Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) is technically more challenging in patients with postsurgical anatomy such as Roux-en-Y anastomosis, frequently mandating an operative intervention. Although limited, there is growing evidence that ERCP can be performed using the balloon-overtube-assisted enteroscopy (BOAE) in patients with complex postoperative anatomy. We present the technical aspects of performing ERCP with the BOAE in patients presenting with complex postsurgical anatomy having biliary problems. ERCP using the BOAE is feasible in patients with complex postsurgical anatomy, permitting diagnostic and therapeutic interventions in 80% of patients.
Keywords: cholangiography, double balloon enteroscopy, hepaticojejunostomy, overtube-assisted enteroscopy, Roux-en-Y anastomosis, single balloon enteroscopy
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is requisite in the management of many pancreatobiliary diseases and has a 95% success rate in the general public; however, among patients with altered small bowel anatomy, the success rate has been approximately half of that [Yamamoto et al. 2001; May et al. 2003; Feitoza and Baron, 2001]. The introduction of the double-balloon enteroscopy (DBE) and single-balloon enteroscopy (SBE) techniques, referred to collectively as balloon-overtube-assisted enteroscopy (BOAE), has greatly improved our ability to perform ERCP in patients with altered upper gastrointestinal (GI) anatomy [Haber, 2007; Mönkemüller et al. 2008]. Spiral enteroscopy, a third overtube-assisted enteroscopy technique, initially showed promise, but is no longer commercially available [Lennon et al. 2012]. Therefore, this report focuses on the two dominant and still available techniques for BOAE-ERCP: SBE and DBE methods.
The purpose of this review is to educate readers on underlying anatomical variations necessitating BOAE techniques, provide a technical description of the procedure, describe success rates regarding anatomical variations, and describe technical difficulties that the endoscopist may encounter during BOAE-ERCP.
Postsurgical anatomy
It is imperative that the endoscopist has a good understanding of postoperative anatomy (Figures 1–4). From the perspective of the endoscopist, we delineate postsurgical anatomy into two subgroups: those that can be accomplished with a standard duodenoscope with standard ERCP accessories, and those that require longer, forward viewing endoscopes (i.e. colonoscope or enteroscope) to accomplish ERCP.
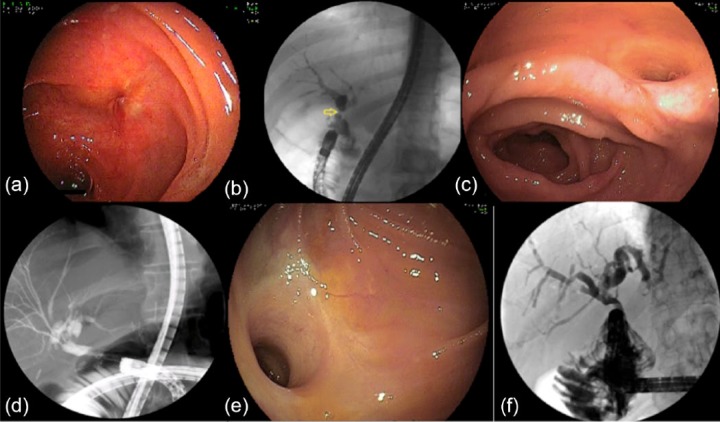
Figure 1.
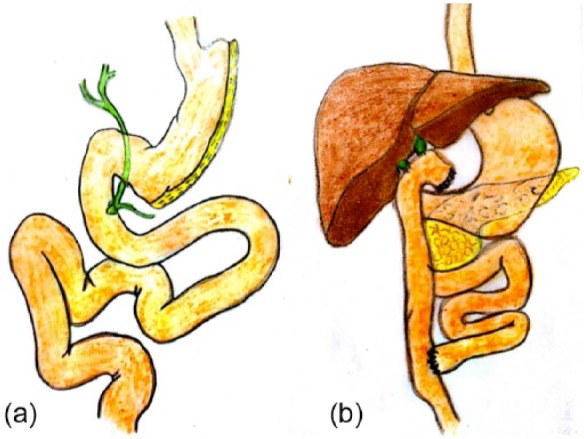
Complex postsurgical upper gastrointestinal anatomy. (a) Gastric sleeve. In these patients endoscopic retrograde cholangiopancreatography can be performed using a standard duodenoscope. (b) Roux-en-Y with hepaticojejunostomy. In this case a double hepaticojejunostomy was performed.
Figures 2.
Billroth II operation. (a) The body and antrum are resected. (b) A gastrojejunostomy is created. The entrance to the afferent limb is usually on the ‘right’.
Figure 3.
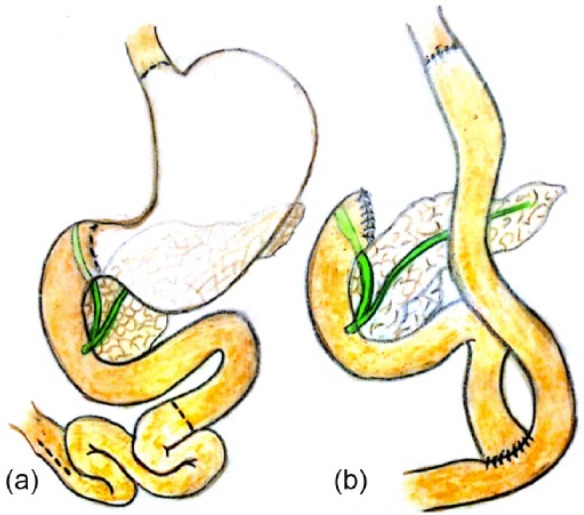
Total gastrectomy with Roux-en-Y anastomosis. (a) Resection of the stomach. (b) Esophagojejunal anastomosis. The proximal anastomosis can be straight or J shaped. If J shaped, careful attention must be paid not to confuse the blind pouch with another limb.
Figure 4.
Classic Kausch–Whipple operation. (a) The schematic shows the lines of resection: antrum, head of pancreas and duodenum. (b) The proximal end of the jejunum is brought to the liver bed and a hepaticojejunostomy is performed. The jejunal limb is used to create a gastrojejunosotmy. Notice that the afferent limb can be quite short, and thus accessible with a colonoscope or even a duodenoscope. However, the success rate of using ‘shorter’ scopes is about 50%.
A standard duodenoscope can be used in patients status post gastric banding, sleeve gastrectomy, or Billroth I. Gastric banding entails the placement of a band circumferentially around the proximal part of the stomach in close proximity to the gastroesophageal junction [Belachew et al. 1995]. The band can be periodically adjusted through a subcutaneous port positioned in the rectus abdominis [Belachew et al. 1995]. A sleeve gastrectomy [Figure 1(a)] involves the resection of the greater curvature of the stomach, while maintaining unaltered continuity between the esophagus, stomach, pylorus, and duodenum [Moy et al. 2008]. The Billroth I procedure involves resection of the distal aspect of the stomach with anastomosis of the proximal stomach to the duodenum [Uyama et al. 1995].
A long scope (e.g. colonoscope) or balloon-assisted enteroscopy is required to gain access to the papilla of Vater or hepaticojejunostomy in patients status post Billroth II gastrojejunostomy [Figure 1(b)] and any technique in which a Roux-en-Y is created [Haber, 2007]. The Billroth II gastrojejunostomy (Figure 2) was initially devised to treat gastric outlet obstruction, but can be applied to any distal subtotal gastrectomy [Goh et al. 1992]. In this technique the jejunum is attached to the proximal gastric remnant in the creation of a gastrojejunal anastomosis [Goh et al. 1992]. The duodenojejunal segment is approximately 15–30 cm in length, with the papilla of Vater intact to provide the second anchor point of the segment [Goh et al. 1992]. Roux-en-Y anastomosis are most commonly performed in conjunction with total gastrectomy with esophagojejunostomy (Figure 3), gastric bypass and pancreaticobiliary procedures, which include pancreaticoduodenectomy (Whipple procedure), pylorus-preserving pancreaticoduodenectomy (modified Whipple procedure) [Figures 1(b) and 4], Frey procedure, and orthotopic liver transplantation with choledochojejunostomy [Feitoza and Baron, 2002; Chahal et al. 2006]. The following is a description of the Roux-en-Y technique used during a gastric bypass procedure:
The stomach is first transected with the anterior portion being formed into a small gastric pouch. Next, the jejunum is transected 30–75 cm distal to the ligament of Treitz. The distal jejunal segment is joined to the anterior gastric pouch in a gastrojejunal anastomosis. This becomes the Roux-limb. The excluded biliary limb is then anastomosed to the jejunum 50-150 cm distal to the gastrojejunal anastomosis in the formation of the jejunojejunal anastomosis [Higa et al. 2000].
Definition of ERCP using the BOAE
BOAE-ERCP is the performance of diagnostic or therapeutic interventions of the biliary or pancreatic ducts in patients who require the use of enteroscopes and devices such as overtubes or overtubes with balloons to access the papilla of Vater or pancreaticobiliary anastomosis due to a long or tortuous path created by prior GI surgery. Success is defined by the most common pitfalls of the technique, namely enteroscopic success and cannulation success. Enteroscopic success is defined as the ability to identify the pancreaticobiliary anastomosis or papilla of Vater. Cannulation success is the ability to cannulate either the papilla or the anastomosis. Cannulation success is commonly subdivided further into diagnostic success and therapeutic success, with diagnostic success defined as the ability to perform a cholangiogram leading to a diagnosis and therapeutic success defined as the ability to treat the underlying disorder (e.g. stone removal, stent insertion, balloon dilation). Resultant complications of BOAE-ERCP are defined according to standard criteria and experience of large centers performing DBE [Cotton et al. 1991; Mensink et al. 2007]. However, there are no studies specifically evaluating the complications associated with BOAE-ERCP.
Patient preparation and type sedation/anesthesia
The operative report should be studied in order to understand the patient’s anatomy and plan for the procedure. In addition, all available GI imaging, including computed tomography, magnetic resonance tomography (MRT), and upper GI series should be reviewed. If the operative report is not available, we recommend that a standard esophagogastroduodenoscopy (EGD) be performed prior to BOAE-ERCP to clarify the anatomy of the upper GI tract. Whether performing enterography (e.g. MRT enterography) assists in the planning of BOAE-ERCP is unknown. Often, Billroth I and II anatomies are confused. In a patient with Billroth I anatomy the ERCP can be performed using a standard duodenoscope. Likewise gastric bypass and gastric sleeve operations are commonly confused. Gastric sleeve [Figure 1(a)] is only a ‘narrowing’ of the stomach, whereas gastric bypass entails a long jejunal interposition, similar to what is performed during a total gastrectomy (Figure 3). In our experience, performing an EGD can be useful to ‘map out’ and clarify the anatomy, and often ERCP can be performed with a standard duodenoscope.
Because many patients requiring BOAE-ERCP have cholestasis and are more likely to have coagulopathies due to vitamin K malabsorption, particular attention should be paid to the prothrombin time, with efforts made to rectify aberrant values with intravenous vitamin K [Clarke et al. 2006]. Both aspirin and P2Y12 platelet inhibitors can be safely continued during ERCP [Boustiere et al. 2011].
Perioperative antibiotics such as ciprofloxacin or ceftriaxone should be provided to prevent cholangitis when biliary drainage is incomplete in patients with post-transplant biliary strictures, patients with communicating pancreatic cysts or pseudocysts. In patients with artificial heart valves we follow the guidelines from the American Society for Gastrointestinal Endoscopy [Banerjee et al. 2008].
Patients should be fasting for at least 6 h prior to the procedure [American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists, 2002]. Due to the complexity and length of the procedure, BOAE-ERCP should be performed using moderate sedation with propofol or under general anesthesia. Although this decision is typically made based on local expertise and preference, we strongly recommend using general anesthesia as the procedure can be lengthy and the minor movements of the patient may result in displacement of stent or loosing cannulation of a tiny hepaticojejunostomy. The use of antispasmodics is not routinely recommended. However, during bile duct cannulation we use intravenous antispasmodics (e.g. hyosciamine) if the motility of the afferent limb is increased.
Technical aspects
Endoscopes
Enteroscopes are divided according to their designed task: diagnostic or therapeutic. They differ in length, scope diameter, working channel diameter, overtube length, overtube diameter. We currently recommend using either a standard 200 cm or ‘short’ 152 cm therapeutic enteroscope with a 2.8 mm accessory channel. A list of enteroscopes and their specifications is provided in Table 1.
Table 1.
Enteroscopy device specifications.
| Specifications |
||||||
|---|---|---|---|---|---|---|
| Enteroscopes | Scope working length (cm) | Scope diameter (mm) | Channel diameter (mm) | Overtube length (cm) | Overtube diameter (mm) | Potential advantages |
| SBE (Olympus, Tokyo, Japan, SIF-Q180) | 200 | 9.2 | 2.8 | 140 | 13.2 | Ease of use |
| DBE (Fujinon, Tokyo, Fujifilm, Japan, EN-450PS/20 | 200 | 8.5 | 2.2 | 145 | 12.2 | Flexibility |
| DBE (Fujinon, Tokyo, Fujifilm, Japan, EN-450T5) | 200 | 9.4 | 2.8 | 145 | 13.2 | Depth of insertion |
| DBE (Fujinon, Tokyo, Fujifilm, Japan, EC-450BI5) | 152 | 9.4 | 2.8 | 105 | 13.2 | ERCP |
| Pentax VSB-3430K | 220 | 11.6 | 3.8 | Any instrument | ||
| SE Spirus medical (Stoughton, MA, USA), discovery SB | * | * | * | 118 | 16 | Shorter examination time |
Either the Fujinon DBE enteroscope or the Olympus SBE enteroscope can be used to perform SE with a SE overtube.
DBE, double-balloon enteroscopy; ERCP, endoscopic retrograde cholangiopancreatography; SB, small bowel; SBE, single balloon enteroscopy; SE, spiral enteroscopy.
Although we were the first to report on the feasibility and potential utility of SBE-ERCP, we currently recommend DBE-ERCP, as the presence of the balloon on the tip of the scope is particularly useful in the presence of tight angulations, nicked bowel and external adhesions [Mönkemüller et al. 2008]. It allows for faster intubation of the afferent limb and intubation of the excluded stomach in patients who have undergone gastric bypass.
Procedure description
Learning curve
Although no formal studies have documented the learning curve associated with BOAE-ERCP, the learning curve associated with DBE has been described. In one trial the mean duration of the first 10 cases was 109 min, while in subsequent cases the mean duration was 92 min. This was associated with a decline in mean fluoroscopy time. There was no change associated with depth of intubation [Mehdizadeh et al. 2006].
Technique of advancing the BOAE into the excluded Roux-en-Y limb
The patient should be placed in decubitus supine position on the table, with a C-arm in place so that fluoroscopic guidance can be provided throughout the procedure [Mönkemüller et al. 2009] (Figure 5).
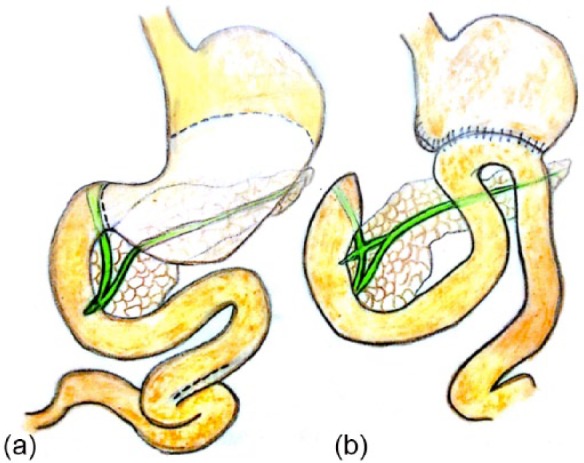
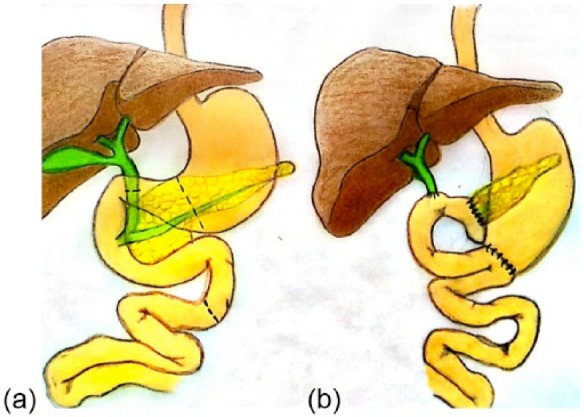
Figure 5.
Fluroscopy findings of enteroscopes during balloon-overtube-assisted enteroscopy for endoscopic retrograde cholangiopancreatography in patients with gastric bypass and Roux-en-Y anastomosis. (a) The limb leading to the excluded stomach may be quite large. As seen from this image, reaching the excluded stomach using standard scopes is impossible and the use of BOAE is mandatory. (b) The excluded stomach shadow can be easily identified by the presence of air delineating its contour (arrows). The scope has entered the stomach through the pylorus.
The push-then-pull method operant during a standard DBE can be used for advancing the enteroscope. Previous abdominal surgery complicates the procedure, with adhesions limiting the mobility of the intestines and inhibiting further intubation of the lumen. It is critical that the enteroscope is not advanced forcefully. Changing the position of the patient or applying external abdominal pressure may aid in advancement of the enteroscope. Fluoroscopy can help the endoscopist visualize the direction the enteroscope is taking, as well as provide estimates as to the degree of looping [Moreels et al. 2009]. The endoscopist must minimize insufflation, as bowel distention can drastically limit enteroscope advancement. Due to its increased rate of absorption, insufflation with carbon dioxide rather than standard air improves intubation depth and lessens postprocedural pain [Domagk et al. 2007].
Measurement of depth of insertion
There are no data on how to measure the depth of insertion during BOAE-ERCP. Because of the presence of adhesions there is no way to exactly evaluate the depth of insertion. Indeed, measuring the depth of insertion during BOAE-ERCP is not useful, as the key issue is to find the afferent and efferent limbs.
Localization of the anastomosis and afferent limb
Finding the afferent limb in patients with gastrojejunostomy (e.g. Billroth II) should not be very difficult, and in most patients the afferent limb entrance is located on the right side. Juxtaposed to this, in patients with Roux-en-Y surgery, the anastomosis is not recognized in up to half of cases during the initial pass, and fluoroscopy should be utilized to aid in the localization of the jejunojejunal anastomosis [Mönkemüller et al. 2009; Moreels et al. 2009]. Fluoroscopic visualization of the enteroscope in the mid-abdomen or pelvis, or depth of insertion in excess of 120–140 cm indicates that the enteroscope missed the anastomosis. At this point, the enteroscope should be retracted slowly in careful search of the anastomosis. The presence of bile, luminal dilation, the loss of circular folds or paradoxical peristalsis are all signs of jejunojejunal anastomosis [Moreels et al. 2009]. Once the anastomosis is reached, the enteroscope should be guided into the limb with bilious drainage or ‘yellow bubbles’ resultant from bile saponification [Mönkemüller et al. 2009]. Because visualization of this is critical, flushing with simethicone should be avoided until the afferent limb has been intubated. Once the anastomosis and afferent limb have been successfully identified, they can be marked with India ink for any future possible procedures [Pohl et al. 2009; Shimatani et al. 2009; Raithel et al. 2011] (Figure 6).
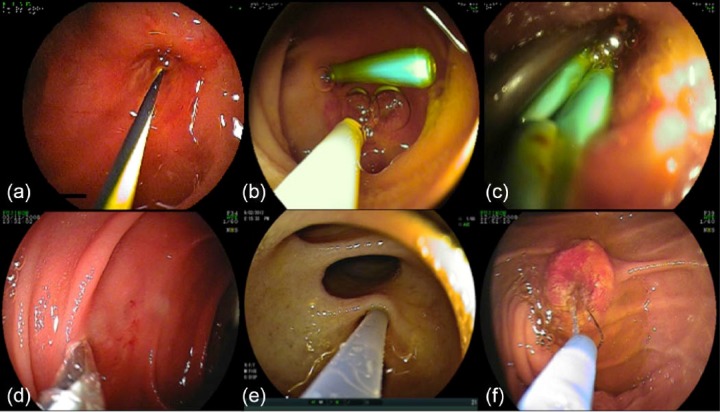
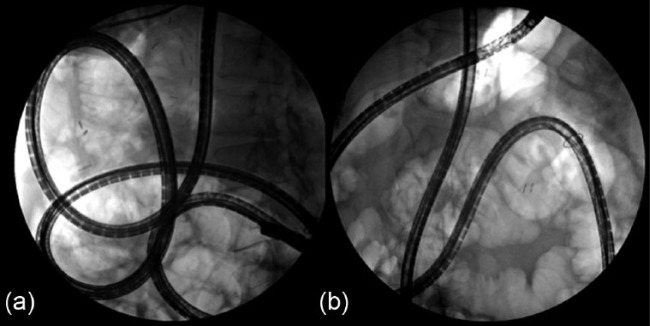
Figure 6.
Roux-en-Y jejunojejunal anastomosis. (a) The afferent limb is on the right. (b) The afferent limb is on the left. In both cases there were bile induced bubbles at the entrance of the limb. However, these bubbles are nonspecific. (c) It is recommended to use an India ink tattoo to mark the afferent limb. However, when the scope has advanced deeply into the efferent limb it is fine to mark the proximal end of this limb. The main objective is to have one limb clearly marked, but the report should clearly specify which one is marked. Marking the efferent limb may be easier and more practical, as the entrance to the afferent limb may be ‘upward’ and angulated. During repeat balloon-overtube-assisted enteroscopy for endoscopic retrograde cholangiopancreatography the upwards going limb with its India ink tattoo may be missed.
Intubation of the afferent limb
Nonangulated anastomoses typically provide no difficulty for intubation; however, they are frequently not the norm. The jejunojejunal anastomosis leading into the afferent limb typically has slight to marked angulation, which can provide a challenge. When intubating, it is useful to advance the enteroscope 15–20 cm into the afferent limb and then inflate its balloon to secure its position [Mönkemüller et al. 2009]. The overtube can then be passed into the afferent limb with its balloon subsequently inflated [Mönkemüller et al. 2009]. Pushing in the enteroscope further while advancing the overtube may provide even further stability in the afferent limb [Mönkemüller et al. 2009]. After the overtube is secure in the afferent limb, the push-then-pull maneuver can be resumed [Mönkemüller et al. 2009]. Frequently it is useful to briefly advance and pull the endoscope in a ‘to and fro’ manner, allowing the intestine to slide over the scope and improving the ability to negotiate through the small bowel turns. Using fluoroscopic control the endoscopist can recognize the enteroscope is moving towards the liver shadow, with the enteroscope assuming either a figure of eight or spiral shape, denoting that the afferent limb has been deeply intubated [Moreels et al. 2009]. The balloon on the tip of the catheter can be inflated and contrast injected into the lumen of the afferent limb to confirm under fluoroscopy correct positioning and the trajectory of the afferent limb [Shimatani et al. 2009]. The presence of percutaneously placed stents can also serve as a localization method for the afferent limb and either the hepaticojejunostomy or the papilla of Vater [Mönkemüller et al. 2009].
Finding the hepaticojejunostomy or papilla during BOAE-ERCP
Successful intubation of the afferent limb, which is typically 50–90 cm long, is defined as localization of the proximal end of the anastomosis (i.e. blind pouch) and ability to identify the opening of the hepaticojejunostomy or papilla of Vater. In all cases, the blind pouch, located under the liver shadow during fluoroscopy, should be carefully identified [Neumann et al. 2009]. The localization of the hepaticojejunostomy or papilla can be somewhat variable, but generally is in the lower left field of endoscopic view [Mönkemüller et al. 2009]. This has an advantage, as the opening of the accessory channel is at the 6 o’clock position, which allows directing the accessory material easier into the biliary opening [Mönkemüller et al. 2009]. Generally, the opening of the hepaticojejunostomy, which sits approximately 10–15 cm distal to the blind end, is very small, making it difficult to identify [Mönkemüller et al. 2009]. Patience and perseverance are often requisite for success. If there is not complete obstruction of the common bile duct, the hepaticojejunostomy may be identified by the exuding of bile from the opening [Moreels et al. 2009]. Less frequently, the hepaticojejunostomy opening is very large, permitting the introduction of the tip of the BOAE into the common bile duct and therefore allowing the performance of a direct cholangioscopy [Mou et al. 2010]. When there are two small orifices in the blind pouch, injection of contrast under fluoroscopy may help identify the common hepatic duct or pancreatic duct.
In cases of Roux-en-Y gastric bypass, DBE allows for advancement of the scope and overtube into their excluded stomach. The balloon on the tip of the scope serves as an anchor, allowing for the overtube to be slid towards the tip of the scope entering from the duodenum, through the pylorus and into the antrum (Figure 7).
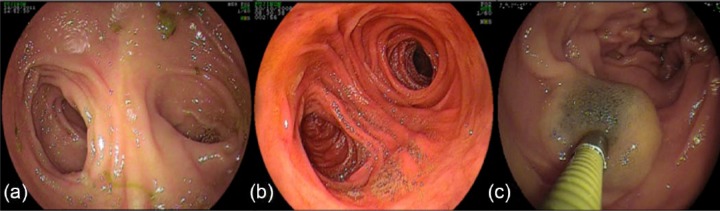
Figure 7.
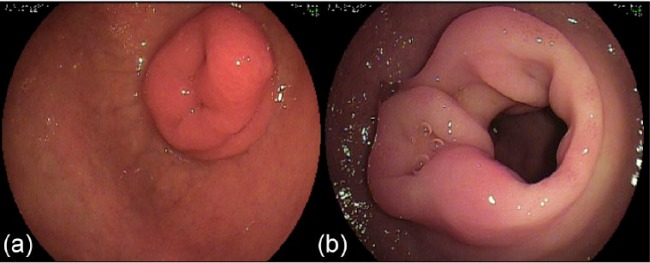
View of the backside of the pylorus in Roux-en-Y gastric bypass. (a) The pylorus extrudes well inside the duodenal bulb. (b) Multiple small erosions on the backside of the pylorus.
Cannulation of the biliary tree
Cannulation of either the native papilla or biliary anastomosis is a requisite precondition for successful ERCP and may provide some difficulty for the endoscopist. It should be noted that repositioning of either the overtube or the enteroscope can be utilized to change the position of the papilla relative to the working channel [Osoegawa et al. 2012]. A soft transparent hood (DH-17EN; Fujifilm, Tokyo, Japan) has successfully been utilized to fix the papilla in place to ease cannulation [Osoegawa et al. 2012]. Cannulation of the biliary tract can be achieved with a tapered tip biliary catheter, several types of 650 cm guidewires or BOAE-ERCP designed sphincterotomes. If conventional cannulation proves to be intractably difficult, a needle-knife precut papillotomy can be performed to facilitate cannulation [Fukatsu et al. 2008]. When performing BOAE-ERCP in patients with previously placed percutaneous stents, the guidewire should be advanced into the common bile duct before removing the percutaneous stents, particularly in patients with an intact papilla.
Cholangiography
With the advent of BOAE-ERCP, we are now able to characterize hepaticojejunostomy strictures, and doing so is helpful in the planning of therapeutic interventions [Mönkemüller and Jovanovic, 2011]. The hepaticojejunostomy orifice may be small (type A) or large (type B) [Mönkemüller and Jovanovic, 2011] (Figure 8). The strictures are categorized by length: short (type 1, <5 mm) or long (type 2, >5 mm); or whether the strictures are entrahepatic (type 3) [Mönkemüller and Jovanovic, 2011].
Figure 8.
Hepaticojejunostomies. (a) Occasionally the hepaticojejunostomy is very small and can only be recognized by the presence of mucus or bile flow. This is a type A anastomosis based on the Mönkemüller and Jovanovic classification. (b) Cholangiogram reveals a short, tight stricture, type 1. Thus, the hepaticojejunostomy is type A1 (small opening, short stricture). (c) Normal or large opening hepaticojejunostomy (type B) anastomosis (large opening). (d) There are intrahepatic strictures and dilations (type 3). Thus, this is a type B3 hepaticojejunostomy anastomosis. (e) Direct cholangiography in a large, type C hepaticojejunostomy. Always perform a direct cholangioscopy using water, saline or carbon dioxide to distend the lumen, as direct insufflation of air into the bile duct is associated with air embolism. (f) The process of direct cholangioscopy and cholangiography is called endoscopic retrograde cholangioscopy and cholangiography.
Therapeutic interventions
In order to perform BOAE-ERCP related interventions, we recommend using either the standard 200 cm or ‘short’ 152 cm therapeutic enteroscope. We would caution against a ‘short’ enteroscope system in patients with long-limb gastric bypass as no prospective or retrospective studies have validated its feasibility in this setting. Importantly, these devices have a 2.8 mm diameter working channel, which allows for a larger variety of therapeutic accessories [Cho et al. 2011; Mönkemüller et al. 2009]. Because standard length enteroscopes are 200 cm long, they require the use of extra-long accessories, which are currently limited [Cho et al. 2011]. Circumventing this limitation, the 152 cm enteroscope can utilize standard length accessories, which may provide some advantage pertaining to therapeutic interventions [Cho et al. 2011; Shimatani et al. 2009; Siddiqui et al. 2013]. Unfortunately, many ERCP tools, including 10 Fr and self-expanding metal stents, require a 3.2 mm working channel. We and others have utilized a rendezvous technique in which a guidewire is passed through a previously placed percutaneous transhepatic biliary drain, and larger accessories can be placed over that guidewire under both fluoroscopic and enteroscopic visualization [Itoi et al. 2009; Mönkemüller et al. 2013a, 2013b]. Additionally, we recently employed a technique to utilize accessories that do not fit through current BOAE working channels in which we utilized a DBE-ERCP to advance a guidewire deep in the biliary tree [Skinner et al. 2013]. The enteroscope was removed out of the overtube while the guidewire was left in place. Subsequently, utilizing fluoroscopic visualization we were able to advance a self-expanding metal stent over the guidewire, through the overtube, which functionally served as an ‘extra-large working channel’, into the biliary tree [Skinner et al. 2013] (Figure 9).
Figure 9.
Interventions during balloon-overtube-assisted enteroscopy for endoscopic retrograde cholangiopancreatography. (a) Insertion of a guidewire through a tiny, type A hepaticojejunostomy. (b) Placement of a single 7 Fr plastic stent. (c) Multistenting using several 5 Fr (pancreatic) plastic stents. We found that pushing the smaller diameter pancreatic stents is much easier than the biliary 7 Fr plastic stents and use the ‘multi-stenting’ concept for bile duct strictures. (d) Balloon dilation of a stenotic hepaticojejunostomy. (e) The scope can be advanced into the biliary tract (i.e. direct cholangioscopy) and then selective cannulation of the branches is performed. Injection of contrast through the scope into the bile ducts. (f) Biliary sphincterotomy using a Billroth II sphincterotome in a patient with Billroth II anatomy. Notice that the direction of the bile duct is at the 5 o’clock position because the papilla is upside down.
Occasionally, the accessory equipment will not advance through the tip of the scope due to the curvature at the tip of the scope. This can be visualized and corrected under fluoroscopy to allow the advancement of the accessory materials. Lubrication of the working channel of the scope with mixed chain triglyceride oil (Fresenius Kabi, Bad Homburg, Germany) or silicone (Silikonspray, Asid Bonz, Böblingen, Herrenberg, Germany) can also be useful.
Outcomes
In aggregate, BOAE-ERCP has shown itself to be tremendously successful in the treatment of biliary complications in patients with altered GI anatomy. Success rates vary depending on the underlying anatomy of the patient. In patients who have undergone a prior Roux-en-Y gastric bypass, enteroscopic success is 80% and ERCP success 70% [Skinner et al. 2014]. In patients who underwent a prior Whipple procedure, enteroscopic success is 85%, while ERCP success is 76%. In patients with underlying Billroth II (BII) anatomy, the success of enteroscopy is 96% and ERCP success is 90% [Skinner et al. 2014]. Cannulation rates appear to be comparable between native papilla and pancreaticobiliary anastomoses, with success rates of 90% and 92% respectively [Skinner et al. 2014]. Success rates appear to be similar between SBE and DBE, and depend most highly on local expertise [Shah et al. 2013]. The complication rate of 3.4% is in fact lower than that of standard ERCP. This is likely due to the fact that a sizeable percentage of patients have pancreaticobiliary anastomoses, which are less susceptible to postprocedure complications such as pancreatitis.
Alternative endoscopic techniques
The two most studied alternative techniques are ERCP through a gastrostomy tract (GERCP) and laparoscopy-assisted ERCP (LA-ERCP). One study demonstrated access to the major papilla was 95% in GERCP procedures versus 63% with BOAE-ERCP; however, it was associated with a 14.5% complication rate versus 3.1% [Choi et al. 2013]. A report comparing LA-ERCP with BOAE-ERCP noted respective success rates of 100% versus 56% in a study underpowered to detect for complication rates [Schreiner et al. 2012]. The use of endoscopic ultrasound guided biliary drainage is limited to patients with intact stomach, but practically impossible in patients with gastric bypass.
Summary
This report demonstrates the technique and utility of BOAE to perform diagnostic and therapeutic pancreatobiliary interventions in patients with surgically distorted small bowel anatomy, such as Roux-en-Y anastomosis with hepaticojejunostomy. Our experience and that of others demonstrates that ERCP with BOAE is feasible. Using BOAE, it is possible to intubate the afferent limb, visualize the hepaticojejunostomy, and demonstrate anastomotic strictures or bile duct stones of the choledochojejunostomy. Therapeutic procedures have included stone extraction, sphincterotomy, biliary stent placement, biliary balloon dilation, stent extraction and application of argon plasma coagulation at angiodysplasias at the hepaticojejunostomy.
BOAE-ERCP is still in its infancy, and with further refinements to the enteroscope, such as a larger working channel and an increased variety of extra-long biliary accessories for the 200 cm enteroscope, efficacy of BOAE-ERCP should continue to improve.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: KM received one honorarium from Cook Medical, Winston Salem, NC, USA for giving one lecture on ‘Gastrointestinal stents’. JVA was awarded the Boston Scientific Visiting Fellowship 2014. He performed this work during his Fellowship at the Basil I. Hirschowitz Center of Endoscopic Excellence at the University of Alabama, Birmingham, USA. MS declares that there is no potential conflict of interest. There was no assistance with study design, data collection, data analysis, or manuscript preparation from anybody else except the authors.
Contributor Information
Matthew Skinner, Basil I. Hirschowitz Endoscopic Center of Excellence, Division of Gastroenterology and Hepatology, Birmingham, AL, USA.
Jacobo Velázquez-Aviña, Basil I. Hirschowitz Endoscopic Center of Excellence, Division of Gastroenterology and Hepatology, Birmingham, AL, USA.
Klaus Mönkemüller, Division of Gastroenterology and Hepatology, Basil Hirschowitz Endoscopic Center of Excellence, Endoscopy Unit, JT 664, 619 19th Street S, Birmingham, AL 35249, USA.
References
- American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 96: 1004–1017 [DOI] [PubMed] [Google Scholar]
- Banerjee S., Shen B., Baron T., Nelson D., Anderson M., Cash B., et al.; ASGE Standards of Practice Committee (2008) Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 67: 791–798 [DOI] [PubMed] [Google Scholar]
- Belachew M., Legrand M., Vincenti V., Deffechereux T., Jourdan J., Monami B., et al. (1995) Laparoscopic placement of adjustable silicone gastric band in the treatment of morbid obesity: how to do it. Obes Surg 5: 66–70 [DOI] [PubMed] [Google Scholar]
- Boustiere C., Veitch A., Vanbiervliet G., Bulois P., Deprez P., Laquiere A., et al.; European Society of Gastrointestinal Endoscopy (2011) Endoscopy and antiplatelet agents. European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 43: 445–461 [DOI] [PubMed] [Google Scholar]
- Chahal P., Baron T., Topazian M., Petersen B., Levy M., Gostout C. (2006) Endoscopic retrograde cholangiopancreatography in post-Whipple patients. Endoscopy 38: 1241–1245 [DOI] [PubMed] [Google Scholar]
- Cho S., Kamalaporn P., Kandel G., Kortan P., Marcon N., May G. (2011) ‘Short’ double-balloon enteroscope endoscopic retrograde cholangiopancreatography in patients with a surgically altered upper gastrointestinal tract. Can J Gastroenterol 25: 615–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi E., Chiorean M., Cote G., El Hajj I., Ballard D., Fogel E., et al. (2013) ERCP via gastrostomy vs. double balloon enteroscopy in patients with prior bariatric Roux-en-Y gastric bypass surgery. Surg Endosc 27: 2894–2899 [DOI] [PubMed] [Google Scholar]
- Clarke D., Pillay Y., Anderson F., Thomson S. (2006) The current standard of care in the periprocedural management of the patient with obstructive jaundice. Ann R Coll Surg Engl 88: 610–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton P., Lehman G., Vennes J., Geenen J., Russell R., Meyers W., et al. (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37: 383–393 [DOI] [PubMed] [Google Scholar]
- Domagk D., Bretthauer M., Lenz P., Aabakken L., Ullerich H., Maaser C., et al. (2007) Carbon dioxide insufflation improves intubation depth in double-balloon enteroscopy: a randomized, controlled, double-blind trial. Endoscopy 39: 1064–1067 [DOI] [PubMed] [Google Scholar]
- Feitoza A., Baron T. (2001) Endoscopy and ERCP in the setting of previous upper GI tract surgery. Part I: reconstruction without alteration of pancreaticobiliary anatomy. Gastrointest Endosc 54: 743–749 [DOI] [PubMed] [Google Scholar]
- Feitoza A., Baron T. (2002) Endoscopy and ERCP in the setting of previous upper GI tract surgery. Part II: postsurgical anatomy with alteration of the pancreaticobiliary tree. Gastrointest Endosc 55: 75–79 [DOI] [PubMed] [Google Scholar]
- Fukatsu H., Kawamoto H., Kato H., Hirao K., Kurihara N., Nakanishi T., et al. (2008) Evaluation of needle-knife precut papillotomy after unsuccessful biliary cannulation, especially with regard to postoperative anatomic factors. Surg Endosc 22: 717–723 [DOI] [PubMed] [Google Scholar]
- Goh P., Tekant Y., Isaac J., Kum C., Ngoi S. (1992) The technique of laparoscopic Billroth II gastrectomy. Surg Laparosc Endosc 2: 258–260 [PubMed] [Google Scholar]
- Haber G. (2007) Double balloon endoscopy for pancreatic and biliary access in altered anatomy (with videos). Gastrointest Endosc 66: S47–S50 [DOI] [PubMed] [Google Scholar]
- Higa K., Boone K., Ho T., Davies O. (2000) Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg 135: 1029–1033; discussion 1033–1034. [DOI] [PubMed] [Google Scholar]
- Itoi T., Ishii K., Sofuni A., Itokawa F., Kurihara T., Tsuchiya T., et al. (2009) Single balloon enteroscopy-assisted ERCP using rendezvous technique for Sharp angulation of Roux-en-Y limb in a patient with bile duct stones. Diagn Ther Endosc 2009: 154084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennon A., Kapoor S., Khashab M., Corless E., Amateau S., Dunbar K., et al. (2012) Spiral assisted ERCP is equivalent to single balloon assisted ERCP in patients with Roux-en-Y anatomy. Dig Dis Sci 57: 1391–1398 [DOI] [PubMed] [Google Scholar]
- May A., Nachbar L., Wardak A., Yamamoto H., Ell C. (2003) Double-balloon enteroscopy: preliminary experience in patients with obscure gastrointestinal bleeding or chronic abdominal pain. Endoscopy 35: 985–991 [DOI] [PubMed] [Google Scholar]
- Mehdizadeh S., Ross A., Gerson L., Leighton J., Chen A., Schembre D., et al. (2006) What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc 64: 740–750 [DOI] [PubMed] [Google Scholar]
- Mensink P., Haringsma J., Kucharzik T., Cellier C., Pérez-Cuadrado E., Mönkemüller K., et al. (2007) Complications of double balloon enteroscopy: a multicenter survey. Endoscopy 39: 613–615 [DOI] [PubMed] [Google Scholar]
- Mönkemüller K., Fry L., Bellutti M., Neumann H., Malfertheiner P. (2008) ERCP using single-balloon instead of double-balloon enteroscopy in patients with Roux-en-Y anastomosis. Endoscopy 40(Suppl. 2): E19–E20 [DOI] [PubMed] [Google Scholar]
- Mönkemüller K., Fry L., Bellutti M., Neumann H., Malfertheiner P. (2009) ERCP with the double balloon enteroscope in patients with Roux-en-Y anastomosis. Surg Endosc 23: 1961–1967 [DOI] [PubMed] [Google Scholar]
- Mönkemüller K., Jovanovic I. (2011) Endoscopic and retrograde cholangiographic appearance of hepaticojejunostomy strictures: a practical classification. World J Gastrointest Endosc 3: 213–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mönkemüller K., McGuire B., Wilcox C., Ramesh J., Dubay D., Eckhoff D. (2013a) Percutaneous balloon dilation and placement of endoscopic biliary stent by using the double-balloon enteroscopy ERCP rendezvous technique. Gastrointest Endosc 78: 383–385 [DOI] [PubMed] [Google Scholar]
- Mönkemüller K., Popa D., McGuire B., Ramesh J., Wilcox C. (2013b) Double-balloon enteroscopy-ERCP rendezvous technique. Endoscopy 45(Suppl. 2): E333–E334 [DOI] [PubMed] [Google Scholar]
- Moreels T., Hubens G., Ysebaert D., Op De, Beeck B., Pelckmans P. (2009) Diagnostic and therapeutic double-balloon enteroscopy after small bowel Roux-en-Y reconstructive surgery. Digestion 80: 141–147 [DOI] [PubMed] [Google Scholar]
- Mou S., Waxman I., Chennat J. (2010) Peroral cholangioscopy in Roux-en-Y hepaticojejunostomy anatomy by using the SpyGlass Direct Visualization System (with video). Gastrointest Endosc 72: 458–460 [DOI] [PubMed] [Google Scholar]
- Moy J., Pomp A., Dakin G., Parikh M., Gagner M. (2008) Laparoscopic sleeve gastrectomy for morbid obesity. Am J Surg 196: e56–e59 [DOI] [PubMed] [Google Scholar]
- Neumann H., Fry L., Meyer F., Malfertheiner P., Monkemuller K. (2009) Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion 80: 52–57 [DOI] [PubMed] [Google Scholar]
- Osoegawa T., Motomura Y., Akahoshi K., Higuchi N., Tanaka Y., Hisano T., et al. (2012) Improved techniques for double-balloon-enteroscopy-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol 18: 6843–6849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohl J., May A., Aschmoneit I., Ell C. (2009) Double-balloon endoscopy for retrograde cholangiography in patients with choledochojejunostomy and Roux-en-Y reconstruction. Z Gastroenterol 47: 215–219 [DOI] [PubMed] [Google Scholar]
- Raithel M., Dormann H., Naegel A., Boxberger F., Hahn E., Neurath M., et al. (2011) Double-balloon-enteroscopy-based endoscopic retrograde cholangiopancreatography in post-surgical patients. World J Gastroenterol 17: 2302–2314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiner M., Chang L., Gluck M., Irani S., Gan S., Brandabur J., et al. (2012) Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc 75: 748–756 [DOI] [PubMed] [Google Scholar]
- Shah R., Smolkin M., Yen R., Ross A., Kozarek R., Howell D., et al. (2013) A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc 77: 593–600 [DOI] [PubMed] [Google Scholar]
- Shimatani M., Matsushita M., Takaoka M., Koyabu M., Ikeura T., Kato K., et al. (2009) Effective ‘short’ double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy 41: 849–854 [DOI] [PubMed] [Google Scholar]
- Siddiqui A., Chaaya A., Shelton C., Marmion J., Kowalski T., Loren D., et al. (2013) Utility of the short double-balloon enteroscope to perform pancreaticobiliary interventions in patients with surgically altered anatomy in a US multicenter study. Dig Dis Sci 58: 858–864 [DOI] [PubMed] [Google Scholar]
- Skinner M., Gutierrez J., Wilcox C., Mönkemüller K. (2013) Overtube-assisted placement of a metal stent into the bile duct of a patient with surgically altered upper-gastrointestinal anatomy during double-balloon enteroscopy-assisted ERCP. Endoscopy 45(Suppl. 2): E418–E419 [DOI] [PubMed] [Google Scholar]
- Skinner M., Popa D., Neumann H., Wilcox C., Mönkemüller K. (2014) ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy 46: 560-572 [DOI] [PubMed] [Google Scholar]
- Uyama I., Ogiwara H., Takahara T., Kato Y., Kikuchi K., Iida S. (1995) Laparoscopic Billroth I gastrectomy for gastric ulcer: technique and case report. Surg Laparosc Endosc 5: 209–213 [PubMed] [Google Scholar]
- Yamamoto H., Sekine Y., Sato Y., Higashizawa T., Miyata T., Iino S., et al. (2001) Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc 53: 216–220 [DOI] [PubMed] [Google Scholar]