Abstract
Introduction:
End-of-life surgical care is a major concern with a significant number of operations performed within the last year of life; surgery for hip fractures is a prime example. Unfortunately, no simple objective tool exists to assess life expectancy in the postoperative period. The goal of our study was to analyze 2 simple geriatric life expectancy calculators to compare with the current Veterans Affairs Surgical Quality Improvement Program (VASQIP) postoperative 30-day mortality calculator.
Methods:
This retrospective study assessed the utility of 3 validated calculators in 47 hip fracture repairs from July 2009 to May 2011. The tools included: 30-day VASQIP mortality calculator, 6-month Minimum Data Set Mortality Risk Index-Revised (MMRI-R), and Four-Year Mortality Index. The VASQIP calculator requires chart review, Current Procedural Terminology (CPT) codes, and laboratory analysis, whereas the mortality risk indices require simple patient questioning if prospective or simple chart review if retrospective. Scoring was performed and mortality risk was compared between survivors and nonsurvivors.
Results:
A total of 47 hip fractures were repaired during the study period with 37 survivors and 10 nonsurvivors. In all, 7 died within 30 days, 2 died within 6 months, and 1 died greater than 6 months after surgery. The mean age (standard deviation [SD]) of all patients undergoing hip fracture repair was 73.6 (13.3) years. The VASQIP calculator mean (SD) 30-day mortality risk was 10.4% (5.4) for nonsurvivors compared to survivors 4.3% (5.5), P < .003; the MMRI-R mean (SD) mortality risk was 35.8% (15.4) for nonsurvivors compared to survivors 14.7% (9.5), P < .001; the Four-Year Mortality Index mean (SD) mortality risk was 60.9% (16.9) for nonsurvivors compared to survivors 48.9% (24.4), P < .09.
Conclusion:
Overall, the VASQIP 30-day and MMRI-R 6-month mortality calculators showed significant differences in mortality risk between survivors versus nonsurvivors in a population with hip fracture. In contrast, the Four-Year Mortality calculator may not sufficiently discriminate operative risk. The easily obtained MMRI-R has the potential to provide information on short-term postoperative mortality risk.
Keywords: frailty, mortality, postoperative, risk, hip fracture, paper
Introduction
Surgical intervention at the end of life is a significant consideration and is associated with many operations performed within the last year of life. One example of end-of-life surgery is repair of acute hip fractures in the elderly population. Despite the ability to repair hip fractures expeditiously and discharge patients, repaired hip fracture mortality remains high over the course of the next year. Data would suggest that it is not the repair of the hip fracture that is the key to mortality, as several studies suggest nonoperative treatment of hip fractures with early mobilization in selected patients results in similar mortality and outcome when compared to an operative approach.1 Specifically, Jain et al showed that bed rest in nonoperatively treated patients is associated with significantly higher mortality within 30 days of hip fracture than both operatively treated patients and those managed with early mobilization. Therefore, in patients who can tolerate operative management, surgical stabilization within a reasonable time frame is preferred, and nonoperative management should be reserved for those who are poor surgical candidates.
There is a clear a need to identify the life expectancy of patients undergoing emergent hip fracture repair whose life expectancy is such that standard of care surgical treatment may not be the ideal option. This point is reinforced by recent literature, which documents that more than 30% of patients have a major surgical procedure within 1 year of their death and many within the last weeks to months of their life. Kwok et al note in the discussion that their results should lead to a “renewed effort to identify the optimum care for dying patients, taking their wishes into account, to ensure that interventions help extend life and reduce suffering.”2(p 1413) Additionally, literature has shown that early institution of palliative care in patients with metastatic non-small cell lung cancer resulted in better quality of life and longer survival times than those receiving standard oncologic intervention alone. Along these lines, it has been shown that patients with hip fracture who are treated nonoperatively with specific attention to the period immediately surrounding the fracture (ie, early mobilization) have similar outcomes to surgically treated patients. The question remains: which patients with hip fracture would do best with nonoperative therapy?3,4
One parameter that may help guide decision making on how best to manage these patients is frailty. A recent meta-analysis found strong evidence for 12 predictors of postoperative mortality following a hip fracture repair, including “nursing home or facility residence, poor preoperative walking capacity, poor activities of daily living, poor mental state, and dementia or cognitive impairment.”5 Interestingly, many of these 12 strong predictors overlap with items included in frailty assessment scales, such as low physical activity and slow walking speed.6 Recently, frailty has been shown to correlate significantly with morbidity and mortality.1,6–8 These studies have primarily relied on common and accepted geriatric measures of frailty, requiring the patient to perform functional maneuvers, which clearly would not be practical in the hip fracture population. Therefore, we sought to identify a frailty-based mortality calculator that would allow for bedside assessment of at-risk patients without the need for physical patient participation in an attempt to establish a relationship between the state of frailty and postoperative mortality risk. We set out to accomplish this by retrospectively applying mortality indices that reflect frailty to a patient population who underwent hip fracture repair.
Methods
Study Design
We conducted a retrospective chart review study of surgical patients who presented to the Omaha Veterans Affairs (VA) Medical Center from July 2009 to May 2011, requiring emergent hip fracture repair. The study was locally approved by Institutional Review Board. These patients were identified by retrieving information on all orthopedic surgeries with Current Procedural Terminology (CPT) and Diagnosis Related Group (DRG) codes including hip fracture during the specified time frame. The CPT codes included open and closed hip reductions, hip fixations, hemiarthroplasties, dynamic screws, and total hip replacements with endoprosthesis.
All charts were accessed via electronic medical record, and relevant information was obtained by reviewing objective chart data (ie, laboratory results and X-ray findings) as well as progress notes from both the nursing staff and the physicians involved in each case. Patient information was collected and entered into an electronic database and data were used to complete 3 separate mortality calculators (JD). Mortality was assessed by the VA electronic medical records, which record all veterans’ dates of death.
Mortality Calculators
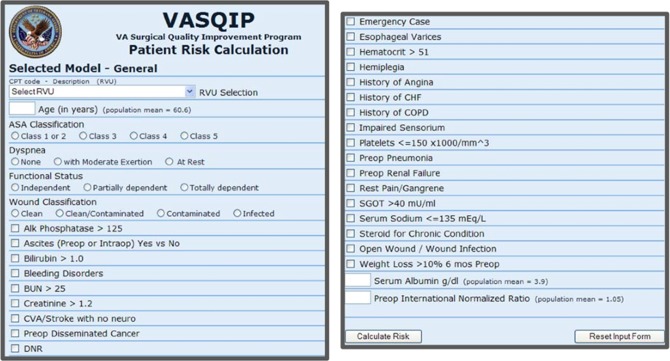
The Veterans Affairs Surgical Quality Improvement Program (VASQIP) calculator is an objective calculation that requires chart review, CPT codes, and laboratory analysis. Utilized and validated throughout the VA Hospital internal quality assurance program, this calculator assesses a patient’s 30-day mortality risk utilizing risk adjustment. There is a specialty model within the VASQIP system that is tailored for orthopaedic procedures, thus allowing for patient risk calculation. The values requested include the procedure relative value unit, patient age, and gender, American Society of Anesthesiology (ASA) classification, dyspnea, functional status, wound classification, bilirubin, serum glutamic-oxaloacetic transaminase, serum sodium, white blood cell count, weight loss, serum albumin, and international normalized ratio (INR) among other variables. This requires significant chart review and associated knowledge of procedure, laboratory value norms, and patient history; see Figure 1.
Figure 1.
Veterans Affairs Surgical Quality Improvement Program (VASQIP) calculator.
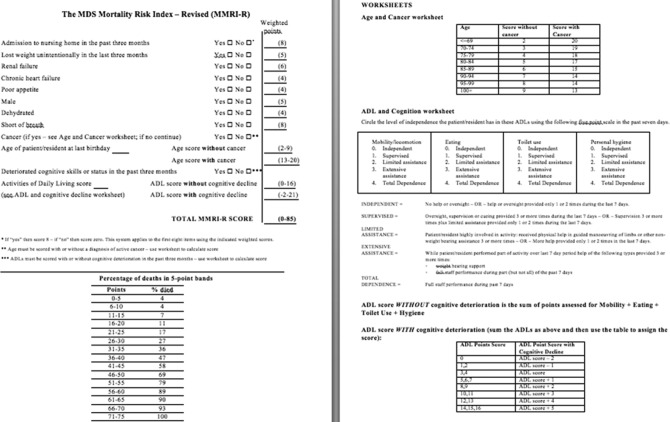
The 6-month Minimum Data Set Mortality Risk Index-Revised (MMRI-R) calculator can be administered to patients in clinic or at bedside. The tool requires calculations based on patient responses. It was validated in nursing home patients and is intended to predict 6-month mortality in this population. It has not been generalized to a surgical population. The 12-item inventory includes admission to a nursing care home within 3 months; unintentional weight loss in the past 3 months; renal failure; chronic heart failure; poor appetite; male gender; dehydration; shortness of breath; active cancer diagnosis; age; deteriorated cognitive skills in the past 3 months; and activities of daily living score. The MMRI-R mortality risk ranges from 4% to 100% based on a 5-point discriminatory scoring system8; see Figure 2 (http://www.ncbi.nlm.nih.gov/pubmed/20637076)
Figure 2.
Minimum Data Set Mortality Risk Index-Revised (MMRI-R) calculator.
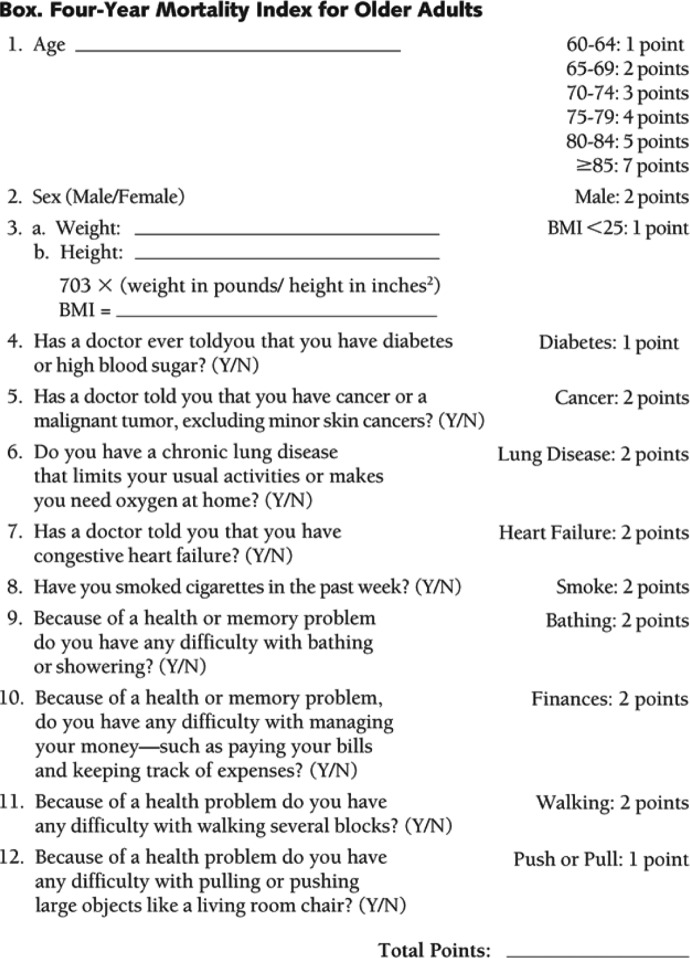
The Four-Year Mortality Index is a 12-item questionnaire and was validated in community-dwelling US adults older than 50 years. The index assigns point values to patients based on age range (50-69, 70-79, and ≥80); sex; body mass index (BMI) <25; diabetes or high blood sugar; cancer excluding minor skin cancer; activity-limiting chronic lung disease; congestive heart failure; cigarette use in the past week; difficulty bathing or showering; difficulty managing finances; difficulty walking several blocks; and difficulty moving large objects; see Figure 3. Lee et al found that “in the validation cohort, the mortality risk ranged from 4% in those with 0 to 5 points, 15% in those with 6 to 9 points, 42% in those with 10 to 13 points, and 64% in those with 14 or more points.”9(p 805) These point values were then graphed against percentage mortality risk, and this graph was utilized to assign a percentage to participants.
Figure 3.
Four-Year Mortality Index.
With all 3 calculators, if data points were not clearly stated in the chart, their respective values were considered absent when calculating patient mortality thus giving a lower predicted mortality, for purposes of the study. Particularly, dehydration status, cognitive decline, and activities of daily living scores were only accounted for if they were expressly stated and confirmed in notes within the patient chart.
Independent Variables
Information on age, race, gender, albumin, INR, hemoglobin, creatinine, and smoking status were collected for each patient. These were analyzed in addition to the data points for the MMRI-R and Four-Year calculators listed previously.
Statistical Analysis
Data were summarized with descriptive statistics. Chi-square tests (Fisher exact tests for sparse distributions) were utilized to assess differences in categorical variables between those living and those who died. Two-sample t tests (Mann-Whitney tests if t test assumptions were not met) were used to assess differences in numeric variables, including the MMRI-R and Four-Year calculators.
Results
A total of 47 hip fractures were repaired during the study period, with a total of 37 survivors and 10 nonsurvivors. Of the nonsurvivors, 7 died within 30 days, 2 died within 6 months, and 1 died more than 6 months after surgery. The mean (SD) age of all patients undergoing hip fracture repair was 73.6 (13.3) years. Of those patients analyzed, 95.7% were male and 97.8% were white. Demographic characteristics are displayed in Table 1. As shown, the general patient characteristics and laboratory values with the exception of albumin were not significant on univariate analysis when comparing the 37 survivors to the 10 nonsurvivors.
Table 1.
Demographic Characteristics of the Full Patient Cohort and Comparison of Demographics Between Survivors and Nonsurvivors.a
| Characteristic | Full Cohort (n = 47) | Survivors (n = 37) | Nonsurvivors (n = 10) | P Value |
|---|---|---|---|---|
| Age, mean ± SD | 73.6 ± 13.28 | 72.6 ± 13.87 | 77.1 ± 10.64 | .17 |
| Sex, % female | 4.3 | 2.7 | 10.0 | .38 |
| Race, % nonwhite | 2.1 | 0.0 | 10.0 | .2 |
| Preoperative location, % | .3 | |||
| Home | 66.0 | 73.0 | 40.0 | |
| Assisted living | 4.3 | 2.7 | 10.0 | |
| Skilled nursing facility | 10.6 | 8.1 | 20.0 | |
| Nursing home | 14.9 | 13.5 | 20.0 | |
| Other | 4.3 | 2.7 | 10.0 | |
| Albumin | 3.7 | 3.8 | 3.1 | .02 |
| Cr | 1.1 | 1.1 | 1.2 | .55 |
| Hgb | 11.6 | 11.8 | 10.9 | .41 |
| INR | 1.1 | 1.1 | 1.1 | .77 |
| Tobacco (cigarette) use, % | 21.3 | 24.3 | 10.0 | .3 |
Abbreviations: SD, standard deviation; Cr, creatinine; Hgb, hemoglobin; INR, international normalized ratio.
a Values of P < .05 indicate statistical significance.
Differences in mean calculated mortality risk between survivors and nonsurvivors were assessed for each of the calculators. For the VASQIP calculator, the mean (SD) calculated 30-day mortality risk was 10.4% (5.4) for nonsurvivors compared to survivors 4.3% (5.5), P < .003. The mean calculated MMRI-R mortality risk was 35.8% (15.4) for nonsurvivors compared to survivors 14.7% (9.5), P < .001. The mean calculated Four-Year Mortality Index mortality risk was 60.9% (16.9) for nonsurvivors compared to survivors, 48.9% (24.4), P < .09; see Table 2.
Table 2.
Calculated Mortality Risk for Survivors Versus Nonsurvivors for the Risk Indices Analyzed Including 30-Day VASQIP Calculator, 6-Month MMRI-R, and Four-Year Mortality Index.a
| Study | Survivor (n = 37) | Nonsurvivor (n = 10) | P Value |
|---|---|---|---|
| VASQIP | 4.3 (5.5) | 10.4 (5.4) | P < .003 |
| MMRI-R | 14.7 (9.5) | 35.8 (15.4) | P < .001 |
| Four-Year | 48.9 (24.4) | 60.9 (16.9) | P < .09 |
Abbreviations: VASQIP, Veterans Affairs Surgical Quality Improvement Program; MMRI-R, Minimum Data Set Mortality Risk Index-Revised.
a Values of P < .05 indicate statistical significance.
Among the independent variables built into each mortality calculator, several showed statistical significance when comparing survivors to nonsurvivors. We analyzed both the MMRI-R and the Four-Year calculators using percentage positive response for the all-or-none questions. For the MMRI-R, positive responses to admission to nursing home in the past 3 months (P = .01), unintentional weight loss in the last 3 months (P = .03), and cognitive decline and activities of daily living (P = .01), all showed statistical significance. For the Four-Year calculator, positive responses to BMI < 25 (P = .01) and difficulty managing finances (P = .04) showed statistical significance. Our results demonstrate that nonsurvival is associated with recent nursing home admission, unintentional weight loss, and cognitive decline and less independence with activities of daily living when compared to survival. This is shown in Table 3.
Table 3.
Comparison of Percentage Positive Response Between Survivors and Nonsurvivors for Independent Variables in the MMRI-R and Four-Year Mortality Index.a
| % Survivors (n = 37) | % Nonsurvivors (n = 10) | P Value | |
|---|---|---|---|
| MMRI-R positive response | |||
| Admission to nursing home in the past 3 months | 5.4 | 40.0 | .01 |
| Lost weight unintentionally in the last 3 months | 2.7 | 30.0 | .03 |
| Renal failure | 2.7 | 0.0 | 1 |
| Chronic heart failure | 8.1 | 20.0 | .29 |
| Poor appetite | 13.5 | 40.0 | .08 |
| Male | 97.3 | 90.0 | .38 |
| Dehydrated | 0 | 0.0 | |
| Short of breath | 18.9 | 10.0 | .67 |
| Cancer | 10.8 | 40.0 | .05 |
| Cognitive decline and Activities of Daily Living | 16.2 | 60.0 | .01 |
| Four-Year positive response | |||
| BMI <25 | 40.5 | 90.0 | .01 |
| Diabetes | 18.9 | 20.0 | 1 |
| Cancer | 8.1 | 30.0 | .1 |
| Lung disease | 24.3 | 20.0 | 1 |
| Heart failure | 8.1 | 20.0 | .29 |
| Smoker | 27.0 | 10.0 | .41 |
| Trouble bathing | 35.1 | 30.0 | 1 |
| Trouble with finances | 0.0 | 20.0 | .04 |
| Trouble walking | 73.0 | 80.0 | 1 |
| Trouble pushing or pulling | 24.3 | 40.0 | .43 |
Abbreviations: BMI, body mass index; MMRI-R, Minimum Data Set Mortality Risk Index-Revised.
a Values of P < .05 indicate statistical significance.
Discussion
Overall, the VASQIP 30-day and MMRI-R 6-month mortality calculators show significantly different mortality risk in survivors versus nonsurvivors in a population with hip fracture. Although the Four-Year Index accounts for lifestyle factors and comorbidities that seem to correlate with mortality risk, it may not sufficiently discriminate operative risk at the extremes of age reflected in the lack of statistical significance. This is most likely because the Four-Year Index relies heavily on patient age for point allocation as opposed to other frailty characteristics. Results of 4-year mortality risk may be reassessed in the future and reanalyzed. For the purpose of this study, the calculated mortality risks from each of the 3 calculators serve less as absolute predictive values. Instead, they provide tools to identify patients at increased risk of postoperative mortality; that is, the higher the calculated mortality risk, the higher the risk of mortality in the postoperative period.
In contrast to the surgically validated VASQIP mortality calculator that requires chart review and objective CPT code and laboratory data, the easily obtained MMRI-R has the potential to assess short-term mortality risk without requiring extensive chart review. The benefits of this index are ease of administration, inclusion of lifestyle factors and functional status, and in our hip fracture population, a significant correlation with postoperative outcome similar to the VASQIP calculator.
In the context of current literature, frailty has been shown to be a significant predictor of postoperative outcome.6 Given that the rate of elderly patients undergoing surgical procedures is rising and that these patients have an increased rate of adverse outcomes when compared to their younger counterparts, measuring frailty and utilizing the results to help guide patient care should be of interest to the and geriatric community. Despite the lack of a clear definition of frailty, there is consensus that postoperative complications are a more telling predictor of survival than preoperative or intraoperative risk factors.10 Makary et al showed that simple functional frailty measures markedly improve the accuracy of other tools like the Lee and Eagle score. Similarly, accounting for frailty improves the widely used ASA score.6 Additionally, as opposed to these traditional preoperative assessments of single organ dysfunction, frailty gives providers insight into overall patient well-being and level of functioning. Makary’s frailty tool requiring patient mobility to assess walking speed and a specialized instrument to measure grip strength is more advanced than the approach used by Robinson et al whereby laboratory data were combined with other functional measures of frailty such as the timed-up-and-go to again accurately predict postoperative complications. In contrast, the MMRI-R is a relatively simple frailty screen that can be administered quickly and that requires only verbal assent to questions regarding comorbidities and functional status as opposed to interactive assessments.
As the population ages, end-of-life surgery will become an even more prominent topic of discussion. Over half of all surgeries performed in the United States are done on patients aged 65 years and older, and as persons live longer and surgical and anesthetic techniques continue to improve, this percentage will likely continue to rise. As Robinson describes in a study evaluating colorectal surgery in older adults, frailty is not only a marker for increased postoperative complications but also predicts increased financial strain on the health care system as frailty is associated with higher 6-month postoperative health care costs.11 Clearly, the decision to perform surgery at the end of life, defined by Kwok et al as occurring within the last year of life, is associated with increased hospital admissions, length of stay, and longer intensive care duration, and this decision is one that many providers and families struggle with in an attempt to optimize care, outcomes, quality of life, and cost burden.2,11 Frailty assessment may be the “tool” to address the concerns regarding end-of-life surgical care. In several populations, including patients with cardiac and colorectal diseases, studies have identified that frailty correlates with postoperative mortality risk.2,10,11 Our study, in addition to the study by Holvik et al, demonstrates that calculated mortality risk correlates with increased incidence of postoperative mortality in the hip fracture repair population.12 Although the tools utilized in this study have been validated in nonsurgical populations, they appear to offer a questionnaire-based measure of functional status that correlates with frailty. Ultimately, identifying determinants of short-term outcome such as 1-year mortality rather than 30-day mortality is important to give providers and patients accurate data for shared decisions.
The strength of the current approach using a simple frailty tool is based on the ease of administration. Previous methods of measuring frailty relied on time-consuming functional testing and analysis, but the MMRI-R applied to a surgical population can be performed at bedside in less than 5 minutes and can also be corroborated with information from caregivers if the patient is unable to provide information. As an indicator of the power of single questions, a history of falls in the 6 months prior to surgery was an independent predictor of poor postoperative outcome when compared to patients who did not fall.13 Although this is not included in the MMRI-R index, it appears to reflect the power of simple questions to predict outcome, which is clearly accounted for in the MMRI-R. As frailty has no consistent definition, we believe the MMRI-R may serve as a screening tool for frailty that can be easily implemented. With that said, we do not advocate the MMRI-R score as a deciding factor in including or excluding surgical candidates. Rather, it offers potential as a standardized tool to be used to preoperatively identify frail patients who are at increased risk for adverse postoperative outcomes.
We recognize several limitations in our study. Being a retrospective review, there are obvious inherent assumptions explained in the methodology that limit the strength of the study. Additionally, our sample size was small, limited to 47 patients. All patients presented with acute hip fracture so the external validity or generalizability to other populations remains to be seen. The majority of our patients were white males in the Veterans health care system. Therefore, the potential for gender, racial, and system bias clearly is present and our results are likely not representative of a more diverse population. Clearly, this study is primarily exploratory in nature and requires further investigation to validate the utility of questionnaire screening tools prospectively in a surgical population.
Conclusion
In summary, we believe that the MMRI-R has potential to identify those patients at increased risk for postoperative mortality. The questionnaire has the ability to be performed rapidly and may give additional information regarding postsurgical outcome to providers and patients. Based on this exploratory study and the current literature, initiation of studies to assess the ability of frailty and mortality indices in hip fracture and other populations to assist in preoperative decision making should be undertaken.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003;27(1):11–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378(9800):1408–1413 [DOI] [PubMed] [Google Scholar]
- 3. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363(8):733–742 [DOI] [PubMed] [Google Scholar]
- 4. Hossain M, Neelanala V, Andrew JG. Results of non-operative treatment following hip fracture compared to surgical intervention. Injury. 2009;40(4):418–421. doi:10.1016/j.injury.2008.10.001 [DOI] [PubMed] [Google Scholar]
- 5. Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676–685 [DOI] [PubMed] [Google Scholar]
- 6. Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–908 [DOI] [PubMed] [Google Scholar]
- 7. Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Med Sci. 2004;59(3):255–263 [DOI] [PubMed] [Google Scholar]
- 8. Porock D, Parker-Oliver D, Petroski GF, Rantz M. The MDS mortality risk index: the evolution of a method for predicting 6-month mortality in nursing home residents. BMC Research Notes. 2010;3:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808 [DOI] [PubMed] [Google Scholar]
- 10. Partridge J, Harari D, Dhesi J. Frailty in the older surgical patient: a review. Age Ageing. 2012;41(2):142–147 [DOI] [PubMed] [Google Scholar]
- 11. Robinson TN, Wu DS, Steigmann GV, Moss M. Frailty predicts increased hospital and six-month healthcare cost following colorectal surgery in older adults. Am J Surg. 2011;202(5):511–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Holvik K, Ranhoff AH, Martinsen MI, Solheim LF. Predictors of mortality in older hip fracture inpatients admitted to an orthogeriatric unit in Oslo, Norway. J Aging Health. 2010;22(8):1114–1131 [DOI] [PubMed] [Google Scholar]
- 13. Jones TS, Wu DS, Robinson TN. Who would have thought? Asking an older adult if they have fallen predicts surgical outcomes. J Am Coll Surg. 2012;215(3):S56 [Google Scholar]