as noncontact football activities (Table 1). The athlete made a gradual return to full participation at 2 months postinjury. He completed the final 3 weeks of the regular season without reaggravating his injury and did not experience further pain or symptoms.
Figure 2.

Passive extension stress view radiograph.
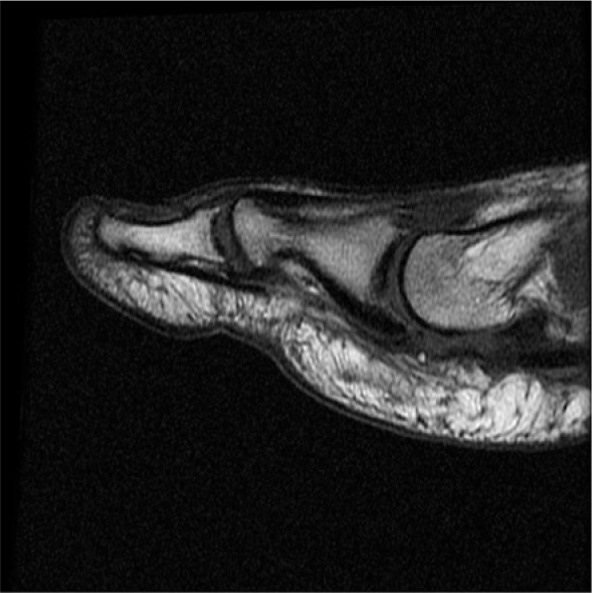
Figure 3.
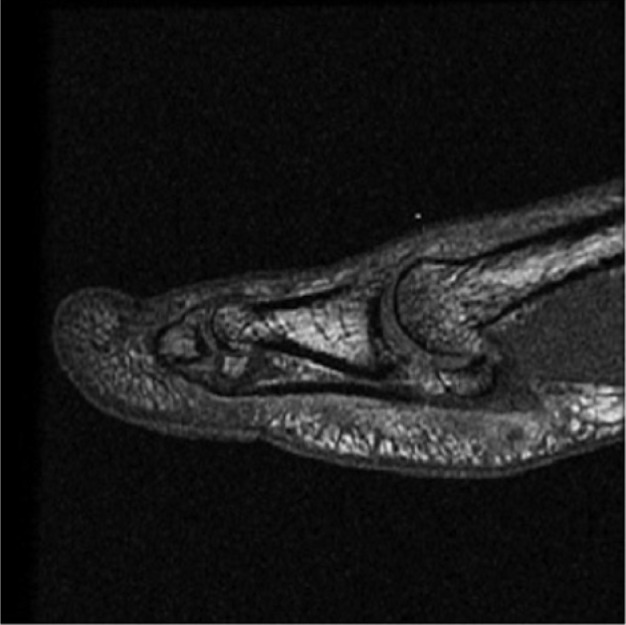
Magnetic resonance imaging confirmed partial ligament disruption of the plantar plate.
Figure 4.

Plantar flexion taping of the first metatarsophalangeal (hallux MP) joint.
Figure 5.

CAM boot with insole and toe cutout.
Figure 6.

Week 4 postinjury radiograph.
Table 1.
Nonsurgical rehabilitation for first metatarsophalangeal (hallux MP) joint injuries
| Phase | Goals | Treatment Interventions | Timeline |
|---|---|---|---|
| Phase 1 | Decrease pain Control swelling and inflammation Sustain ROM |
Ice E-stim for pain control (IFC, TENS) Toe/foot taping Grade 1-2 ankle mobilizations Marble/towel exercises Aquatic exercise |
4-14 days |
| Phase 2 | Increase weightbearing Normalize gait Improve ROM Increase strength (foot, ankle, hips, core musculature) |
Continued modalities as needed Toe/foot taping Customized orthotic Carbon graphite shank Marble/towel exercises Gait training Aquatic exercise Stability exercises Leg raises, band work Grade 3-4 ankle mobilizations Grade 1-2 hallux MP mobilizations |
2-6 weeks |
| Phase 3 | Increase strength Improve proprioception and balance Improve endurance and conditioning |
Customized footwear Aqua jogging Grade 3-4 ankle, hallux MP mobilizations Treadmill jogging/running Single-leg squats/stability exercises Ladder drills Circuit training/conditioning |
6-10 weeks |
ROM, range of motion; E-stim, electrical stimulation; IFC, interferential current; TENS, transcutaneous electrical nerve stimulation.
Case 2
A 21-year-old (height, 180 cm; weight, 102 kg) fullback sustained a hyperextension injury to his left hallux MP joint while attempting to block a teammate during a spring football practice. He had immediate pain, difficulty weightbearing, and was unable to continue practice. Orthopaedic evaluation found a positive Lachman test, with radiographs consistent for retraction of the sesamoids in his left hallux MP joint. MRI confirmed a plantar plate injury with high signal of the distal plantar plate and low T1-weighted signal within the sesamoids because of postinjury edema (Figure 7). Clinical and radiologic evaluation confirmed the unstable joint, and surgical intervention was needed (Figure 8). In surgery, a complete disruption of the plantar plate from the sesamoids extending from medial to lateral along with hemorrhage in the flexor tendon sheath was repaired. He was initially casted in slight plantar flexion with great toe flexion, then was fitted for a bunion strap 2 weeks postsurgery to allow active plantar flexion but no dorsiflexion while nonweightbearing. He progressed to full weightbearing at 6 weeks postsurgery, eventually transitioning into a shoe with a custom orthotic. Rehabilitation followed protocol (Table 2), with progressions postsurgery that included running (10 weeks), agility drills (12 weeks), noncontact football drills (14 weeks), limited contact (16 weeks), and full return to play (18 weeks). He returned to fall football activities, reporting occasional mild dorsal pain with end-range hallux MP dorsiflexion during active motion and pushoff.
Figure 7.
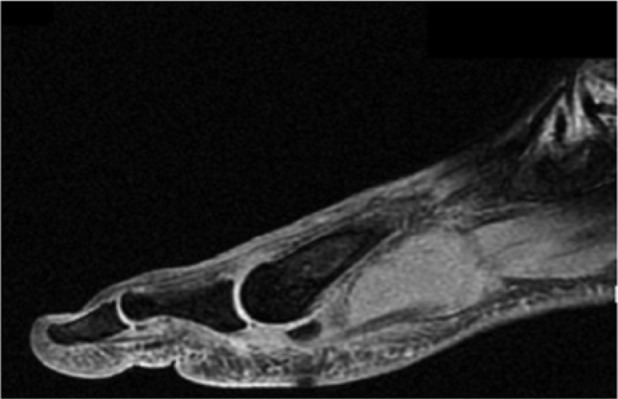
Magnetic resonance imaging–confirmed plantar plate injury.
Figure 8.

Radiographic findings indicating plantar plate injury.
Table 2.
Postoperative rehabilitation for plantar plate injuries
| Phase | Rehabilitation Goals | Treatment Interventions | Timeline |
|---|---|---|---|
| Phase 1 | Protect repair Control pain, swelling, and inflammation Maintain core and hip strength Maintain skin integrity Ensure proper circulation and tissue healing Maintain cardiovascular conditioning |
Immobilization, anti-inflammatory medications Toe spica splint, CAM boot, bunion strap Anti-inflammatory medications Core exercises (TrA activation, marching, bridging) Leg raises, clamshells UBE |
4-6 weeks |
| Phase 2 | Decrease pain, swelling, and inflammation Improve ROM Increase core and hip strength Increase intrinsic muscle and ankle strength Progress weightbearing activities Normalize gait Improve conditioning |
Ice, E-stim for pain control (IFC, TENS) Grade 3-4 ankle, grade 1-2 hallux MP mobilizations Marble/towel and Theraband exercises Squats, controlled heel raises, band exercises, lunges Toe/foot taping, customized orthotics Carbon graphite shank Assisted (crutches)/unassisted gait training Bike, aquatic exercise |
6-10 weeks |
| Phase 3 | No pain or swelling with progressions Improve ROM Improve single leg strength and stability Progress conditioning Initiate agility and plyometric exercises |
Continued modalities, toe/foot taping as needed Customized orthotic, carbon graphite shank Grade 3-4 ankle, grade 3 hallux MP mobilizations Multidirectional lunges, single leg squats Bosu/foam pad balance exercises Bike, aqua jogging, elliptical, treadmill jogging Ladder drills, box jumps, bounds/hopping exercises |
10-12 weeks |
| Phase 4 | Advance agility and plyometric drills Include sports-specific drills and exercises Return to play |
Customized footwear Treadmill jogging/running Single leg squats/stability exercises Ladder/agility drills with multidirectional planting and cutting Circuit training/conditioning Sport participation |
12-20 weeks |
ROM, range of motion; hallux MP, first metatarsophalangeal joint; TrA, transversus abdominis; UBE, upper body ergometry; E-stim, electrical stimulation; IFC, interferential current; TENS, transcutaneous electrical nerve stimulation.
Case 3
A 22-year-old (height, 185.4 cm; weight, 140.6 kg) offensive lineman sustained a left hallux MP joint injury during a football game in week 8 of the fall season after an opposing player fell onto his foot from behind. He felt a “pop” with immediate pain in his big toe and was unable to continue in the game. Physical findings included swelling along the plantar surface of his left hallux MP joint, pain during active toe flexion, and tenderness to palpation along the plantar and medial surfaces. Lachman test results were negative. He had difficulty weightbearing on his left foot. Radiographs showed no fracture or dislocation. MRI revealed plantar plate injury with disruption of the tibial portion and partial injury to the fibular aspect of the plantar plate (Figure 9). The MRI also revealed early hallux MP degenerative changes (Figure 9). This athlete was a redshirt senior and wanted to attempt to complete the season. Being clinically stable, he continued with football activities as tolerated when sufficient progress was seen with physical therapy (Table 1). Taping and a carbon graphite shank in his athletic shoe provided stability and support for the hallux MP joint, and the athlete participated in team warm-up and noncontact drills within 3 weeks postinjury. He was placed in a larger, more rigid football shoe to accommodate the shank and toe taping and was medically cleared to play limited repetitions. During postseason assessments, surgery was recommended because of previous radiological findings, continued pain limiting function, and his desire to pursue professional football. He underwent an open reduction and repair with fixation surgery 1 week following the last game of the season. A complete disruption of the plantar plate on the medial side, a proximal capsular tear one third of the way up through the collateral ligament and abductor tendon on the medial side, and a small chondral lesion of the tibial sesamoid were repaired and addressed in surgery. After surgery, he was placed in a CAM boot with use of a bunion strap to prevent hallux MP dorsiflexion and progressed according to protocol (Table 2). He returned to full football activity at 5 months, including professional football camps, without restrictions.
Figure 9.
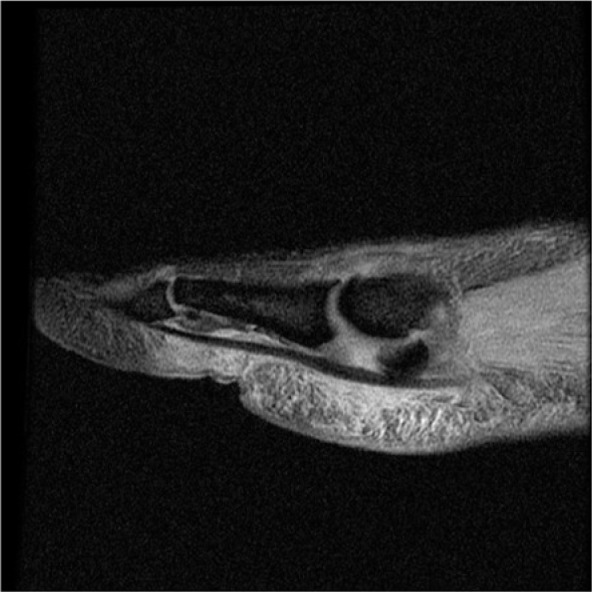
First metatarsophalangeal (hallux MP) joint degenerative changes and plantar plate injury.
Case 4
A 22-year-old redshirt senior (height, 185 cm; weight, 138 kg) defensive lineman sustained an injury to his right great toe during summer football conditioning drills when he slipped while applying plantar pressure on his toe. He felt immediate pain and was unable to continue. Lachman test results were positive. MRI revealed irregularity, soft tissue edema, and bony fragments around the medial sesamoid consistent with a plantar plate injury and avulsion (Figure 10). One week postinjury, surgery was performed to address complete disruption of the plantar plate and avulsion off the proximal phalanx on the medial aspect of the sesamoid complex/plantar plate and 2 small (1-2 mm) osteochondral defects on the metatarsal head. Surgery procedures included repair of the right plantar plate complex as well as partial excision of the proximal phalanx of the hallux MP and proximal phalanx into the first toe at the site of the bony avulsion. Rehabilitation began the day after surgery and progressed according to protocol (Table 2), with the initial goal of returning to fall football activities. He was cleared for full participation in football activities 10 weeks postsurgery, which corresponded to week 1 of the fall season. He progressed and participated in practices and games while wearing an orthotic and a shank in his football cleat. He reaggravated the injury in week 5 when his foot was landed on during practice. He was withheld from contact activities over the next 2 weeks, progressing as symptoms allowed. He was cleared to resume contact activities at 6 weeks following the recurrent injury because of improvement in symptoms and function during his rehabilitation. He participated in all practices and games throughout the remainder of the season.
Figure 10.
Injury to medial sesamoid in the plantar plate.
Case 5
An 18-year-old freshman (height, 198 cm; weight, 125 kg) offensive lineman sustained a left plantar plate injury during practice in week 4 of the fall season when a teammate fell on the athlete’s heel as he was falling forward. He had immediate pain and swelling, and was unable to continue. Lachman test results were positive. MRI taken 2 days postinjury confirmed plantar plate disruption, with proximal migration of the medial sesamoid and tear of the intersesamoidal ligament (Figure 11). Surgery (10 days postinjury) resulted in the athlete missing the remainder of the football season. Surgical procedures included repair of the abductor tendon, plantar plate at site of avulsion from the distal pole of the medial sesamoid, and the intersesamoidal ligament. He remained nonweightbearing for 2 weeks postsurgery before progressing toward a toe spacer and CAM boot. Additional precautions in rehabilitation included hallux MP joint flexion and extension no greater than 20° and 5°, respectively, because of the repair of both the plantar plate and intersesamoidal ligament. Follow-up radiographs (7 weeks postsurgery) demonstrated appropriate anatomic positioning of the medial sesamoid (Figure 12). He began full weightbearing (week 8) using a customized shank and orthotic placed in his left shoe. He progressed well through rehabilitation (Table 2), and initiated jogging, dynamic balance activities, and agility drills 12 weeks postsurgery. After completion of the rehabilitation protocol, he returned to full activity the next season.
Figure 11.
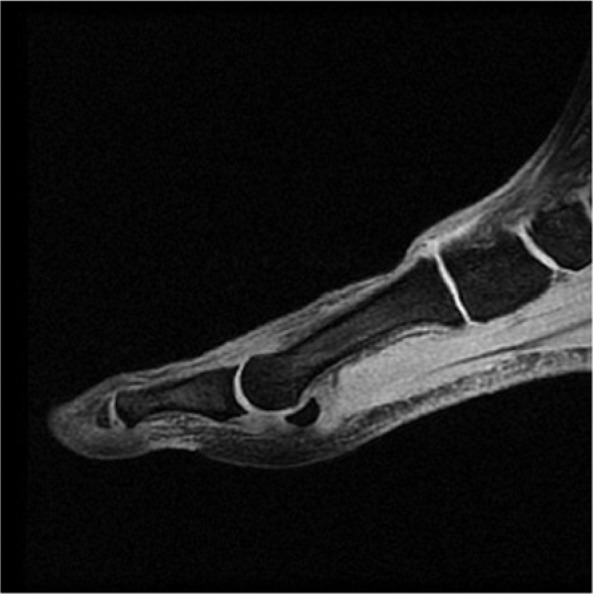
Proximal migration of medial sesamoid and classic “tipped tea cup” sign indicative of complete plantar plate disruption.
Figure 12.

Postoperative radiograph indicating appropriate anatomic positioning of the medial sesamoid.
Discussion
The anatomic structures within the hallux MP joint play an important role in stabilization of the joint during weightbearing and pushoff. The plantar plate connects the proximal phalanx to the metatarsal head and provides dorsal-plantar stability by controlling dorsiflexion motion of the hallux MP and interphalangeal joints (Figure 1). The insertion of the plantar plate at the proximal phalanx is overlapped by the insertion of the flexor hallucis brevis. Embedded within this tendon are the sesamoids, which are stabilized by the intersesamoidal ligament. The sesamoids transmit as much as 50% body weight and extreme loads (>300%) during pushoff.12 Being positioned within the flexor hallucis brevis tendon, they play an important role in powering flexion motion by increasing the mechanical advantage of the hallux MP joint.15 Further, they protect the flexor hallucis longus tendon by cushioning the hallux MP joint and dispersing the impact on the metatarsal head.10 Given their positioning of the sesamoids and their importance in distributing impact loads affecting the lower extremity, injury to the sesamoids and the associated ligamentous structures can significantly affect gait and function.
Diagnosis of plantar plate injury can be difficult given a similar mechanism of injury seen in turf toe.14 Variance to the typical hyperextension mechanism on a fixed foot may include varus and valgus forces or a force on the back of the heel that causes the great toe to hyperextend. These other mechanisms can lead to multistructural injury involving the flexor hallucis brevis, sesamoids, intersesamoidal ligament, and plantar plate.14 In isolated turf toe injuries, pain is typically distal to the sesamoids, but this pain pattern cannot reliably distinguish between a turf toe or a plantar plate injury when multiple structures are involved.
Determination of surgical and nonsurgical intervention for hallux MP joint injuries depends on the severity of the injury. The Lachman test of the great toe is a key clinical examination to determine the stability or instability of the plantar plate. Grading of the injury can then be determined based on Lachman test results and physical presentation of the injury. Grade 1 and 2 injuries, usually accompanied by swelling, decreased ROM, and partial tearing of the ligamentous structures, indicated by slight ligament laxity and mild pain, can be treated nonsurgically with gradual progression toward weightbearing activities and normalized gait.3 Generally, this injury is clinically stable based on hallux MP Lachman testing relative to the contralateral side.3 Return to play for these injuries can vary from 2 to 6 weeks depending on rehabilitation progression and sport demands. Grade 3 injuries, accompanied by significant pain, swelling, metatarsophalangeal instability, and complete disruption of the plantar plate structures, can be managed conservatively with long-term immobilization. Surgery is usually required if there is no resolution of symptoms or improvement in function.3 Additional surgical indications include traumatic hallux valgus deformity, vertical instability (with positive hallux MP Lachman test), large capsular avulsion with an unstable joint, sesamoid retraction, or fracture.3 Surgical intervention would repair damaged structures of the plantar plate and the associated flexor tendons as well as excision of bony fragments that cannot be reattached because of complete avulsion. Waldrop et al18 established a quantitative grading scale when evaluating radiographs of turf toe injuries when comparing changes of movement in the sesamoids on stress view compared with an intact state. A 3-mm increase in distance from the sesamoids to the proximal phalanx was predictive of a severe injury to the plantar plate (Figure 13).18 History, physical examination, imaging, and collection of quantitative data may provide the best algorithm for determining surgical and nonsurgical cases. Rehabilitation should focus on restoring joint range of motion, muscle strength, neuromuscular coordination, and gait mechanics.6
Figure 13.
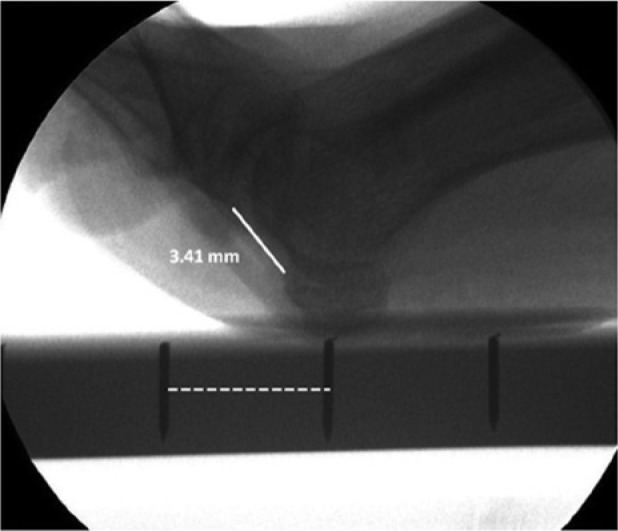
Fluoroscopic measurement of plantar plate ligaments under manual stress. Reprinted with permission from Waldrop et al.18
Summary
Injuries to the hallux MP joint can be complex, involving multiple structures. A thorough evaluation is necessary to identify the need for either conservative or surgical intervention, which varies depending on the severity of injury and the structures involved. Level of function, footwear, playing surface, and use of customized support should all be considered when returning the athlete to sport.
Acknowledgments
The authors would like to acknowledge the contributions of Donald T. Kirkendall, PhD, ELS, in editing this article.
Footnotes
The following authors declared potential conflicts of interest: Claude T. Moorman III, MD, is a consultant for Smith & Nephew and has stock/stock options with HealthSport; Mark E. Easley, MD, is a board member of the American Orthopaedic Foot & Ankle Society and is a consultant for Exactech, Tornier, and DT MedSurg.
References
- 1. Albers D, Agnone M, Isear J. Rehabilitation and taping techniques in the athlete: hallux and first ray problems. Tech Foot Ankle Surg. 2003;2:67-72 [Google Scholar]
- 2. Anderson R. Turf toe injuries of the hallux metatarsophalangeal joint. Tech Foot Ankle Surg. 2002;1:102-111 [Google Scholar]
- 3. Anderson R, Shawen S. Great toe disorders. In: Porter DA, Schon LC, eds. Baxter’s The Foot and Ankle in Sport. Philadelphia, PA: Elsevier Health Science; 2007:411-433 [Google Scholar]
- 4. Bowers KD, Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8:81-83 [PubMed] [Google Scholar]
- 5. Brophy RH, Gamradt SC, Ellis SJ, et al. Effect of turf toe on foot contact pressures in professional American football players. Foot Ankle Int. 2009;30:405-409 [DOI] [PubMed] [Google Scholar]
- 6. Chinn L, Hertel J. Rehabilitation of ankle and foot injuries in athletes. Clin Sports Med. 2010;29:157-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clanton TO, Butler JE, Eggert A. Injuries to the metatarsophalangeal joints in athletes. Foot Ankle. 1986;7:162-176 [DOI] [PubMed] [Google Scholar]
- 8. Clanton TO, Ford JJ. Turf toe injury. Clin Sports Med. 1994;13:731-741 [PubMed] [Google Scholar]
- 9. Coker TP, Arnold JA, Weber DL. Traumatic lesions of the metatarsophalangeal joint of the great toe in athletes. Am J Sports Med. 1978;6:326-334 [DOI] [PubMed] [Google Scholar]
- 10. Dedmond BT, Cory JW, McBryde A., Jr. The hallucal sesamoid complex. J Am Acad Orthop Surg. 2006;14:745-753 [DOI] [PubMed] [Google Scholar]
- 11. Fahey TD. Athletic Training: Principles and Practice. Palo Alto, CA: Mayfield; 1986 [Google Scholar]
- 12. Maglaya CL, Cook C, Zarzour H, Moorman CT. Return to division 1A football following a 1st metatarsophalangeal joint dorsal dislocation. N Am J Sports Phys Ther. 2010;5:131-142 [PMC free article] [PubMed] [Google Scholar]
- 13. McBryde AM, Jr, Anderson RB. Sesamoid foot problems in the athlete. Clin Sports Med. 1988;7:51-60 [PubMed] [Google Scholar]
- 14. McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin. 2009;14:135-150 [DOI] [PubMed] [Google Scholar]
- 15. McCormick JJ, Anderson RB. Rehabilitation following turf toe injury and plantar plate repair. Clin Sports Med. 2010;29:313-323 [DOI] [PubMed] [Google Scholar]
- 16. Richardson EG. Injuries to the hallucal sesamoids in the athlete. Foot Ankle. 1987;7:229-244 [DOI] [PubMed] [Google Scholar]
- 17. Rodeo SA, O’Brien S, Warren RF, Barnes R, Wickiewicz TL, Dillingham MF. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med. 1990;18:280-285 [DOI] [PubMed] [Google Scholar]
- 18. Waldrop NE, 3rd, Zirker CA, Wijdicks CA, LaPrade RF, Clanton TO. Radiographic evaluation of plantar plate injury: an in vitro biomechanical study. Foot Ankle Int. 2013;34:403-408 [DOI] [PubMed] [Google Scholar]


