Abstract
Background:
Relatively few patients have dual-energy x-ray absorptiometry to quantify the magnitude of bone loss as they age. Recent work correlates mean computed tomography (CT) attenuation in the level I (L1) vertebra with bone mineral density (BMD), making it possible to objectively evaluate the magnitude of bone loss in osteoporosis by this method. The aims of this study were to evaluate the utility of using CT scans in patients with acute thoracic and lumbar spine fractures to diagnose osteoporosis and using CT attenuation to evaluate the association between age and BMD.
Methods:
We performed a retrospective study of patients with acute fractures of the thoracic or lumbar spine who had also undergone an abdominal (or L1) CT scan and compared mean CT attenuation in L1 against threshold values. We also compared differences in CT attenuation between younger (<65 years) and older (≥65 years) and older patients.
Results:
A total of 124 patients were evaluated (74 thoracic and 50 lumbar fractures). Overall, there was a strong correlation between age and bone density as measured by CT attenuation (r = −.76). Among those with thoracic fractures (<65 years), mean CT attenuation was 196.51 HU. Forty-one patients were ≥65 years and had mean CT attenuation of 105.90 HU (P < .001). In patients with lumbar fractures, 27 patients were <65 years and had a mean CT attenuation of 192.26 HU and 23 patients were ≥65 years and had mean CT attenuation of 114.31 HU (P < .001). At the threshold of 110 HU, set for specificity, the magnitude of difference between the age-stratified cohorts was greater in the thoracic spine (P < .0001 vs P = .003).
Discussion:
Using opportunistic CT, we demonstrate the relative frequency of osteoporosis in patients with acute fractures of the thoracic and lumbar spine and confirm that the association increases with age. The CT attenuation may provide a cheap and convenient method to help confirm a clinical diagnosis of osteoporosis in patients with fractures.
Keywords: osteoporosis, fracture, spine, bone mineral density, BMD, CT attenuation
Background
Patients aged 65 years and older are rapidly increasing as a proportion of the overall US population. Current projections indicate that each year, 3.5 million people turn 65, and at the current rate, that 20% of the US population will be aged older 65 by 2020.1 Specific changes in the spine are associated with aging. One well-recognized change is a progressive reduction in bone mineral density (BMD); this reduction in BMD results in an increased susceptibility to fractures both in the axial and in the appendicular skeleton.2 Given the weight-bearing function of the thoracic and lumbar spines, impairment in the quality of the bone can lead to compression fractures. These fractures, like osteoporosis in general, occur with increased frequency in women.3
The spine contains the greatest volume of metabolically active trabecular bone in the body.4 The loss of these same trabeculations is one of the defining features of osteoporosis.5 The process by which osteoporosis develops is associated with the preferential loss of horizontal trabeculae, the impact of which is a reduction in the ability of vertebrae to withstand compressive, axial forces. This declination of bone structure leads to vertebral compression fractures, most of which occur in the thoracic and thoracolumbar spine.4 These fractures, which can cause a painful and disabling kyphosis, also have a strong risk of occurring at multiple levels. Additionally, they are a strong predictor of future fractures.6
In patients who have sustained fractures thought to be secondary to an underlying reduction in BMD, dual-energy x-ray absorptiometry (DXA) scanning is indicated to elucidate and quantify BMD. The US Preventive Services Task Force7 recommend that all women older than 65 years of age and all men older than 70 years of age should be tested for osteoporosis, with the caveat that both men and women below 65 years should be tested for osteoporosis in the presence of an appropriate risk profile, such as those with fragility fractures. In spite of these recommendations, less than one-third of older women in the United States and one-twentieth of older men have had a BMD test.8 Even after low-velocity trauma, only 10% to 20% of older patients are tested for osteoporosis.9
The advent of an analysis that accurately correlates bone density obtained from computed tomography (CT) attenuation (using scans of the abdomen ordered for a variety of reasons unrelated to the patients’ bone density) with a diagnosis of osteoporosis10 offers the unique opportunity to rapidly quantify BMD in patients. This approach may potentially avoid the need for DXA scans, reduce radiation exposure, and save costs in patients who have already had an abdominal (or lumbar) CT scan performed for reasons other than measuring their BMD. Previous attempts at correlating BMD obtained from CT scans with DXA scans11 have been in relatively small samples, have lacked numerical thresholds to aid definitive diagnosis, have been equivocal about the role of lumbar vertebral level, and finally have included measurements of the cortical bone, which can be a source of overestimates in BMD.12 As osteoporosis is a relatively silent disease early on, and as abdominal CT scans are commonly performed in older patients8 for a variety of other reasons, opportunistic evaluation of BMD offers the opportunity to correlate CT attenuation, BMD, and osteoporosis in acute fractures of the spine. The aims of this study were to thus evaluate the utility of using CT scans in patients with acute thoracic and lumbar spine fractures to diagnose osteoporosis and using CT attenuation to evaluate the association between age and BMD.
Patients and Methods
Following institutional review board approval, we reviewed the cases of patient who presented to a level I (LI) trauma center between June 2010 and December 2012. Patients were included in the review if they were adults (≥18 years old) with an acute presentation for a fracture in either their thoracic spine or their lumbar spine (except L1). In addition, patients must have had a CT scan of their abdomen in either the 6 months preceding their acute presentation or the 6 months following their acute presentation. Patients were excluded if they were minors, if they had a fracture through the L1 vertebra, or if they had a CT scan that was performed outside of the prescribed period of time.
Images were acquired on General Electric scanners (VCT 64 slice or LightSpeed 16 slice; GE Healthcare, Waukesha, WI). The CT scanners that were used for acquiring images were calibrated daily during the period of time in which all initial images were taken.
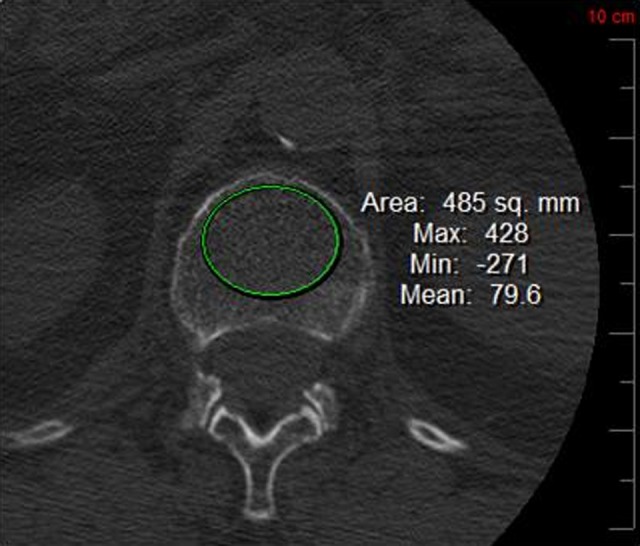
Using a picture archiving and communications system, regions of interest were selected. The method was identical to that used by Pickhardt et al.10 The L1 vertebra was identified in the axial plane and viewed in bone and soft tissue windows. The largest elliptical area over the body of L1 that could be selected, without including the cortex, was chosen. Although not excluded, we also ensured that specific areas with hardware present were avoided, as were areas of focal heterogeneity, and the posterior venous complex. For each patient, mean CT attenuation in HU was measured.10 Additional values obtained include maximum and minimum CT attenuation (HU; Figures 1 and 2).
Figure 1.

Nonosteoporotic region of interest.
Figure 2.
Osteoporotic region of interest.
Bone mineral density was evaluated by comparing values for CT attenuation in HU with previously published thresholds.10 The thresholds were evaluated as follows: (1) ≤110 HU or >110 HU, which was selected to achieve approximately 90% specificity in differentiating osteoporosis from nonosteoporosis, (2) ≤135 HU or >135 HU, which was selected to achieve a balanced specificity and sensitivity in differentiating between osteoporosis and nonosteoporosis, and (3) ≤160 HU or >160 HU, which was selected to achieve a sensitivity of around 90% sensitivity in differentiating osteoporosis from nonosteoporosis and to achieve a balanced sensitivity and specificity in differentiating normal from low BMD (Figure 3).
Figure 3.
Flow diagram for patients with acute fractures of the thoracic and lumbar spine fractures.
Statistics
The coefficient of correlation (r) was derived using Microsoft Excel (Microsoft, Redmond, Washington). The patient cohort was stratified by aged into 2 groups (<65 and ≥65 years). The mean CT attenuation in HU was compared using a Student t-test. For each threshold value, the proportion of each age stratified group above or below the threshold was compared using a Fisher exact test.
Results
A total of 204 patients were screened, with those aged <65 years accounting for 106 fractures and those ≥65 years accounting for 98 fractures. In the younger cohort, the majority of fractures were caused by motor vehicle collisions (MVCs) and falls from height, 40 and 31 patients, respectively, while in the older cohort, falls from standing height or less accounted for most injuries (49 patients).
Of those screened, 124 were included in the study. In all, 74 had thoracic spine fractures, and 50 patients had lumbar spine fractures.
There was a correlation between age and BMD, with a progressive reduction in CT attenuation (HU) as age increased (r = −.76; Figure 4).
Figure 4.
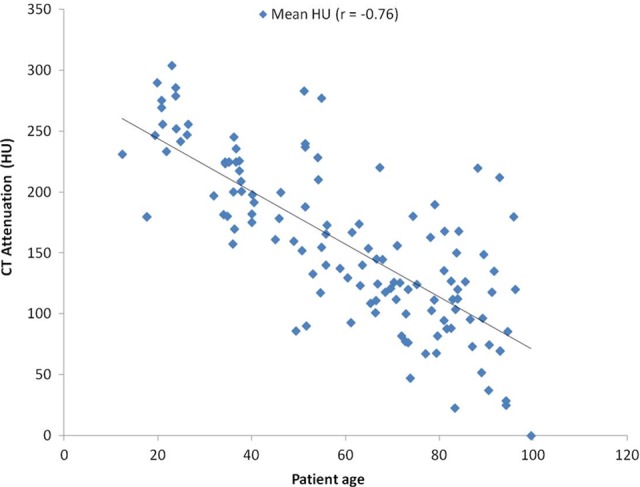
Bone mineral density as a function of age as measured using computed tomography (CT) attenuation.
In patients with thoracic spine fractures, 33 were younger than 65 years while 41 were aged 65 years and older. Mean value for CT attenuation in the younger cohort with thoracic fractures was 196.51 HU, compared with a value of 105.90 HU in patients aged 65 years and older (P < .0001; Table 1).
Table 1.
Comparison of CT Attenuation in the Thoracic Spine for Patients Aged <65 Years Versus Patients Aged ≥65 Years.
| Thoracic Spine | <65 Years | ≥65 Years | P Value |
|---|---|---|---|
| n | 33 | 41 | |
| Mean HU | 196.51 | 105.90 | 9.3 × 1013 |
| SD of mean HU | 48.87 | 45.10 | |
| HU ≤ 110 | 4 | 22 | .0002 |
| HU > 110 | 29 | 19 | |
| HU ≤ 135 | 7 | 33 | 4.14 × 10−7 |
| HU > 135 | 26 | 8 | |
| HU ≤160 | 7 | 35 | 2.43 × 10−8 |
| HU > 160 | 26 | 6 |
Abbreviations: CT, computed tomography; SD, standard deviation.
In the patients with thoracic spine fractures, 9 opportunistic screening CTs were primary abdominal CT scans, while 65 were derived from CT scans of the spine. In the patients with lumbar spine fractures, 2 opportunistic screening CTs were primary abdominal CT scans, while 48 were derived from CT scans of the spine (Table 1).
Using the threshold of 110 HU, 4 (12%) of the 33 patients were osteoporotic. Approximately half of the patients aged 65 years and older were osteoporotic, 22 (54%) of the 41. With approximately 90% specificity, 54% of patients aged 65 years or older were osteoporotic while 12% of patients younger than 65 years were osteoporotic (P < .0001; Table 1).
Using the threshold of 135 HU, 7 (21%) of the 33 patients aged less than 65 years were osteoporotic, and 33 (80%) of the 41 patients aged 65 years and older were osteoporotic. With balanced for specificity and sensitivity, 21% of patients aged below 65 years of age and 80% of patients aged 65 years and older were osteoporotic (P < .0001).
Using the threshold of 160 HU, 7 (21%) of the 33 patients aged less than 65 years were osteoporotic and 35 (85%) of the 41 patients aged 65 years and over were osteoporotic. With approximately 90% sensitivity, 21% of patients aged below 65 years of age and 85% of patients aged 65 years and older were osteoporotic (P < .0001; Table 1).
Fifty patients with lumbar spine fractures were evaluated, and of these, 27 were aged less than 65 years while 23 were aged 65 years and older. In the younger cohort, the mean value for CT attenuation was 192.26 HU, whereas the mean value for the older cohort of patients was 114.31 HU. The difference between these mean values for CT attenuation was significant, with P < .0001 (Table 2).
Table 2.
Comparison of CT Attenuation in the Lumbar Spine for Patients Aged <65 Years versus Patients Aged ≥65 Years.
| Lumbar Spine | <65 Years | ≥65 Years | P Value |
|---|---|---|---|
| n | 27 | 23 | |
| Mean HU | 192.26 | 114.31 | 2.6 × 10−6 |
| SD of mean HU | 54.62 | 46.87 | |
| HU ≤ 110 | 2 | 10 | .006 |
| HU > 110 | 25 | 13 | |
| HU ≤ 135 | 4 | 16 | .0001 |
| HU > 135 | 23 | 7 | |
| HU ≤ 160 | 9 | 20 | .00016 |
| HU > 160 | 18 | 3 |
Abbreviations: CT, computed tomography; SD, standard deviation.
Using the 110 HU threshold, 2 (7%) of the 27 patients aged younger than 65 years were osteoporotic and 10 (43%) of the 23 patients aged 65 years and older were above osteoporotic. With approximately 90% specificity, 7% of those aged younger than 65 years were osteoporotic while 43% of those aged 65 years and older were osteoporotic (P = .006; Table 2).
Using the 135 HU threshold, 4 (15%) of the 27 patients aged younger than 65 years were above this threshold, whereas 16 (70%) of the 23 patients aged 65 years and older were osteoporotic. With balanced sensitivity and specificity, 15% of those aged younger than 65 years were osteoporotic while 70% of those aged 65 years and older were osteoporotic (P = .0001; Table 2).
Using the 160 HU threshold, 9 (33%) of the 27 patients aged younger than 65 years were osteoporotic, and 20 (87%) of the 23 patients aged 65 years and older were osteoporotic. With approximately 90% sensitivity, 33% of those aged younger than 65 years were osteoporotic while 87% of those aged 65 years and older were osteoporotic (P = .00016).
With the balanced threshold for differentiating normal BMD from low BMD (160 HU), 87% and 33% of the older and younger cohort, respectively, had low BMD.
Discussion
Although aging is known to be associated with reduced BMD, which can predispose to spine fractures, this is the first study that uses CT attenuation to outline the frequency with which BMD is reduced in a cohort of patients presenting specifically with acute fractures of the spine. As the majority of patients who should get DXA scanning do not actually do so,8 the use of CT attenuation thus provides a simple, accessible, and potentially cost-effective way of broadening access to BMD measurement in populations at risk of fractures.
Our data support the view that age-related bone loss may be implicated in a significant proportion of the fractures in patients aged 65 years and older, who present with acute spine fractures. Although DXA scans are relatively cheap and accessible, comparatively few patients who, based on guidelines, should have them done actually have DXA performed.8 The use of CT attenuation in opportunistic scans of the abdomen (ie, scan ordered for other reasons) to generate estimates of BMD at no extra cost and with a negligible investment of time may greatly help this group of patients in the context of spine fractures. If a fracture is found to be associated with osteoporosis, appropriate management could be initiated, possibly reducing the likelihood of any kind of fracture in the future. This is particularly pertinent because the best predictor of a fragility fracture is a previous fracture.6
It should be noted that opportunistic screening is not sufficiently developed to be used in the prediction of future fracture risk, in the same way as is, for example, the WHO FRAX Score. However, given the sensitivity and specificity of this new and simple technique, it may serve as a rapid assessment tool. As an initial mechanism, in the presence of a suspicion of low BMD or clinical suspicion of osteoporosis, it could trigger a formal bone health evaluation. The recent literature suggests that the use of DXA scans may actually be declining. This has been attributed to various reasons, one of which is related to unfavorable reimbursement rates.13 Given the ongoing changes in the funding of health care, and the ubiquitous presence of tight budgets, this approach may help deliver the aims of improved bone health, without the added considerations of cost. The addition of opportunistic CT screening may further help the improvement in bone health among populations at risk.
Although the presence of a fragility fracture should raise the suspicion of underlying osteoporosis, which should then lead to a thorough evaluation of the patient’s bone health, as advocated by the American Orthopaedic Association’s “Own the bone” initiative,14 evidence suggests many patients may not be having their BMD tested subsequent to these falls. The cohort in this study comprises the full age spectrum of adults, with younger patients generally sustaining fractures from high-velocity mechanisms such as MVCs and falls from height, while older patients sustained fractures from low-velocity mechanisms, which mainly involved falls from standing height or lower. It should be noted that although CT attenuation may offer a degree of diagnostic accuracy that may not have been previously available, it is not a panacea and should not be used as a primary method for evaluating BMD; when CT images are already available, however, it is a powerful tool.
Bony changes associated with aging and degeneration4 are such that the use of DXA can actually overestimate BMD.15 This anomaly highlights one of the potential benefits of the CT attenuation-based approach as an over estimation of BMD may reduce the accuracy of DXA in older patients. In fact, previous work actually suggests that patient classified as being nonosteoporotic go on to sustain osteoporotic fractures.16,17 These patients may have been more accurately evaluated if their L1CT attenuation was evaluated, assuming the availability of these images. In Pickhardt et al,10 of the patients with vertebral fractures, 52% were found to be osteoporotic using DXA scanning,10 whereas 97% had low BMD as measured by CT attenuation.8 Given these issues with DXA, it might be important to use another measurement of BMD.
Bone mineral density measurements at L1 were found to be more accurate than other levels of the spine.10 As L1 is recognized with relative ease and is present in CT scans of the chest and abdomen, nonspecialists could potentially use this technique with minimal additional training requirement.
The use of CT attenuation should be differentiated from quantitative CT (QCT) measurement of bone density. The latter generates T scores that do not completely correspond with DXA scores, which means that their clinical use, to date, has been relatively limited.18 In addition, the use of CT attenuation is demonstrably more effective that QCT in the spine in terms of the quality and predictive value of the results.10,19 A greater amount of time and technical expertise is required to generate BMD values using QCT, compared to CT attenuation.
Osteoporosis is a significant consideration in the fixation of spine fractures; previous work has demonstrated that insertional torque for pedicle screws is positively correlated with BMD.20 The impact of this is the possibility that reduced torque is associated with less secure fixation—a clearly undesirable prospect. Screw loosening may cause loss of correction and nonunions. There is also the suggestion that screw loosening may be associated with adjacent segment compression fractures proximal to the fixed segment.
Once this technique is better established and more developed, future work could evaluate or model the fracture risk reduction, at a population level, of patients who have their BMD evaluated opportunistically. Potential directions for other future work would be to use this technique in helping confirm a clinical suspicion of osteoporosis in patients with fractures at other anatomical sites, such as the hip and distal radius.
There are limitations to this study. It is a retrospective evaluation. Also, the use of CT attenuation in the prediction of fracture risk is not currently possible as it is based exclusively on the values derived from attenuation at the level of L1.21 As previously mentioned, the process of aging and degeneration can cause changes that limit the accuracy of DXA, so the accuracy of DXA scales are, themselves, limited.
Overall, the use of CT attenuation to help in the assessment of osteoporosis in patients who may have sustained fractures of their thoracic and lumbar spine may provide an accessible and cost-efficient method for improving patient care in this group of patients.
Acknowledgment
The authors thank Mary Van Beusekom, ELS (HealthPartners) for editing this manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Taylor JA, Bussières A. Diagnostic imaging for spinal disorders in the elderly: a narrative review. Chiropr Man Therap. 2012;20(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Melton LJ III. Epidemiology of spinal osteoporosis. Spine (Phila Pa 1976). 1997;22(24 suppl): 2S–11S [DOI] [PubMed] [Google Scholar]
- 3. Lane JM, Russell L, Khan SN. Osteoporosis. Clin Orthop Relat Res. 2000;(372):139–150 [DOI] [PubMed] [Google Scholar]
- 4. Jeong GK, Bendo JA. Spinal disorders in the elderly. Clin Orthop Relat Res. 2004;(425):110–125 [DOI] [PubMed] [Google Scholar]
- 5. Myers ER, Wilson SE. Biomechanics of osteoporosis and vertebral fracture. Spine (Phila Pa 1976). 1997;22(24 suppl):25S–31S [DOI] [PubMed] [Google Scholar]
- 6. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA III, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15(4):721–739 [DOI] [PubMed] [Google Scholar]
- 7. U.S. Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154(5):356–364 [DOI] [PubMed] [Google Scholar]
- 8. Majumdar SR, Leslie WD. Conventional computed tomography imaging and bone mineral density: opportunistic screening or “incidentaloporosis”? Ann Intern Med. 2013;158(8):630–631 [DOI] [PubMed] [Google Scholar]
- 9. Majumdar SR, McAlister FA, Johnson JA, et al. Interventions to increase osteoporosis treatment in patients with ‘incidentally’ detected vertebral fractures. Am J Med. 2012;125(9):929–936 [DOI] [PubMed] [Google Scholar]
- 10. Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158(8):588–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tay WL, Chui CK, Ong SH, Ng AC. Osteoporosis screening using areal bone mineral density estimation from diagnostic CT images. Acad Radiol. 2012;19(10):1273–1282 [DOI] [PubMed] [Google Scholar]
- 12. Klingberg E, Lorentzon M, Mellström D, et al. Osteoporosis in ankylosing spondylitis—prevalence, risk factors and methods of assessment. Arthritis Res Ther. 2012;14(3):R108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. King AB, Fiorentino DM. Medicare payment cuts for osteoporosis testing reduced use despite tests' benefit in reducing fractures. Health Aff (Millwood). 2011;30(12):2362–2370 [DOI] [PubMed] [Google Scholar]
- 14. Tosi LL, Gliklich R, Kannan K, Koval KJ. The American Orthopaedic Association's “own the bone” initiative to prevent secondary fractures. J Bone Joint Surg Am. 2008;90(1):163–173 [DOI] [PubMed] [Google Scholar]
- 15. Yu W, Glüer CC, Fuerst T, Grampp S, Li J, Lu Y, Genant HK. Influence of degenerative joint disease on spinal bone mineral measurements in postmenopausal women. Calcif Tissue Int. 1995;57(3):169–174 [DOI] [PubMed] [Google Scholar]
- 16. Siris ES, Brenneman SK, Barrett-Connor E, et al. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the national osteoporosis risk assessment (NORA). Osteoporos Int. 2006;17(4):565–574 [DOI] [PubMed] [Google Scholar]
- 17. Schuit SC, van der Klift M, Weel AE, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone. 2004;34(1):195–202 [DOI] [PubMed] [Google Scholar]
- 18. Engelke K, Adams JE, Armbrecht G, et al. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom. 2008;11(1):123–162 [DOI] [PubMed] [Google Scholar]
- 19. Pickhardt PJ, Lee LJ, del Rio AM, et al. Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res. 2011;26(9):2194–2203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine (Phila Pa 1976). 2000;25(7):858–864 [DOI] [PubMed] [Google Scholar]
- 21. Kanis JA, McCloskey EV, Johansson H, Oden A, Ström O, Borgström F. Development and use of FRAX in osteoporosis. Osteoporos Int. 2010;21 suppl 2:S407–S413 [DOI] [PubMed] [Google Scholar]



