Abstract
Despite calls for process-oriented models for child maladjustment due to heightened marital conflict in the context of parental depressive symptoms, few longitudinal tests of the mechanisms underlying these relations have been conducted. Addressing this gap, the present study examined multiple factors longitudinally that link parental depressive symptoms to adolescent adjustment problems, building on a conceptual model informed by emotional security theory (EST). Participants were 320 families (158 boys, 162 girls), including mothers and fathers, who took part when their children were in kindergarten (T1), second (T2), seventh (T3), eighth (T4) and ninth (T5) grades. Parental depressive symptoms (T1) were related to changes in adolescents’ externalizing and internalizing symptoms (T5), as mediated by parents’ negative emotional expressiveness (T2), marital conflict (T3), and emotional insecurity (T4). Evidence was thus advanced for emotional insecurity as an explanatory process in the context of parental depressive symptoms.
Keywords: depressive symptoms, marital conflict, emotional insecurity, explanatory process
Children of depressed parents are more likely to develop adjustment problems, including externalizing and internalizing problems, than children of nondepressed parents (Weissman, Warner, Wickramaratne, Moreau, & Olfson, 1997). Family influences, including marital conflict, are identified as factors in relations between parental depressive symptoms and child adjustment (e.g., Rice, Harold, Shelton, & Thapar, 2006). Although early reviews advanced that marital conflict factored importantly in these relations (Downey & Coyne, 1990), limited follow-up investigations are evident beyond studies providing further support for marital conflict as a risk factor for maladjustment (e.g., Murray et al., 2011; Nomura, Wickramaratne, Warner, Mufson, & Weissman, 2002). Despite calls for testing specific theoretical models for child adjustment due to marital conflict in the context of parental depressive symptoms (e.g., Cummings, Davies, & Campbell, 2000), few longitudinal tests have been conducted. The scant tests of process models are based upon cross-sectional or short-term longitudinal studies (e.g., Du Rocher Schudlich & Cummings, 2007), limiting inferences about longer-term outcomes. In this context, emotional security theory (EST, Davies & Cummings, 1994) is emerging as a promising explanatory model that provides a theoretical basis for explaining the impact of marital conflict on child adjustment (Cummings & Davies, 2010). The present report tests a theoretically-based model, derived from EST, for effects associated with parental depressive symptoms on child maladjustment spanning across childhood into adolescence.
Conceptual Model
Parents’ depressive symptoms are hypothesized to be related to adolescents’ internalizing and externalizing symptoms through pathways involving parental positive and negative emotional expressiveness, marital conflict, and emotional insecurity as explanatory constructs. Supporting a focus on depressive symptoms, subclinical as well as clinical levels of depressive symptoms are associated with risk for psychosocial dysfunction (Garber, 2006; Sheeber, Davis, Leve, Hops, & Tildesley, 2007). Parental depressive symptoms are predicted to be related to parents’ more negative and less positive emotionality in the family, fostering greater destructive interparental conflict. Destructive marital conflict, in turn, is hypothesized to be related to adolescents’ emotional insecurity, and, subsequently, internalizing and externalizing symptoms.
Parental Depressive Symptoms
Both paternal and maternal depressive symptoms and conflict behavior impact child adjustment (Ramchandani et al., 2008; Shelton & Harold, 2008). In a meta-analysis, Connell and Goodman (2002) found that both maternal and paternal depression were associated with children's internalizing and externalizing problems. In another meta-analysis, Kane and Garber (2004) reported moderate associations between paternal depression and children's internalizing and externalizing disorders. Relatedly, Kane and Garber (2009) found that paternal depressive symptoms were associated with adolescents’ externalizing and internalizing symptoms. Father-child conflict and negative communication mediated the link between paternal depressive symptoms and externalizing problems. Thus, depressive symptoms in both parents are linked with negative child outcomes (Jacob & Johnson, 1997; Low & Stocker, 2005; Reeb, Conger, & Wu, 2010; van Roekel et al., 2011). To account for the overall impact of parental depressive symptoms present in the family in predicting links with adolescent adjustment, mothers’ and fathers’ depressive symptoms are combined in this study.
Parental Emotional Expressiveness
The likelihood of more negative and less positive emotional expressiveness in the family is heightened in the context of parental depressive symptoms. Depressed adults exhibit heightened negative and low positive emotionality (Clark & Watson, 1991; Perils et al., 2005). Prior studies have indicated that negative emotional expressiveness in depressed adults is linked with children's dysregulation and maladjustment (Feng, Shaw, Skuban, & Lane, 2007; Goodman, Adamson, Riniti, & Cole, 1994). Parental negative emotionality is also related to negative child and family functioning (e.g., Fosco & Grych, 2007; Halberstadt, 1983; Laible, 2006; Wong, McElwain, & Halberstadt, 2009). Thus, both parental emotionality and expressiveness play important roles in relation to family processes and child adjustment.
Marital Conflict
Adult depression is linked to negative marital communications and marital conflict (Beach, Smith, & Fincham, 1994; Du Rocher Schudlich, Papp, & Cummings, 2004; 2011; Rehman, Ginting, Karimiha, & Goodnight, 2010; Whisman, 2001). Parental depressive symptoms and associated marital communications do not necessarily translate into greater destructive marital conflict. Rather, parental depression is expected to be related to marital conflict, as a function of parents’ negativity in the family. For example, resolved or constructive everyday disagreements may relate to positive, rather than negative, child outcomes including prosocial behavior over time (McCoy, Cummings, & Davies, 2009). However, evidence continues to mount that the risk for child maladjustment is increased because of destructive marital conflict in the context of parental depressive symptoms (e.g., Hanington, Heron, Stein, & Ramchandani, 2012; Keller, Cummings, Peterson, & Davies, 2009). Accordingly, we expect that negative emotional expressiveness in the home will play a role in heightening destructive marital conflict. In summary, we propose that parents’ negative emotional expressiveness in the family will be associated with children's risk for adjustment problems as a function of heightened marital conflict (Low & Stocker, 2005).
Children's Emotional Insecurity
Theoretically-based models for relations between marital conflict and adolescent functioning in the context of parental depressive symptoms have been little investigated. EST provides a theoretical model for the impact of parental depressive symptoms on child adjustment through marital conflict. In a cross-sectional study, emotional insecurity in response to marital conflict styles mediated relations between parental depressive symptoms and child maladjustment (e.g., Du Rocher Schudlich & Cummings, 2007). In another short-term longitudinal study, Kouros, Merrilees, and Cummings (2008) reported that marital conflict moderated with paternal depressive symptoms to predict children's emotional insecurity two year later. However, with regard to these issues, the findings to date are relatively complex and qualified, underscoring the need for further study.
According to EST, children's emotional security is related to their personal sense of protection and safety, which is among the most salient in a hierarchy of human goals (Waters & Cummings, 2000). An analogy is to think about emotional security as a bridge between the child and the world; high functioning interparental relations allow parents to serve as a secure base, supporting the child's exploration and relationships with others. When negative marital relations erode this ‘bridge’, children may lose confidence and become hesitant or uncertain how to move forward, unable to find appropriate footing within themselves or in interactions with others. A theoretical assumption is that preserving a sense of security is a goal that organizes children's ways of responding to marital conflict (e.g., behavioral dysfunction, involvement in conflict, avoidance).
Relations between Parental Depressive Symptoms and Adolescent Adjustment
There is evidence suggesting that parental depressive symptoms in early childhood have effects that last into later developmental periods (e.g. Nomura et al., 2002). However, questions remain about an explanatory mechanism accounting for such relations, including marital conflict and emotional insecurity. Tests of process models for these relations involving martial conflict over substantial periods of time have rarely been conducted. Such research is essential for advancing developmental models of explanatory mechanisms. This report examines relations between parental depressive symptoms and child adjustment in the marital context across childhood and adolescence. By utilizing a well-defined process model across major developmental periods, the present study also extends previous research by examining the long-term significance of parental depressive symptoms.
A developmental psychopathology model of emotional insecurity posits that experiential history of parental depressive symptoms and associated family processes may predict adolescent adjustment problems (Cummings, Davies, & Campbell, 2000). Developmental transformations across childhood and adolescence may amplify or dilute the magnitude of pathways among parental depressive symptoms, emotional insecurity, and maladjustment. Increases in coping repertoires in adolescence may be offset by greater risk for emotional insecurity. That is, relative to younger children, adolescent worries and security concerns may be elevated by their greater sensitivity to adult problems and their longer histories of exposure to family risk. Highlighting the significance of early adversity, Hammen and Brennan (2003) found that children exposed to maternal depression prior to 10 years of age were twice as likely to develop clinical depression as children of never-depressed mothers. With regards to postnatal depression, Murray and colleagues (2011) found that postnatally depressed mothers had children at risk for depression by 16 years of age, particularly when maternal depression had been accumulating for more than 17 months during the postnatal period.
The Current Study
This study examines relations between parental depressive symptoms and symptoms of adolescent maladjustment through a theoretically-based conceptual model. The impact of parents’ depressive symptoms is examined in the context of parental emotional expressiveness, marital conflict and children's insecurity about interparental relations (Cummings, Merrilees & George, 2010). Parental depressive symptoms (T1) and emotional expressiveness (T2) were assessed in early childhood, and marital conflict (T3), emotional insecurity (T4), and externalizing and internalizing problems (T5) were examined in adolescence. Parents’ negative emotionality in the family is expected to mediate relations between parental depressive symptoms and adjustment outcomes, both directly and by elevating marital conflict. Children's emotional insecurity about marital conflict is hypothesized to mediate relations between marital conflict and adolescents’ adjustment (Cummings & Davies, 2010). With regard to the theoretical model guiding this study, a central goal is to further test whether emotional insecurity serves as an explanatory variable for relations between parental depressive symptoms and child adjustment through pathways of heightened marital conflict. The stringency of this model test is increased by including autoregressive controls at T1 accounting for all of the variables subsequently included in model testing.
Method
Participants
Participants included 320 families (158 boys, 162 girls) taking part in a larger, dual-site longitudinal study, consisting of two cohorts of families. Families were recruited from communities in the Midwest and Northeast through flyers distributed to local schools, churches, community events, and neighborhoods. Families participated when children were in kindergarten (T1), second (T2), seventh (T3), eighth (T4), and ninth (T5) grades. The original cohort of families (n = 235; 108 boys, 127 girls; T1 M age = 6.00, SD= .45) were eligible to participate if they had a child in kindergarten, all three family members had been cohabitating for a minimum of three years, and all members were English proficient. A second cohort of families (n = 85; 50 boys, 35 girls; T3 M age = 12.75, SD = .55) was recruited to participate for an adolescence phase of the longitudinal study when the original sample of children were in seventh grade. This second cohort was designed to match the original cohort. Eligibility criteria for the supplemental cohort of families required that all three family members were cohabitating for a minimum of one year, had a child in the seventh grade, and were English proficient.
Families from both cohorts were recruited to be representative of the demographics of the communities from which they were drawn. Of participants, 72.77% were White, 17.46% were Black or African American, 4.05% were Hispanic, and 5.72% reported multiple or other racial and ethnic backgrounds. Most couples were married at recruitment (88.13%) and were the biological parent of the participating child (93.44% mothers, 83.44% fathers). At T1, the median of mother-reported family annual income ranged between $40,000-54,999 (n = 63) and at T3 between $55,000-74,999 (n = 60).
Supporting inclusion of the two cohorts in the research design, the cohort of supplemental families did not differ from families recruited during kindergarten on key demographics including race and ethnicity, relationship to the child, family income, parent education, and marital status at T3. In addition, supplemental families did not differ from the original cohort of families on key study variables at T3 including parental depressive symptoms, marital conflict, emotional insecurity, and child behavioral problems. Fathers and mothers in the new cohort (M = 42.21, SD = 7.97; M = 40.46, SD = 6.30, respectively) were younger compared to parents of the longitudinal families (M = 44.34, SD = 5.93, F(1,252) = 5.73, p <.05; M = 42.30, SD = 5.78, F(1,276) = 5.64, p <.05 respectively). Children in the new cohort (M = 12.75, SD= .55) were older than the longitudinal children (M = 12.58, SD = .57, F(1,267) = 5.39, p <.05). There was a larger percentage of male children in the supplemental cohort (n = 50, 58.82% male) compared to the original cohort (n = 108, 45.96% male; χ2(1) = 3.99, p<.05).
Of the families recruited during kindergarten, 93.6% (n = 220) were retained during the second grade assessment (T2). Of families participating at T2, 89.1% (n = 196) were retained at the seventh grade assessment (T3). Of families participating at T3, 95.9% (n = 188) were retained at the eighth grade assessment. Of families participating at T4, 95.2% (n = 179) were retained at the ninth grade assessment. Families retained at T5 did not differ from families lost to attrition on key demographic and study variables at T1 including parental depressive symptoms, marital conflict, positive emotional expressiveness, emotional insecurity, child behavioral problems, parent age, relationship to child, marital status, family income, race and ethnicity. Families lost to attrition by T5 had parents who reported higher levels of negative emotional expressiveness at the start of the study (M = 41.99, SD = 9.08) compared to families retained at T5 (M = 45.22, SD = 11.89), F(1, 234) = 4.68, p <.05.
Of the supplemental families recruited during the adolescent phase at T3, 88.2% (n = 75) were retained one year later at the T4 assessment. Of the supplemental families participating at T4, 92.0% (n = 69) were retained at the T5 assessment. Supplemental families lost to attrition at T5 did not differ at their recruitment (T3) from retained families on any demographic or study variables, including parental depressive symptoms, marital conflict, emotional insecurity, child behavioral problems, parent age, relationship to child, marital status, and family income.
Children's teachers were recruited to complete survey packets about the child. At T5, adolescents and mothers provided names of children's school teachers. At T5, 212 teachers (84.8% of participating families; Median grade level = 9) completed survey packets about the study child. T5 teachers reported knowing the child for an average of 13.25 months (SD = 9.87). Additionally, the majority of T5 teachers (95.7%) reported knowing the child moderately or very well.
Procedure
At each time point, families participated in two laboratory visits. Each visit lasted approximately two and half hours. At the start of each visit, informed consent or assent was obtained from each family member. Parents received monetary compensation for their participation and children received a small toy during childhood years and a gift card during the adolescent years. Study protocol was in accordance with the Institutional Review Boards at each site. Data for the present study was drawn from the kindergarten, second, seventh, eighth, and ninth grade time points. Data for the newly recruited families were included in the present analyses and full maximum likelihood estimation was used to utilize all available data.
Measures
Parental Depressive Symptoms
At T1, mothers and fathers completed the 20-item Center for Epidemiological Studies Depression scale (CES-D; Radloff, 1977) assessing depressive symptomotology in the past week. Participants responded on a scale from 0 (less than a day) to 3 (5-7 days) indicating how frequently the experienced each symptom over the last week; scores are summed with higher scores reflecting more depressive symptoms. The CES-D has good discriminant validity and moderate test-retest reliability (Radloff, 1977). The CES-D had good internal reliability in the current sample for mothers (α = .87) and fathers (α = .86). Scores of 16 or higher indicate clinical levels of depression. In the current sample, 16.67% of mothers and 13.73% of fathers scored in the clinical range of depressive symptoms at T1.
Parental Self-Expressiveness
At T1 and T2, mothers and fathers completed the 12-item negative emotional expressiveness subscale and the 12-item positive emotional expressiveness subscale of the Self-Expressiveness in the Family Questionnaire (SEFQ; Halberstadt, Cassidy, Stifter, Parke, & Fox, 1995) assessing the frequency in which each parent expresses negative and positive emotions in the family. Participants responded on a 9-point likert scale; items were summed with higher scores indicating more frequent expressions of negative and positive emotions. A composite parent-report of expressed emotion was created by averaging mother and father reports of expressiveness. The SEFQ had good internal reliability in the current study (parent-composite report for negative expressiveness at T1α = .87 and T2 α = .86; parent-composite report for positive expressiveness at T1 α = .91 and T2 α = .92).
Destructive Marital Conflict
At T1 and T3, mothers and fathers completed the O'Leary Porter Scale (OPS; Porter & O'Leary, 1980), a 9-item self-report measure of the frequency of overt hostility in the marital relationship that occurs in the presence of the child. Participants rated the frequency of hostility in the marital relationship on a 4-point likert scale with higher summed scores indicating more frequent hostility. The internal reliability for the current sample was α = 0.77 and α = 0.78 for T1 and T3 mother-report and α = 0.75 and α = 0.80 for T1 and T3 father-report for overt hostility, respectively.
Mothers and fathers also completed the frequency subscale of the Conflicts and Problem-Solving Scales (CPS; Kerig, 1996) at T1 and T3. The Frequency subscale is a two-item subscale measuring the frequency of both minor and major conflicts in the marital relationship on a six-point likert scale ranging from once a year or less to just about everyday. Scores on the major conflict score are weighted and the sum of both the frequency of major and minor conflicts is computed; scores on the frequency scale range from three to eighteen with higher scores indicating more frequent conflict. The CPS has good convergent and divergent validity (Kerig, 1996). The frequency scale of the CPS has adequate internal reliability for the current sample (mothers at T1 α =.76, T3 α = .71; fathers at T1 α = .75, T3 α = .67).
Emotional Insecurity
At T4, adolescents completed the Security in the Interparental Subscale (SIS; Davies, Forman, Rasi, & Stevens, 2002). The SIS measures different responses children have to witnessing marital conflict. Adolescents completed the Emotional Reactivity (9 items), Behavioral Dysregulation (3 items), and Destructive Internal Representations (4 items) subscales assessing different manifestations of emotional insecurity about the marital relationship. The Emotional Reactivity subscale assesses the degree to which children react emotionally (e.g., I feel angry; I feel scared) to conflict. The Behavioral Dysregulation subscale assesses the degree to which children respond behaviorally (e.g., I try to clown around or cause trouble; I yell at or say unkind things to people in my family) to marital disputes. The Destructive Internal Representations subscale assesses adolescent's destructive representations (e.g., I worry about my family's future; I worry about what they're going to do next)of the family. Adolescents rated each statement on a 4-point likert scale from 1 (not at all true of me) to 4 (very true of me); higher scores indicate more emotional insecurity. The SIS has good convergent and predictive validity (Davies, Forman, Rasi, & Stevens, 2002). The internal reliabilities for the current sample were emotional reactivity α = 0.88; behavioral dysregulation α = 0.43; and destructive representations α = 0.83. As Davies and colleagues (2002) suggested, the lower level of internal consistency for behavioral dysregulation may be attributable to its relatively fewer number of items (i.e., 3) consisted in the subscale.
At T1 mothers and fathers complete the Security in the Marital Subsystem scale (SIMS; Davies, Forman, Rasi, & Stevens, 2002). Parents completed the behavioral dysregulation subscale (5 items), which measured the use of aggressive or angry reactions to witnessing marital discord. The emotional reactivity subscale (10 items) measured the degree to which children responded emotionally (e.g., mad, scared) to marital disputes. Parents rated each response on a five point likert scale ranging from 1 (not at all like him/her) to 5 (a whole lot like him/her). Scores for each subscale were summed with higher scores indicating more emotional insecurity to witnessing marital conflict. The internal reliability for the current sample were mother-report of behavioral dysregulation α = .84, and emotional reactivity α =.74 and father-report of behavioral dysregulation α = .83, and emotional reactivity α =.71.
Child Internalizing and Externalizing Problems
At T1 and T5, mothers and fathers completed the internalizing and externalizing problems subscales of the Child Behavior Checklist (Achenbach, 1991). The internalizing problems subscale (30 items) reflects anxious, withdrawn, and depressive symptoms. The externalizing problems subscale (32 items) reflects delinquent and aggressive behaviors exhibited by the child. Parents rated children's behaviors on a 3-point likert scale, with higher scores indicating more problem behavior. The CBCL had good internal reliability for the current sample at both time points (Mothers: T1 Internalizing α = .84, T1 Externalizing α = .88, T4 Internalizing α = .83, T4 Externalizing α = .90; Fathers: T1 Internalizing α = .88, T1 Externalizing α = .90, T4 Internalizing α = .91, T4 Externalizing α = .90). T1 internalizing and externalizing problems were averaged to create a parent-report composite score and were included as autoregressive controls in the current study.
At T5, adolescents completed the CES-D as a self-report measure of depressive symptoms. The CES-D has been found to be suitable for assessing depression in adolescence (Radloff, 1991; Roberts, Andrews, Lewinsohn, & Hops, 1990). The CES-D had good internal reliability in the current sample (α = .89). Scores of 16 or higher indicate clinical levels of depression in adults. In the current sample, 23.4% of adolescents scored in the clinical range of depression at T5. At T5, adolescents also completed the Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1978) assessing anxiety symptoms. Adolescents stated whether each statement is true or not of them on a yes/no scales (37 items). The number of yes responses was summed with higher scores indicating higher levels of anxiety. The RCMAS has good construct validity and adequate reliability during adolescence (Reynolds, 1980; Reynolds & Paget, 1983). The RCMAS had good internal reliability in the current study (α = 0.86).
At T5, adolescents and teachers completed conducts problems subscale of the Strengths and Difficulties Questionnaire at each of the annual assessments (SDQ; Goodman, 1997) assessing adolescent conduct problems (5 items). Participants rated the items on a 3-point likert scale. Scores were summed and higher scores indicated more conduct problems. The SDQ conduct problem scale had adequate internal reliability in the current sample (adolescent report α = .64, teacher report α = .71). Although relatively low internal consistencies for the subscales SDQ are reported, the aim in scale construction was choosing items to maximize clinical significance as well as statistical consistency. Consistent with these goals, the SDQ subscales have been found to correlate more highly with interview-based ratings of clinical symptoms compared to the CBCL and discriminate between high and low risk samples, further supporting crierion validity.
Results
Table 1 shows the means, standard deviations, and correlations among all study variables. Maternal and paternal depressive symptoms were positively correlated (r = .21, p = .001). A paired-samples t-test was conducted to compare the level of depressive symptoms reported by fathers (M = 8.41; SD = 7.57) and mothers (M = 8.94; SD = 7.96). Results did not indicate a significant difference in reported depressive symptoms [t(231) = .88, ns]. Thus, a composite score of average parental depressive symptoms was used in the full model. In the larger longitudinal study, parents reported on their own depressive symptoms at T1, T3, T4, and T5. The average correlation of the parental composite of depressive symptoms across time was .48, all ps< .001. Parental depressive symptoms were relatively stable across time in this study; a repeated-measures analysis of variance indicated that composite levels of parental depression did not significantly change over the course of the study [F(3,157) = 1.91, ns]. Analysis of variance was conducted to examine the gender differences in T5 adjustment. Compared to boys, girls exhibited a higher level of self-reported depressive symptoms (Mgirls = 12.54, SDgirls = 9.84; Mboys = 9.60, SDboys = 8.54), F(1, 242) = 6.15, p < .05 and anxiety symptoms (Mgirls = 9.76, SDgirls = 5.72; Mboys = 7.35, SDboys = 5.14), F(1, 228) = 11.15, p < .01 and lower levels of maternal-reported externalizing problems (Mgirls = 2.52, SDgirls = 3.17; Mboys = 3.44, SDboys = 3.37), F(1, 240) = 4.79, p < .05. Girls and boys exhibited similar levels of paternal-reported externalizing symptoms and child- and teacher-reported conduct problems and similar levels of maternal- and paternal-reported internalizing problems at T5. Child gender was included as a covariate in the T5 internalizing and externalizing problems in the model.
Table 1.
Correlations and Descriptive Statistics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 PR Depressive | -- | |||||||||||||||||||||||||||||||
| 2. T1 PR NE | .41** | -- | ||||||||||||||||||||||||||||||
| 3. T1PR PE | −.25** | −.21** | -- | |||||||||||||||||||||||||||||
| 4. T2 PR NE | .32** | .60** | −.19** | -- | ||||||||||||||||||||||||||||
| 5. T2 PR PE | −.24** | −.17* | .66** | −.18** | -- | |||||||||||||||||||||||||||
| 6. T1 MR Hostility | .25** | .32** | −.09 | .27** | −.02 | -- | ||||||||||||||||||||||||||
| 7. T1 FR Hostility | .28** | .30** | −.08 | .17* | −.02 | .59** | -- | |||||||||||||||||||||||||
| 8. T1 MR Conflict Freq. | .25** | .32** | −.12 | .25** | −.07 | .61** | .37** | -- | ||||||||||||||||||||||||
| 9. T1 FR Conflict Freq. | .28** | .34** | −.16* | .31** | −.09 | .46** | .54** | .51** | -- | |||||||||||||||||||||||
| 10.T3 MR Hostility | .09 | .26** | −.06 | .29** | .03 | .45** | .25** | .31** | .17* | -- | ||||||||||||||||||||||
| 11. T3 FR Hostility | .21** | .33** | −.03 | .22** | .03 | .31** | .51** | .10 | .23** | .42** | -- | |||||||||||||||||||||
| 12. T3 MR Conflict Freq | .10 | .25** | −.06 | .27** | .03 | .31** | .27** | .36** | .30** | .57** | .32** | -- | ||||||||||||||||||||
| 13. T3 FR Conflict Freq | .10 | .18* | −.11 | .18* | −.06 | .21** | .32** | .25** | .41** | .33** | .51** | .42** | -- | |||||||||||||||||||
| 14. T1 MR Emo. React. | .24** | .34** | −.21** | .23** | −.16* | .19** | .11 | .15* | .15* | .07 | .07 | −.04 | .02 | -- | ||||||||||||||||||
| 15. T1 FR Emo. React. | .30** | .30** | −.30** | .20** | −.09 | .08 | .18** | .10 | .13 | .03 | .12 | .01 | .09 | .32** | -- | |||||||||||||||||
| 16. T1 MR Beh. Dysreg | .20** | .30** | −.16* | .19** | −.21** | .24** | .19** | .16* | .14* | .19** | .16* | .18* | .01 | .34** | .13 | |||||||||||||||||
| 17. T1 FR Beh. Dysreg | .14* | .28** | −.15* | .12 | −.01 | .11 | .20** | .02 | .08 | .12 | .24** | .12 | .08 | .25** | .43** | .33** | -- | |||||||||||||||
| 18. T4 CR Destruct Rep | .10 | .08 | .01 | .09 | .02 | .10 | .15 | .00 | .14 | .27** | .23** | .19** | .28** | .06 | .12 | .03 | .07 | -- | ||||||||||||||
| 19. T4 CR Emo. React. | .10 | .15 | −.11 | .17* | −.08 | −.04 | .05 | −.11 | .03 | .31** | .22** | .19** | .25** | .10 | .16 | .06 | .09 | .67** | -- | |||||||||||||
| 20. T4 CR Beh. Dysreg. | .05 | .12 | −.17* | .07 | −.13 | .16* | .04 | .11 | .15 | .18** | .09 | .10 | .15* | .07 | .07 | .11 | .05 | .32** | .29** | -- | ||||||||||||
| 21. T1 MR Internalizing | .22** | .31** | −.10 | .28** | −.16* | .19** | .05 | .15* | .04 | .21** | .17* | .09 | .05 | .27** | .12 | .19** | .12 | .01 | .06 | .03 | -- | |||||||||||
| 22. T1FR Internalizing | .25** | .27** | −.17** | .31** | −.19** | .05 | .13* | .10 | .16* | .10 | .20* | .09 | .11 | .27** | .20** | .16* | .19** | .19* | .19* | .03 | .49** | -- | ||||||||||
| 23. T5 MR Internalizing | .09 | .14 | −.01 | .20** | −.08 | .07 | −.04 | .06 | −.02 | .18** | .08 | .08 | .02 | .00 | −.03 | .17* | −.02 | .07 | .08 | −.03 | .44** | .20** | -- | |||||||||
| 24. T5 FR Internalizing | .09 | .17* | −.10 | .34** | −.15 | −.01 | .05 | .00 | .02 | .12 | .21** | .02 | .15* | .03 | −.01 | .05 | .06 | .29** | .19* | .12 | .25** | .40** | .44** | -- | ||||||||
| 25. T5 CR Depressive | .02 | −.08 | −.06 | −.03 | −.06 | .11 | .01 | .03 | −.04 | .16* | .15* | .02 | −.03 | −.02 | −.01 | .02 | −.05 | .26** | .25** | .25** | .02 | .10 | .27** | .19** | -- | |||||||
| 26. T5 CR Anxiety | −.02 | .02 | −.02 | .09 | −.04 | .03 | −.01 | .07 | .06 | .18** | .17* | .04 | .09 | −.05 | .05 | .14 | .05 | .27** | .29** | .08 | .10 | .09 | .37** | .24** | .66** | -- | ||||||
| 27. T1 MR Externalizing | .18** | .30** | −.11 | .24** | −.16* | .15* | .07 | .16* | .09 | .19** | .12 | .17* | .06 | .25** | .04 | .44** | .26** | .10 | .14 | −.02 | .62** | .30** | .33** | .15 | .04 | .17* | -- | |||||
| 28. T1 FR Externalizing | .20** | .38** | −.14* | .23** | −.19** | .01 | .13 | .09 | .14* | .01 | .10 | .10 | .07 | .24** | .14* | .35** | .33** | .23** | .27** | −.01 | .26** | .56** | .05 | .30** | .06 | .14 | .55** | -- | ||||
| 29. T5 MR Externalizing | .15* | .15* | −.06 | .20* | −.19* | .02 | −.08 | .07 | −.06 | .13 | −.02 | .17* | .04 | .10 | .03 | .29** | .09 | .12 | .12 | .08 | .23** | .11 | .54** | .37** | .16* | .19** | .46** | .32** | -- | |||
| 30. T5 FR Externalizing | .18* | .19* | −.05 | .34** | −.09 | .07 | .14 | .09 | .11 | .08 | .19** | .20** | .18** | .07 | .12 | .23** | .22** | .29** | .23** | .15* | .16 | .29** | .32** | .65** | .14 | .16* | .27** | .46** | .72** | -- | ||
| 31. T5 CR Conduct Prob | .10 | .04 | −.04 | .04 | −.04 | .11 | .06 | .04 | −.01 | .05 | .09 | −.03 | −.08 | .09 | .03 | .09 | .05 | .25** | .13 | .22** | −.12 | −.06 | .20** | .21** | .36** | .27** | .09 | .21** | .44** | .42** | -- | |
| 32. T5 TR Conduct Prob | .18* | .08 | −.04 | .09 | −.09 | .09 | .09 | .07 | .02 | .02 | .06 | .09 | −.06 | −.16 | −.04 | −.08 | −.09 | .21** | .18* | .04 | −.11 | .04 | −.03 | .19* | −.04 | −.07 | −.04 | .20* | .27** | .41** | .38** | -- |
| Mean | 8.66 | 42.77 | 79.99 | 3.32 | 6.76 | 12.09 | 11.65 | 8.22 | 8.14 | 1.10 | 1.11 | 5.84 | 5.43 | 16.69 | 16.19 | 8.05 | 8.05 | 5.44 | 13.74 | 3.53 | 2.25 | 2.37 | 1.64 | 1.63 | 11.12 | 8.61 | 4.84 | 5.46 | 2.97 | 3.23 | 1.82 | .44 |
| SD | 6.08 | 9.90 | 10.90 | .78 | .93 | 4.82 | 4.60 | 3.07 | 3.30 | .49 | .52 | 2.08 | 2.15 | 5.76 | 5.65 | 3.42 | 3.19 | 2.34 | 5.09 | 1.04 | 1.97 | 2.20 | 1.72 | 2.08 | 9.33 | 5.57 | 3.55 | 4.10 | 3.29 | 3.89 | 1.75 | 1.10 |
Note. PR = Parental-composite Report. MR = Mother Report. FR = Father Report. CR = Child Report. TR = Teacher Report.
p< .05
p< .01.
To examine the relations prospectively in a structural equation modeling framework, data were assessed from when the children were in kindergarten to when they were in the ninth grade to examine associations among parental depression at T1, parental positive and negative expressiveness at T2, marital conflict at T3, adolescent emotional insecurity at T4, and internalizing and externalizing problems at T5. MPLUS Version 7 (Muthén & Muthén, 1998-2012) was used with maximum likelihood method to examine the model fit to the observed variance and covariance matrices. Latent constructs were created for a) marital conflict using maternal and paternal reports of marital hostility and conflict frequency at T1 and T3, b) adolescents’ emotional insecurity using adolescent report of emotional reactivity, behavioral dysregulation, and destructive representations at T4 and maternal and paternal reports of emotional reactivity and behavioral dysregulation at T1, c) internalizing problems using maternal and paternal reports of internalizing problems at T5 and adolescent report of depressive and anxiety symptoms at T5, and d) externalizing problems using maternal and paternal reports of externalizing problems at T5 and adolescent and teacher reports of conduct problems at T5. T1 internalizing and externalizing problems were included as manifest variable autoregressive controls using composite reports of maternal and paternal reports of problems. Full information maximum likelihood estimation was used to handle missing data. Child gender and autoregressive effects of T1 were incorporated in the model to control for parents’ positive and negative emotional expressiveness, marital conflict, adolescents’ emotional insecurity, and internalizing and externalizing problems over time. To account for shared reporter variance on latent variables with multiple reporters, residual variances were allowed to correlate among manifest indicators of the same reporter for the marital conflict, emotional insecurity, and adjustment latent variables. Additionally, residual variances for child report of adjustment at T5 were allowed correlate. To account for shared measurement variance, residual variances were also allowed to correlate a) across time points on the same scale for the same reporter and b) across reporters on the same time point for the marital conflict and adjustment variables. Mediation effects were examined by bootstrapping, as this method can yield more accurate estimates of the standard error of the indirect effects than alternative approaches to testing mediation (Shrout & Bolger, 2002).
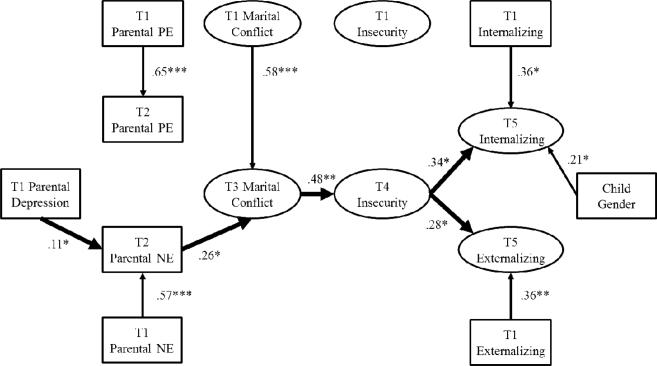
Findings indicated that the model fit was adequate, χ2(363) = 558.25, p < .001,CFI = .92, RMSEA = .04, SRMR = .07 (see Figure 1). With regard to specific pathways, Table 2 shows the unstandardized parameter estimates, bootstrap standard errors, and significance levels in the measurement and the structural models1. After controlling the effects of family processes at T1, T1 parental depressive symptoms significantly predicted T2 parental negative emotional expressiveness (β = .11, p < .05), which predicted subsequent marital conflict at T3 (β = .26, p < .05). In contrast, T1 parental depressive symptoms did not predict positive emotional expressiveness at T2, ns. Positive emotional expressiveness also did not predict subsequent marital conflict at T3, ns. T3 marital conflict predicted T4 adolescents’ emotional insecurity (β = .48, p < .01), which predicted subsequent T5 internalizing problems (β = .34, p <.05) and T5 externalizing problems (β = .28, p <.05).
Figure 1.
Model findings of overall T1 parental depressive symptoms, T2 parental negative and postive emotional expressiveness, T3 marital conflict, T4 adolescent emotional insecurity, and T5 adolescent internalizing and externalizing problems. , χ2(363) = 558.25, p < .001,CFI = .92, RMSEA = .04, SRMR = .07. Only significant pathways are depicted. Standardized parameter estimates are presented. Correlation and manifest indicators are omitted (See Table 2 for full model results). *p < .05. **p < .01. ***p < .001. T5 Internalizing Problems R2 = .34. T5 Externalizing Problems R2 = .27. NE = Negative Emotional Expressivess. PE = Postive Emotional Expressiveness.
Table 2.
Unstandardized Parameter Estimates of the Measurement and Structural Model of the Parental Depression Model Depicted in Figure 1.
| Parameter Estimate | Unstandardized (SE) | p-value |
|---|---|---|
| Measurement Model | ||
| T3 Marital Conflict → MR Marital Hostility | 1.00f | -- |
| T3 Marital Conflict → FR Marital Hostility | .95 (.32) | < .01 |
| T3 Marital Conflict → MR Conflict Frequency | 3.66 (1.04) | .00 |
| T3 Marital Conflict → FR Conflict Frequency | 3.75 (1.46) | .01 |
| T4 Emotional Insecurity → CR Destructive Representations | 1.00f | -- |
| T4 Emotional Insecurity → CR Emotional Reactivity | 1.90 (.36) | .00 |
| T4 Emotional Insecurity → CR Behavioral Dysregulation | .19 (.05) | .00 |
| T5 Internalizing Problems → MR Internalizing Problems | 1.00f | -- |
| T5 Internalizing Problems → FR Internalizing Problems | 1.23 (.54) | .02 |
| T5 Internalizing Problems → CR Depressive Symptoms | 3.47 (1.66) | .04 |
| T5 Internalizing Problems → CR Anxiety Symptoms | 2.66 (1.07) | .02 |
| T5 Externalizing Problems → MR Externalizing Problems | 1.00f | -- |
| T5 Externalizing Problems → FR Externalizing Problems | 1.28 (.21) | .00 |
| T5 Externalizing Problems → CR Externalizing Problems | .36 (.06) | .00 |
| T5 Externalizing Problems → TR Conduct Problems | .20 (.08) | .02 |
| Measurement Model – T1 Autoregressive Controls | ||
| T1 Marital Conflict → MR Marital Hostility | 1.00f | -- |
| T1 Marital Conflict → FR Marital Hostility | .87 (.18) | .00 |
| T1 Marital Conflict → MR Conflict Frequency | .57 (.11) | .00 |
| T1 Marital Conflict → FR Conflict Frequency | .65 (.15) | .00 |
| T1 Emotional Insecurity → MR Emotional Reactivity | 1.00f | -- |
| T1 Emotional Insecurity → FR Emotional Reactivity | .71 (.35) | < .01 |
| T1 Emotional Insecurity → MR Behavioral Dysregulation | .65 (.24) | < .01 |
| T1 Emotional Insecurity → FR Behavioral Dysregulation | .51 (.15) | < .01 |
| Structural Model | ||
| T1 Parental Depressive Symptoms → T2 Parental NE | .01 (.01) | .04 |
| T1 Parental Depressive Symptoms → T2 Parental PE | −.01 (.01) | .40 |
| T1 Parental Depressive Symptoms → T3 Marital Conflict | −.002 (.01) | .78 |
| T1 Parental Depressive Symptoms → T4 Emotional Security | −.01 (.04) | .83 |
| T1 Parental Depressive Symptoms → T5 Internalizing Probs | −.01 (.02) | .57 |
| T1 Parental Depressive Symptoms → T5 Externalizing Probs | .02 (.04) | .58 |
| T2 Parental NE → T3 Marital Conflict | .11 (.05) | .02 |
| T2 Parental NE → T4 Emotional Insecurity | −.12 (.31) | .69 |
| T2 Parental NE → T5 Internalizing Problems | .16 (.17) | .35 |
| T2 Parental NE → T5 Externalizing Problems | .39 (.41) | .34 |
| T2 Parental PE → T3 Marital Conflict | .05 (.03) | .11 |
| T2 Parental PE → T4 Emotional Insecurity | −.07 (.23) | .76 |
| T2 Parental PE → T5 Internalizing Problems | −.13 (.11) | .24 |
| T2 Parental PE → T5 Externalizing Problems | −.26 (.33) | .43 |
| T3 Marital Conflict → T4 Emotional Insecurity | 2.91 (1.02) | < .01 |
| T3 Marital Conflict → T5 Internalizing Problems | .03 (.60) | .96 |
| T3 Marital Conflict → T5 Externalizing Problems | −.67 (1.33) | .62 |
| T4 Emotional Insecurity → T5 Internalizing Problems | .17 (.07) | .02 |
| T4 Emotional Insecurity → T5 Externalizing Problems | .37 (.19) | < .05 |
| Child Gender → T5 Internalizing Problems | .43 (.21) | .04 |
| Child Gender → T5 Externalizing Problems | −.13 (.40) | .75 |
| Structural Model – Autoregressive Controls | ||
| T1 Parental NE → T2 Parental NE | .05 (.01) | .00 |
| T1 Parental PE → T2 Parental PE | .06 (.004) | .00 |
| T1 Marital Conflict → T3 Marital Conflict | .06 (.02) | < .01 |
| T1 Emotional Insecurity → T4 Emotional Insecurity | −.01 (.14) | .95 |
| T1 Internalizing Problems → T5 Internalizing Problems | .21 (.11) | .05 |
| T1 Externalizing Problems → T5 Externalizing Problems | .29 (.11) | .01 |
| Covariances | ||
| T1 Depressive Symptoms ↔ T1 Parental NE | 24.23 (4.52) | .00 |
| T1 Depressive Symptoms ↔ T1 Parental PE | −16.76 (4.20) | .00 |
| T1 Depressive Symptoms ↔ T1 Marital Conflict | 8.16 (2.13) | .00 |
| T1 Depressive Symptoms ↔ T1 Emotional Insecurity | 7.46 (2.37) | < .01 |
| T1 Depressive Symptoms ↔ T1 Internalizing Problems | 2.95 (.72) | .00 |
| T1 Depressive Symptoms ↔ T1 Externalizing Problems | 4.33 (1.31) | < .01 |
| T1 Parental NE ↔ T1 Parental PE | −22.70 (7.93) | < .01 |
| T1 Parental NE ↔ T1 Marital Conflict | 16.60 (4.19) | .00 |
| T1 Parental NE ↔ T1 Emotional Insecurity | 17.83 (4.81) | .00 |
| T1 Parental NE ↔ T1 Internalizing Problems | 6.00 (1.44) | .00 |
| T1 Parental NE ↔ T1 Externalizing Problems | 10.88 (3.27) | < .01 |
| T1 Parental PE ↔ T1 Marital Conflict | −6.39 (3.28) | .05 |
| T1 Parental PE ↔ T1 Emotional Insecurity | −12.42 (4.59) | < .01 |
| T1 Parental PE ↔ T1 Internalizing Problems | −2.99 (1.25) | .02 |
| T1 Parental PE ↔ T1 Externalizing Problems | −4.87 (2.50) | .05 |
| T1 Marital Conflict ↔ T1 Emotional Insecurity | 4.52 (1.77) | .01 |
| T1 Marital Conflict ↔ T1 Internalizing Problems | 1.31 (.65) | < .05 |
| T1 Marital Conflict ↔ T1 Externalizing Problems | 2.21 (1.21) | .07 |
| T1 Emotional Insecurity ↔ T1 Internalizing Problems | 2.46 (.83) | < .01 |
| T1 Emotional Insecurity ↔ T1 Externalizing Problems | 6.43 (1.45) | .00 |
| T1 Internalizing Problems ↔ T1 Externalizing Problems | 3.34 (.60) | .00 |
| Child Gender ↔ T1 Depressive Symptoms | −.17 (.23) | .47 |
| Child Gender ↔ T1 Parental NE | −.24 (.39) | .54 |
| Child Gender ↔ T1 Parental PE | −.18 (.40) | .66 |
| Child Gender ↔ T1 Marital Conflict | .08 (.15) | .59 |
| Child Gender ↔ T1 Emotional Insecurity | −.33 (.17) | .05 |
| Child Gender ↔ T1 Internalizing Problems | .002 (.07) | .98 |
| Child Gender ↔ T1 Externalizing Problems | −.41 (.12) | .00 |
| W6 Internalizing Problems ↔ W6 Externalizing Problems | 1.15 (.54) | .03 |
Note. Bolded values indicate significant parameters. MR = Mother Report; FR = Father Report; TR = Teacher Report; CR = Child Report; NE = Negative Emotional Expressiveness. PE = Positive Emotional Expressiveness.
indicates fixed factor loadings.
To test for mediation effects, bootstrapping was conducted. Specifically, the indirect effects of parental depressive symptoms on parental negative expressiveness, marital conflict, adolescent emotional insecurity, and internalizing and externalizing problems were examined. Using the current data, the 95% confidence interval [CI] based on 1000 bootstrap samples with replacement indicated that the indirect effects of parental depressive symptoms on adolescents’ internalizing and externalizing problems included zeros, indicating that altogether, parental negative expressiveness, marital conflict and emotional insecurity did not mediate the linkage between parental depressive symptoms and adolescent behavior problems. Next specific indirect pathways were examined, the 95% confidence interval [CI] based on 1000 bootstrap samples with replacement indicated that the specific indirect effect of parental depressive symptoms on adolescents’ emotional insecurity did not include a zero (95% CI: .001, .018), providing support for parental negative emotional expressiveness and marital conflict as significant mediators between parental depressive symptoms and adolescent insecurity. The 95% confidence interval [CI] based on 1000 bootstrap samples with replacement indicated that the specific indirect effects of parental negative emotional expressiveness on adolescent internalizing and externalizing problems did not include zeros (95% CI: .014, .212; 95% CI: .016, .544, respectively), supporting the mediating roles of marital conflict and emotional insecurity between parental negative expressiveness and adolescent adjustment. Finally, to further establish the temporal relationship between study variables, we ran the model in the opposite direction. For example, we tested whether child internalizing or externalizing symptoms related to parental negative expressiveness, marital conflict, or emotional insecurity. None of these relations were statistically significant.
Discussion
The findings thus supported a specific theoretically-based model for the effects of marital conflict associated with parental depressive symptoms on children's maladjustment spanning across childhood and into adolescence. Emotional insecurity was related to adolescent adjustment in the context of a broader conceptual model of family risk, advancing evidence for emotional insecurity as an explanatory process associated with the effects of heightened marital conflict due to the presence of parental depressive symptoms. This report adds to the evidence for the impact of parents’ depressive symptoms on children's insecurity about interparental relations. Parents’ depressive symptoms were related to changes in adolescents’ behavior problems over time, as mediated by a chain of relations involving children's emotional insecurity about marital conflict. The findings thus extend support for emotional insecurity in explanatory models based on cross-sectional tests (Du Rocher Schudlich & Cummings, 2007) and short-term longitudinal tests (Kouros et al., 2008).
The results also build upon a study by Cummings, Cheung, and Davies (2013), which reported short-term longitudinal support for relations between parents’ depressive symptoms when children were in kindergarten and children's elevated internalizing symptoms in second grade, with parental negative emotional expressiveness and emotional insecurity as mediating variables. The present study importantly extends this investigation by also including (a) marital conflict and (b) externalizing symptoms in the conceptual model, (c) assessing emotional insecurity and adjustment at different points in time (i.e., eighth and ninth grades, respectively), and (d) predicting over a longer time course through adolescence. Moreover, the present study provides one of the few tests supporting process models for these relations across developmental periods (i.e., childhood and adolescence).
This study also demonstrated the role of children's regulatory processes (i.e., emotional insecurity) associated with parental depressive symptoms and their internalizing and externalizing problems. Indexed by specific classes of behavioral responses, the emotional security system included emotional reactivity, destructive internal representations, and behavioral dysregulation. Heightened emotional and behavioral reactivity associated with emotional insecurity may increase children's vulnerability to developing psychological symptoms over time. For example, prolonged operation of the emotional security system, including preoccupation, vigilance, and distress associated with destructive exchanges between parents, requires considerable expenditure of psychobiological resources, leaving children with fewer resources for coping with threats, challenges, and stressors.
The findings add to accumulating evidence for the impact of parents’ depressive symptoms on the development of their children. The results also highlight the role of negative, but not positive, emotional expressiveness in the family associated with parental depressive symptoms in links with heightened marital conflict. By identifying links between parental depressive symptoms in early childhood and changes in adolescent adjustment, this study indicates potential long-term implications of parental depression. In addition, the current findings are consistent with the notion that the negative impact of depressive symptoms on the child and family is related to the extent to which parents’ negative emotional expressiveness is elevated. Links between parental depressive symptoms and marital conflict may be more likely when depressive symptoms are associated with expressed negative emotion. In predicting change in children's behavior problems, the current findings underscore the significance of negative family emotional environment and children's regulatory processes associated with emotional insecurity.
The present study indicated indirect effects prospectively, consistent with the predictions of our developmental model. Parental depressive symptoms were longitudinally linked with adjustment problems via negative emotional expressiveness, marital conflict, and emotional insecurity. Parental depression ultimately undermined adolescent internalizing and externalizing symptoms by setting in motion dysfunctional familial expressions of negative emotions and insecure response processes in the child. A goal for future research is disentangling these longitudinal effects over time as a function of parent gender.
Limitations of the study merit consideration. Autoregressive controls were limited to T1. Autoregressive control across time points would further improve the robustness of the model in future studies (Cole & Maxwell, 2003). The inclusion of tested variables across multiple time points may better identify when a particular effect is the most prominent to child adjustment. For example, depression is a recurrent condition, with episodes lasting from two months to several years (Lehmann, 1983). The inclusion of parental depressive symptoms across time would allow researchers to pinpoint whether proximal or distal depressive symptoms are more predictive of child adjustment. Next, although the fit indices for the structural equation model were adequate, they were not excellent by current standards and should be interpreted with caution. Specific indicators for several constructs changed over time in the context of this longitudinal model test. In particular, we utilized different measures of the same constructs across time in some instances (e.g., emotional security, internalizing, and externalizing problems) to better assess variables in a developmentally appropriate manner. In this context we cannot test or establish measurement invariance, which is a limitation. The structural model should, therefore, be interpreted with caution. The internal consistency for some manifest variables (e.g., conduct problems on the SDQ) is lower than typically regarded as acceptable. To further explore the directionality and predictability of change, future studies may utilize latent change models (McArdle, 2009).
Although the addition of a supplementary cohort (n = 85) increased the statistical power of the analyses, we did not have data for parental depressive symptoms and emotional expressiveness from these participants during childhood. However, recruitment criteria for the additional cohort were designed to match the original cohort and the demographics at both sites. Although the samples did not differ on most demographic and study variables, supporting the combination of these samples, future studies should replicate the current SEM findings using a larger sample size, with a consistent cohort of families.
In terms of implications, findings were based on representative community samples, and thus may not be generalizable to clinical samples, families facing substantial hardships, or more ethnically diverse samples. Moreover, structured interviews or observational measures of parental depressive symptoms and marital conflict would further strengthen these constructs. Despite these limitations, this multi-reporter, prospective study addresses gaps in understanding specific pathways associated with emotional insecurity about interparental relations between parental depressive symptoms and child internalizing symptoms.
These findings have implications for intervention and prevention efforts, as well as clinical practice. The importance of parents’ emotional behaviors associated with depressive symptoms was underscored. Both parents should be made aware of their expressions of emotions and marital conflict in the family in relation to children's appraisals of safety and security. Psycho-educational approaches hold promise for helping parents learn better ways to communicate their feelings with each other (Cummings & Schatz, 2012). Parents may be able to reduce children's risk for emotional insecurity and adjustment problems by altering their pattern of emotional expression or conflict resolution towards other family members. For example, specific mechanisms addressed in the Cummings and Schatz (2012) protocol for a community-based program, pertinent to the current findings, included improving the quality of marital and family conflict and increasing children's emotional security about interparental and parent-child relationships. Amidst the complex mix of factors associated with parental depressive symptoms, the present study further illuminates factors affecting children's adjustment. Psychological interventions geared toward improving emotional communications and conflict resolution in the family by parents with depressive symptoms merits future investigation.
Footnotes
Further analyses were conducted to examine a model that excluded variables without significant contributions to the pathways of interest. A reduced model with T1 and T2 positive emotional expressiveness and T1 emotional insecurity removed from analyses resulted in similar findings, in which significant pathways remained significant and fit indices were comparable (reduced model: χ2(224) = 347.01, p < .001, CFI = .94, RMSEA = .04, SRMR = .06). The full model was retained for inclusion of these theory-driven constructs.
Contributor Information
E. Mark Cummings, University of Notre Dame.
Rebecca Y. M. Cheung, University of Notre Dame
Kalsea Koss, Institute of Child Development, University of Minnesota.
Patrick T. Davies, University of Rochester
References
- Achenbach TM. Manual for the Child Behavior Checklist: 4-18 and 1991 Profile. University of Vermont Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Beach SRH, Smith DA, Fincham FD. Marital interventions for depression: Empirical foundation and future prospects. Applied & Preventive Psychology. 1994;3:233–250. doi:10.1016/S0962-1849(05)80097-6. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. doi: 10.1037/0021843X.100.3.316. [DOI] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children's internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. doi:10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Cheung RYM, Davies P. Prospective relations between parental depression, negative expressiveness, emotional insecurity, and children's internalizing symptoms. Child Psychiatry and Human Development. 2013;44(6):698–708. doi: 10.1007/s10578-013-0362-1. doi: 10.1007/s10578-013-0362-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. The Guilford Press; New York: 2010. [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental psychopathology and family process: Theory, research, and clinical implications. Guilford Publications, Inc; New York: 2000. [Google Scholar]
- Cummings EM, Merrilees CE, George MW. Fathers, marriages, and families: Revisiting and updating the framework for fathering in family context. In: Lamb ME, editor. The role of the father in child development. 5thEd. John Wiley & Sons, Inc.; New York: 2010. pp. 154–176. [Google Scholar]
- Cummings EM, Schatz JN. Family conflict, emotional security, and child development: Translating research findings into a prevention program for community families. Clinical Child and Family Psychology Review. 2012;15:14–27. doi: 10.1007/s10567-012-0112-0. [DOI] [PubMed] [Google Scholar]
- Davies PT, Cummings EM. Marital conflict and child adjustment: An emotional security hypothesis. Psychological Bulletin. 1994;116:387–411. doi: 10.1037/0033-2909.116.3.387. doi: 10.1037/0033-2909.116.3.387. [DOI] [PubMed] [Google Scholar]
- Davies PT, Forman EM, Rasi JA, Stevens KI. Assessing children's emotional security in the interparental relationship: The security in the interparental subsystem scales. Child Development. 2002;73:544–562. doi: 10.1111/1467-8624.00423. doi:10.1111/1467-8624.00423. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Cummings EM. Parental dysphoria and children's adjustment: Marital conflict styles, children's emotional security, and parenting as mediators of risk. Journal of Abnormal Child Psychology. 2007;35:627–639. doi: 10.1007/s10802-007-9118-3. doi: 10.1007/s10802-007-9118-3. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, Cummings E. Relations of husbands’ and wives’ dysphoria to marital conflict resolution strategies. Journal of Family Psychology. 2004;18:171–183. doi: 10.1037/0893-3200.18.1.171. doi:10.1037/0893-3200.18.1.171. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, Cummings EM. Relations between spouses’ depressive symptoms and marital conflict: A longitudinal investigation of the role of conflict resolution styles. Journal of Family Psychology. 2011;25:531–540. doi: 10.1037/a0024216. doi: 10.1037/a0024216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Skuban EM, Lane T. Emotional exchange in mother-child dyads: Stability, mutual influence, and associations with maternal depression and child problem behavior. Journal of Family Psychology. 2007;21:714–725. doi: 10.1037/0893-3200.21.4.714. doi: 10.1037/08933200.21.4.714. [DOI] [PubMed] [Google Scholar]
- Fosco GM, Grych JH. Emotional expression in the family as a context for children's appraisals of interparental conflict. Journal of Family Psychology. 2007;21:248–258. doi: 10.1037/0893-3200.21.2.248. [DOI] [PubMed] [Google Scholar]
- Garber J. Depression in children and adolescents: Linking risk research and prevention. American Journal of Preventative Medicine. 2006;31:S104–S125. doi: 10.1016/j.amepre.2006.07.007. doi: 10.1016/j.amepre.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Child Psychology & Psychiatry & Allied Disciplines. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Adamson LB, Riniti J, Cole S. Mothers’ expressed attitudes: Associations with maternal depression and children's self-esteem and psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1265–1274. doi: 10.1097/00004583-199411000-00007. doi: 10.1097/00004583-199411000-00007. [DOI] [PubMed] [Google Scholar]
- Halberstadt AG. Family expressiveness styles and nonverbal communication skills. Journal of Nonverbal Behavior. 1983;8:14–26. doi: 10.1007/BF00986327. [Google Scholar]
- Halberstadt AG, Cassidy J, Stifter CA, Parke RD, Fox NA. Self expressiveness within the family context: Psychometric support for a new measure. Psychological Assessment. 1995;7:93–103. doi: 10.1037/1040-3590.7.1.93. [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry. 2003;60(3):253–258. doi: 10.1001/archpsyc.60.3.253. doi: 1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hanington L, Heron J, Stein A, Ramchandani P. Parental depression and child outcomes – is marital conflict the missing link? Child: Care, Health and Development. 2012;38:520–529. doi: 10.1111/j.1365-2214.2011.01270.x. doi:10.1111/j.1365-2214.2011.01270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Johnson SL. Parent–child interaction among depressed fathers and mothers: Impact on child functioning. Journal of Family Psychology. 1997;11:391–409. doi:10.1037/0893-3200.11.4.391. [PubMed] [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children's psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. doi:10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kane P, Garber J. Parental depression and child externalizing and internalizing symptoms: Unique effects of fathers’ symptoms and perceived conflict as a mediator. Journal of Child and Family Studies. 2009;18:465–472. doi:10.1007/s10826-008-9250-x. [Google Scholar]
- Keller PS, Cummings EM, Peterson KM, Davies PT. Marital conflict in the context of parental depressive symptoms: Implications for the development of children's adjustment problems. Social Development. 2009;18:536–555. doi: 10.1111/j.1467-9507.2008.00509.x. doi:10.1111/j.1467-9507.2008.00509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerig PK. Assessing the links between interparental conflict and child adjustment: The conflicts and problem-solving scales. Journal of Family Psychology. 1996;10:454–473. doi:10.1037/0893-3200.10.4.454. [Google Scholar]
- Kouros CD, Merriless CE, Cummings EM. Marital conflict and children's emotional security in the context of parental depression. Journal of Marriage and Family. 2008;70:684–697. doi: 10.1111/j.1741-3737.2008.00514.x. doi:10.1111/j.1741-3737.2008.00514.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laible D. Maternal emotional expressiveness and attachment security: Links to representations of relationships and social behavior. Merrill Palmer Quarterly. 2006;52:645–670. doi:10.1353/mpq.2006.0035. [Google Scholar]
- Lehmann HE. Clinical evaluation and natural course of depression. Journal of Clinical Psychiatry. 1983;44:5–10. [PubMed] [Google Scholar]
- Low SM, Stocker C. Family functioning and children's adjustment: Associations among parents' depressed mood, marital hostility, parent-child hostility, and children's adjustment. Journal of Family Psychology. 2005;19:394–403. doi: 10.1037/0893-3200.19.3.394. doi:10.1037/0893-3200.19.3.394. [DOI] [PubMed] [Google Scholar]
- McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annual review of psychology. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- McCoy K, Cummings EM, Davies PT. Constructive and destructive marital conflict, emotional security and children's prosocial behavior. Journal of Child Psychology and Psychiatry. 2009;50:270–279. doi: 10.1111/j.1469-7610.2008.01945.x. doi: 10.1111/j.1469-7610.2008.01945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, Cooper P. Maternal postnatal depression and the development of depression in offspring up to 16 years of age. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:460–470. doi: 10.1016/j.jaac.2011.02.001. doi: 10.1016/j.jaac.2011.02.001. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Sixth Edition. Muthén & Muthén; Los Angeles, CA: 1998-2012. [Google Scholar]
- Nomura Y, Wickramaratne PJ, Warner V, Mufson L, Weissman MM. Family discord, parental depression and psychopathology in offspring: Ten-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:402–409. doi: 10.1097/00004583-200204000-00012. doi: 10.1097/00004583-200204000-00012. [DOI] [PubMed] [Google Scholar]
- Perils RH, Fraguas R, Fava M, Trivedi MH, Luther JF, Wisniewski SR, Rush AJ. Prevalence and clinical correlates of irritability in major depressive disorder: A preliminary report from the sequenced treatment alternatives to relieve depression study. Journal of Clinical Psychiatry. 2005;66:159–166. doi:10.4088/JCP.v66n0202. [PubMed] [Google Scholar]
- Porter B, O'Leary KD. Marital discord and childhood behavior problems. Journal of Abnormal Child Psychology. 1980;8:287–295. doi: 10.1007/BF00916376. doi: 10.1007/BF00916376. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Radloff LS. The use of the center for epidemiologic studies depression scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. doi:10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Ramchandani PG, O'Connor TG, Evans J, Heron J, Murray L, Stein A. The effects of pre- and postnatal depression in fathers: A natural experiment comparing the effects of exposure to depression on offspring. Journal of Child Psychology & Psychiatry. 2008;49:1069–1078. doi: 10.1111/j.1469-7610.2008.02000.x. doi:10.1111/j.1469-7610.2008.02000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeb BT, Conger KJ, Wu EY. Paternal depressive symptoms and adolescent functioning: The moderating effect of gender and father hostility. Fathering. 2010;8:131–142. doi: 10.3149/fth.0801.131. doi: 10.3149/fth.0801.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehman US, Ginting J, Karimiha G, Goodnight JA. Revisiting the relationship between depressive symptoms and marital communication using an experimental paradigm: The moderating effect of acute sad mood. Behaviour Research and Therapy. 2010;48:97–105. doi: 10.1016/j.brat.2009.09.013. doi: 10.1016/j.brat.2009.09.013. [DOI] [PubMed] [Google Scholar]
- Reynolds CR. Concurrent validity of what I think and feel: The revised children's manifest anxiety scale. Journal of Consulting and Clinical Psychology. 1980;48:774–775. doi: 10.1037//0022-006x.48.6.774. doi: 10.1037/0022-006X.48.6.774. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Paget KD. National normative and reliability data for the revised children's manifest anxiety scale. School Psychology Review. 1983;12(3):324–336. [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children's manifest anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Rice F, Harold GT, Shelton KH, Thapar A. Family conflict interacts with genetic liability in predicting childhood and adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:841–848. doi: 10.1097/01.chi.0000219834.08602.44. doi: 10.1097/01.chi.0000219834.08602.44. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the center for epidemiologic studies depression scale. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2:122–128. doi: 10.1037/1040-3590.2.2.122. [Google Scholar]
- Sheeber LB, Davis B, Leve C, Hops H, Tildesley E. Adolescents’ relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton KH, Harold GT. Interparental conflict, negative parenting, and children's adjustment: Bridging links between parents’ depression and children's psychological distress. Journal of Family Psychology. 2008;5:712–724. doi: 10.1037/a0013515. doi:10.1037/a0013515. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. doi:10.1037/1082-989X.7.4.422. [PubMed] [Google Scholar]
- van Roekel E, Engels RCME, Verhagen M, Goossens L, Scholte RHJ. Parental depressive feelings, parental support, and the serotonin transporter gene as predictors of adolescent depressive feelings: A latent growth curve analysis. Journal of Youth and Adolescence. 2011;40:453–462. doi: 10.1007/s10964-010-9560-3. doi: 10.1007/s10964-010-9560-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters E, Cummings EM. A secure base from which to explore close relationships. Child Development. 2000;49:164–172. doi: 10.1111/1467-8624.00130. doi:10.1111/1467-8624.00130. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents: 10 years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. Retrieved from http://search.proquest.com/docview/619195536?accountid=12874. [DOI] [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. American Psychological Association; Washington, DC: 2001. pp. 3–24. [Google Scholar]
- Wong MS, McElwain NL, Halberstadt AG. Parent, family, and child characteristics: Associations with mother- and father-reported emotion socialization practices. Journal of Family Psychology. 2009;23:452–463. doi: 10.1037/a0015552. doi:10.1037/a0015552. [DOI] [PubMed] [Google Scholar]