Abstract
Background:
The assessment of oral health status of children in government and private schools provide data on the oral health status of children from different socio-economic background.
Aim:
The aim of the following study is to assess and to compare the oral hygiene status, gingival status and caries experience between children from government and private schools in Andhra Pradesh, India.
Subjects and Methods:
A combination of cluster and stratified random sampling was employed to select the study participants. Oral hygiene status, gingival status and caries experience was assessed and compared among 12- and 15-year-old children from three government and private schools each. The examination was carried out by three trained and calibrated investigators using a mouth mirror and explorer under natural daylight.
Results:
A total of 604 children (331 government and 273 private) were examined in the study. The mean oral hygiene index-simplified (OHI-S) was higher among government school children (2.9 [1.1]) compared private school children (0.6 [0.4]). The mean gingival score and mean decayed missing filled teeth were also higher among government school children compared with private school children. A significantly higher number of children in the government schools had poor oral hygiene status, moderate to severe gingivitis and caries experience.
Conclusion:
The prevalence of oral diseases was relatively less among children from private schools in comparison with those from government schools. Hence, the children from government schools should be given the priority compared with private school children in any school dental health programs planned on a statewide basis.
Keywords: Decayed missing filled teeth, Gingivitis, Oral health status, Oral hygiene status, School children
Introduction
Oral health is an inseparable part of general health. In many industrialized countries, a significant improvement in oral health among children and adolescents, especially with respect to dental caries has been witnessed in the last 2 decades.[1,2,3] This dramatic change in the trend may be attributed to the modification in the dietary habits, improved oral hygiene practices, effective use of fluorides, and establishment of school-based preventive programs.[4,5] Conversely, the oral diseases are on the rise in many developing and underdeveloped countries.[6,7]
India, a developing country, faces many challenges in rendering oral health needs. The majority of Indian population resides in rural areas.[8] It is necessary to know the prevalence and distribution of oral health problems and understand the dental health practices that people follow. Such information is basic for formulation of oral health policies and appropriate programs. The appropriate policies and programs will facilitate in improving awareness and knowledge of the general public about the preventive and promotive aspects of oral health as well as, to create the required services and train the necessary dental manpower to meet these needs.[9] Lack of awareness about dental diseases has resulted in gross neglect of oral health.[10]
Children <18 years constitute about 40% of the Indian population.[11] There is lack of organized school health programs in our country. The children in schools are relatively easily accessible, compared to any other population groups for any health promotion programs aimed at effecting the lifestyle changes. School health programs have proven effective in promoting health in many developed countries.[12,13] The New Zealand school dental nurse program implemented in the early part of the 20th century to combat the oral health problems of the school going children reflects the benefits of organized school dental programs.[14]
India does not have a national oral health policy at present, though a National health policy has been drafted. This suggests that the policy makers are neglectful of oral health, and its promotion is not being given the necessary attention in our country. Policy makers have to be made aware that oral health is fundamental to general health and well-being.[15]
In view of the limited resources, the implementation of school health policy, if not oral health policy may cater to the oral health needs of 40% of the school children. According to current estimates, 80% of all schools in the country are government schools, making the government, the major provider of education.[16] Most of the schools run by the private sector are situated in urban areas and these schools usually house children from middle, upper middle and upper socio-economic classes.[17] It is important to identify the risk groups to best utilize the scant resources in the present circumstances. The assessment of oral health status of children in government and private schools may provide us baseline data on the oral health status of children from different socio-economic background. This helps in prioritizing the services to the high risk groups when policies and programs for school going children are implemented. The surveys reporting the oral health status of government and private school children were scanty in Andhra Pradesh, India. The present study assessed and compared the oral health status between government and private school children in Andhra Pradesh, India in an attempt to identify the high risk groups.
Subjects and Methods
The study was cross-sectional in nature and ethical clearance for the study was obtained from the institutional ethics committee, Government Dental College and Hospital, Hyderabad.
Selection of study participants
The selection of study participants was done using a combination of cluster and stratified random sampling technique. Initially, two stage cluster sampling was used for the selection of the required number of schools for the study. In the first stage, all the localities in Hyderabad were listed and this list was used for randomly choosing two different localities. Then, all the government and private secondary schools in the selected localities were listed out. Each locality had around 8-10 government and private schools. Three government and private schools each from these localities was again randomly selected using the lottery method. This resulted in the selection of approximately one-third of the government and private schools in each locality.
The head masters of the selected secondary schools were apprised about the study protocol by the principle investigator and permission to carry out the study was obtained from the headmasters of these schools after clarifying all the queries raised by them. The list of 12- and 15-year-old children in the selected schools was obtained from the concerned headmasters and children in each of the age groups were given a unique identifier.
A stratified random sampling was used for selecting the male and female children from these schools. All the males and females in each of these age groups were first stratified. Then, either the first or the second number (either odd or even) was selected using a lottery method and subsequently, every alternate student from this number onwards was selected. This resulted in the inclusion of 50% of the children in each age and gender groups in the selected schools. A verbal consent was obtained from each participant besides informed consent from their parents. The consent for conducting the clinical examination of children was obtained from the parents by means of a circular issued through the school system.
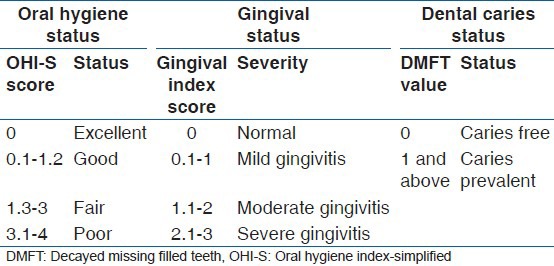
The examination of the selected school children was carried out by three trained and calibrated examiners over a period of 3 months from November 2012 to January 2013 after obtaining informed consent from the students and their parents. The training and calibration of the investigators was carried out in the Department of Public Health Dentistry, Government Dental College over a period of 1 week. The kappa statistics for inter examiner reliability with respect to oral hygiene index-simplified (OHI-S), gingival index (GI) and decayed missing filled teeth (DMFT) index were 0.8, 0.7 and 0.9, respectively. The clinical examination of the children was done in the school premises under natural day light on a plastic chair using a mouth mirror and explorer. A set of 30 mouth mirrors and explorers were used in the present study. The oral hygiene status, gingival status and dental caries experience was assessed using OHI-S (Greene and Vermillion 1964),[18] GI (Loe and Silness 1963)[19] and DMFT index (Klein, Palmer, Knutson 1938).[20] The autoclaved set of instruments was used for clinical oral examination of the children. The subjects were divided into four categories based on the oral hygiene simplified score and gingival scores. The subjects were classified into two categories (caries free or caries prevalent) depending on the DMFT score. The details of categorization and the criteria employed are depicted in Table 1.
Table 1.
Criteria employed for classifying the study participants into different categories based on OHI-S, gingival and DMFT scores
Data were initially entered onto a data collection sheet. Data were then entered onto personal computer and statistical analysis was performed using SPSS version 20 (Chicago, USA). The OHI-S, GI and DMFT sores were expressed in mean and standard deviation (SD). The distribution of study participants based on oral hygiene status, gingival status and caries experience were expressed as frequencies and percentages. The statistical analysis was done using t-test, Mann–Whitney U-test and Chi-square test. The statistical significance was fixed at 0.05.
Results
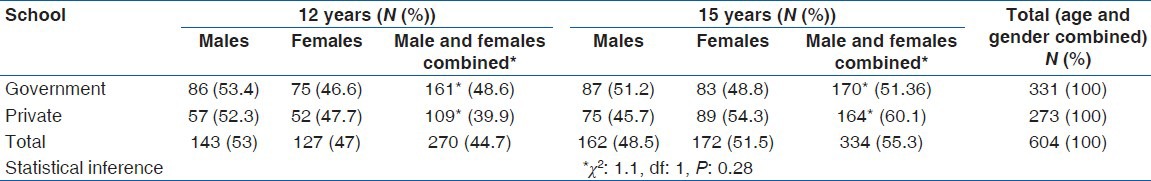
A total of 604 children were examined in the present study. Among this, 331 were from government schools and 273 from private schools. There was no statistically significant difference in age and gender distribution of study participants between government and private schools [P = 0.28 Table 2]. The mean OHI-S and gingival scores between government and private school children were compared using independent sample t-test (distribution was normal). The mean DMFT between children from Government and private schools was compared using Mann–Whitney U-test (distribution was not normal). The distribution of the children in relation to oral hygiene status, severity of gingivitis, caries experience was compared using the Chi-square test.
Table 2.
Age and gender distribution of the children in government and private schools
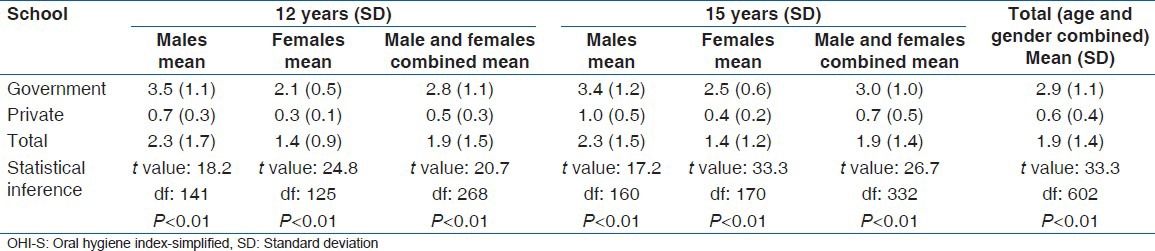
Oral hygiene status
The mean OHI-S score for the study population was 1.9 (1.4 - SD). The mean OHI-S score was significantly higher among children from Government schools (2.9 [1.1]) than from private schools (0.6 [0.4]) [P < 0.01, Table 3].
Table 3.
Mean OHI-S score among the study participants
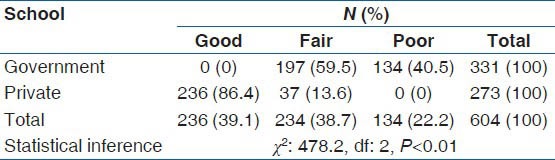
Oral hygiene status was good among 39.1% of the school children (mean OHI-S score <1.2). It was fair (mean OHI-S score between 1.3 and 3) and poor (mean OHI-S >3) among 38.7% and 22.2% of the study participants respectively. Good oral hygiene status was found among 86.4% of the children from private schools while none of the children from government schools had this. The children with poor oral hygiene status were significantly higher in government schools (40.5%) compared to private schools (22.2%) [P < 0.01, Table 4].
Table 4.
Distribution of study participants according to oral hygiene status
Gingival status
The mean gingival score for the study population was 1.2 and SD of 0.6. The mean gingival score was significantly less among private school children (0.7 [0.3]) compared to government school children (1.6 [0.5]) [P < 0.01, Table 5]. The government school children had a higher mean gingival score compared to private school children even when a separate comparison was made among different age and gender groups [Table 5].
Table 5.
Mean gingival score among the study participants
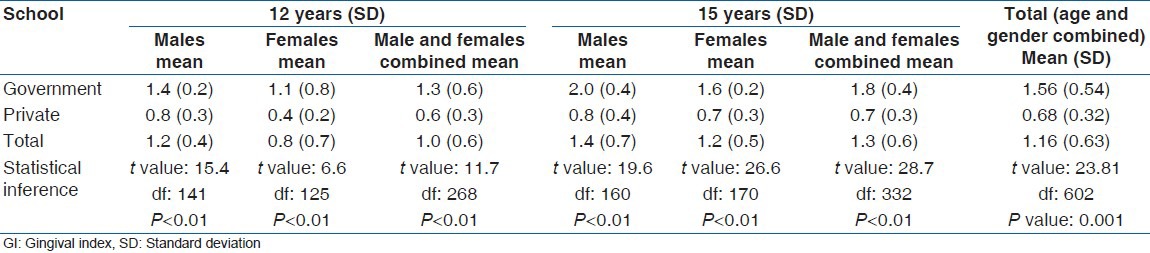
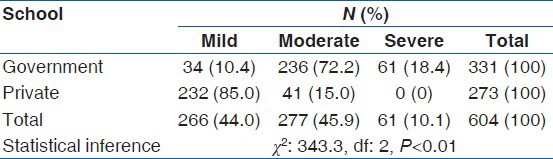
None of the children in the present study had healthy gingiva. Mild gingivitis was found among 44% of the children. Moderate and severe gingivitis was found among 45.9% and 10.1% of the study participants respectively. The prevalence of mild and moderate gingivitis among private school children was 85% and 15%, respectively. None of these children had severe gingivitis. Only 10.4% of the children from government schools had mild gingivitis, while 72.2% had moderate and 18.4% had severe gingivitis. Significantly higher proportion of children from government schools had moderate to severe gingivitis compared to private school children [P < 0.01, Table 6].
Table 6.
Prevalence of mild, moderate and severe gingivitis among the study participants
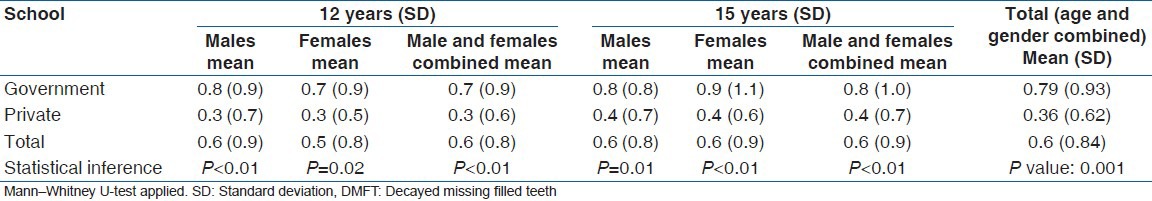
Dental caries experience
The mean DMFT score for the study population was 0.6 with a SD of 0.8. The mean DMFT score among government school children was 0.8 (0.9) was significantly higher compared private school children (0.4 [0.6]) [P < 0.01, Table 7]. These results were true even when a separate comparison was made among different age and gender groups between government and private schools [Table 7].
Table 7.
Mean DMFT among the study participants
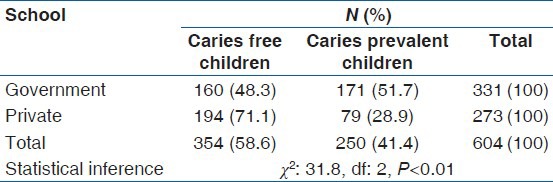
The prevalence of dental caries among the study participants was 41.4%. The prevalence was significantly higher [P < 0.01, Table 8] among government school children (51.7%) compared to private school children (28.9%).
Table 8.
Dental caries prevalence among the study participants
Discussion
A healthy mouth enables an individual to speak, eat and socialize without the feeling of any discomfort or embarrassment.[21] Schools provide a platform for the promotion of health and oral health not only for the students, but also for the staff, families, and members of the community as a whole.[22] Although, oral health is an integral part of general health, it has not received any significant consideration in national health policies or in the planning of national health programs in many developing countries.[15] The present study was undertaken to assess and compare the oral health status of children from government and private schools which may be a proxy for children from different socio-economic background. The identification of high risk groups facilitate prioritizing the services to the most deserving especially when resources are sparse.
A higher percentage of children from the private schools had good oral hygiene status compared to government school children in the present study. The oral hygiene practices[8,23,24,25] and dental care utilization[26] are better among children from private schools. The result was in agreement with the widely held view that the private school students were from relatively higher socio-economic status families than the public school children and as a result, there was close monitoring of tooth brushing habits especially in the morning among children from private schools. A study by Lateefat et al.,[27] found a higher percentage of students attending the private school to have good oral hygiene status (61.4%) compared to those attending public school (21%). Another study by Batwala et al.[28] found lower odds for plaque (odds ratio [OR]: 0.6, 95% confidence interval (CI): 0.4-0.9) and calculus (OR: 0.4, 95% CI: 0.2-0.9) among school children attending private schools. The lower odds among private school children indicate poor oral hygiene status among children from government schools in comparison with those from private schools. The results of our study were consistent with these findings and others.[29]
The mean gingival score as well as the prevalence of moderate and severe gingivitis was higher among children in government schools compared to those in private schools in the present study. Shailee et al.[23] in their study found healthy periodontium among 16.6% of the 12-year-old children from government schools while this was found among 83.4% of the participants from private schools. A significantly higher percentage of 15-year-old children from private schools had healthy periodontium (28.4%) compared to those from government schools (14%). A significantly higher percentage of 12 years and 15-year-old children from government schools had bleeding (51% and 53.2%) calculus (58.8% and 24.8%) compared to those from private schools (bleeding - 49% and 52.1%, respectively among 12 and 15-year-old) (Calculus - 41.2% and 16.5%, respectively among 12- and 15-year-old). They concluded that the periodontal condition was relatively healthy among children from private schools compared to those from government schools. The difference was attributed to somewhat irregular oral hygiene practices among children in government schools which in turn may be linked to their lower socio-economic status and lower utilization of dental services. The results of our study were in agreement with the findings of this study and others.[8]
The mean DMFT score among the study participants was 0.6 (0.8) with overall prevalence of 41.4%. The prevalence of dental caries prevalence among 12-year-old children was 53.8% in the National oral Health Survey and Fluoride Mapping in India. The study participants in the present study were recruited from an endemic fluoride belt. The lower DMFT value and lower prevalence of dental caries in the present study compared to the national average may be attributed to the protective effect mediated by continuous exposure of the teeth to fluoridated water among our study participants.
The mean DMFT score as well as the prevalence of dental caries was higher among children in the government schools compared to those in private schools in the present study. The mean number of untreated decayed teeth, teeth missing because of dental caries was significantly higher among government school children, while the mean number of filled teeth was higher among private school children.
A study by Shailee et al.[23] found a statistically significant difference in mean DMFT between the government and the private schools. The prevalence of dental caries among 12 years and 15-year-old children from government schools was 70.3% and 66%, respectively. The prevalence among 12 years and 15-year-old children from private schools was 32.8% and 35.9%, respectively. The caries experience was higher among the children attending government schools compared to private school children. This difference was attributed to lack of awareness, affordability, or underutilization of dental care facilities by the children in the government schools. The higher mean filled teeth among children in private schools was attributed to parents’ attitude and dental awareness, which was reflected in the child's oral health maintenance. The results of our study were consistent with the findings of this study and others.[30,31]
The present study may be considered as a pilot study in the state of Andhra Pradesh. The results of the present study need to be validated by a larger study on a statewide basis. Such studies will facilitate the policy makers in at least considering the implementation of effective school based preventive programs in schools with higher needs, if not simultaneously in all schools.
Conclusion
From the results of the present study, we can conclude that the oral hygiene status, gingival health and dental caries status was poor among government school children compared to those in private schools. Although, oral health care services needs to be offered for all children, it is very essential to offer these services to children from government schools which normally house children from low socio-economic background on a priority basis. The oral health services specifically targeted toward high risk children is the need of the hour due to scant resources.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Burt BA. Trends in caries prevalence in North American children. Int Dent J. 1994;44:403–13. [PubMed] [Google Scholar]
- 2.Petersen PE, Christensen LB, Moller IJ, Johansen KS. Continuous improvement of oral health in Europe. J Ir Dent Assoc. 1994;40:105–7. [PubMed] [Google Scholar]
- 3.Beltrán-Aguilar ED, Estupiñán-Day S, Báez R. Analysis of prevalence and trends of dental caries in the Americas between the 1970s and 1990s. Int Dent J. 1999;49:322–9. doi: 10.1111/j.1875-595x.1999.tb00532.x. [DOI] [PubMed] [Google Scholar]
- 4.Bratthall D, Hänsel-Petersson G, Sundberg H. Reasons for the caries decline: What do the experts believe? Eur J Oral Sci. 1996;104:416–22. doi: 10.1111/j.1600-0722.1996.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Geneva: WHO; 2000. Global Oral Health Data Bank. [Google Scholar]
- 6.Petersen PE, Danila I, Delean A, Grivu O, Ionita G, Pop M, et al. Oral health status among schoolchildren in Romania, 1992. Community Dent Oral Epidemiol. 1994;22:90–3. doi: 10.1111/j.1600-0528.1994.tb01579.x. [DOI] [PubMed] [Google Scholar]
- 7.Petersen PE, Razanamihaja N. Oral health status of children and adults in Madagascar. Int Dent J. 1996;46:41–7. [PubMed] [Google Scholar]
- 8.Mahesh Kumar P, Joseph T, Varma RB, Jayanthi M. Oral health status of 5 years and 12 years school going children in Chennai city – An epidemiological study. J Indian Soc Pedod Prev Dent. 2005;23:17–22. doi: 10.4103/0970-4388.16021. [DOI] [PubMed] [Google Scholar]
- 9.Bali RK, Mathur VB, Talwar PP, Chanana HB. India New Delhi: Dental Council of India; 2004. National Oral Health Survey and Fluoride Mapping 2002-03. [Google Scholar]
- 10.Shekar BR, Suma S, Kumar S, Sukhabogi JR, Manjunath BC. Malocclusion status among 15 years old adolescents in relation to fluoride concentration and area of residence. Indian J Dent Res. 2013;24:1–7. doi: 10.4103/0970-9290.114910. [DOI] [PubMed] [Google Scholar]
- 11.Gross Enrolment Ratios in Primary and Upper Primary Schools. Selected Educational Statistics, Ministry of Human Resource Development, Government of India. Infochange education. News and analysis on social justice and developmental issues in India. [Last cited on 2014 Feb 22]. Available from: http://www.infochangeindia.org/education/statistics/gross-enrolmentratios-in-primary-and-upper-primary-schools.html .
- 12.Wells J, Barlow J, Stewart-Brown S. A systematic review of universal approaches to mental health promotion in schools. Health Educ J. 2003;103:197–220. [Google Scholar]
- 13.Swart D, Reddy P. Establishing networks for health promoting schools in South Africa. J Sch Health. 1999;69:47–50. doi: 10.1111/j.1746-1561.1999.tb06366.x. [DOI] [PubMed] [Google Scholar]
- 14.Nash DA, Friedman JW, Kardos TB, Kardos RL, Schwarz E, Satur J, et al. Dental therapists: A global perspective. Int Dent J. 2008;58:61–70. doi: 10.1111/j.1875-595x.2008.tb00177.x. [DOI] [PubMed] [Google Scholar]
- 15.Chandrashekar BR, Suma S, Kiran K, Manjunath BC. The use of school teachers to promote oral hygiene in some secondary school students at Hyderabad, Andhra Pradesh, India: A short term prospective pilot study. J Family Community Med. 2012;19:184–9. doi: 10.4103/2230-8229.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Primary education system in India. Education in India. [Last cited on 2013 Aug 31]. Available from: http://www.en.wikipedia.org/wiki/Education_in_India#cite_note-envision-20 .
- 17.Desai S, Dubey A, Vanneman R, Banerji R. Private schooling in India: A new educational landscape. India Human Development Survey Working Paper No. 11. [Last cited on 2013 Aug 31]. Available from: http://www.ihds.umd.edu/IHDS_papers/PrivateSchooling.pdf .
- 18.Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 19.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 20.Klein H, Palmer CE, Knutson JW. Studies on dental caries. I. Dental status and dental needs of elementary school children. Public Health Rep. 1938;53:751. [Google Scholar]
- 21.Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: An opportunity for oral health promotion. Bull World Health Organ. 2005;83:677–85. [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Geneva: WHO; 1999. Status of School Health. Report of the School Health Working Group and WHO Expert Committee on Comprehensive School Health Education and Promotion. [Google Scholar]
- 23.Shailee F, Girish MS, Kapil RS, Nidhi P. Oral health status and treatment needs among 12- and 15-year-old government and private school children in Shimla city, Himachal Pradesh, India. J Int Soc Prev Community Dent. 2013;3:44–50. doi: 10.4103/2231-0762.115715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wierzbicka M, Petersen PE, Szatko F, Dybizbanska E, Kalo I. Changing oral health status and oral health behaviour of schoolchildren in Poland. Community Dent Health. 2002;19:243–50. [PubMed] [Google Scholar]
- 25.Taani DQ. Caries prevalence and periodontal treatment needs in public and private school pupils in Jordan. Int Dent J. 1997;47:100–4. doi: 10.1111/j.1875-595x.1997.tb00683.x. [DOI] [PubMed] [Google Scholar]
- 26.Taani DQ. Relationship of socioeconomic background to oral hygiene, gingival status, and dental caries in children. Quintessence Int. 2002;33:195–8. [PubMed] [Google Scholar]
- 27.Lateefat S, Musa OI, Kamaldeen AS, Buhari AS, Saka AO. Determinants of oral hygiene status among junior secondary school students in Ilorin West local government area of Nigeria. IOSR J Pharm Biol Sci. 2012;1:44–8. [Google Scholar]
- 28.Batwala V, Mulogo EM, Arubaku W. Oral health status of school children in Mbarara, Uganda. Afr Health Sci. 2007;7:233–8. [PMC free article] [PubMed] [Google Scholar]
- 29.Bamigboye O, Akande TM. Oral hygiene status of students in selected secondary schools in Osogbo, Nigeria. Niger Med Pract. 2007;51:71–5. [Google Scholar]
- 30.de Almeida CM, Petersen PE, André SJ, Toscano A. Changing oral health status of 6- and 12-year-old schoolchildren in Portugal. Community Dent Health. 2003;20:211–6. [PubMed] [Google Scholar]
- 31.Shailee F, Sogi GM, Sharma KR, Nidhi P. Dental caries prevalence and treatment needs among 12- and 15- Year old schoolchildren in Shimla city, Himachal Pradesh, India. Indian J Dent Res. 2012;23:579–84. doi: 10.4103/0970-9290.107330. [DOI] [PubMed] [Google Scholar]


