Abstract
Background
Definition and diagnosis of constipation remain challenging, partly due to different perceptions of the disease by doctors and patients.
Aim
To evaluate prevalence and features of constipation among individuals seen in general practice, by comparing different diagnostic instruments.
Methods
Standardized questionnaires and the Bristol stool form scale were distributed to all subjects attending 10 general practitioners for any reason in a 2-week period. The questionnaires investigated constipation defined according to: (1) self-perception (yes/no); (2) a visual analogue scale; (3) Rome III Criteria.
Results
The prevalence of constipation in 1306 subjects (790 female, 516 male) resulted: (1) 34% self-reported; (2) 28% by visual analogue scale; (3) 24% by Rome Criteria. Constipation was more frequent in females. A high frequency of symptoms of obstructed defecations was observed with differences among patients with self-reported constipation with or without Bristol stool type 1–2.
Conclusions
Prevalence of constipation among individuals attending their GP ranges between 24 and 34%, according to the different definitions adopted. Symptoms of obstructed defecations are frequent. The combination of self-evaluation and the Bristol stool type scale is potentially useful to identify subgroups of patients with different clinical features in general practice.
Keywords: Constipation, epidemiology, general practice, Rome criteria, questionnaire
Background
Constipation is a common pathological condition characterized by a sensation of impaired defecation.1,2 It has been estimated that constipation affects 12–17% of the general population worldwide, with a higher prevalence among females and elderly people.3–6 Constipation is the main reason for seeing a physician in 1.2% of the US population7 and a significant increase in the proportion of ambulatory care relating to this condition has been observed in the last decade, such that it currently represents the fourth leading referral cause in outpatient clinics.8 The majority of constipated patients, are seen by general practitioners (GPs),2,9 revealing a relevant social and economic burden.2,10,11
The definition and, consequently, the diagnosis of constipation are still challenging. Notwithstanding the introduction of the Rome Criteria for the diagnosis of constipation,1 the perception of the disease by the patient remains a cornerstone in the patient–doctor relationship. Individual perception markedly influences epidemiological and clinical data in the field.3,12–15
The aim of the present study was to evaluate the clinical features of constipation among individuals seeking medical help at the GP level in Italy, according to both subjective and standardized diagnostic criteria.
Methods
This study was designed and carried out in accordance with the Helsinki Declaration (Edinburgh revision, 2000). Data were collected from all adult patients attending 10 GPs distributed throughout Italy (four in the north, two in the centre, four in the south) during a 2-week period. Each patient was requested to complete a structured questionnaire including demographic and anamnestic data as well as a symptom evaluation of constipation, independently of the reasons prompting referrals.
Constipation was evaluated by means of three different methods: (1) direct question: ‘do you consider yourself suffering of constipation?’ (Self-C); (2) visual analogue scale16 10-cm long: position 0 cm, ‘do you feel not at all suffering constipation?’; position 10 cm, ‘do you feel extremely suffering constipation?’ (VAS-C); and (3) Rome III Criteria for constipation1 (Rome-C). Presence of symptoms compatible with irritable bowel symptoms with constipation (IBS-C), was not investigated, since the two conditions are often overlapping16 and a differential diagnosis between IBS-C and chronic constipation was beyond the scope of the present study. The Bristol stool form scale17 was also submitted to all subjects. Office staff assisted the investigated subjects in the comprehension of the questionnaires if needed. Completed questionnaires were collected anonymously in a dedicated box.
A diagnosis of constipation was established on whether the patients answered ‘yes’ to Self-C, and/or scored themselves >2 out of 10 cm in VAS-C,18 and/or scored positive for Rome-C. Patients not fulfilling any of the three criteria were considered not constipated (Not-C). Data were analysed by Chi-squared analysis and multivariate analysis.
Results
During the 2 weeks of the study period, 1460 subjects were seen in 10 participating GP offices and received the questionnaires. Of these, 1306 (89.5%) completed and returned the questionnaire. The study population consisted of 516 males (39.5%) and 790 females (60.5%). Only 128 patients (10.5% of responders; missing data: 7.0%) reported less than three evacuations a week; and 320 reported evacuations with hard stools (25.4%), 824 normal stools (65.4%), and 116 mushy stools (9.2%).
As shown in Figure 1, the frequency of missing data was higher (p = 0.01) when using VAS (15.9%) compared to the Rome Criteria (6.0%) and self-reported criteria (2.9%) and higher (p = 0.01) when using Rome Criteria compared to self-reported criteria, without age differences.
Figure 1.
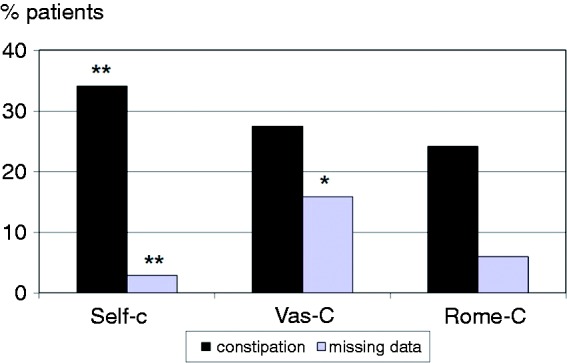
Frequency of constipation and missing data in 1306 patients answering questionnaires on constipation during a GP visit.
Self-C: self-reported constipation (positive answer at the direct question: ‘Do you consider yourself suffering of constipation?’); VAS-C: constipation measured by a visual analogue scale (score >2 out of 10 cm); Rome-C: constipation defined according to the Rome III Criteria
*p = .0.01 vs. Rome-C by chi-squared test.
**p = 0.01 vs. VAS-C and Rome-C by chi-squared test.
The prevalence of constipation differed according the diagnostic method (Figure 1). Self-C was reported by 433 patients (34.1%; 72.5% females), VAS-C by 302 patients (27.5%; 73.8% females), and Rome-C by 298 patients (24.2%; 72.8% females), resulting in a higher prevalence rate for Self-C compared to VAS-C and Rome-C (p = 0.01).
Analysis of demographic data showed that the frequency of constipation was invariably higher (p = 0.01) in females compared to males: 39.8% vs. 22.7% in Self-C patients; 28.2% vs. 15.3% in VAS-C patients; and 26.4% vs. 15.5% in Rome-C patients. Multivariate analysis confirmed a higher prevalence of females in all groups of constipated individuals, as compared to control subjects (Table 1).
Table 1.
Demographic features in 1306 patients answering questionnaires on constipation during a GP visit according to constipation and questionnaire
| Demographic feature | Self-C (n = 433) | VAS-C (n = 302) | Rome-C (n = 298) | Not-C (n = 759) |
|---|---|---|---|---|
| Gender | ||||
| Male | 119 (27.5) | 79 (26.2) | 81 (27.2) | 349 (46.0) |
| Female | 314 (72.5) | 223 (73.8) | 217 (72.8) | 410 (54.0)a |
| Age (years) | ||||
| <55 | 196 (45.5) | 132 (43.7) | 136 (45.6) | 372 (49.2) |
| >55 | 235 (54.5) | 170 (56.3) | 162 (54.4) | 384 (50.8) |
| Total | 431 (100.0) | 302 (100.0) | 298 (100.0) | 756 (100.0) |
| NR | 2 (0.5) | 0 (0.0) | 0 (0.0) | 3 (0.4) |
| School level | ||||
| Low | 262 (61.4) | 190 (63.3) | 189 (64.1) | 440 (59.1) |
| High | 165 (38.6) | 110 (36.7) | 106 (35.9) | 304 (40.9) |
| Total | 427 (100.0) | 300 (100.0) | 295 (100.0) | 744 (100.0) |
| NR | 6 (1.4) | 2 (0.7) | 3 (1.0) | 15 (2.0) |
| Physical activity | ||||
| Light | 343 (81.7) | 244 (83.8) | 239 (84.2) | 489 (70.9) |
| Moderate–high | 77 (18.3) | 47 (16.2) | 45 (15.8) | 201 (29.1) |
| Total | 420 (100.0) | 291 (100.0) | 284 (100.0) | 690 (100.0) |
| NR | 13 (3.0) | 11 (3.6) | 14 (4.7) | 69 (9.0) |
Values are n (%).
Self-C: self-reported constipation (positive answer at the direct question: ‘Do you consider yourself suffering of constipation?’); VAS-C: constipation measured by a visual analogue scale (score >2 out of 10 cm); Rome-C: constipation defined according to the Rome III criteria; Not-C: patients not fulfilling any of the three criteria; NR: not reported.
p = 0.01 vs. Self-C, VAS-C, and Rome C, by multivariate analysis.
Figure 2 shows the prevalence of constipation in different age groups according to different diagnostic techniques. The frequency of constipation was higher (p = 0.04) in older patients (age >65 years) compared to 56–65-year-old group in Self-C and Vas-C patients.
Figure 2.
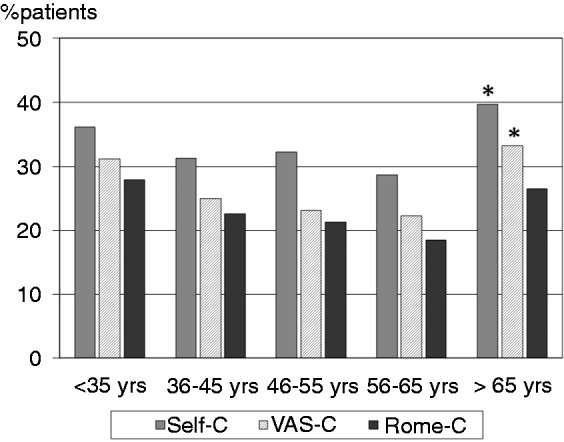
Age group prevalence of constipation in 1306 patients answering questionnaires on constipation during a GP visit.
Self-C: self-reported constipation (positive answer at the direct question: ‘Do you consider yourself suffering of constipation?’); VAS-C: constipation measured by a visual analogue scale (score >2 out of 10 cm); Rome-C: constipation defined according to the Rome III Criteria.
*p = 0.04 vs. 56–65 years by multivariate analysis.
A subgroup classification of Self-C patients was obtained by applying the Bristol Scale: patients with Bristol score 1–2 were defined Bristol positive (Self-C + Bristol), those fulfilling criteria 3–6 Bristol negative (Self-C – Bristol). Table 2 shows that there were no differences in the demographic features among Self-C + Bristol, Self-C – Bristol, and Rome-C patients.
Table 2.
Demographic features of the constipated patients defined according Rome Criteria or self-reported with or without Bristol stool type 1 or 2
| Demographic feature | Self-C (n = 433) | Self-C + Bristol (n = 256) | Self-C – Bristol (n = 177) | Rome-C (n = 298) |
|---|---|---|---|---|
| Gender | ||||
| Male | 119 (27.5) | 61 (23.8) | 58 (32.8) | 81 (27.2) |
| Female | 314 (72.5) | 195 (76.2) | 119 (67.2) | 217 (72.8) |
| Age (years) | ||||
| <55 | 196 (45.5) | 118 (46.1) | 78 (44.6) | 136 (45.6) |
| >55 | 235 (54.5) | 138 (53.9) | 97 (55.4) | 162 (54.4) |
| Total | 431 (100.0) | 256 (100.0) | 175 (100.0) | 298 (100.0) |
| NR | 2 (0.5) | 0 (0.0) | 2 (1.1) | 0 (0.0) |
| School level | ||||
| Low | 262 (61.4) | 161 (63.1) | 101 (58.7) | 189 (64.1) |
| High | 165 (38.6) | 94 (36.9) | 71 (41.3) | 106 (35.9) |
| Total | 427 (100.0) | 255 (100.0) | 172 (100.0) | 295 (100.0) |
| NR | 6 (1.4) | 1 (0.4) | 5 (2.8) | 3 (1.0) |
| Physical activity | ||||
| Light | 343 (81.7) | 206 (83.7) | 137 (78.7) | 239 (84.2) |
| Moderate–high | 77 (18.3) | 40 (16.3) | 37 (21.3) | 45 (15.8) |
| Total | 420 (100.0) | 246 (100.0) | 174 (100.0) | 284 (100.0) |
| NR | 13 (3.0) | 10 (3.9) | 3 (1.7) | 14 (4.7) |
Values are n (%).
Self-C: self-reported constipation (positive answer at the direct question: ‘Do you consider yourself suffering of constipation?’); Self-C + Bristol: Self-C with Bristol score 1–2; Self-C – Bristol: Self-C with Bristol score 3–6; Rome-C: constipation defined according to the Rome III Criteria; NR: missing data.
Table 3 summarizes evacuation frequency and characteristics (stool consistency, straining, manual manoeuvers and feeling of incomplete defecation). Self-C and the subgroup Self-C – Bristol patients were characterized by lower frequency of all the above features, compared to Rome-C patients (p = 0.01) and Self-C + Bristol (p = 0.01), with the only exception of weekly evacuation between the two subgroups of Self-C. When compared with Rome-C patients, Self-C + Bristol patients complained significantly less of straining at evacuations and incomplete defecation (p = 0.01).
Table 3.
Clinical features of constipated patients defined according Rome Criteria or self-reported with or without Bristol stool type 1 or 2
| Clinical feature | Self-C (n = 433) | Self-C + Bristol (n = 256) | Self-C – Bristol (n = 177) | Rome-C (n = 298) |
|---|---|---|---|---|
| Weekly evacuation | ||||
| ≤2 | 105 (25.6 a) | 84 (35.1) | 21 (12.3 a) | 104 (36.4) |
| >2 | 305 (74.4) | 155 (64.9) | 150 (87.7) | 182 (63.6) |
| Total | 410 (100.0) | 239 (100.0) | 171 (100.0) | 286 (100.0) |
| NR | 23 (5.3) | 17 (6.6) | 6 (3.4) | 12 (4.0) |
| Stools | ||||
| Bristol type 1–2 | 278 (59.6 a) | 256 (100.0)b | 0 (0.0)c | 227 (76.2) |
| Bristol type 3–7 | 175 (40.4) | 0 (0.0) | 177 (100.0) | 71 (23.8) |
| Total | 433 (100.0) | 256 (100.0) | 177 (100.0) | 298 (100.0) |
| NR | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Straining at evacuations | ||||
| Yes | 223 (53.2 a) | 172 (69.1)b | 51 (30.0)c | 253 (86.1) |
| No | 196 (46.8) | 77 (30.9) | 119 (70.0) | 41 (13.9) |
| Total | 419 (100.0) | 249 (100.0) | 170 (100.0) | 294 (100.0) |
| NR | 14 (3.2) | 7 (2.7) | 7 (4.0) | 4 (1.3) |
| Manual manoeuvers | ||||
| Yes | 70 (16.7 a) | 60 (24.2) | 10 (5.8)c | 86 (29.4) |
| No | 349 (83.3) | 188 (75.8) | 161 (94.2) | 207 (70.6) |
| Total | 419 (100.0) | 248 (100.0) | 171 (100.0) | 293 (100.0) |
| NR | 14 (3.2) | 8 (3.1) | 6 (3.4) | 5 (1.7) |
| Incomplete defecation | ||||
| Yes | 202 (47.6 a) | 156 (61.9)b | 46 (26.7)c | 228 (76.5) |
| No | 222 (52.4) | 96 (38.1) | 126 (73.3) | 70 (23.5) |
| Total | 424 (100.0) | 252 (100.0) | 172 (100.0) | 298 (100.0) |
| NR | 9 (5.3) | 4 (1.5) | 5 (2.8) | 0 (0) |
| Symptoms of outlet disordersd | ||||
| Yes | 275 (67.1 a) | 201 (81.7)b | 74 (45.1)c | 287 (98.0) |
| No | 135 (32.9) | 45 (18.3) | 90 (54.9) | 6 (2.0) |
| Total | 410 (100.0) | 246 (100.0) | 164 (100.0) | 293 (100.0) |
| NR | 23 (2.1) | 10 (1.6) | 13 (7.3) | 5 (1.7) |
Values are n (%).
Self-C: self-reported constipation (positive answer at the direct question: ‘Do you consider yourself suffering of constipation?’); Self-C + Bristol: Self-C with Bristol score 1–2; Self-C – Bristol: Self-C with Bristol score 3–6; Rome-C: constipation defined according to the Rome III Criteria; NR: missing data.
p = 0.01 vs. Self-C+Bristol and Rome-C by multivariate analysis.
p = 0.01 vs. Rome-C by multivariate analysis.
p = 0.01 vs. Self-C and Self-C +Bristol and Rome-C by multivariate analysis.
Symptoms of outlet disorders: presence of at least one of straining at evacuation, manual manoeuvers, and incomplete defecation.
Discussion
The present study was carried out to evaluate epidemiological and clinical features of constipation in individuals attending, for any reason, the GP office. Although the study was performed in a GP setting, the subjects evaluated can be considered to some extent comparable to the general population in our country, since a very large number of individuals, including healthy subjects, attend the GP office for several reasons not exclusively linked to health problems. In fact, it has been estimated that more than 90% of the general population visit a GP study in the course of 3 years.19
Constipation was diagnosed by different methods. In fact, Herz and coworkers20 had shown that patients and doctors refer to different entities when they talk of constipation: 55% of patients define constipation differently from accepted medical definitions, whereas doctors still look at constipation mainly as a reduced number of weekly bowel movements The prevalence of constipation in the general population is estimated to be 10–30 % in Western countries, with a women/men ratio of 3:1, but these data may be strongly influenced by the methods of detection. The prevalence perceived by the patient is generally higher than that measured on the basis of internationally accepted criteria such as the Rome Criteria.3,12–14 This aspect bears relevant implications. For instance, the prevalence of constipation in the USA fell from 113 to 63 million people simply by changing the method of detection.3 These patients, when referring to a bowel problem, should be evaluated according to their concept of health and their expectancies in order to help them to improve their quality of life.
The demographic features of patients with constipation appear to be scarcely influenced by the diagnostic system adopted, with a higher prevalence in women being invariably confirmed. On the other hand, the three methods used in this study differ from the point of view of efficiency and ease of being understood, as demonstrated by the different percentages of missing cases. The use of a visual analogue scale seems more difficult to manage, leading to a failure to use in about 15% of cases with respect to the 6% in the case of Rome Criteria and about 3% with self-reporting. This difficulty could affect the possibility of a routine use of the visual analogue scale in this contest and should be taken into consideration, when designing new instruments for the measurement of symptom severity.
In the population included in the present study, the prevalence of self perceived constipation ranged from 33.2% to 23.2 %, according to the different methods used and is comparable with 27.2 %12 and 29.2 %,16 obtained in Canada and Turkey, respectively. The prevalence of constipation based on symptoms is lower (21.1%), similarly to previously published values ranging from 11.6 % to 24.4 %,3,12–14 with a single dissonance in the work by Pamuk and colleagues18 who, by studying a selected sample of physicians and nurses, reported values of 39.6%. In keeping with the data from the literature and regardless of the diagnostic methods adopted, the prevalence of constipation was confirmed to be greater in women than in men, with a female/male ratio ranging from 2.6 to 2.8:1,3–6 while incomplete defecation and straining at evacuation resulted more frequent than the reduced number of weekly evacuations, particularly in females.21
Symptoms suggestive of the syndrome of obstructed defecation were probably higher in the investigated population than what originally anticipated. In fact, about 20% of the subjects reported a sense of incomplete evacuation and 6% would rely on manoeuvers in support of the pelvic floor to facilitate evacuation, a figure that rises up to 16% in subjects who must manually empty the rectum. Similar figures must convince GPs to investigate carefully these aspects of the problem in all patients complaining of chronic constipation.
The combined use of the Bristol stool form scale17 and a direct question allowed us to identify two subgroups of patients among those who self-defined constipatation. The two subgroups had similar demographic features, but the group of Self-C patients with stools of Bristol type 1–2 differs from the remaining subjects in the frequency of some symptoms of obstructed defecation such as straining at evacuation and incomplete defecation. The frequency of these symptoms was lower in Self-C patients with stools type 1–2 compared to Rome C, but higher when compared to Self-C with stool type 3–7. These results raise interesting scenarios on the use in general practice diagnostic instruments simpler than the Rome criteria. The combination of self assessment of patient perceptions and questions about the stool type could represent a valuable diagnostic tool at the GP level, as opposed to more cumbersome questionnaires designed for research purposes, but this hypothesis needs to be tested in specific studies.
In summary, the results of this study confirm that constipation is a frequent condition, particularly among females. Diagnosis of constipation is markedly influenced by the different perception that affected individuals have of the condition with respect to what is diagnosed by using the current symptom-based diagnostic criteria. Diagnostic methods based on visual analogue scales could be difficult to be managed by a substantial proportion of patients. Complaints of obstructed defecation are very frequent in the population, so that GPs should take a careful medical history in order to manage all these patients appropriately. The combination of self-evaluation and the Bristol stool scale identifies a subgroup of patients with distinct clinical features. Ad-hoc-designed studies are needed to evaluate the clinical utility in general practice of simple instruments to assess constipated patients based on to their concept of health and their expectancies.
Acknowledgements
The authors thank the other members of the research group who carried out the questionnaires in their clinical activities: Luciano Bertolusso (Cuneo), Alberto Bozzani (Monza), Francesco Giacovelli (Palermo), Ignazio Grattagliano (Bari), Luigi Napoli (Napoli), and Cristina Nebiacolombo (Genova),
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Longstreth GF, Thompson G, Chey WD, et al. Functional bowel disorders. Gastroenterology 2006; 130: 1480–1491 [DOI] [PubMed] [Google Scholar]
- 2.Lindberg G, Hamid SS, Malfertheiner P, et al. World Gastroenterology Organisation Global Guideline: constipation-a global perspective. J Clin Gastroenterol 2011; 45: 483–487 [DOI] [PubMed] [Google Scholar]
- 3.Stewart WF, Liberman JN, Sandler RS, et al. Epidemiology of constipation (EPOC) study in the United States: relation of clinical subtypes to sociodemographic features. Am J Gastroenterol 1999; 94: 3530–3540 [DOI] [PubMed] [Google Scholar]
- 4.Peppas G, Alexiou VG, Mourtzoukou E, et al. Epidemiology of constipation in Europe and Oceania: a systematic review. BMC Gastroenterology 2008; 8: 5–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCrea GL, Miaskowski C, Stotts NA, et al. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J Pain Symptom Manage 2009; 37: 737–745 [DOI] [PubMed] [Google Scholar]
- 6.Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol 2011; 106: 1582–1591 [DOI] [PubMed] [Google Scholar]
- 7.Sonneberg A, Koch TR. Physician visits in the United States for constipation: 1958 to 1986. Dig Dis Sci 1989; 34: 606–611 [DOI] [PubMed] [Google Scholar]
- 8.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012; 143: 1179–1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah ND, Chitkara DK, Locke GR, et al. Ambulatory care for constipation in the United States, 1993–2004. Am J Gastroenterol 2008; 103: 1746–1753 [DOI] [PubMed] [Google Scholar]
- 10.Lacy BE, Brunton SA. Partnering with the gastroenterologist to evaluate patients with chronic constipation. Med Gen Med 2005; 7: 19–19 [PMC free article] [PubMed] [Google Scholar]
- 11.Nyrop KA, Palsson OS, Levy RL, et al. Costs of health care for irritable bowel syndrome, chronic constipation, functional diarrhoea and functional abdominal pain. Aliment Pharmacol Ther 2007; 26: 237–248 [DOI] [PubMed] [Google Scholar]
- 12.Pare P, Ferrazzi S, Thompson WG, et al. An epidemiological survey of constipation in Canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol 2001; 96: 3130–3137 [DOI] [PubMed] [Google Scholar]
- 13.Talley NJ, Fleming KC, Evans JM, et al. Constipation in an elderly community: a study of prevalence and potential risk factors. Am J Gastroenterol 1996; 91: 1666–16667 [PubMed] [Google Scholar]
- 14.Wong ML, Wee S, Pin CH, et al. Sociodemographic and lifestyle factors associated with constipation in an elderly Asian community. Am J Gastroenterol 1999; 94: 1283–1291 [DOI] [PubMed] [Google Scholar]
- 15.Bellini M, Alduini P, Bassotti G, et al. Self-perceived normality in defecation habits. Dig Liver Dis 2006; 38: 103–108 [DOI] [PubMed] [Google Scholar]
- 16.Wong RK, Palsson OS, Turner MJ, et al. Inability of the Rome III criteria to distinguish functional constipation from constipation-subtype irritable bowel syndrome. Am J Gastroenterol 2010; 105: 2228–2234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol 1997; 32: 920–924 [DOI] [PubMed] [Google Scholar]
- 18.Pamuk ON, Pamuk GE, Çelik AF. Revalidation of description of constipation in terms of recall bias and visual scale analog questionnaire. J Gastroenterol Hepatol 2003; 18: 1417–1422 [DOI] [PubMed] [Google Scholar]
- 19.Green LA, Fryer GE, Jr, Yawn BP, et al. The ecology of medical care revisited. N Engl J Med 2001; 344: 2021–2025 [DOI] [PubMed] [Google Scholar]
- 20.Herz MJ, Kahan E, Zalevski S, et al. Constipation: a different entity for patients and doctors. Fam Pract 1996; 13: 156–159 [DOI] [PubMed] [Google Scholar]
- 21.Johanson JF, Kralstein J. Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther 2007; 25: 599–608 [DOI] [PubMed] [Google Scholar]


