Abstract
Objectives
This systematic review and meta-analysis was conducted to determine the mid- to long-term clinical outcomes for a medial-pivot total knee replacement (TKR) system. The objectives were to synthesise available survivorship, Knee Society Scores (KSS), and reasons for revision for this system.
Methods
A systematic search was conducted of two online databases to identify sources of survivorship, KSS, and reasons for revision. Survivorship results were compared with values in the National Joint Registry of England, Wales, and Northern Ireland (NJR).
Results
A total of eight studies that included data for 1146 TKRs performed in six countries satisfied the inclusion/exclusion criteria. Pooled component survivorship estimates were 99.2% (95% CI, 97.7 to 99.7) and 97.6% (95% CI, 95.8 to 98.6) at five and eight years, respectively. Survivorship was similar or better when compared with rates reported for all cemented TKRs combined in the NJR and was significantly better than some insert types at mid-term intervals. The weighted mean post-operative KSS was 87.9 (73.2 to 94.2), in the excellent range. Similar cumulative revision rates and KSS were reported at centres in the United States, Europe, and Asia.
Conclusions
The subject system was associated with survivorship and KSS similar or better than that reported for other TKR systems.
Cite this article: Bone Joint Res 2014;3:297–304
Keywords: Total knee arthroplasty, Meta-analysis, Systematic review, Medial-pivot
Article focus
To synthesise available survivorship, Knee Society Scores (KSS), and reasons for revision for a medial-pivot total knee replacement (TKR) system.
Key messages
The subject system was associated with survivorship and KSS similar to or better than that reported for other TKR systems.
An evaluation of reasons for revision did not indicate an increase in revisions due to the unique tibial insert articulation.
Similar low cumulative revision rates and KSS in the excellent range were achieved in patients from the United States, Europe, and Asia.
Strengths and limitations
This is the first systematic review and meta-analysis for outcomes associated with a TKR system based upon the medial-pivot philosophy.
Data synthesised in this review are from various sources including over 1100 patients implanted at 12 centres in six different countries.
A study limitation was that registry data were used as a comparator, which includes data for surgeons of all skill levels and product experience.
Introduction
Total knee replacement (TKR) is one of the most frequently performed orthopaedic surgeries worldwide and demand is expected to grow to as high as 3.48 million procedures per year by 2030 in the United States alone.1 TKR is generally associated with high component survivorship, with the National Joint Registry of England, Wales and Northern Ireland (NJR) reporting 96.8% survival for all cemented TKRs combined at nine years’ follow-up.2 Despite this relatively high survivorship, certain failure modes, such as instability, persist. Instability accounted for 14% of all TKR revisions reported to the NJR in 2012.2
The ADVANCE Medial-Pivot System (MicroPort Orthopedics Inc., Arlington, Tennessee), formerly marketed by Wright Medical Technology Inc., was introduced in 1998 with the intention of providing increased stability and kinematics that mimic those of a natural knee (Fig. 1). The medial-pivot design features an asymmetrical tibial insert that controls the anterior-posterior translation of the femur in the medial compartment, while allowing unrestricted movement of the femur in the lateral compartment. This results in the lateral condyle pivoting around the medial condyle to create movement similar to that of the normal knee.3,4
Fig. 1.

Image of the ADVANCE Medial-Pivot System (image courtesy of MicroPort Orthopedics Inc., Arlington, Tenessee).
Many available TKR systems are designed based on the four-bar link theory and feature J-curved femoral components. These designs are intended to recreate the femoral rollback of the natural knee, but can actually lead to anterior femoral sliding or ‘paradoxical motion’.3,5 The ADVANCE Medial-Pivot System features both anterior and posterior lips in the medial compartment intended to replace the posterior cruciate ligament (PCL) and anterior cruciate ligament (ACL), respectively, and prevent paradoxical movement. Studies have linked this system to the ability to perform highly demanding tasks in terms of knee stability, such as rising from a chair without compensation from their non-operated limbs6 and increased patient preference over posterior-stabilised (PS), mobile bearing, and PCL-retaining implant designs.7
While these outcomes are important and may play a role in patient satisfaction, it is also necessary to have evidence of traditional measures of clinical success such as component survivorship and functional outcome scores. This has become increasingly significant as healthcare systems worldwide move towards evidence-based medicine. The objectives of this systematic review and meta-analysis were to synthesise available component survivorship, Knee Society Scores (KSS), and evaluate any reported reasons for revision for this system.
Materials and Methods
Search strategy
A protocol-driven, systematic search of the PubMed and Google Scholar online databases was conducted in accordance with the PRISMA statement.8 The following terms were searched in both databases: 1) “wright medical” “advance” “total knee”; 2) “wright medical” “advance” “medial pivot”; 3) “wright medical” “advance” “knee arthroplasty”; 4) “medial pivot” “long-term”; 5) “medial pivot” “medium-term”; and 6) “medial pivot” “mid-term”. There were no limitations used in the PubMed database, with the exception of the use of quotations, which forced the database to look for the exact search terms. During the Google Scholar searches, quotations were again used and the “include citations” and “include patents” boxes were left unchecked.
Inclusion/exclusion criteria
To be included, studies had to report component survivorship or post-operative KSS9 for patients undergoing primary TKR with the subject system. If results for a cohort were reported in multiple citations, only the source with the longest follow-up was included. Case reports, articles not written in the English language, articles not related to the subject system, articles focusing only on treating specialised populations (e.g. fractures, trauma), and articles not appearing in peer-reviewed journals (e.g. conference proceedings) were excluded.
Article selection
The six searches were performed in both online databases on October 29, 2013. Evaluation of articles for inclusion was conducted by two reviewers (DAF and KS). The results were reviewed and duplicate citations were removed. The title of each unique citation was then reviewed and any citation unrelated to the subject system or TKR was removed. The abstracts of the remaining citations were reviewed, and any not satisfying the inclusion/exclusion criteria were removed. Finally, the full-text articles of the remaining citations were reviewed. Disagreements in article inclusion at each phase were resolved by the reviewers meeting and gaining consensus. Figure 2 provides details of the search and selection process.
Fig. 2.
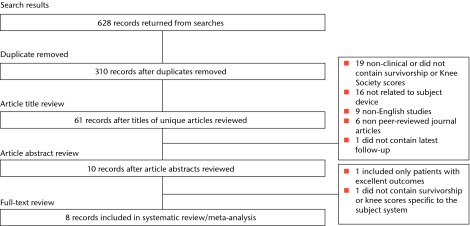
Diagram showing the search and selection process for the systematic review
Data extraction
Relevant data were extracted and included number of TKRs; mean follow-up; demographics (mean age, percentage female patients, percentage osteoarthritic patients, percentage TKRs with cement fixation, percentage bilateral patients); survivorship estimates; KSS; number of revisions and the reasons for any revisions. Data were verified by both reviewers (DAF and KS).
Statistical analysis
Reviewer agreement was assessed using a kappa statistic for each step of the article selection process. Demographics and KSS from all studies were combined into weighted means and percentages. Survivorship estimates from the included studies were analysed and pooled using a meta-analysis random effects model, similar to the methods reported by Hopley, Crossett and Chen.10 Sensitivity analyses for component survivorship were performed according to study type (retrospective, randomised prospective). Sensitivity analyses of KSS and cumulative rates of revision were performed according to geographic location (United States, Europe, and Asia).
All meta-analysis calculations were performed using Comprehensive Meta-Analysis Version 2.0 (Biostat Inc., Englewood, New Jersey). Because most studies do not report the number of TKRs remaining at risk for each follow-up interval, it was assumed that all TKRs had at least two years’ follow-up. It was assumed that the number of TKRs at risk decreased by 5% each year thereafter. This method allows for a conservative estimate of patient attrition.10
Pooled survivorship estimates were compared with the combined survivorship reported for all TKRs with cement fixation in the NJR.2 Pooled survivorship estimates were also compared with each type of insert (unconstrained fixed bearing, unconstrained mobile bearing, PS fixed bearing, PS mobile bearing, constrained condylar and all-polyethylene tibia) with cement fixation. The NJR was selected because it is a large, well-established registry that reports survivorship estimates for each follow-up year. Cement fixation was selected because it is the most common fixation method and six of the eight included studies that featured only TKRs implanted with cement fixation. Differences in survivorship estimates were considered significant if there was no overlap of the 95% confidence intervals (CI) for the two groups being compared.10 An odds ratio was also calculated comparing the cumulative rate of revision from the included studies with that of all cemented TKRs included in the 2013 Annual Report of the Australian Orthopaedic Association National Joint Replacement Registry (AOA NJRR).11 The NJR could not be used for this comparison because the cumulative number of revisions could not be determined from the 2013 annual report.
Results
Study selection and characteristics
A total of 628 results were returned, of which there were eight unique studies that satisfied the inclusion/exclusion criteria.12-19 Kappa statistics for the level of agreement for the article title and article abstract reviews were 0.979 (95% CI, 0.951 to 1.000) and 0.938 (95% CI, 0.817 to 1.000), respectively. These values suggest excellent inter-observer agreement, as kappa statistics between 0.8 and 1.0 suggest ‘almost perfect’ agreement beyond chance.20 A kappa statistic was not calculated for the full-text review due to complete agreement between observers. Heterogeneity between studies at each interval was evaluated (I2 = 0.00), but the p-value was > 0.05, suggesting that caution is needed when interpreting this statistic. Included studies contained data for 1146 TKRs implanted at 12 centres in six countries (Table I). There were four prospective outcome studies,12,14,16,19 two retrospective outcome studies,17,18 and two prospective randomised studies.13,15
Table I.
Demographics from the studies included in the systematic review and meta-analysis
| Source | Study design | Country | Number of knees | Mean follow-up (yrs) (range) | Mean age (yrs) (range) | % Female | % OA | % Cement fixation | % Bilateral |
|---|---|---|---|---|---|---|---|---|---|
| Anderson et al19 | Prospective | USA | 298 | 5.4 (5.0 to 7.6) | 69.0 (39 to 87) | 59.7 | 95.3 | 94.0 | 7.9 |
| Bae et al18 | Retrospective | South Korea | 137 | 3.9 (2.0 to 7.1) | 66.6 (42 to 83) | 94.1 | 91.9 | 100.0 | 15.1 |
| Chinzei et al17 | Retrospective | Japan | 85 | 7.7 (6.0 to 12.0) | 70.2 (51 to 88) | 93.4 | 70.6 | 100.0 | 11.8 |
| Fan et al16 | Prospective | Taiwan | 58 | 5.4 (NR) | 65.1 (48 to 83) | 76.3 | 94.8 | 100.0 | 5.3 |
| Ishida et al15 | Prospective, randomised | Japan | 20 | 4.7 (4.0 to 5.1) | 71.0 (60 to 81) | 95.0 | 100.0 | NR | 0.0 |
| Karachalios et al14 | Retrospective | Greece | 284 | 6.7 (4.0 to 9.0) | 71.0 (52 to 84) | 82.0 | 75.0 | 100.0 | 26.2 |
| Kim et al13 | Prospective, randomised | South Korea | 92 | 2.6 (2.0 to 3.0) | 69.5 (55 to 81) | 92.3 | 100.0 | 100.0 | 100.0 |
| Vecchini et al12 | Prospective | Italy | 172 | 7.0 (4.0 to 10.0) | 71.0 (31 to 85) | 73.7 | 91.3 | 100.0 | 7.5 |
| Cumulative | - | - | 1146 | 5.7 | 69.4 | 78.0 | 87.8 | 98.4 | 20.6 |
NR, not reported
The weighted mean patient age was 69.4 years (65.1 to 71.0). The cumulative percentage of patients implanted for a primary diagnosis of osteoarthritis was 87.8%. The cumulative percentage of female patients was 78.0%, with only a single study reporting < 73.7% female patients.19 Cement fixation was used in 98.4% of patients and only a single study reported any components implanted with cementless fixation.19 The cumulative percentage of bilateral patients was 20.6%, which was affected by the inclusion of a study that enrolled only bilateral patients.13 Excluding this study, the cumulative percentage of bilateral patients was 13.7%.
Survivorship
Table II shows the survivorship estimates from four studies that reported Kaplan–Meier estimates of survivorship12,14,17,19 and three studies that specifically stated there were no revisions at final follow-up.13,15,16 Also shown are the pooled survivorship estimates from these studies. The pooled survivorship was greater than the combined survivorship reported for all cemented TKRs in the NJR at each interval between two and eight years’ follow-up. This difference was significant only at the six-year interval. When the two randomised, prospective studies were removed as part of sensitivity analysis, the subject system had significantly increased survivorship at four, five and six years.
Table II.
Survivorship summary and comparison with the NJR
| Source | Survivorship (%) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| One year (%) | Two years (%) | Three years (%) | Four years (%) | Five years (%) | Six years (%) | Seven years (%) | Eight years (%) | Nine years (%) | ||||||||||
| Anderson et al19 | 99.7 | 99.7 | 99.7 | 99.7 | 99.7 | 99.1 | 97.4 | 97.4 | - | |||||||||
| Chinzei et al17 | - | - | - | - | - | - | - | 98.3 | - | |||||||||
| Fan et al16 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | - | - | - | - | |||||||||
| Ishida et al15 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | - | - | - | - | |||||||||
| Karachalios et al14 | 100.0 | 100.0 | 100.0 | 99.6 | 99.1 | 99.1 | 97.5 | 97.5 | 97.5 | |||||||||
| Kim et al13 | 100.0 | 100.0 | - | - | - | - | - | - | - | |||||||||
| Vecchini et al12 | - | - | - | - | - | - | 98.6 | - | - | |||||||||
| Pooled survivorship: ADVANCE medial-pivot | 99.5 (98.4 to 99.8) | 99.5 (98.4 to 99.8) | 99.5 (98.1 to 99.9) | 99.4 (98.1 to 99.8) | 99.2 (97.7 to 99.7) | 99.1 (97.7 to 99.7) | 97.7 (96.0 to 98.6) | 97.6 (95.8 to 98.6) | 97.5 (65.6 to 100.0) | |||||||||
| NJR: all cemented TKRs | 99.62 (99.60 to 99.64) | 99.04 (99.01 to 99.07) | 98.55 (98.51 to 98.59) | 98.19 (98.15 to 98.24) | 97.89 (97.84 to 97.94) | 97.64* (97.58 to 97.69) | 97.37 (97.30 to 97.44) | 97.12 (97.03 to 97.20) | 96.88 (96.76 to 96.99) | |||||||||
| NJR: cemented, unconstrained, fixed | 99.67 (99.65 to 99.69) | 99.12 (99.08 to 99.16) | 98.67 (98.62 to 98.71) | 98.34 (98.29 to 98.39) | 98.08 (98.01 to 98.14) | 97.81 (97.74 to 97.88) | 97.56 (97.47 to 97.64) | 97.29 (97.19 to 97.40) | 97.10 (96.96 to 97.23) | |||||||||
| NJR: cemented, unconstrained, mobile | 99.49 (99.40 to 99.57) | 98.78 (98.63 to 98.91) | 98.16 (97.97 to 98.33) | 97.65* (97.43 to 97.85) | 97.35* (97.11 to 97.57) | 97.11* (96.84 to 97.35) | 96.86 (96.56 to 97.14) | 96.69 (96.34 to 97.01) | 96.22 (95.60 to 96.76) | |||||||||
| NJR: cemented, PS, fixed | 99.57 (99.53 to 99.61) | 98.97 (98.91 to 99.03) | 98.47 (98.39 to 98.55) | 98.11 (98.01 to 98.20) | 97.72 (97.60 to 97.82) | 97.48* (97.36 to 97.60) | 97.21 (97.06 to 97.35) | 96.94 (96.76 to 97.11) | 96.68 (96.42 to 96.92) | |||||||||
| NJR: cemented, PS, mobile | 99.32 (99.11 to 99.48) | 98.44 (98.13 to 98.71) | 97.78 (97.40 to 98.11) | 97.27* (96.83 to 97.65) | 96.92* (96.44 to 97.34) | 96.47* (95.91 to 96.96) | 96.16 (95.51 to 96.72) | 96.16 (95.51 to 96.72) | 94.99 (92.94 to 96.45) | |||||||||
| NJR: cemented, constrained condylar | 98.98 (98.42 to 99.34) | 98.15 (97.39 to 98.70) | 97.44 (96.49 to 98.13) | 96.96* (95.87 to 97.76) | 96.65* (95.46 to 97.53) | 96.65* (95.46 to 97.53) | 96.35 (94.96 to 97.36) | 95.52 (93.04 to 97.13) | 95.52 (93.04 to 97.13) | |||||||||
| NJR: cemented, all poly tibia | 99.61 (99.39 to 99.75) | 99.07 (98.73 to 99.32) | 98.52 (98.05 to 98.88) | 98.26 (97.73 to 98.67) | 97.71 (97.02 to 98.24) | 97.59 (96.85 to 98.16) | 97.36 (96.45 to 98.04) | 97.36 (96.45 to 98.04) | 97.36 (96.45 to 98.04) | |||||||||
*Statistically significant
Pooled survivorship for the subject system was also greater than that reported for all cemented insert types in the NJR at each interval outside of one year. These differences were significant during mid-term follow-up intervals (four, five and six years) when compared with unconstrained mobile bearing, PS mobile bearing, and constrained condylar bearing types. The difference was also significant at the six-year interval when compared with PS fixed bearings.
Knee Society Scores
Table III shows the mean KSS for the eight included studies. Seven studies reported mean post-operative KSS in the ‘excellent’ range (80 to 100)13-19 and the remaining study reported a mean score in the ‘good’ range (70 to 79).12 The weighted mean KSS was 87.9. Post-operative mean Knee Society function scores ranged from 65.0 to 85.4, with a weighted mean of 80.0.
Table III.
Mean Knee Society and function scores
| Source | Number of knees | Knee Society scores | Knee Society function scores | |||
|---|---|---|---|---|---|---|
| Pre-operative | Post-operative | Pre-operative | Post-operative | |||
| Anderson et al19 | 298 | 33.0 | 90.0 | NR | NR | |
| Bae et al18 | 137 | 59.6 | 91.5 | 53.6 | 85.4 | |
| Chinzei et al17 | 85 | 36.2 | 92.1 | 31.4 | 73.4 | |
| Fan et al16 | 58 | 30.5 | 91.1 | 36.7 | 82.3 | |
| Ishida et al15 | 20 | 34.0 | 89.0 | 40.0 | 65.0 | |
| Karachalios et al14 | 284 | 31.6 | 91.3 | 42.9 | 80.9 | |
| Kim et al13 | 92 | 29.0 | 87.0 | 45.0 | 80.0 | |
| Vecchini et al12 | 172 | 28.3 | 73.2 | 49.1 | 78.9 | |
| Cumulative | 1146 | 34.9 | 87.9 | 44.4 | 80.0 | |
Sensitivity analysis of KSS showed that weighted mean post-operative KSS were within the excellent range for all geographic regions: United States (90.0), Europe (84.4), and Asia (90.3). Weighted mean post-operative Knee Society function scores were also similar in the United States (80.4), Europe (80.1), and Asia (80.0).
Revisions
Table IV shows a summary of the number of revisions, reasons for revisions, and cumulative revision rates. There were 14 revisions for a cumulative revision rate of 1.22%. The most common reasons for revision were infection (0.34%), aseptic loosening (0.26%) and pain (0.17%). There were no reported revisions for instability. A sensitivity analysis revealed the cumulative revision rate in studies conducted in Asia was approximately half that reported in the United States (1.67%, 5 of 298 TKRs) and Europe (1.31%, 6 of 456 TKRs). The calculated odds ratio comparing the cumulative revision rate from the included studies with that for all cemented TKRs in the AOA NJRR was 0.44 (95% CI 0.26 to 0.73, p < 0.01).
Table IV.
Summary of revisions and cumulative revision rates
| Source | Number of knees | Number of revisions | Cumulative revision rate (%) | Reason for revision | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infection n (%) | Aseptic loosening n (%) | Pain n (%) | Septic loosening n (%) | Trauma n (%) | Unknown n (%) | ||||||||||
| Anderson et al19 | 298 | 5 | 1.67 | 0 (0.00) | 0 (0.00) | 2 (0.67) | 0 (0.00) | 0 (0.00) | 3 (1.00) | ||||||
| Bae et al18 | 137 | 2 | 1.45 | 1 (0.72) | 1 (0.72) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||||||
| Chinzei et al17 | 85 | 1 | 1.17 | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (1.17) | 0 (0.00) | 0 (0.00) | ||||||
| Fan et al16 | 58 | 0 | 0.00 | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||||||
| Ishida et al15 | 20 | 0 | 0.00 | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||||||
| Karachalios et al14 | 284 | 4 | 1.40 | 1 (0.35) | 2 (0.70) | 0 (0.00) | 0 (0.00) | 1 (0.35) | 0 (0.00) | ||||||
| Kim et al13 | 92 | 0 | 0.00 | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||||||
| Vecchini et al12 | 172 | 2 | 1.16 | 2 (1.16) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||||||
| Cumulative | 1146 | 14 | 1.22 | 4 (0.34) | 3 (0.26) | 2 (0.17) | 1 (0.08) | 1 (0.08) | 3 (0.26) | ||||||
Discussion
The current systematic review synthesises available clinical evidence (survivorship, functional outcomes, and reasons for revision) for the ADVANCE Medial-Pivot System from over 1100 TKRs performed in six countries.
Survivorship
The pooled survivorship was 99.2% (95% CI, 97.7 to 99.7) and 97.6% (95% CI, 95.8 to 98.6) at five and eight years’ follow-up, respectively. The survivorship estimate of 97.5% at nine years was based upon a single source with a wide 95% CI (65.6% to 100.0%), suggesting a small number of patients at nine years’ follow-up. Survivorship for the subject system was significantly greater than that reported for unconstrained mobile bearing, PS mobile bearing, and constrained condylar bearing types at mid-term follow-up intervals (four, five and six years). It was also significantly greater than PS fixed bearings at six years. This may indicate a potential benefit to the subject system in terms of survivorship at mid-term follow-up when compared with four of the six insert types, including both mobile bearing and PS subgroups. There were no significant differences at any interval with the remaining insert types. Future analyses of longer-term studies are needed to confirm and determine if these trends continue.
The pooled survivorship estimates agree with recent arthroplasty registry reports. The NJR reported 96.02% (95% CI 94.34 to 97.21) survivorship at nine years for over 5000 TKRs implanted with the subject system.2 Similarly, the Danish Knee Arthroplasty Register reported 95.7% (95% CI 93.9 to 97.5) survivorship at ten years’ follow-up for over 1400 TKRs implanted with cement fixation.21 Finally, the Regional Register of Orthopedic Prosthetic Implantology in the Emilia–Romagna region of Italy reported 95.5% (95% CI 93.4 to 7.5) survivorship at nine years’ follow-up for nearly 500 TKRs.22
The lone exception is the 2013 Annual Report of the AOA, which reported separate ten-year survivorship rates for two combinations of the subject system.11 The ADVANCE-ADVANCE I combination describes an older version of the system with a different tibial insert locking detail that is no longer sold. This combination had a reported survivorship of 88.1% (95% CI 78.8 to 93.5) but the width of the 95% CI suggests this may not be a reliable estimate. The ADVANCE-ADVANCE II combination had a reported survivorship of 92.5% (95% CI 90.6 to 94.1). Outside of the registry, favourable results have been reported for the subject system in Australia. One study reported just a single revision for the insertion of a patellar component in a cohort of 50 consecutive patients at a mean follow-up of 9.96 years.23 The authors reported “good pain relief and functional improvement according to KSS, WOMAC Scores, and on subjective patient questionnaires”.
Knee Society scores
In all studies that reported pre-operative values, mean KSS and function scores were improved at final follow-up. A total of seven of the eight studies reported mean post-operative KSS in the ‘excellent’ range, with the remaining study reporting a mean in the ‘good’ range. One study enrolled single-stage bilateral subjects with the subject system in one knee and a DePuy PFC mobile-bearing prosthesis (Warsaw, Indiana) in the other.13 While the authors reported KSS in the excellent range for the subject system, the values were statistically lower than those for the system in the contralateral knee (mean of 87 vs 94, p = 0.021). There were no radiological differences between the systems or any revisions in either group.
The cumulative post-operative KSS and function scores were 87.9 and 80.0, respectively. These values compared favourably with the pooled scores of 88.0 and 78.0 at five to six years’ follow-up reported in a recent meta-analysis.10 That study included 17 mean KSS for various TKR systems at between five and six years of follow-up pooled from 12 peer-reviewed articles that were included in TKR technological assessments performed by the Agency for Healthcare Research and Quality in the United States24 and the Ministry of Health and Long-Term Care in Canada.25 KSS were similar in the United States, Europe, and Asia. This is of interest because different cultures have different demands for TKR outcomes. For example, Asian populations often require higher flexion for culturally important activities.26
The subject system did not have a noticeably different KSS from those reported for other systems. This is not unexpected, with the documented ceiling effect of this scoring system likely limiting its ability to detect differences between individual systems.27 The KSS also does not assess the ability of patients to perform more demanding tasks, such as kneeling and squatting. A recent study has shown patients describing these activities as ‘very important’ and that their post-operative expectations to perform them are often unfulfilled.28 This may explain why there is no difference in KSS, yet a recent study showed the subject system is preferred by patients over PS, mobile-bearing, and PCL-retaining designs.7
Revisions
The cumulative revision rate for all studies was 1.22%. Odds ratio calculations showed the subject system was associated with significantly less risk of revision when compared with that reported for all cemented TKRs in the AOA NJRR. The cumulative revision rates for the United States (1.67%, five of 298 TKRs), and Europe (1.31%, six of 456 TKRs) were similar, while the rate for Asia (0.76%, three of 392 TKRs) was approximately half that seen in the other two regions. It is possible the difference in rates for these regions is simply that the Asian studies have shorter follow-up times than those conducted in Europe and the United States. There were five revision modes specified in the included studies: infection (four revisions, 0.34%); aseptic loosening (three revisions, 0.26%); pain (one revision, 0.08%); trauma (one revision, 0.08%); and septic loosening (one revision, 0.08%).
Theoretically, the medial-pivot design provides a large contact area in the medial compartment and lower contact stresses, which should result in lower insert wear. Some reports, however, have speculated that the constrained medial compartment could result in excessive insert wear or stresses, leading to failure.4,16 Particular attention was paid to any revisions that could be indicative of these failures (e.g. aseptic loosening, instability, insert exchanges, or insert fractures/breakage). In total, there were three revisions for aseptic loosening. Two of these were reported by the authors as being caused by “patient selection and surgical errors”.14 The other revision occurred at 1.8 years’ follow-up and was described as loosening of the tibial component that led to varus alignment.18 There were no revisions reported due to instability, insert exchanges, or insert fracture/breakage. The cumulative revision rate of 0.26% (three revisions/1146 TKRs) for these causes does not suggest a higher rate of failure due to the constraint placed on the medial compartment of the insert.
Limitations
The use of registry data as a comparator is the main limitation due to possible differences in patient populations (i.e. indications for surgery, gender, age, activity levels) and the inclusion of data for surgeons of all skill and specific product experience levels. This limitation is minimised because the TKR population in the NJR was similar to the patient demographics from the included studies. Both consisted of mostly female patients, had patients with a mean age of 69 years and the majority of patients had a primary indication of osteoarthritis (98.0% in the NJR vs 87.8%).
All meta-analyses are limited by the potential for publication bias. Funnel plots were created and all data points at each follow-up interval fell within the 95% CI, possibly indicating a lack of publication bias. With a mean of 3.5 data points for each follow-up interval, it is not possible to reliably evaluate symmetry or speculate if this would remain true if more studies were available for inclusion. Another limitation which afflicts meta-analyses in general is the lack of a quality assessment for included articles.
Only data from English language peer-reviewed journals were included in this systematic review. This limitation can lead to potential omission of relevant data presented at conferences that never reach publication or data included in non-English language journals. A final limitation is the assumption that overlapping CIs do not contain statistical differences. There are cases where this may not hold true, but in those situations, the differences would likely not be very large due to the overlapping confidence intervals.29
In conclusion, the subject system is associated with survivorship and KSS that are similar to or better than those reported for other TKR systems. An evaluation of reasons for revision did not indicate an increase in revisions due to the unique tibial insert articulation. Similar low cumulative revision rates and KSS in the excellent range were achieved in patients from the United States, Europe, and Asia.
Funding Statement
None declared
Footnotes
Author contributions:D. A. Fitch: Study design, Literature searches, Study inclusion/exclusion assessment, Manuscript preparation
K. Sedacki: Study design, Study inclusion/exclusion assessment, Data analysis, Manuscript preparation
Y. Yang: Study design, Data analysis, Manuscript preparation
ICMJE Conflict of Interest:D. A. Fitch, K Sedacki and Y. Yang are paid employees of MicroPort Orthopedics Inc.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg [Am] 2007;89-A:780–785 [DOI] [PubMed] [Google Scholar]
- 2.No authors listed. National Joint Registry of England, Wales, and Northern Ireland. Annual Report., ed, 2013. http://www.njrcentre.org.uk/njrcentre/Home/tabid/36/Default.aspx (date last accessed 25 July 2014).
- 3.Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ. Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res 2003;410:139–147 [DOI] [PubMed] [Google Scholar]
- 4.Miyazaki Y, Nakamura T, Kogame K, et al. Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty 2011;26:1038–1044 [DOI] [PubMed] [Google Scholar]
- 5.Komistek RD, Dennis DA, Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res, 2003;410:69–81 [DOI] [PubMed] [Google Scholar]
- 6.Reynolds S, Lamontagne M, Dervin G. Sit-to-stand symmetry following total knee arthroplasty with a medial pivot knee. https://www.isakos.com/meetings/2013congress/onsite/AbstractView.aspx?EventID=6605 (date last accessed 17 September 2014).
- 7.Pritchett JW. Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J Arthroplasty 2011;26:224–228 [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–269 [DOI] [PubMed] [Google Scholar]
- 9.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 1989;248:13–14 [PubMed] [Google Scholar]
- 10.Hopley CD, Crossett LS, Chen AF. Long-term clinical outcomes and survivorship after total knee arthroplasty using a rotating platform knee prosthesis: a meta-analysis. J Arthroplasty 2013;28:68–77 [DOI] [PubMed] [Google Scholar]
- 11.No authors listed. Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2013. https://aoanjrr.dmac.adelaide.edu.au/ (date last accessed 20 August 2014).
- 12.Vecchini E, Christodoulidis A, Magnan B, et al. Clinical and radiologic outcomes of total knee arthroplasty using the Advance Medial Pivot prosthesis. A mean 7 years follow-up. Knee 2012;19:851–855 [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Yoon SH, Kim JS. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res 2009;467:493–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karachalios T, Roidis N, Giotikas D, et al. A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. Knee 2009;16:484–488 [DOI] [PubMed] [Google Scholar]
- 15.Ishida K, Matsumoto T, Tsumura N, et al. No difference between double-high insert and medial-pivot insert in TKA. Knee Surg Sports Traumatol Arthrosc 2014;22:21–25 [DOI] [PubMed] [Google Scholar]
- 16.Fan CY, Hsieh JT, Hsieh MS, Shih YC, Lee CH. Primitive results after medial-pivot knee arthroplasties: a minimum 5-year follow-up study. J Arthroplasty 2010;25:492–496 [DOI] [PubMed] [Google Scholar]
- 17.Chinzei N, Ishida K, Tsumura N, et al. Satisfactory results at 8 years average follow-up after ADVANCE Medial-Pivot Total Knee Arthroplasty. Knee 2014;21:387–390 [DOI] [PubMed] [Google Scholar]
- 18.Bae DK, Song SJ, Cho SD. Clinical outcome of total knee arthroplasty with medial pivot prosthesis a comparative study between the cruciate retaining and sacrificing. J Arthroplasty 2011;26:693–698 [DOI] [PubMed] [Google Scholar]
- 19.Anderson MJ, Kruse RL, Leslie C, et al. Medium-term results of total knee arthroplasty using a medially pivoting implant: a multicenter study. J Surg Orthop Adv 2010;19:191–195 [PubMed] [Google Scholar]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174 [PubMed] [Google Scholar]
- 21.No authors listed. Danish Knee Arthroplasty Register Annual Report 2013 https://www.knee.dk/groups/grp_login.php (date last accessed 20 August 2014).
- 22.No authors listed. Register of the Orthopaedic Prosthetic Implants: annual report 2011. https://ripo.cineca.it/ (date last accessed 20 August 2014).
- 23.Brinkman JM, Bubra PS, Walker P, Walsh W, Bruce W. Mid-term results using a medial pivot total knee replacement: single centre, single surgeon outcome compared to the Australian National Joint Registry Data. Bone Joint J 2013;(Supp15):24 [Google Scholar]
- 24.Kane RL, Saleh KJ, Wilt TJ, et al. Total knee replacement. Evid Rep Technol Assess (Summ) 2003;86:1–8 [PMC free article] [PubMed] [Google Scholar]
- 25.No authors listed. Health Quality Ontario: total knee replacement: an evidence-based analysis Ont Health Technol Assess Ser 2005;5:1–51 [PMC free article] [PubMed] [Google Scholar]
- 26.Kanekasu K, Banks SA, Honjo S, Nakata O, Kato H. Fluoroscopic analysis of knee arthroplasty kinematics during deep flexion kneeling. J Arthroplasty 2004;19:998–1003 [DOI] [PubMed] [Google Scholar]
- 27.Na SE, Ha CW, Lee CH. A new high-flexion knee scoring system to eliminate the ceiling effect. Clin Orthop Relat Res 2012;470:584–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scott CE, Bugler KE, Clement ND, et al. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg [Br] 2012;94-B:974–981 [DOI] [PubMed] [Google Scholar]
- 29.Dorey FJ. In brief: statistics in brief: Confidence intervals: what is the real result in the target population? Clin Orthop Relat Res 2010;468:3137–3138 [DOI] [PMC free article] [PubMed] [Google Scholar]


