Abstract
Purpose:
This study aimed to compare the differences in functional recovery between patients undergoing plate and nail fixation in the very early period after surgery.
Method:
This study was designed as a controlled clinical trial that included 18 patients who were surgically treated with either dynamic hip screw as plate fixation or proximal femoral nail as nail fixation for stable intertrochanteric fractures. In particular, all patients selected for the study reported walking completely independently without the use of walking aids prior to sustaining their initial fracture. In all, 8 patients (mean age, 73.8 years; range, 65-89 years) were treated with plate fixation (group plate) and 10 patients (mean age, 79.7 years; range, 70-90 years) were treated with nail fixation (group nail). Functional evaluations were assessed every week after surgery using the Japanese Orthopaedic Association (JOA) hip functional scores and active range of motion (ROM) of the hip joint.
Results:
The recovery of activities of daily living (ADLs) according to JOA hip functional scores at week 4 after surgery was significantly better in group nail than in group plate (P = .03), whereas active ROM of hip flexion improved significantly in group plate than in group nail at weeks 3 and 4 after surgery (P = .04 and P = .02, respectively).
Conclusions:
The results suggested that nail fixation may provide a more rapid recovery of ADLs than that of plate fixation in the very early period after surgery. However, plate fixation may provide better ROM of hip flexion than that of nail fixation.
Keywords: early functional recovery, dynamic hip screw, proximal femoral nail, stable intertrochanteric fractures
Introduction
Early functional recovery is extremely important for elderly patients with femoral intertrochanteric fractures to shorten their hospital stay, omit the necessity of further nursing and care services, and reduce associated medical expenditures. This is particularly true in Japan, which is one of the countries with most aged society in the world. The 2 types of implants used for treating intertrochanteric fractures include a plate type and a nail type. No prior comparative studies have evaluated early functional recovery (ie, within the first month) of patients after fixation with either device.
Recent studies comparing these 2 devices have been published, focusing on technique, surgical invasiveness, clinical recovery, and complications; however, which fixation method is superior remains controversial.1–9 These prior studies have included patients with various types of fractures (stable and unstable) and variable characteristics in terms of preinjury physical fitness, intelligence, and psychological status. Therefore, the inclusion of patients with variable characteristics could influence the results of a study involving clinical recovery.
Furthermore, the type of fracture (stable vs unstable) has been reported to affect mobility until complete bony union is achieved.10,11 In addition, the patient’s preinjury physical fitness level, locomotive ability, mental status, and intelligence are all characteristics that can influence postoperative rehabilitation. To accurately compare the difference in clinical outcomes between these 2 fixation methods, in this study, we attempted to eliminate as much variability as possible among patients selected for this study.
We hypothesized that surgical invasiveness associated with each fixation method may independently influence functional recovery at a very early stage after surgery. The purpose of this study was to demonstrate which of the 2 types of implants improved locomotive ability, including the ability to stand and walk independently, at the very early stage.
Patients and Methods
Patients and Inclusion Criteria
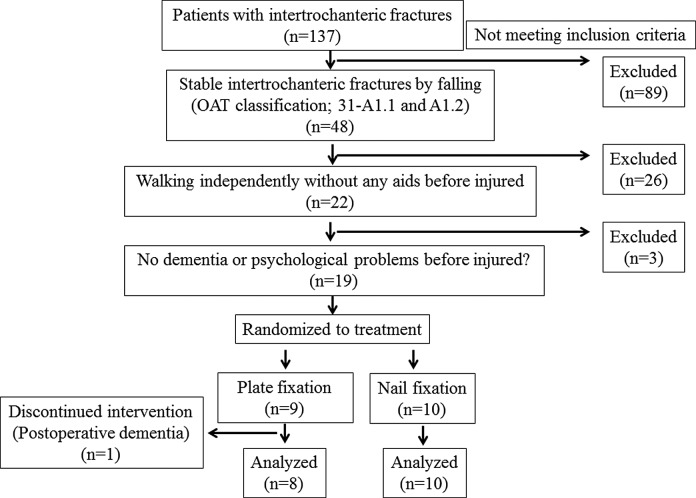
The inclusion criteria for this study are shown in Figure 1. This was a controlled clinical trial of 18 patients who were surgically treated for femoral intertrochanteric fractures in an alternating sequence by first nail fixation and then plate fixation by 2 orthopedic surgeons including the first author between 2009 and 2012. These patients had simple intertrochanteric fractures, 31-A1.1 and A1.2, that were diagnosed by the other 2 senior orthopedic surgeons using plain radiography according to the Orthopaedic Trauma Association (OTA) classification.12 All patients selected for this study reported walking independently without the use of walking aids such as walking frames or canes before sustaining their initial fracture (ie, they had equivalent activities of daily living [ADLs]). A total of 8 patients (6 women and 2 men; mean age, 73.8 years; range, 65-89 years) were treated with plate fixation (group plate) and 10 patients (6 women and 4 men; mean age, 79.7 years; range, 70-90 years) were treated with nail fixation (group nail). Informed consent to participate in this clinical study as well as for the surgical procedure was obtained from all patients before surgery. Simple fractures such as a femoral basal neck fracture, the minor trochanter as fracture fragment, and comminuted greater trochanteric fractures were excluded. Patients with pathological fractures, high-energy injuries, or other multiple injuries were excluded. Patients with apparent dementia or other psychological problems and severe perioperative or postoperative complications that would result in delayed postoperative rehabilitation (ie, bronchopneumonia, cardiac failure, urinary tract infection, or postoperative delirium) in the early period after surgery were also excluded (Figure 1).
Figure 1.
Inclusion and exclusion criteria of the study.
In reality, 1 patient who underwent plate fixation was excluded because of postoperative delirium and developing dementia that affected rehabilitation. No patients with severe perioperative or postoperative complications in the early period after surgery were observed.
Surgical Procedures and Rehabilitation
Manual closed reduction of the fracture was performed successfully using a traction device. As determined by intraoperative fluoroscopy, the ideal femoral neck–shaft angle was 130° and the ideal anteversion angle was 20°. Dynamic hip screw with 2 distal locking screws was used for plate fixation, while extra small proximal femoral nail with 1 distal screw was used for nail fixation. The angle of blade to plate and that of blade to nail were 130°.
The ideal position of the blade was just central to the femoral neck both in the lateral and in the anteroposterior fluoroscopic view. The tip of the blade was inserted at a distance of 5 mm up to subchondral bone of femoral head in the anteroposterior fluoroscopic view.
A physiotherapist supervised full weight-bearing and walking exercises that were performed on day 1 after surgery. Plain anteroposterior and lateral radiographs were also obtained for each patient to confirm complete union of the bone.
Evaluation of Factors Affecting Postoperative Locomotive Ability
Patient characteristics and surgical invasiveness
Body mass index, waiting period for surgery, time length of surgery, and intraoperative blood loss were evaluated for each patient. Postoperative blood loss was estimated in each patient by determining the decrease in blood hemoglobin from day 1 to week 1 after surgery.
Functional evaluation
The following factors affecting functional mobility were evaluated for the groups every week from weeks 1 to 4 by 3 physiotherapist.
Pain and ADLs scores according to the Japanese Orthopaedic Association (JOA) hip functional scores: Pain in each patient was assessed according to the pain criteria established by the JOA. Subjective pain assessment is shown in Table 1 and divided into 6 categories (total = 40 points).
Table 1.
Pain Scores (Points).
| 40 | No pain with ambulation |
| 35 | Walking without pain but with discomfort |
| 30 | Can walk without pain, but pain occurs when starting to walk or after long walks |
| 20 | No spontaneous pain or pain while walking and completely relieved by rest |
| 10 | Somewhat spontaneous or pain while walking that is partially relieved by rest |
| 0 | Continuous spontaneous pain through night |
Activities of daily living scores were assessed in each patient through subjective assessment and were divided into the following 2 categories (total = 40 points): walking ability (total = 20 points) and activity scores (total = 20 points; Table 2). Walking ability scores were divided into 6 levels. Activity scores included 5 actions and each action was evaluated using 3 levels.
Active range of motion (ROM), angle of hip flexion, and abduction: The active range of hip flexion was measured with patients lying on their backs and with their knees moderately bent. The active range of hip abduction was measured with patients lying on the side opposite the surgical leg.
Time to achieve active straight leg raising (SLR)13: Patients were also evaluated for their ability to achieve active SLR for more than 60 seconds in the supine position. Their heels were required to remain no less than 10 cm from the floor, and patients were timed to see how long they could maintain SLR. If patients could maintain SLR for more than 60 seconds, they passed the SLR test.
Time to achieve independent standing on the surgical leg13:Patients were evaluated based on their ability to stand on the surgical leg for more than 60 seconds. If patients could maintain this posture for more than 60 seconds, they passed this evaluation.
Table 2.
Walking Ability and Activity Scores (Points).
| Walking ability | |
| 20 | Able to walk without any complaints |
| 18 | Able to walk for long distances with light claudication |
| 15 | Able to walk continuously 30 minutes or 2 km without the use of walking aid or cane |
| 10 | Able to walk continuously for 15 minutes or 500 m without the use of a walking aid or cane |
| 5 | Able to walk on level surface with aid of a cane |
| 0 | Inability to walk because of pain |
| Activity | |
| Sitting | |
| 4 | Able to accomplish activity easily |
| 2 | Able to accomplish activity with use of hands |
| 0 | Inability to perform activity |
| Continuing to stand on both feet | |
| 4 | Over 30 minutes |
| 2 | >5 but <30 minutes |
| 0 | Less than 5 minutes |
| Crouching down and standing up | |
| 4 | Able to accomplish activity easily |
| 2 | Able to accomplish activity with use of hands |
| 0 | Inability to perform activity |
| Going up and down stairs | |
| 4 | Able to accomplish activity easily |
| 2 | Able to accomplish activity with use of hands |
| 0 | Inability to perform activity |
| Getting in and out of the car | |
| 4 | Able to accomplish activity easily |
| 2 | Able to accomplish activity with use of hands |
| 0 | Inability to perform activity |
| Total 20 points | |
Statistical Analysis
Statistical analysis was performed using SPSS software for Windows (SPSS Inc, Chicago, Illinois). The P values were calculated using nonparametric independent sample tests; the Mann-Whitney U test for 2 related samples and the Wilcoxon signed-rank test were used. P values <.05 were considered significant.
Results
Surgical Invasiveness
Operation time in group plate was significantly greater than that in group nail (P = .03). However, no difference in the postoperative decrease in hemoglobin was observed between day 1 (P = .89) and week 1 after surgery (P = .91). No patient received blood transfusion (Table 3).
Table 3.
Patient Characteristics and Surgical Invasiveness.a
| Group Plate | Group Nail | ||
|---|---|---|---|
| N = 8 | N = 10 | P value | |
| Age | 73.75; range 65-89 | 79.7; range 70-90 | .20 |
| Sex | |||
| Male | 2 | 4 | |
| Female | 6 | 6 | |
| BMI | 21.06 (SD 2.74) | 21.38 (SD 3.80) | .72 |
| Waiting period for surgery, day | 5.25 (SD 2.19) | 5.60 (SD 2.41) | .62 |
| Time length of surgery, minutes | 52.50 (SD 11.21) | 39.00 (SD 15.12) | .033b |
| Intraopretative blood loss, mL | 39.50 (SD 29.31) | 37.50 (SD 26.59) | .96 |
| Decrease in blood hemogrobin, g/dL | |||
| At day 1 after surgery | 1.64 (SD 1.38) | 1.64 (SD 0.93) | .89 |
| At week 1 after surgery | 2.15 (SD 1.07) | 2.04 (SD 0.99) | .91 |
Abbreviations: BMI, body mass index; SD, standard deviation.
a Values are mean.
b Statistically significant difference between the groups.
Functional Evaluation
Pain and ADL scores according to JOA hip functional scores
No significant differences in pain scores were observed in patients at any given week; however, a tendency for improvement in pain was observed in group nail at weeks 3 and 4 after surgery (P = .12, P = .16, respectively; Table 4).
Table 4.
Functional Evaluation.a
| The Week After Surgery | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Pain scores | ||||
| Group plate | 11.25 (SD 8.35) | 16.25 (SD 9.16) | 20.00 (SD 7.56) | 21.25 (SD 8.35) |
| Group nail | 13.00 (SD 8.23) | 20.00 (SD 8.16) | 25.50 (SD 5.99) | 26.50 (SD 5.80) |
| P value | .77 | .42 | .12 | .16 |
| ADL scores | ||||
| Group plate | 4.38 (SD 2.83) | 6.00 (SD 3.74) | 8.25 (SD 5.78) | 9.50 (SD 5.18) |
| Group nail | 7.10 (SD 4.36) | 10.70 (SD 4.97) | 13.90 (SD 7.34) | 16.30 (SD 6.85) |
| P value | .15 | .055 | .068 | b.027 |
| Hip flexion,° | ||||
| Group plate | 78.75 (SD 24.89) | 91.88 (SD 22.03) | 106.88 (SD 12.23) | 111.25 (SD 11.57) |
| Group nail | 78.00 (SD 11.35) | 90.00 (SD 4.71) | 94.50 (SD 7.25) | 96.50 (SD 9.73) |
| P value | .75 | .30 | b.036 | b.019 |
| Hip abduction, ° | ||||
| Group plate | 16.88 (SD 9.98) | 23.13 (SD 13.87) | 28.75 (SD 11.88) | 30.00 (SD 11.34) |
| Group nail | 20.00 (SD 8.50) | 23.50 (SD 8.18) | 25.00 (SD 6.67) | 26.00 (SD 6.58) |
| P value | .55 | .93 | .43 | .28 |
| SLR, seconds | ||||
| Group plate | 21.38 (SD 26.42) | 31.00 (SD 27.68) | 51.38 (SD 10.04) | 60.00 (SD 0.00) |
| Group nail | 15.70 (SD 20.61) | 35.60 (SD 23.85) | 46.90 (SD 19.21) | 50.60 (SD 16.85) |
| P value | .63 | .52 | .77 | .10 |
| Standing, seconds | ||||
| Group Plate | 6.88 (SD 12.80) | 12.13 (SD 22.84) | 16.25 (SD 22.80) | 22.86 (SD 28.26) |
| Group Nail | 0.30 (SD 0.95) | 8.00 (SD 18.43) | 23.90 (SD 26.22) | 25.89 (SD 27.18) |
| P value | .34 | .54 | .36 | .59 |
Abbreviations: ADLs, activities of daily living; SD, standard deviation; SLR, straight leg raise.
a Values are mean.
b Statistically significant difference between the groups.
In contrast, group nail had significantly higher scores than group plate for the ADLs assessment at week 4 after surgery (P = .03), with an improving trend observed at weeks 1, 2, and 3 (P = .15, P = .055, and P = .068, respectively).
Active ROM, angle of hip flexion, and abduction
Group plate had a significantly greater active ROM of hip flexion than that of group nail at weeks 3 and 4 after surgery (P = .04 and P = .02, respectively), whereas no significant difference was observed in ROM of hip abduction between the groups at any week.
Time to achieve active SLR
Group plate tended to achieve better recovery at week 4 than that of group nail (P = .10).
Time to achieve independent standing on the surgical leg
No significant differences were observed between the groups at any week. Although patients of group nail were unable to stand on the affected leg at weeks 1 and 2, they dramatically recovered at week 3 (P = .04).
Discussion
Previous studies on functional recovery in similar patients have produced varied results. Hardy et al reported that patients undergoing nail fixation had significantly improved mobility at 1 and 3 months after surgery.14 Pajarinen et al also described that patients achieved early walking more effectively after nail fixation than that after plate fiaxation.15 In contrast, Madsen et al reported that patients undergoing plate fixation had better walking ability (to a level almost equivalent to the preinjury status) at 6 months after surgery.16 In contrast, Utrilla et al reported no difference in functional outcomes between patients who underwent plate and nail fixation. However, when they evaluated patients with unstable intertrochanteric fractures, the results showed that nail fixation resulted in better outcomes.11 No prior studies have compared functional recovery in the very early period after surgery. In this study, we evaluated the recovery of ADLs every week in the very early period after surgery, that is, within 1 month after surgery. In addition, the use of the strict inclusion criteria in selecting patients for this study enabled us to compare the difference between the 2 methods more accurately.
Surgical invasiveness could further affect the postoperative recovery of ADLs. Our results suggested no significant difference in the invasiveness of either procedure. Operation time in group plate was greater than that in group nail. This difference was probably related to the longer time required to repair dissected muscles such as the iliotibial tract and vastus lateralis muscle. However, no significant differences were observed between the groups in terms of postoperative blood loss. These results are comparable with those of Hong et al.17
Differences in the postoperative recovery of ADLs between groups plate and nail can be attributed to postoperative bone stability and invasiveness of each procedure to the hip muscles. In terms of bone stability, patients undergoing nail fixation had significantly better ADL scores than those undergoing plate fixation but did not perform well when required to stand on the surgical leg with full weight bearing. Aros et al reported that the mechanical axis of the intramedullary nail lies closer to the axis of the femur in nail fixation than in plate fixation. Therefore, nail could decrease mechanical bending stress to the implant.18 Thus, the mechanical superiority of nail may explain the early achievement of stable gait and the ability to crouch.
In contrast, group nail did not perform as well in terms of active ROM of hip flexion. Hip flexion requires contraction of complex muscle groups, including the rectus femoris, iliopsoas, tensor fasciae latae, and gluteus medius muscles.19 Thus, this difference was probably related to differences in surgical invasiveness to the tensor fasciae latae and gluteus medius muscles. These muscles are invaded at the nail insertion point only in nail fixation. Although patients treated with nail fixation could not stand on the affected leg at weeks 1 and 2 after surgery, they finally achieved the ability to stand on 1 leg at week 3. This dramatic recovery could be associated with the eventual recovery of the gluteus medius muscle after nail fixation.
Some limitations were observed in this study. The majority of patients considered for this study were elderly individuals with intertrochanteric fractures who met the exclusion criteria due to deterioration of locomotive ability, dementia, or another excluding factor. Thus, there were only a few patients who were able to continue and complete the study. Further randomized studies including a larger number of patients are necessary to determine the ideal implant for treating intertrochanteric fractures. In conclusion, we found novel evidence for functional recovery in the very early period after surgery in this prospective study with a small sample size.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ahrengart L, Tornkvist H, Fornander P, et al. A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res. 2002;(401):209–222 [DOI] [PubMed] [Google Scholar]
- 2. Domingo LJ, Cecilia D, Herrera A, Resines C. Trochanteric fractures treated with a proximal femoral nail. Int Orthop. 2001;25(5):298–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boldin C, Seibert FJ, Fankhauser F, Peicha G, Grechenig W, Szyszkowitz R. The proximal femoral nail (PFN); a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow-up of 15 months. Acta Orthop Scand. 2003;74(1):53–58 [DOI] [PubMed] [Google Scholar]
- 4. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2005 Oct 19;(4):CD000093. [DOI] [PubMed] [Google Scholar]
- 5. Bannister GC, Gibson AG, Ackroyd CE, Newman JH. The fixation and prognosis of trochanteric fractures. A randomized prospective controlled trial. Clin Orthop Relat Res. 1990;(254):242–246 [PubMed] [Google Scholar]
- 6. Aune AK, Ekeland A, Odegaard B, Grøgaard B, Alho A. Gamma nail vs compression screw for trochanteric femoral fractures. 15 reoperations in a prospective, randomized study of 378 patients. Acta Orthop Scand. 1994;65(2):127–130 [DOI] [PubMed] [Google Scholar]
- 7. Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73(2):330–334 [DOI] [PubMed] [Google Scholar]
- 8. Dujardin FH, Benez C, Polle G, Alain J, Biga N, Thomine JM. Prospective randomized comparison between a dynamic hip screw and a mini-invasive static nail in fractures of the trochanteric area: preliminary results. J Orthop Trauma. 2001;15(6):401–406 [DOI] [PubMed] [Google Scholar]
- 9. Harrington P, Nihal A, Singhania AK, Howell FR. Intramedullary hip screw versus sliding hip screw for unstable intertrochanteric femoral fractures in the elderly. Injury. 2002;33(1):23–28 [DOI] [PubMed] [Google Scholar]
- 10. Mahomed N, Harrington I, Kellam J, Maistrelli G, Hearn T, Vroemen J. Biomechanical analysis of the Gamma nail and sliding hip screw. Clin Orthop Relat Res. 1994;(304):280–288 [PubMed] [Google Scholar]
- 11. Utrilla AL, Reig JS, Munoz FM, Tufanisco CB. Trochanteric gamma nail and compression hip screw for trochanteric fractures: a randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005;19(4):229–233 [DOI] [PubMed] [Google Scholar]
- 12. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 suppl):S1–S133 [DOI] [PubMed] [Google Scholar]
- 13. Nakamura K, Kawaguchi H. Locomotive syndrome. Nihon Rinsho. 2011;69(7):1323–1331 [PubMed] [Google Scholar]
- 14. Hardy DC, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998;80(5):618–630 [DOI] [PubMed] [Google Scholar]
- 15. Pajarinen J, Lindahl J, Michelsson O, Savolainen V, Hirvensalo E. Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Joint Surg Br. 2005;87(1):76–81 [PubMed] [Google Scholar]
- 16. Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Strømsøe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998;12(4):241–248 [DOI] [PubMed] [Google Scholar]
- 17. Hong JY, Suh SW, Park JH, Shin YS, Yoon JR, Yang JH. Comparison of soft-tissue serum markers in stable intertrochanteric fracture: dynamic hip screw versus proximal femoral nail – A preliminary study. Injury. 2011;42(2):204–208 [DOI] [PubMed] [Google Scholar]
- 18. Aros B, Tosteson AN, Gottlieb DJ, Koval KJ. Is a sliding hip screw or im nail the preferred implant for intertrochanteric fracture fixation? Clin Orthop Relat Res. 2008;466(11):2827–2832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Michael Schünke. Prometheus: AllgemeineAnatomie und Bewegungssystem: LernAtlas der Anatomie. Germany: Georg ThiemeVerlag; 2009:424–429 [Google Scholar]