Abstract
Antibiotic resistance has become a major public health problem and the antibiotics pipeline is running dry. Bacteriophages (phages) may offer an ‘innovative’ means of infection treatment, which can be combined or alternated with antibiotic therapy and may enhance our abilities to treat bacterial infections successfully. Today, in the Queen Astrid Military Hospital, phage therapy is increasingly considered as part of a salvage therapy for patients in therapeutic dead end, particularly those with multidrug resistant infections. We describe the application of a well-defined and quality controlled phage cocktail, active against Pseudomonas aeruginosa and Staphylococcus aureus, on colonized burn wounds within a modest clinical trial (nine patients, 10 applications), which was approved by a leading Belgian Medical Ethical Committee. No adverse events, clinical abnormalities or changes in laboratory test results that could be related to the application of phages were observed. Unfortunately, this very prudent ‘clinical trial’ did not allow for an adequate evaluation of the efficacy of the phage cocktail. Nevertheless, this first ‘baby step’ revealed several pitfalls and lessons for future experimental phage therapy and helped overcome the psychological hurdles that existed to the use of viruses in the treatment of patients in our burn unit.
Keywords: Phage therapy, burn wound, infection, Pseudomonas aeruginosa, Staphylococcus aureus, antibiotic resistance
Introduction
Multidrug resistance, first reported in the 1970s, has become a major threat to the progress made in infection control worldwide. Each year in the EU, an estimated 25,000 patients die from infections with multidrug-resistant (MDR) bacteria [1]. Also in burn units, a large number of infections are virtually untreatable. Whereas Staphylococcus aureus remains a common early colonizer of burn wounds, Pseudomonas aeruginosa is known as the most common cause of life-threatening infection in burn patients [2,3]. Both bacteria, but especially P. aeruginosa, are known for their intrinsic and acquired resistance to many antibiotics. Persistent multidrug-resistant P. aeruginosa strains have frequently been reported to cause nosocomial outbreaks of infection in burn units [4,5].
Bacteriophages (phages) are (among) the most abundant and ubiquitous organisms on Earth and are the natural controllers of bacteria. They are the ‘viruses’ of the bacteria and are able to lyse, among others, strains of S. aureus or P. aeruginosa, irrespective of the antibiotic susceptibility of these strains. As such, they may offer an independent means of infection treatment, which can be combined or alternated with antibiotic therapy and may enhance our abilities to treat bacterial infections successfully [6]. Since the 1920s, phages have been used to treat all sorts of bacterial infections in Eastern Europe and the former USSR States, with the Eliava Institute in Tbilisi (Georgia) as one of the key centers [7]. The advent of antibiotics, which exhibited a broader spectrum of activity and which could be produced easier in large quantities (i.e. in a commercially more profitable manner), forced phage therapy to the margins of Western medicine. With the worldwide spreading of MDR bacteria, however, the therapeutic use of phages is going through a renaissance in the Western world [8].
The few burn wound related phage therapy papers in the scientific literature [9-17] suggest that phages could have the potential to control bacterial burn wound infection.
Phages were shown to be able to rescue burned mice from infection caused by P. aeruginosa and Klebsiella pneumonia [9,10]. In 1990, in Egypt, 30 patients with burn wounds were treated during 5-17 days with between 15 and 45 phage-saturated dressings [11]. The clinical success ratio was difficult to assess because of the lack of validated controls, but the mere fact that not-endotoxin-purified phages had been applied massively to burn wounds, without reporting adverse effects, could be indicative for their intrinsic harmlessness. Soothill and colleagues showed that in a test population of 14 guinea pigs with excised burn wounds to which 6 x 105 cfu/ml of P. aeruginosa and 1.2 x 107 P. aeruginosa BS24 phages were applied simultaneously and upon which the excised tissue was replaced, 6 out of 7 phage treated grafts were not rejected, whereas all 7 of non phage treated grafts failed [12]. Weber-Dabrowska et al. reported the treatment of 49 burn wounds in human patients, infected with P. aeruginosa, S. aureus, Escherichia coli, Klebsiella and/or Proteus. Forty-two patients fully recovered and the condition of the remaining 7 patients improved markedly [13]. A 2005 publication addressed the treatment of local radiation injuries in two individuals, using a novel biodegradable preparation capable of sustained release of phages and ciprofloxacin [14]. The same product was applied in Georgia on 22 patients with infected venous static ulcers and other poorly healing wounds, after standard therapy had failed [15]. Seventy percent of the patients showed full recovery after a period ranging from 6 days to 15 months. In the UK, the group of Soothill reported the case of a 27-year-old male with 50% TBSA burned and excised burn wounds covered with skin grafts, which became infected with P. aeruginosa after several months [16]. Grafted areas broke down rapidly despite appropriate antibiotic treatment. Therefore, treatment with ‘purified’ phages was started. Phages multiplied in the wound and a 43 to 1200-fold increase of phages was observed. Three days after phage application, P. aeruginosa could not be isolated from swabs and subsequent extensive grafting was successful.
There are, however, some major obstacles hampering the clinical application of phages in Western medicine [18-22]. In the EU, discussions between small and medium-sized enterprises (SMEs) and competent authorities led to the classification of bacteriophages as human medicinal products (biologicals) regulated under the European Human Code for Medicines (Directive 2001/83/EC). A handful of companies are now struggling to take large-scale and uniform phage cocktails through the elaborate and expensive medicinal product licensing pathway. Funding for the development of phages as medicinal products is difficult to obtain, since intellectual property (IP) protection for phages (products of nature) is very fragile. In addition, we feel that in hospital settings phage therapy would better be served by small-scale productions and distributions of tailor made phage preparations [21,22]. Finally, but not less important, the reluctance to embrace phage therapy is also linked to the false perception of viruses, with which phages are identified – often without nuance –, as ‘enemies of life’ [23]. As a result, in the Western world, phages for controlling microbial contamination in food and the food-processing environment are readily used, while no phage medicinal products are currently authorized for human use [24].
In 2007, we developed a well-defined phage cocktail, BFC-1, which was active against the P. aeruginosa and S. aureus strains that populated the burn wound center of the Queen Astrid Military Hospital. The quality controlled production process of BFC-1 was mainly based on our experience in producing cell and tissue autografts and allografts for human transplantation (regulated under Directive 2004/23/EC of the European Parliament and of the Council) and was published in 2009 [25].
This paper gives an account of the first application, in 2007, of BFC-1 on colonized burn wounds in the burn wound center of the Queen Astrid Military Hospital. Since in 2007 phages were not yet classified as medicinal products, these phage applications were performed within a small (9 patients, 10 single dose applications) investigator driven clinical trial (no sponsor) under the responsibility and supervision of a leading Medical Ethical Committee. The study was not designed according to one of the common phases (I, II or III) of the classical medicinal product approval process and we did not solicit for approval by any regulatory authority for future use in the general population (marketing authorization). The study was notified (by the ethical committee) to the national competent authorities and informed consent was obtained from the patients. The parties involved in this study had no commercial interests.
Materials and methods
Phage cocktail
The phage cocktail BFC-1, which was evaluated in this study, consisted of three exclusively lytic phages, designed for the treatment of P. aeruginosa and S. aureus infections in burn wound patients [25]. Based on successive selection rounds three phages were retained from an initial pool of 82 P. aeruginosa and 8 S. aureus phages, specific for the P. aeruginosa and S. aureus strains that were the most prevalent in the burn wound center of the Queen Astrid Military Hospital. This cocktail, consisting of P. aeruginosa phages 14/1 (Myoviridae) and PNM (Podoviridae) and S. aureus phage ISP (Myoviridae), at a concentration of 109 plaque forming units (pfu)/ml of each phage, was produced and purified of endotoxin according to Merabishvili et al. [25]. Quality controls included stability (shelf life), determination of pyrogenicity, sterility and cytotoxicity, confirmation of the absence of temperate phages and transmission electron microscopy-based confirmation of the presence of the expected virion morphologic particles as well as of their specific interaction with the target bacteria. Phage genome and proteome analysis confirmed the lytic nature of the phages and the absence of toxin-coding genes.
Patients’ inclusion criteria
Nine acute burn wound patients with MDR P. aeruginosa and/or S. aureus burn wound colonization, as determined by classical bacterial culture and species identification and antibiotic susceptibility testing using the VITEK 2 system (bioMérieux) of routine burn wound swabs, were included in this study. Pregnant women and patients in critical condition (APACHE II score > 20) were not included. Only patients with burn wounds that allowed for punch biopsy sampling were included. Patients or their legal representatives were provided with relevant and understandable information regarding the study and the need to give informed consent before they participated in the study. A no-fault (regardless of liability) compensation insurance was provided to the patients.
General trial set up
We compared the standard treatment for P. aeruginosa and S. aureus burn wound colonization with a phage treatment. Since an objective evaluation and classification of burn wounds is impossible and colonization and infection levels can vary significantly, we compared both treatments on the same colonized burn wound.
Just before the application of BFC-1, the colonized burn wound was divided into two halves. One half received the standard treatment, the other half the phage treatment with BFC-1. Two biopsies were taken by the MD in charge of the patient using a 4 mm punch biopsy needle (Labo Stiefel); one in the centre of the zone where BFC-1 was to be applied, the other in the centre of the zone where the standard treatment was to be applied. Tissue biopsies were preceded by local anesthesia (xylocaine 2%, Asta Zeneca). It was shown that infiltration with additive-free lidocaine 1% into a ring block shortly before the biopsy procedure did not affect the result of bacterial culture provided that culture was started within 2 hours [26]. Biopsy sites were sutured with green ethilon 4/0 (standard treatment site) or with blue prolene 4/0 (BFC-1 site). The MD in charge of the patient applied a single-dose of approximately 1 ml of sterile and endotoxin-purified BFC-1 per 50 cm2 on one half of the burn wound, using a 5 ml syringe with a spray adapter (Coster®) (Figure 1). The other half of the burn wound was treated with antimicrobial substances according to the standard treatment protocols. Patients with suspected P. aeruginosa burn wound infection were administered amikacin (single initial dose of 25 mg/kg body weight) in combination with ceftazidime (single initial dose of 1 g) or meropenem (2 g/8 h) systemically. Patients with suspected S. aureus burn wound infection were treated with systemic vancomycin (single initial dose of 1 g) or linezolid (2 x 600 mg/d).
Figure 1.
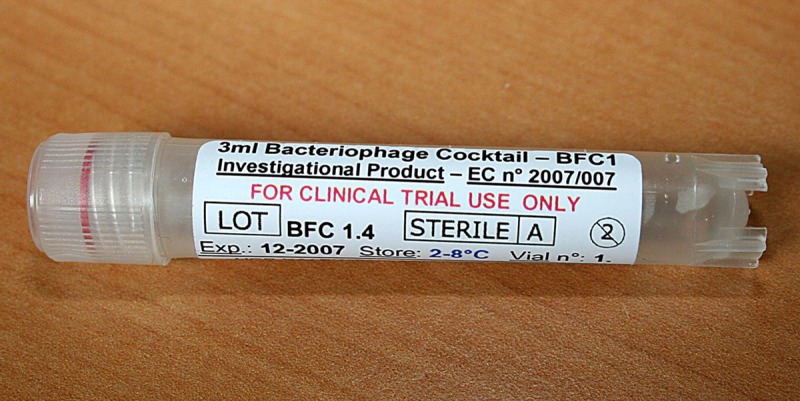
A vial of bacteriophage cocktail BFC-1.
A digital photograph was taken of the burn wound. The entire burn wound was then covered with dressings, gauze and bandages according to the standard treatment protocols. Two to five hours later, the burn wound was uncovered. Immediately, two biopsies were taken next to (within 2 cm) the previous ones. A digital photograph was taken of the burn wound. The entire burn wound was further treated according to standard protocols. The wound biopsies were immediately weighed and collected into separate, sterile and adequately labeled microtubes (Eppendorf AG) containing 0.5 ml of sterile phosphate buffered saline (PBS) and transported to the laboratory for bacterial load determination.
The main objective of this study was to explore the hurdles that early Western phage therapy clinical trials would inevitably face. The secondary objective was to document eventual adverse events and therapeutic effects.
Determination of bacterial load
The biopsies were immediately homogenized, on ice, for 1 min at 30000 rpm, using a tissue tearer (Biospec Products, Inc.). Serial tenfold dilutions of the homogenized wound biopsy samples were spread, in triplicate, on blood agar, Manitol Salt Agar (MSA) and cetrimide agar plates (media were purchased from Becton Dickinson). Colony counts were performed after overnight incubation at 37°C. The bacterial load, expressed as colony forming units (cfu) per g tissue, was calculated for each biopsy.
Monitoring of eventual adverse events
Patient medical files were screened for adverse events, clinical abnormalities and changes in laboratory test results that could be related to the application of phages. Clinical abnormalities that were screened for included cardiovascular, renal, and respiratory complications and pain. Clinical laboratory tests included the blood formula and standard haemostasis, biochemical, pharmacological and toxicological parameters.
Informed consent and approval of a leading Medical Ethical Committee
This clinical trial was conducted with the understanding and the consent of the human subjects. The study protocol was cleared by the Medical Ethical Committee of the Vrije Universiteit Brussel (VUB), which also notified the competent authorities.
Results
Ten BFC-1 applications were performed on 9 patients (4 males, 5 females; mean age 61 years; age range, 27 to 88 years; mean TBSA burned, 30%; TBSA burned range, 6-45%). The surface of the burn wounds to which BFC-1 was administered averaged 95 cm2 (range 25-150 cm2) and on average 0.03 ml of BFC-1 (equating 107 phages) per cm2 were applied in a single dose. The second biopsies were obtained 181 min (range 120-240 min) after BFC-1 application. Standard treatment consisted of Isobetadine® gel (Meda Pharma) (n = 4) and Mepilex® Ag (Mölnlycke) (n = 1). Five applications occurred within the time frame of a surgical procedure, prior to which the burn wounds had been washed with Hibitane (5%) and filtered tab water.
The 10 burn wounds to which BFC-1 was administered were colonized or infected with MDR (resistance to a representative of at least 3 classes of antibiotics) strains of P. aeruginosa (n = 7), S. aureus (n = 1) or both P. aeruginosa and S. aureus (n = 2). This distinction was based on the results of the most recent routine bacteriological screening of the burn wounds, associated to relevant clinical signs and biological markers. Despite the initial indications of colonization or infection, bacterial cultures of the homogenised biopsies taken before and after BFC-1 application showed only a very small bacterial load (a few colonies) in 8 of the 10 applications. In the two remaining applications bacterial loads before BFC-1 application were 103 and 108 cfu per g tissue. In all cases, the bacterial load remained unchanged, after BFC-1 application as well as after standard treatment.
No adverse events were reported and no clinical or laboratory test abnormalities related to the application of phages were observed.
Discussion
Hurdles
It was far from easy to get this small pilot study on the rail. We had to disarm a lot of resistance. This reluctance towards phage therapy was expected and was largely due to pre- and misconceptions about phage therapy. For example, we were asked to submit our phage cocktail to the National approval system for Genetically Modified Organisms (GMO), in which the safety for humans, animals and the environment is thoroughly assessed. Then, the experts of the insurance company that was asked to provide the no-fault compensation insurance assimilated phages with viruses and consequently assigned our modest experiment to risk class 5 (on a scale from 1 to 7), which resulted in a relatively high premium. Some editors and reviewers, who evaluated a former paper describing the quality controlled production of our phage cocktail, asked for conventional pharmaceutical tests and clinical trials, which take many years and cost millions of euros. They reckoned phages should be considered as classical drugs. Although phages are therapeutic agents, we disagree on the fact they have to be considered as classical drugs. Phages are evolving natural controllers of bacteria. If one were to consider them as a stable ‘drug’, and apply the whole regulatory framework thereof, their composition and characteristics are not meant to vary. Unfortunately, bacteria are expected to escape such ‘stable’ phage preparations and the real power of the use of phages would be lost. The real added value of phages as antimicrobials relies on the possibility to generate certified phage preparations on faster time scales than those common for classical medicinal products. Then and only then will we have a ‘new’ powerful and sustainable tool in the fight against bacterial diseases. Hence, if they are to be successful, phages cannot be considered as classical molecules and will thus need a dedicated regulatory framework with adequate and realistic production and quality control requirements [20].
Pitfalls
During this study, we were confronted with some significant technical and logistic problems. We opted for biopsy samples to monitor the bacterial load of the burn wounds because they are still considered to be the gold standard by the majority of researchers [2,27,28]. On reflection, we found this technique to be very elaborate (e.g. necessitated local anesthesia and complex sample processing) and at some occasions we were confronted with patient and/or nursing aversion to biopsies. All in all, biopsy sampling turned out to impede the clinical trial in our burn wound center. In the future, we will likely opt for semi-quantitative swab cultures instead of quantitative biopsy cultures for the monitoring of burn wound colonization, even if this is bound to result in less accurate quantification of burn wound colonization or infection.
The disappointing bacterial load of wound tissue at the moment of BFC-1 application was probably due to the long period (up to 7 days) between initial detection of a potential candidate with MDR P. aeruginosa and/or S. aureus burn wound colonization and the actual enrollment of this patient in the study. Major reasons for this were the delays in receiving antibiograms and obtaining informed consent. Meanwhile patients were treated with potent topical antimicrobials, dressings and systemic antibiotics. Some treatments were even applied minutes before the start of the trial. In the future, we will probably use clinical signs and biological markers of burn wound colonization or infection, instead of deferred bacteriological results, as inclusion criterion for this type of clinical trial. This would of course imply the inclusion of all P. aeruginosa and S. aureus burn wound infections, not only those with MDR strains. Finally, the sprayed BFC-1 cocktail had the tendency to run off the burn wound. The use of a suitable carrier, such as a gel or a dressing that is compatible with phage activity, seems more appropriate.
Notwithstanding these pitfalls, we were not expecting that a one-off application of 3 ml of BFC-1 on a small wound surface would generate conclusive proof of the efficacy of BFC-1.
Why publish (now)?
This study ran from the end of 2007 until 2008 and we planned to publish a report in a peer-reviewed scientific journal in the course of 2008. However, we decided to abandon the idea of a widespread scientific report of this study because it did not go as expected. We would use the experience gained during this small pilot study to set up a larger double blind study. Unfortunately, we had to put our plans on hold because meanwhile phages were classified as medicinal products and the subsequent and unattainable obligation to comply with the classical pharmaco-economical framework. We had waived publication, but colleagues from like-minded research groups were interested in the fate of our study and encouraged us to publish our experiences, as they might be helpful in convincing their competent authorities and ethical committees in approving experimental phage applications and in designing future studies. In addition, the study is increasingly mentioned (obviously without citing a peer-reviewed publication) in other scientific papers and this often without including relevant facts and details. Finally, we realized that this study had been an essential and necessary step towards the acceptance of phage therapy in our burn wound center. Since then the medical and nursing staff of our hospital has grown familiar with phages and deemed them safe for topical use on burn wounds. Today, phage therapy is increasingly part of the successful treatment of a handful of ‘abandoned’ patients with MDR infections, outside of a clinical trial and conform to the requirements of article 37 the Declaration of Helsinki (Unproven Interventions in Clinical Practice). Recently, the Belgian Ministry of Defense approved a feasibility study for the establishment of a dedicated phage therapy center in the Queen Astrid Military Hospital. On the first of June 2013, Phagoburn (www.phagoburn.eu), a project funded by the European Commission under the 7th Framework Programme for Research and Development was launched. It aims at evaluating phage therapy for the treatment of burn wounds infected with Escherichia coli and P. aeruginosa.
Conclusions
This small pilot study did identify some significant pitfalls and hurdles associated with phage therapy related clinical trials and broke down the psychological barriers with the healthcare team. The local topical application of bacteriophage cocktail BFC-1 on 10 burn wounds in 9 patients did not elicit any adverse events whatsoever.
Acknowledgements
We gratefully acknowledge Gunther Verween for his technical assistance. The authors would like to acknowledge the research community “Phagebiotics” (WO.022.09) grant from the FWO Vlaanderen.
Disclosure of conflict of interest
None to declare.
References
- 1.ECDC/EMEA Joint Working Group. The bacterial challenge: time to react. EMEA doc. ref. EMEA/576176/2009. Stockholm, September 2009. doi 10.2900/2518. Available from: http://www.ecdc.europa.eu/en/publications/Publications/0909_TER_The_Bacterial_Challenge_Time_to_React.pdf.
- 2.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin Microbiol Rev. 2006;19:403–34. doi: 10.1128/CMR.19.2.403-434.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altoparlak U, Erol S, Akcay MN, Celebi F, Kadanali A. The time-related changes of antimicrobial resistance patterns and predominant bacterial profiles of burn wounds and body flora of burned patients. Burns. 2004;30:660–4. doi: 10.1016/j.burns.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Hsueh PR, Teng LJ, Yang PC, Chen YC, Ho SW, Luh KT. Persistence of a multidrug-resistant Pseudomonas aeruginosa clone in an intensive care burn unit. J Clin Microbiol. 1998;36:1347–5. doi: 10.1128/jcm.36.5.1347-1351.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pirnay JP, De Vos D, Cochez C, Bilocq F, Pirson J, Struelens M, Duinslaeger L, Cornelis P, Zizi M, Vanderkelen A. Molecular epidemiology of Pseudomonas aeruginosa colonization in a burn unit: persistence of a multidrug-resistant clone and a silver sulfadiazine-resistant clone. J Clin Microbiol. 2003;41:1192–202. doi: 10.1128/JCM.41.3.1192-1202.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kutter E, De Vos D, Gvasalia G, Alavidze Z, Gogokhia L, Kuhl S, Abedon ST. Phage therapy in clinical practice: treatment of human infections. Curr Pharm Biotechnol. 2010;11:69–86. doi: 10.2174/138920110790725401. [DOI] [PubMed] [Google Scholar]
- 7.Sulakvelidze A, Alavidze Z, Morris JG Jr. Bacteriophage therapy. Antimicrob Agents Chemother. 2001;45:649–59. doi: 10.1128/AAC.45.3.649-659.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thiel K. Old dogma, new tricks – 21st Century phage therapy. Nat Biotechnol. 2004;22:31–6. doi: 10.1038/nbt0104-31. [DOI] [PubMed] [Google Scholar]
- 9.McVay CS, Velásquez M, Fralick JA. Phage therapy of Pseudomonas aeruginosa infection in a mouse burn wound model. Antimicrob Agents Chemother. 2007;51:1934–8. doi: 10.1128/AAC.01028-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumari S, Harjai K, Chhibber S. Bacteriophage versus antimicrobial agents for the treatment of murine burn wound infection caused by Klebsiella pneumoniae B5055. J Med Microbiol. 2011;60:205–10. doi: 10.1099/jmm.0.018580-0. [DOI] [PubMed] [Google Scholar]
- 11.Abul-Hassan HS, El-Tahan k Massoud B, Gomaa R. Bacteriophage therapy of Pseudomonas burn wound sepsis. Annals of the MBC. 1990;3:262–6. Available from: http://www.medbc.com/annals/review/vol_3/num_4/text/vol3n4p262.htm. [Google Scholar]
- 12.Soothill JS. Bacteriophage prevents destruction of skin grafts by Pseudomonas aeruginosa . Burns. 1994;20:209–11. doi: 10.1016/0305-4179(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 13.Weber-Dabrowska B, Mulczyk M, Górski A. Bacteriophage therapy of bacterial infections: an update of our institute’s experience. Arch Immunol Ther Exp (Warsz) 2000;48:547–51. [PubMed] [Google Scholar]
- 14.Jikia D, Chkhaidze N, Imedashvili E, Mgaloblishvili I, Tsitlanadze G, Katsarava R, Glenn Morris J Jr, Sulakvelidze A. The use of a novel biodegradable preparation capable of the sustained release of bacteriophages and ciprofloxacin, in the complex treatment of multidrug-resistant Staphylococcus aureus-infected local radiation injuries caused by exposure to Sr90. Clin Exp Dermatol. 2005;30:23–6. doi: 10.1111/j.1365-2230.2004.01600.x. [DOI] [PubMed] [Google Scholar]
- 15.Markoishvili K, Tsitlanadze G, Katsarava R, Morris JG Jr, Sulakvelidze A. A novel sustained-release matrix based on biodegradable poly(ester amide)s and impregnated with bacteriophages and an antibiotic shows promise in management of infected venous stasis ulcers and other poorly healing wounds. Int J Dermatol. 2002;41:453–8. doi: 10.1046/j.1365-4362.2002.01451.x. [DOI] [PubMed] [Google Scholar]
- 16.Marza JA, Soothill JS, Boydell P, Collyns TA. Multiplication of therapeutically administered bacteriophages in Pseudomonas aeruginosa infected patients. Burns. 2006;32:644–6. doi: 10.1016/j.burns.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 17.Soothill J. Use of bacteriophages in the treatment of Pseudomonas aeruginosa infections. Expert Rev Anti Infect Ther. 2013;11:909–15. doi: 10.1586/14787210.2013.826990. [DOI] [PubMed] [Google Scholar]
- 18.Verbeken G, De Vos D, Vaneechoutte M, Merabishvili M, Zizi M, Pirnay JP. European regulatory conundrum of phage therapy. Future Microbiol. 2007;2:485–91. doi: 10.2217/17460913.2.5.485. [DOI] [PubMed] [Google Scholar]
- 19.Huys I, Pirnay JP, Lavigne R, Jennes S, De Vos D, Casteels M, Verbeken G. Paving a regulatory pathway for phage therapy. Europe should muster the resources to financially, technically and legally support the introduction of phage therapy. EMBO Rep. 2013;14:951–4. doi: 10.1038/embor.2013.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verbeken G, Pirnay JP, Lavigne R, Jennes S, De Vos D, Casteels M, Huys I. Call for a dedicated European legal framework for bacteriophage therapy. Arch Immunol Ther Exp (Warsz) 2014;62:117–29. doi: 10.1007/s00005-014-0269-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pirnay JP, De Vos D, Verbeken G, Merabishvili M, Chanishvili N, Vaneechoutte M, Zizi M, Laire G, Lavigne R, Huys I, Van den Mooter G, Buckling A, Debarbieux L, Pouillot F, Azeredo J, Kutter E, Dublanchet A, Górski A, Adamia R. The phage therapy paradigm: prêt-à-porter or sur-mesure? Pharm Res. 2011;28:934–7. doi: 10.1007/s11095-010-0313-5. [DOI] [PubMed] [Google Scholar]
- 22.Pirnay JP, Verbeken G, Rose T, Jennes S, Zizi M, Huys I, Lavigne R, Merabishvili M, Vaneechoutte M, Buckling A, De Vos D. Introducing yesterday’s phage therapy in today’s medicine. Future Virol. 2012;7:379–90. [Google Scholar]
- 23.Villareal LP. Overall issues of virus and host evolution. In: Villareal LP, editor. Viruses and the evolution of life. Washington DC: ASM Press; 2005. pp. 1–28. [Google Scholar]
- 24.Endersen L, O'Mahony J, Hill C, Ross RP, McAuliffe O, Coffey A. Phage therapy in the food industry. Annu Rev Food Sci Technol. 2014;5:327–49. doi: 10.1146/annurev-food-030713-092415. [DOI] [PubMed] [Google Scholar]
- 25.Merabishvili M, Pirnay JP, Verbeken G, Chanishvili N, Tediashvili M, Lashkhi N, Glonti T, Krylov V, Mast J, Van Parys L, Lavigne R, Volckaert G, Mattheus W, Verween G, De Corte P, Rose T, Jennes S, Zizi M, De Vos D, Vaneechoutte M. Quality-controlled small-scale production of a well-defined bacteriophage cocktail for use in human clinical trials. PLoS One. 2009;4:e4944. doi: 10.1371/journal.pone.0004944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berg JO, Mössner BK, Skov MN, Lauridsen J, Gottrup F, Kolmos HJ. Antibacterial properties of EMLA and lidocaine in wound tissue biopsies for culturing. Wound Repair Regen. 2006;14:581–5. doi: 10.1111/j.1743-6109.2006.00157.x. [DOI] [PubMed] [Google Scholar]
- 27.Perez-Cappellano R, Manelli JC, Palayret D, Carlin G, Echinard C, Jouglard JP. Evaluation of septicemia risk in burn patients. Parallel between skin bacterial count and blood culture. Nouv Presse Med. 1976;5:1831–2. [PubMed] [Google Scholar]
- 28.Taddonio TE, Thomson PD, Tait MJ, Prasad JK, Feller I. Rapid quantification of bacterial and fungal growth in burn wounds: biopsy homogenate Gram stain versus microbial culture results. Burns Incl Therm Inj. 1988;14:180–4. doi: 10.1016/0305-4179(88)90035-6. [DOI] [PubMed] [Google Scholar]


