Abstract
Objective:
To determine the demographic and health care characteristics of elderly family health team patients who are frequent emergency department (ED) users, focusing on potentially inappropriate medications (PIMs) and access to primary care services.
Design:
Cross-sectional retrospective chart review.
Setting:
Academic family medicine clinic in Toronto, Ontario.
Participants:
A total of 46 elderly patients (age >65 years) with 4 or more visits to a University Health Network–affiliated ED between April 1, 2010, and March 31, 2011.
Main outcome measures:
Using the validated STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions) criteria, PIMs were identified. The primary objective was to determine whether PIMs were associated with more frequent ED use. The secondary objective was to determine whether patients who had previously undergone a clinic pharmacist-led medication review had fewer PIMs. We also determined the health characteristics of these patients at the time of their last ED visit of the study period. Utilization of primary care resources, both prior to and after ED visits, was determined.
Results:
Sixty-five percent of patients were taking at least 1 PIM. The total number of PIMs in the study population was 71. Having more PIMs was significantly correlated with a higher number of ED visits (r = 0.32, p < 0.05). Patients with a previous medication review had a similar number of PIMs compared with those without a review. The mean number of concurrent medications was 12.1 and the mean Charlson Comorbidity Index score was 3.7. Significant delay between hospital discharge and primary care follow-up (median 13 days) was observed.
Conclusion:
Elderly patients who are more frequent ED users have a greater number of PIMs. Primary care resources appear to be underused in this population.
Knowledge into Practice.
Polypharmacy is highly prevalent in the population of elderly patients with frequent emergency department (ED) visits. There is a significant correlation between the number of potentially inappropriate medications (PIMs), as per the STOPP criteria, and the number of ED visits.
Pharmacists are ideally situated to help reduce PIM use in this population. Pharmacists should use validated tools, such as the STOPP criteria, to guide medication reviews and provide evidence-based drug therapy recommendations to prescribers.
This population underuses alternative levels of care (e.g., “same-day” appointments, urgent care clinics). Pharmacists can be effective patient educators on when and how to access different levels of care.
Mise En Pratique Des Connaissances.
La prévalence de la polypharmacie est très élevée chez les personnes âgées qui fréquentent souvent le service d’urgence. Or il existe une importante corrélation entre le nombre de médicaments potentiellement inappropriés, selon les critères STOPP, et le nombre de visites au service d’urgence.
Les pharmaciens sont dans une position idéale pour aider à réduire l’usage des médicaments potentiellement inappropriés dans cette population. Les pharmaciens devraient utiliser des outils valides, comme les critères STOPP, pour orienter la revue des médicaments et formuler des recommandations pharmacothérapeutiques fondées sur des données probantes à l’intention des médecins prescripteurs.
Cette population sous-utilise les autres niveaux de soins, comme les cliniques offrant des rendez-vous le jour même et les cliniques de soins d’urgence. Les pharmaciens peuvent jouer un rôle d’éducation efficace auprès de ces patients en leur indiquant quand et comment utiliser les différents niveaux de soins.
Introduction
Canadians were found to be the most frequent users of emergency departments (EDs) in an 11-country comparison.1 From 2005 to 2006, Canada spent a total of 1.8 billion dollars on EDs.2 In an effort to improve the appropriate utilization of these departments, researchers have been devoting more resources into studying factors associated with frequent ED visits.3
Frequent users of the ED contribute to a disproportionate number of visits. Unfortunately, no standard definition of “frequent use” exists, although most studies have used a definition of 4 or more ED visits per year.4 A systematic review of ED literature determined that these frequent users represent 4.5% to 8% of all ED patients but contribute to 21% to 28% of all visits.4 Age older than 65 years and polypharmacy are 2 important risk factors associated with frequent ED use.4-7
A recent Canadian study found that 12% of ED visits to a large tertiary hospital were drug related and 68% of those were deemed to have been preventable.8 Several tools, such as the validated Screening Tool of Older Persons’ potentially inappropriate Prescriptions (STOPP) criteria, have been created to help front-line clinicians identify potentially inappropriate medication use in the elderly.9,10 STOPP lists 65 clinically significant criteria for inappropriate prescribing in the elderly.9
Unlike the Beers criteria,11 a checklist developed to help clinicians identify potentially inappropriate medication use in older adults, the medications included in the STOPP criteria have been consistently associated with an increased risk of hospitalization in elderly patients.12,13 Of note, at the time of this study, the updated 2012 Beers criteria had not been published.14 One prospective study found that 62.2% of drug-related events that led to ED presentation and urgent hospitalization were listed in the STOPP criteria.12
A review of the literature reveals several classes of medications that have been consistently associated with an increased risk for adverse drug reactions and ED usage, even when they are not used under clinical scenarios that would designate them as potentially inappropriate medications as per STOPP criteria. For this reason, these classes of medications, such as antipsychotics and benzodiazepines, can be considered “high risk” in the elderly population.8,15,16
This pilot study aims to describe the health care characteristics and the prevalence of potentially inappropriate medications (PIMs), as described by the STOPP criteria, in the elderly population who are frequent ED users. Our primary objective was to determine whether taking a higher number of STOPP criteria PIMs is a risk factor for increased ED usage in this population.
Methods
Site and study subjects
This was a cross-sectional retrospective chart review at an interprofessional, primary care clinic that serves approximately 14,000 patients and is located within a tertiary-level hospital. This clinic includes 3 primary care pharmacists, who were the main developers and operators of this study. This site is an academic teaching site for family medicine residents and health professional trainees, including 1 pharmacy resident per year. The study received the hospital’s Research Ethics Board approval.
The hospital’s electronic medical record was used to identify eligible subjects between April 1, 2010, and March 31, 2011. Patients were eligible for inclusion if they met the following criteria during this time period: ≥4 visits to an ED associated with the hospital network, ≥65 years old at the time of their most recent ED visit and rostered with a physician located in our clinic.
Data collection
Data were gathered using a standardized data collection form that was validated internally by having 3 separate investigators trial the form, ensuring consistency. Sources of data included both the hospital’s electronic medical record and our clinic’s health records. Only data from the patient’s last ED visit of the year were collected, since our primary objective was to determine the health care characteristics of this patient population, not to track their progress within that year.
The data collected included specifics of the patient’s ED visit, basic demographics, health care utilization, best possible medication list, comorbidities and pertinent physical assessment and laboratory values. Discrepancies between data sources were few in number, but all were discussed thoroughly between authors JW, PM and DK until consensus was obtained. The STOPP criteria were used to identify PIMS. Of note, medications that fulfilled more than 1 STOPP criterion were counted towards multiple PIMs in our calculations.
To determine the list of medication classes that would be deemed as “high risk,” PubMed and EMBASE databases were searched using the following MESH search terms: “Drug Toxicity,” “Aged” and “Emergency Service, Hospital.” Our research group reviewed the resulting literature and while there is no universally accepted list, we recognized that certain medication classes were frequently associated with ED visits in elderly patients. We refer to these as “high-risk” medications.
Two modifications were made to the validated STOPP criteria to align them with Canadian practice. Glyburide was added to the criterion of “glibenclamide or chlorpropamide with type 2 diabetes mellitus.” The addition of glyburide was justified, as it has been linked to an increased risk of hypoglycemia in the elderly.17,18 Second, the indications of gastroesophageal reflux disease (GERD) and esophagitis were added to the criterion of “proton pump inhibitors (PPIs) for peptic ulcer disease at full therapeutic dosage for >8 weeks.” This falls in line with recommendations from the Canadian Association of Gastroenterology19 and is supported by a landmark study.20
Outcomes
The primary study outcome was to determine the number of PIMs at ED presentation and whether an increased number of PIMs was associated with more frequent ED use in this population. The secondary outcome was the comparison of PIM frequency in patients with previous medication reviews with the clinic pharmacist versus those who had not been seen.
Statistical analysis
Descriptive analyses were performed with SPSS (Statistical Package for the Social Sciences, version 11.0 for Windows; SPSS, Inc., an IBM Company, Chicago, IL). Pearson correlations (r) were calculated to measure associations between patient demographics, health care characteristics, ED usage and number of PIMs. Statistical significance was prespecified by a p < 0.05.
A Welch t-test was used to compare whether patients who received a medication review from a clinic pharmacist had fewer PIMs compared with patients who had not.
Results
Demographics
Forty-six patients met the inclusion criteria and had a combined total of 284 ED visits in the study period. The mean (SD) age was 76.3 (6.6) years and 50% were female (Table 1). Median number of ED visits was 6 (Figure 1).
Table 1.
Demographics at the time of last emergency department (ED) visit (n = 46)
| Characteristics | Value |
|---|---|
| Sex, n (%) | |
| Male | 23 (50) |
| Female | 23 (50) |
| Age, mean (SD), y | 76.3 (6.6) |
| Age group in years, n (%) | |
| 65-74 | 18 (39.1) |
| 75-84 | 24 (52.2) |
| ≥85 | 4 (8.7) |
| Days since last ED visit | |
| Mean (SD) | 61.5 (67.1) |
| Median | 37.5 |
| Time of ED registration, n (%) | |
| During regular clinic hours* | 27 (58.7) |
| After regular clinic hours | 19 (41.3) |
| Number of medications† | |
| Mean (SD) | 12.1 (5.8) |
| Range | 1-27 |
| Charlson Comorbidity Index score‡ | |
| Mean (SD) | 3.7 (2.6) |
| Range | 0-12 |
Regular clinic hours (Monday, Tuesday, and Thursday, 0900-2000; Wednesday, 1330-2000; Friday, 830-1630; Saturday, 0900-1300).
Includes all prescription, over-the-counter and complementary medicines.
The Charlson Comorbidity Index score was calculated using 1 point for history of myocardial infarction, peripheral vascular disease, past stroke or transient ischemic attack, or diabetes without complications; 2 points for heart failure, chronic pulmonary disease, mild liver disease, nonmetastatic cancer within the past 5 years, or diabetes with end-organ damage; 3 points for dementia or mild cognitive impairment, or connective tissue disease; 4 points for moderate to severe liver disease or human immunodeficiency virus infection; and 6 points for metastatic cancer.
Figure 1.
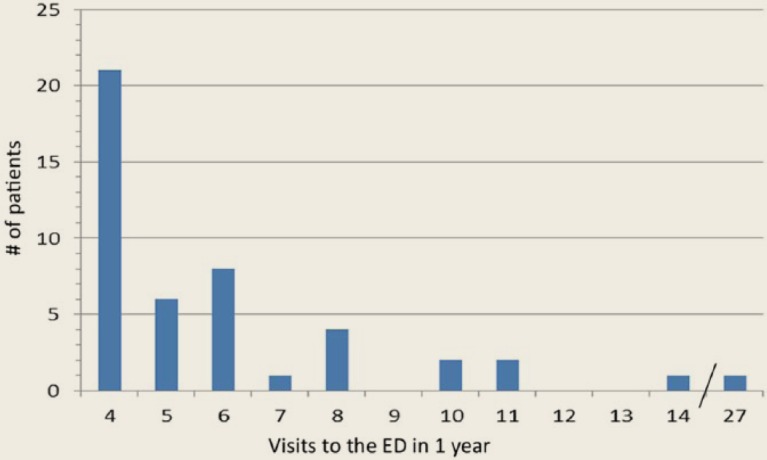
Frequency of emergency department (ED) visits
Almost one-quarter (23.9%) of patients were admitted as inpatients. More than half had a Canadian Triage and Acuity Scale (CTAS) score of 3 (urgent). The CTAS score is used by ED personnel to triage patients by the acuity of their presenting symptoms.21 Mean (SD) number of medications recorded was 12.1 (5.8), which included both scheduled medications and those taken on an as-needed basis (Table 1). The mean (SD) Charlson Comorbidity Index score was 3.7 (2.6) out of a possible 29 (Table 1). This prognostic index provides a weighted score based on a predefined list of comorbid conditions that quantifies a patient’s prognosis. A patient’s number of medications and Charlson Comorbidity Index score were both positively correlated with a higher acuity of ED visit (Pearson r = −0.30, p < 0.05 and Pearson r = −0.42, p < 0.01, respectively).
During the 1-year period prior to their last ED visit, patients had a mean (SD) number of 5.6 (3.9) visits with their primary care provider. When considering all visits to the clinic (i.e., with other physicians, nurses, pharmacists or allied health care workers), the mean (SD) number of visits increased to 10.4 (8.6). Only 9 patients (19.6%) had a medication review with a clinic pharmacist.
After patients were discharged from hospital, 9 patients (19.6%) did not make an appointment with a primary care provider within 1 year; 2 patients (4.3%) died. Of the remaining 35 patients, it took a median of 13 days for patients to see a physician or nurse practitioner. Patients with fewer primary care visits during the study period took longer to book a primary care follow-up appointment after their ED visit (Pearson r = −0.43, p = 0.01).
Potentially inappropriate medications (PIMs)
Using the STOPP criteria, we identified 71 PIMs in our patient population at the time of their ED presentation. Table 2 lists the top 10 most frequently prescribed PIMs. Two-thirds of patients were taking 1 or more STOPP criteria PIMs at the time of ED presentation. Of these patients, 43% were taking 1 PIM, 23% were taking 2 PIMs and the rest were taking 3 or more. Use of proton pump inhibitors (PPIs) at full therapeutic doses for >8 weeks was the most common PIM identified. The 5 medications that were responsible for the greatest number of potential drug therapy problems were acetylsalicylic acid (ASA) (26.1%), PPIs (21.7%), opioids (15.2%), calcium channel blockers (14.3%) and warfarin (14.3%). Patients who had had a medication review with a pharmacist were not taking fewer inappropriate medications (t [10] = 0.87, p = 0.41). The number of PIMs was the only factor that significantly correlated with the number of ED visits (Pearson r = 0.32, p < 0.05).
Table 2.
Most frequently prescribed potentially inappropriate medications as per the Screening Tool of Older Persons’ potentially inappropriate Prescriptions (STOPP) criteria9
| Potentially inappropriate medications listed in STOPP | n (%) | % of all potentially inappropriate medications identified |
|---|---|---|
| Proton pump inhibitors for peptic ulcer disease, esophagitis or gastroesophageal reflux disease at full therapeutic dosage for >8 weeks | 10 (21.7) | 14.1 |
| Calcium channel blockers with chronic constipation | 6 (13.0) | 8.5 |
| Aspirin with no history of coronary, cerebral or peripheral vascular symptoms or occlusive event | 4 (8.7) | 5.6 |
| Use of aspirin and warfarin in combination without histamine H2-receptor antagonist or proton pump inhibitor | 4 (8.7) | 5.6 |
| Tricyclic antidepressants with an opiate or calcium channel blocker | 4 (8.7) | 5.6 |
| Aspirin at doses >150 mg/day | 3 (6.5) | 4.2 |
| Alpha-blockers in males with frequent incontinence (i.e., 1 or more episodes of incontinence daily) | 3 (6.5) | 4.2 |
| Neuroleptic drugs in those with recurrent falls (≥1 fall in past 3 months) | 3 (6.5) | 4.2 |
| Long-term opiates in those with recurrent falls (≥1 fall in past 3 months) | 3 (6.5) | 4.2 |
| Any duplicate drug class prescription | 3 (6.5) | 4.2 |
High-risk medications were frequently used in the study population, with antiplatelet agents being the most common (Figure 2). High-risk medications were documented to be the direct cause of 3 (6.5%) ED visits. Two were associated with warfarin (resulting in bleeds) and 1 was associated with nonadherence with furosemide (resulting in heart failure exacerbation).
Figure 2.
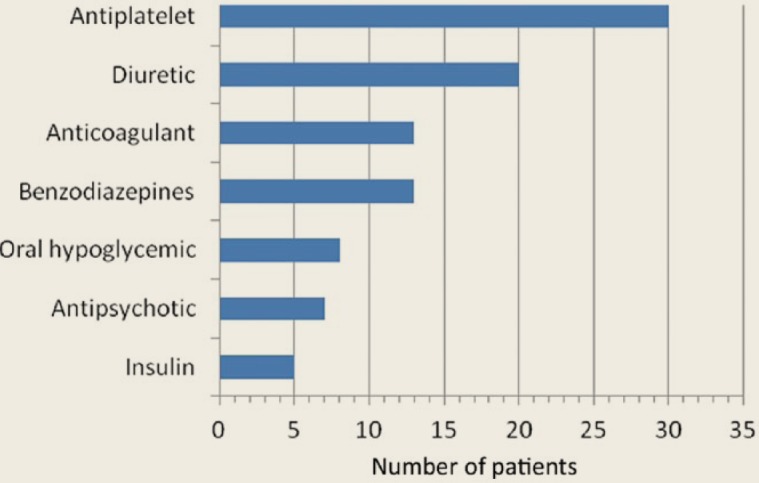
Frequency of high-risk medication usage
Discussion
In this study, it was found that PIMs are highly prevalent in the elderly population with frequent ED visits, with two-thirds of our study population having at least 1 PIM at the time of their ED presentation. Also, it was determined that a higher number of PIMs was positively correlated with more ED visits.
While our study did not find that pharmacist-directed medication reviews led to fewer PIMS in this population, our study was likely too underpowered for this. Previous studies provide evidence that pharmacist involvement leads to improved detection and management of drug therapy problems in the general population.22,23 Future prospective studies are needed to evaluate the impact of pharmacists on reducing ED usage, as well as outcomes more reflective of pharmacist interventions, such as frequency of adverse drug events.24
Polypharmacy, most commonly defined as taking 6 or more medications,25 has been associated with poor health outcomes such as increased risk of adverse drug reactions, hospitalization and nursing home placement.26 Using this definition, polypharmacy was more prevalent in our population (89.1%) compared with the general elderly population that uses ED services (30%-50%).6,27 This is consistent with previous studies that have identified polypharmacy as a risk factor for frequent ED use. Potentially inappropriate medications, use of high-risk medications and multiple comorbidities were also highly prevalent in our study population.
Given that our main finding is that both PIMs and polypharmacy appear to be significant risk factors for frequent ED use, community pharmacists are ideally situated to provide meaningful interventions such as full medication reviews. Unfortunately, 1 Canadian study found that fewer than half of all senior patients have received a medication review where potentially inappropriate prescribing could be identified.7 Fortunately, numerous provinces have recently implemented funding for pharmacist-led medication reviews. The first step for community pharmacists would be the accurate identification of the patients in their practices who are frequent ED users. Appointments for full medication reviews should be booked, preferably during periods of pharmacist overlap. The use of validated tools, such as the STOPP criteria, can help guide the appointment and provide evidence-based recommendations to the patient’s prescribers.
As part of the LACE criteria developed by Canadian researchers, a person’s Charlson Comorbidity Index score is one component of several to help predict risk of early readmission to hospital after discharge.28 LACE is a mnemonic of 4 variables that have been shown to be associated with this outcome: Length of a patient’s inpatient stay (L), his or her Acuity of admission (A), Charlson Comorbidity Index score (C), and Emergency department use in the 6 months prior to admission (E). Unsurprisingly, our results show that elderly patients who are frequent ED users have a large number of concurrent conditions. In the above-mentioned Canadian study, their population of inpatients had an average Charlson Comorbidity Index score of 0.5 compared with a mean score of 3.7 in our study population.8 This indicates that comorbidity burden is likely also an important risk factor for frequent use of the ED. Our study adds to current literature by demonstrating that in elderly patients with frequent ED visits, polypharmacy and a higher Charlson Comorbidity Index score are significantly correlated with ED visits of higher acuity. Based on our results, future development of criteria to identify elderly patients at high risk of frequent ED usage should include both comorbidity burden and number of PIMs.
Interestingly, we observed that 58.7% of study patients visited the ED while our clinic was open and one-quarter of these ED visits were considered less urgent or nonurgent. This suggests that a number of ED visits could have been avoided had patients sought care in our clinic instead. Further education for clinicians and patients on what constitutes the best usage of different levels of care (i.e., primary care vs. emergency care) may be beneficial.
Our study population had fewer visits per year to a primary care provider (5.6 ± 3.9) compared with the Ontario average of 7 for patients ≥65 years old.29 Fewer visits could mean lack of follow-up and regular monitoring of chronic conditions and medications and could ultimately contribute to more ED usage.30
Another concern raised by our study is the long delay (mean 26.4 days, median 13 days) between hospital discharge and a follow-up clinic visit. Almost 20% of the study population did not make an appointment with a physician or nurse practitioner within 1 year of hospital discharge. Interventions to expedite family physician follow-up within 2 weeks of ED discharge have been shown to decrease further ED usage in the general population.31 Improving communication between EDs and primary care providers could be one such intervention to facilitate timely follow-up and improve continuity of care.
Future research at this clinic will focus on medication regimen optimization, improving communication with nearby EDs and improving patient follow-up with their regular primary care provider, especially after ED discharge. A prospectively designed study will determine whether these interventions have the ability to reduce the frequency of potentially inappropriate prescribing and ultimately ensure the more appropriate usage of EDs.
Limitations
While every effort was made to capture all medication use, it is possible that some medications, such as those taken on an as-needed basis and supplements, were not consistently recorded in the charts. We were also unable to determine medication adherence.
Another limitation was the small sample size, since information about visits to external EDs could not be captured. Although these limitations existed, these results effectively represent the experiences of our primary care clinic. Future research could validate our findings by comparing them to similar populations in other primary care settings. Finally, since we did not collect information on PIMs in our patients with infrequent or no ED visits, we cannot demonstrate causation between number of PIMs on more frequent ED visits, only correlation.
Conclusions
Our study showed that potentially inappropriate and other high-risk medications were highly prevalent in the elderly population with frequent ED visits. We also determined that the STOPP criteria are a valuable tool for pharmacists to help identify potentially inappropriate medications in elderly patients, as our study showed that these medications were associated with more frequent ED use. While our study was not adequately powered to show that primary care pharmacists are able to reduce PIMs, we hope it is a starting point for future, larger studies. Furthermore, this patient population appeared to underuse primary care resources, both before and after ED usage. Future research should evaluate interventions aimed at improving primary care follow-up and reducing use of potentially inappropriate medications. ■
Footnotes
Author Contributions:All of the authors conceived the study. Jeffrey Wong drafted the manuscript. All of the authors reviewed, edited and approved the final manuscript.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Health Council of Canada. How do Canadians rate the health care system? Results from the 2010 Commonwealth Fund International Health Policy Survey. Available: www.healthcouncilcanada.ca/tree/2.04-Commonwealth_FINAL_E_Nov2010.pdf (accessed July 5, 2012).
- 2. Dawson H, Zinck G. CIHI Survey: ED spending in Canada: a focus on the cost of patients waiting for access to an in-patient bed in Ontario. Healthc Q 2009;12:25-8. [DOI] [PubMed] [Google Scholar]
- 3. Doupe MB, Palatnick W, Day S, et al. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Ann Emerg Med 2012;60:24-32. [DOI] [PubMed] [Google Scholar]
- 4. LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data and the policy implications. Ann Emerg Med 2010;56:42-8. [DOI] [PubMed] [Google Scholar]
- 5. McMillan RE, Stokes-Lampard H, Large R. What influences recurrent presentations of older people to the emergency department? N Z Med J 2011;124:93-8. [PubMed] [Google Scholar]
- 6. Hohl CM, Dankoff J, Colacone A, et al. Polypharmacy, adverse drug-related events and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med 2001;38:666-71. [DOI] [PubMed] [Google Scholar]
- 7. Reason B, Terner M, Moses McKeag A, et al. The impact of polypharmacy on the health of Canadian seniors. Fam Pract 2012;29:427-32. [DOI] [PubMed] [Google Scholar]
- 8. Zed PJ, Abu-Laban RB, Balen RM, et al. Incidence, severity and preventability of medication-related visits to the emergency department: a prospective study. CMAJ 2008;178:1563-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gallagher P, Ryan C, Byrne S, et al. STOPP (Screening Tool of Older Persons Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008;46:72-83. [DOI] [PubMed] [Google Scholar]
- 10. Ryan C, O’Mahony D, Byrne S. Application of STOPP and START criteria: interrater reliability among pharmacists. Ann Pharmacother 2009;43:1239-44. [DOI] [PubMed] [Google Scholar]
- 11. Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 2003;163:2716-24. [DOI] [PubMed] [Google Scholar]
- 12. Hamilton H, Gallagher P, Ryan C, et al. Potentially inappropriate medications defined by STOPP criteria and the risk of adverse drug events in older hospitalized patients. Arch Intern Med 2011;171:1013-9. [DOI] [PubMed] [Google Scholar]
- 13. Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers’ criteria. Age Ageing 2008;37:673-9. [DOI] [PubMed] [Google Scholar]
- 14. American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012;60:616-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Budnitz DS, Pollock DA, Weidenbach KN, et al. National surveillance of emergency department visits for outpatient adverse drug events. JAMA 2006;296:1858-66. [DOI] [PubMed] [Google Scholar]
- 16. Budnitz DS, Lovegrove MC, Shehab N, et al. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365:2002-12. [DOI] [PubMed] [Google Scholar]
- 17. van Staa T, Abenhaim L, Monette J. Rates of hypoglycemia in users of sulfonylureas. J Clin Epidemiol. 1997;50:735-41. [DOI] [PubMed] [Google Scholar]
- 18. Deusenberry CM, Coley KC, Korytkowski MT, et al. Hypoglycemia in hospitalized patients treated with sulfonylureas. Pharmacotherapy 2012;32:613-7. [DOI] [PubMed] [Google Scholar]
- 19. Armstrong D, Marshall JK, Chiba N, et al. Canadian Consensus Conference on the management of gastroesophageal reflux disease in adults—update 2004. Can J Gastroenterol 2005;19:15-35. [DOI] [PubMed] [Google Scholar]
- 20. Vigneri S, Termini R, Leandro G, et al. A comparison of five maintenance therapies for reflux esophagitis. N Engl J Med 1995;333:1106-10. [DOI] [PubMed] [Google Scholar]
- 21. Bullard MJ, Unger B, Spence J, et al. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) adult guidelines. CJEM 2008;10:136-51. [DOI] [PubMed] [Google Scholar]
- 22. Elliott RA, Martinac G, Campbell S, et al. Pharmacist-led medication review to identify medication-related problems in older people referred to an aged care assessment team: a randomized comparative study. Drugs Aging 2012;29:593-605. [DOI] [PubMed] [Google Scholar]
- 23. McKinnon A, Jorgenson D. Pharmacist and physician collaborative prescribing: for medication renewals within a primary health centre. Can Fam Physician 2009;55:e86-91. [PMC free article] [PubMed] [Google Scholar]
- 24. Kaur S, Mitchell G, Vitetta L, et al. Interventions that can reduce inappropriate prescribing in the elderly: a systematic review. Drugs Aging 2009;26:1013-28. [DOI] [PubMed] [Google Scholar]
- 25. Bushardt RL, Massey EB, Simpson TW, et al. Polypharmacy: misleading, but manageable. Clin Interv Aging 2008;3:383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Frazier SC. Health outcomes and polypharmacy in elderly individuals: an integrated literature review. J Gerontol Nurs 2005;31:4-11. [DOI] [PubMed] [Google Scholar]
- 27. Banerjee A, Mbamalu D, Ebrahimi S, et al. The prevalence of polypharmacy in elderly attenders to an emergency department—a problem with a need for an effective solution. Int J Emerg Med 2011;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ 2010;182:551-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chan BTB, Schultz SE. Supply and utilization of general practitioner and family physician services in Ontario. ICES Investigative Report. Toronto (ON): Institute for Clinical Evaluative Sciences; 2005. Available: www.ices.on.ca/file/FP-GP_aug08_FINAL.pdf (accessed August 1, 2012). [Google Scholar]
- 30. Ionescu-Ittu R, McCusker J, Ciampi A, et al. Continuity of primary care and emergency department utilization among elderly people. CMAJ 2007;177:1362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brandon WR, Chambers R. Reducing emergency department visits among high-using patients. J Fam Pract 2003;52:637-40. [PubMed] [Google Scholar]


