The 2014 Canadian Hypertension Education Program (CHEP) recommendations for the diagnosis and management of hypertension1 represent the 15th annual iteration of these evidence-based guidelines. Since 1999, CHEP and Hypertension Canada have undertaken numerous knowledge translation initiatives to raise awareness and improve the level of hypertension control across the country, and these guidelines represent one key strategy. Pharmacists are a key audience for the CHEP guidelines, as pharmacist care has been conclusively demonstrated to improve outcomes in people with hypertension.2-4
In 2011, we published a complete set of CHEP guidelines specific to the needs of pharmacists5 and an update paper outlining the changes since those guidelines was published in this journal last year.6 The purpose of this article is to highlight the changes made in the 2014 version of the guidelines and their supporting evidence. Therefore, readers are encouraged to interpret this update in conjunction with those previous publications, available on the Canadian Pharmacists Journal website at www.cpjournal.ca, as well as the full guidelines at www.hypertension.ca. Additional information on sodium reduction efforts, health policy considerations and adherence recommendations can be found on the Hypertension Canada website.
Threshold for initiating drug therapy in the very elderly
The 2013 guidelines introduced a specific systolic blood pressure (BP) target, of <150 mmHg, for the very elderly (defined as those 80 years or older) with isolated systolic hypertension. To align with this new target, the 2014 guidelines recommend that the threshold for initiating drug therapy in this population be 160 mmHg systolic, with no diastolic threshold defined. As described in our 2012-2013 update,6 these targets specific to the very elderly were made based on the findings of the HYVET trial.7 In this study, nearly 4000 patients age ≥80 years with sustained systolic BP of >160 mmHg were randomized to either placebo or indapamide 1.5 mg daily, with the option of also adding perindopril 2 to 4 mg daily with the goal of attaining a target BP of <150/80 mmHg. The study was stopped early when significant reductions in all-cause mortality were observed in the treatment group (mean BP achieved of 144/77 mmHg) compared with the placebo group (mean BP 158/84 mmHg). Statistically significant improvements were also noted for heart failure and major cardiovascular events, with a trend for a reduction in fatal and nonfatal stroke.
Given concerns with precipitating adverse effects related to BP lowering in this population, particularly among those who are frail, clinicians are reminded that any decisions related to initiation or intensification of drug therapy in the very elderly should be made following an individual risk-benefit analysis. Readers are also reminded that those patients enrolled in the HYVET study were relatively healthy, and nearly two-thirds had already received treatment for hypertension. Therefore, treatment decisions for frailer patients or incident cases may require additional considerations when deciding on whether to initiate drug therapy.
Caution in lowering diastolic BP to <60 mmHg in coronary artery disease
It is generally observed that lower BP is associated with lower cardiovascular event risk.8 However, an early report9 from the Framingham study found a J-shaped relationship between diastolic BP and coronary death in patients with a history of myocardial infarction (MI), although this relationship was not observed among those without a previous MI, or for systolic BP. This relationship was determined to be independent of a number of clinical factors, including pre-MI diastolic BP, use of antihypertensive drugs, left ventricular function and serum cholesterol, or demographic factors including age, diabetes status, smoking status, hematocrit or weight.
It has been proposed that this J-curve relationship may be the result of hypoperfusion of cardiac tissue during diastole in patients with coronary artery stenosis. This leads to myocardial ischemia, since the coronary arteries are perfused during diastole.10,11 The myocardial perfusion pressure (MPP) during diastole, defined as the difference between the aortic diastolic pressure and the right atrial pressure, can therefore be measured to examine the relationship between blood pressure reduction and the effect on MPP. A 2013 study12 was designed specifically to examine this relationship, with the goal of informing treatment targets. This observational study followed a consecutive sample of 101 patients visiting a cardiac catheterization laboratory for the assessment of coronary artery disease, excluding those presenting with an acute MI. The study found a significant linear relationship between aortic diastolic BP and MPP. Considering that an MPP of 50 mmHg approximates zero blood flow in patients with hypertension, 1.6% of patients with diastolic BP of 75 mmHg or greater were at this threshold, increasing to 16% of those with diastolic BP of 65 mmHg and over 50% among those with diastolic BP of 60 mmHg. The same relationship between diastolic BP and MPP was seen among patients with diabetes regardless of their hypertension status.
Given the significant linear relationship observed in this study between diastolic BP and risk of hypoperfusion, the 2014 guidelines advise caution in lowering diastolic BP to ≤60 mmHg among patients with established coronary artery disease. This recommendation has been assigned a Grade D level of evidence due to the observational nature of this single study, potential sources of confounding that have not yet been accounted for, such as baseline risk or comorbidities, and observed J-curves among placebo groups or those with little change in blood pressure treatment in other studies.
Additional evidence supporting reduced sodium intake for hypertensive patients
A Cochrane systematic review and meta-analysis published in 2013 provided additional evidence supporting public health recommendations for sustained modest reductions in sodium intake.13 To be included, trials had to randomize subjects to either moderately reduced salt intake or usual salt intake for a minimum of 4 weeks, no concomi-tant interventions (both nonpharmacological or pharmacological) could be provided to either group and the reduction in 24-hour urinary sodium observed had to be 40 to 120 mmol, which is equivalent to a daily salt reduction of 2.3 to 7.0 g. Studies were excluded if the subjects included children, pregnant women or those with medical conditions other than hypertension (e.g., heart failure or diabetes). The study prespecified subgroup analyses for hypertensive versus nonhypertensive subjects.
Of the 34 trials identified, 22 trials involving 999 participants were conducted in hypertensives. The median age of subjects was 50 years, and usual salt intake was estimated at 9.5 g/day and median BP was 148/93 mmHg. Subjects randomized to reduced salt intake had a mean intake reduction of 4.4 g/day and systolic and diastolic BP reductions of 5.4 and 2.8 mmHg, respectively (p < 0.001 for both). This relationship was found to be dose-dependent, with greater sodium reduction associated with greater blood pressure reduction. These results are clinically significant at both the individual and population level and support efforts by CHEP and health professionals to advocate for reduced sodium intake. This is relevant for pharmacists, as many pharmacies also sell packaged foods and snacks that are high in sodium.
Glycated hemoglobin (A1c) added as an option in routine laboratory investigations
Glycated hemoglobin (A1c) has been added to the list of routine laboratory tests as part of preliminary investigations for patients with hypertension. This is consistent with the Canadian Diabetes Association 2013 Clinical Practice Guidelines, which state that screening for type 2 diabetes can be done through the use of fasting plasma glucose (FPG) and/or glycated hemoglobin (A1c).14
This recommendation stemmed from the results of a systematic review15 suggesting that fasting glucose and A1c have similar sensitivity and specificity in the detection of diabetes. Furthermore, a study on over 2000 adults at high risk of diabetes found the sensitivity and specificity of A1c and fasting glucose to be virtually identical at threshold values of 6.1% and 6.1 mmol/L, respectively.16 When both tests were combined, the sensitivity and specificity was found to increase to over 96%.
Use of low-dose ASA for primary prevention
The 2014 guidelines revised the recommendation regarding the use of low-dose acetylsalicylic acid (ASA) (defined as 80-81 mg daily) therapy for primary prevention by narrowing the target population from all controlled hypertensive patients to only those 50 years or older. This recommendation was made to be more consistent with the population enrolled in the Hypertension Optimal Trial (HOT) upon which the recommendation is based. HOT randomized 18,780 patients aged 50 to 80 years with a diastolic BP of 100 to 115 mmHg to 1 of 3 diastolic targets (≤90, ≤85 or ≤80 mmHg) and to ASA or placebo. In this study, with a mean follow-up of 3.8 years, ASA therapy was found to reduce the incidence of major cardiovascular events from 10.5% to 8.9% (p = 0.03).17 The change in target population age also considered the benefits of ASA in the prevention of cancer18 and risk of ASA-associated bleeding.19 This recommendation is consistent with those of other organizations that have modeled the benefits versus risks of low-dose ASA therapy across various age groups.18,20
However, when silent myocardial infarctions were included in the composite end point of major cardiovascular events in HOT, the results were found to be inconclusive. Upon re-review, it is unclear if silent infarctions were specified a priori as a component of this composite end point. Because of this uncertainty, this recommendation has also been downgraded from a Grade A to a Grade B.
Other CHEP initiatives of interest to Canadian pharmacists
PEPonline: The Société québécoise d’hypertension artérielle (SQHA) and Hypertension Canada now offer a Professional Education Program online training course (PEPonline). This 15-hour online course for Canadian health professionals is divided into multiple sessions discussing the pathogenesis of hypertension, assessment of blood pressure and cardiovascular risk, pharmacotherapy, lifestyle modification and patient adherence. At the end of the program, participants will receive a certificate of completion. In addition, a pharmacist-specific Hypertension Provider Certification program is planned using the PEPonline program as a base. Pharmacists interested in this program can register and find additional information at https://hypertension.ca/en/professional/pep-online.
CHEP Recommendations on the Go: The complete CHEP recommendations are also available as a free app for iPhone and iPad devices through iTunes (https://itunes.apple.com/ca/app/chep-canadian-hypertension/id467972468?mt=8) and for Android devices through Google Play (https://play.google.com/store/apps/details?id=com.medbrane.chep).
Conclusion
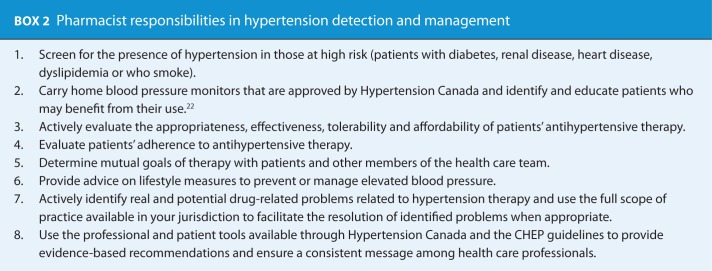
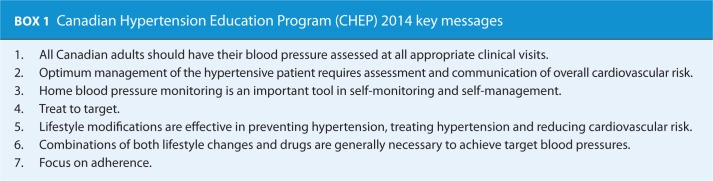
Canada currently has one of the highest rates of blood pressure awareness and control worldwide, but with approximately one-third of patients receiving treatment for hypertension remaining uncontrolled and nearly 1 in 5 Canadians with high blood pressure unaware of their condition,21 pharmacists have the skills, resources and, importantly, the opportunity to further improve the detection and management of patients with hypertension. In order to do so, pharmacists need to be aware of changes made to the annual guidelines in light of new evidence. A summary of the changes to the CHEP guidelines in 2014 is provided in Table 1. In addition to these changes, the 7 key points highlighted by CHEP in 2014 are provided in Box 1, and guidance on the role of pharmacists in hypertension management is provided in Box 2.
Table 1.
Summary of updates to the 2014 Canadian Hypertension Education Program (CHEP) guidelines
| CHEP 2013 | CHEP 2014* |
|---|---|
| Routine and optional laboratory tests for the investigation of patients with hypertension | |
| Fasting blood glucose (Grade D) | Fasting blood glucose and/or glycated hemoglobin (A1c) (Grade D) |
| Global vascular protection therapy for adults with hypertension without compelling indications for specific agents | |
| Strong consideration should be given to the addition of low-dose ASA therapy in hypertensive patients (Grade A in patients older than 50 years). Caution should be exercised if blood pressure is not controlled (Grade C). | Consideration should be given to the addition of low-dose ASA therapy in hypertensive patients ≥50 years (Grade B). Caution should be exercised if blood pressure is not controlled (Grade C). |
| Health behaviour management | |
| For prevention and treatment of hypertension, a dietary sodium intake of 1500 mg (65 mmol) per day is recommended for adults 50 years or younger, 1300 mg (57 mmol) per day if age 51 to 70 years and 1200 mg (52 mmol) per day if older than 70 years (Grade B). | To decrease blood pressure, consider reducing sodium intake towards 2000 mg (5 g of salt or 87 mmol of sodium) per day (Grade A). |
| Choice of therapy for adults with hypertension without compelling indications for specific agents | |
| Recommendations for hypertensive patients with coronary artery disease: 5) In high-risk patients, when combination therapy is being used, choices should be individualized. The combination of an ACE inhibitor and a dihydropyridine CCB is preferable to an ACE inhibitor and a diuretic in selected patients (Grade A). |
Recommendations for hypertensive patients with coronary artery disease: 5) In high-risk patients, when combination therapy is being used, choices should be individualized. The combination of an ACE inhibitor and a dihydropyridine CCB is preferable to an ACE inhibitor and a diuretic in selected patients (Grade A). 6) When lowering SBP to target levels in patients with established CAD (especially if ISH is present), be cautious when the diastolic blood pressure is ≤60 mmHg because of concerns that myocardial ischemia may be exacerbated (Grade D). |
| Recommendations for individuals with isolated systolic hypertension 6) In the very elderly (80 years and older), the target for SBP should be <150 mmHg (Grade C). |
Recommendations for individuals with isolated systolic hypertension 6) In the very elderly (80 years and older), who do not have diabetes or target organ damage, the SBP threshold for initiating drug therapy is ≥160 mmHg and the SBP target is <150 mmHg (Grade C). |
ACE, angiotensin-converting enzyme; ASA, acetylsalicylic acid; CCB, calcium channel blocker; ISH, isolated systolic hypertension; SBP, systolic blood pressure. *Bold text represents changes to the 2014 guidelines from the 2013 guidelines.
The full hypertension guidelines are now available on the Hypertension Canada website (www.hypertension.ca) and will also be published in the Canadian Journal of Cardiology. Pharmacists are also encouraged to become familiar with the many resources available on the Hypertension Canada website for use in providing evidence-based care for patients with hypertension. ■
Footnotes
Author Contributions:S. Houle, R. Padwal and L. Poirier drafted the manuscript. All authors reviewed, edited and approved the final version of the manuscript.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Dr. Tsuyuki did not participate in the peer review of this article.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hypertension Canada. Canadian Hypertension Education Program (CHEP) 2014. Recommendations. Available: www.hypertension.ca/en/chep (accessed April 7, 2014).
- 2. Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care 2010;48:923-33. [DOI] [PubMed] [Google Scholar]
- 3. Santschi V, Chiolero A, Burnand B, et al. Impact of pharmacist care in the management of cardiovascular disease risk factors: s systematic review and meta-analysis of randomized trials. Arch Intern Med 2011;171:1441-53. [DOI] [PubMed] [Google Scholar]
- 4. Santschi V, Chiolero A, Paradis G, et al. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care 2012;35:2706-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Houle SKD, Tsuyuki RT, Campbell NRC. The Canadian Hypertension Education Program (CHEP) 2011 guidelines for pharmacists. Can Pharm J (Ott) 2011;144:295-304. [Google Scholar]
- 6. Houle SKD, Padwal R, Tsuyuki RT. The 2012-2013 Canadian Hypertension Education Program (CHEP) guidelines for pharmacists: an update. Can Pharm J (Ott) 2013;146:146-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Beckett NS, Peters R, Fletcher AE, et al. , for the HYVET study group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887-98. [DOI] [PubMed] [Google Scholar]
- 8. Lewington S, Clarke R, Qizilbash N, et al. ; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360(9349):1903-13. [DOI] [PubMed] [Google Scholar]
- 9. D’Agostino RB, Belanger AJ, Kannel WB, Cruickshank JM. Relation of low diastolic blood pressure to coronary heart disease death in presence of myocardial infarction: the Framingham Study. BMJ 1991;303:385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cruickshank JM. Clinical importance of coronary perfusion pressure in the hypertensive patient with left ventricular hypertrophy. Cardiology 1992;81:283-90. [DOI] [PubMed] [Google Scholar]
- 11. Messerli FH, Panjrath GS. The J-curve between blood pressure and coronary artery disease or essential hypertension: exactly how essential? J Am Coll Cardiol 2009; 54:1827-34. [DOI] [PubMed] [Google Scholar]
- 12. Rabkin SW, Waheed A, Poulter RS, Wood D. Myocardial perfusion pressure in patients with hypertension and coronary artery disease: implications for DBP targets in hypertension management. J Hypertens 2013;31:975-82. [DOI] [PubMed] [Google Scholar]
- 13. He FJ, Li J, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 14. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2013 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes 2013;37(suppl 1):S1-S212. [DOI] [PubMed] [Google Scholar]
- 15. Bennett CM, Guo M, Dharmage SC. HbA(1c) as a screening tool for detection of type 2 diabetes: a systematic review. Diabet Med 2007;24:333-43. [DOI] [PubMed] [Google Scholar]
- 16. Hu Y, Liu W, Chen Y, et al. Combined use of fasting plasma glucose and glycated hemoglobin A1c in the screening of diabetes and impaired glucose tolerance. Acta Diabetol 2010;47:231-6. [DOI] [PubMed] [Google Scholar]
- 17. Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial. Lancet 1998;351:1755-62. [DOI] [PubMed] [Google Scholar]
- 18. Calonge N, Petitti DB, DeWitt TG, Gordis L. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2009;150:396-404. [DOI] [PubMed] [Google Scholar]
- 19. Rothwell PM, Fowkes FG, Belch JF, et al. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet 2011;377(9759):31-41. [DOI] [PubMed] [Google Scholar]
- 20. Vandvik PO, Lincoff AM, Gore JM, et al. Primary and secondary prevention of cardiovascular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(2 Suppl):e637S-e668S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McAlister FA, Wilkins K, Joffres M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ 2011;183:1007-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Houle SKD, Campbell NRC, Tsuyuki RT. Home blood pressure monitoring plays a key role in hypertension management: review of applications, effectiveness and technique for pharmacists. Can Pharm J (Ott) 2011;141:18-20. [Google Scholar]